Abstract
In primary care centers, emotional disorders (EDs; depression, anxiety, and somatoform disorders) frequently appear to be associated. However, there is no previous information on the key (bridge) symptoms that maintain comorbidity. The current study aimed to identify symptoms that may play a linking role in bridging comorbidity among EDs from a network analysis perspective. A sample of adult primary care patients (N = 1704) with symptoms of EDs was assessed using the Patient Health Questionnaire (PHQ). Network analysis was applied to examine the network structure, communities, expected influence, and bridge symptoms between depressive, anxiety, and somatic symptoms. Sad mood and low energy were the most central symptoms. Furthermore, low energy, fainting spells, sad mood, and restlessness were detected as prominent bridge symptoms between anxiety, depression, and somatic symptoms. These bridge symptoms could be therapeutic targets for early intervention and prevent the development of comorbidity among EDs. The results of this research highlight the importance of symptom-specific functional properties for the activation of communities within EDs, providing new insights on a complex phenomenon such as comorbidity.
Similar content being viewed by others
Avoid common mistakes on your manuscript.
Introduction
The term comorbidity has traditionally been used in psychopathology to indicate that two or more different disorders co-occur at the same time in the same person (Feinstein, 1970). Comorbidity is very frequent among mental disorders worldwide (Vos et al., 2015). Approximately more than 40% of individuals presenting a mental disorder for at least one year meet the diagnostic criteria for an additional disorder in the same period (Kessler et al., 2005). In the primary care (PC) setting, a high prevalence of patients request help due to the presence of depression, anxiety, and/or somatic symptoms. In this context, the widespread use of transdiagnostic models justifies the high coexistence between symptoms of different disorders (Frances et al., 2020; González-Blanch, 2018a). This co-occurrence is not only associated with an unfavorable prognosis, such as poorer post-treatment outcomes, greater functional deterioration and disability, poorer quality of life, and/or higher suicide rates (Den Boeft et al., 2016; González-Blanch et al., 2018b; Walters et al., 2011), but also with an increased use of health services and a high cost burden for public health systems (Gilbody et al., 2006; Hüsing et al., 2018; Mahmud et al., 2021).
Comorbidity has been explained by the common-cause model as the covariation between two underlying and unobservable entities (i.e., disorders), giving rise to the observed symptoms (Fried et al., 2017). In recent years, the network approach has been proposed as an alternative conceptualization of comorbidity. This network approach argues that mental disorders could be understood as networks of symptoms that interact with each other, influencing mutually. Networks are composed of two fundamental elements: the nodes (circles) that represent the objects of study (in our case, symptoms) and the edges that represent the connections between the nodes. According to this approach, two or more subgroups of symptoms (communities) are directly interconnected by one or more intermediate symptoms that serve as a link, what are known as bridge symptoms (i.e., important symptoms for linking groups of nodes within the network) (Cramer et al., 2010). Conversely, communities are defined as a set of densely connected nodes (clusters) with more dispersed connections to outside nodes. In psychopathology, these communities represent subgroups of symptoms with topological properties similar (functional units) and different to the rest of the network (Fortunato & Hric, 2016). Identifying these communities can be useful to determine how the symptoms are grouped in the network, without assuming a prior organization based on the diagnostic categories of classification systems. The network view of symptoms as a complex interacting system (McNally, 2021) also involves the study of bridge symptoms that might link these communities (Jones et al., 2021) and thus provides insight about the potential role of specific symptoms in the development or maintenance of comorbidity. These analyses offer new ways to gain a better understanding about the complexity of comorbidity (Barthel et al., 2020; Dobson et al., 2021) since identifying symptoms could be potential therapeutic targets to prevent the activation of other communities.
Previous research has used network analysis to explore associations between anxiety and depression. For example, Cramer et al. (2010) analyzed symptom networks of major depressive disorder (MDD) and generalized anxiety disorder (GAD) and observed that the presence shared diagnostic symptoms (fatigue, sleep disturbance, concentration difficulty) favored the maintenance of comorbidity. Moreover, Beard et al. (2016) examined the relationship between anxiety and depression and found that symptoms of depressed mood and worrying too much had a greater influence than the rest of the nodes within the network. Interestingly, a recent study has shown that physical symptoms (e.g., agitation or psychomotor retardation, difficulty relaxing, or restlessness) could be key to understanding the frequent connection between depressive and anxious symptoms (Kaiser et al., 2021). Similar results were found by Park and Kim (2020), who observed that irritability and nervousness act as bridge symptoms in individuals with MDD and anxiety problems.
However, few investigations have included somatic symptoms within a network of anxiety and depressive symptoms to explore comorbidity, even though, as previously described, their association is high (González-Blanch, 2018a). Bekhuis et al., (2016a2016b) estimated the network structure of somatic symptoms and found that both neurovegetative and cognitive-affective symptoms of major depression and generalized anxiety have strong associations with somatic symptoms. The results also indicated the importance of analyzing the specific associations between the different emotional and somatic symptoms, instead of exclusively considering comorbidity as a nexus between disorders (Bekhuis et al., 2016a, 2016b). In this regard, they observed differences between the symptoms in terms of the strength of the association established with the symptoms of another domain (somatic or MDD/GAD). Most previous studies have focused on the association between symptoms of EDs. However, little information is available on the key (bridge) symptoms that could aid clinicians in selecting the optimal treatment and help reduce high rates of comorbidity. In sum, in this paper, we shed light on comorbidity of EDs at the symptom level. As such, we will examine whether some symptoms are more related to some than others, whether all symptoms are equally important, and whether there are other symptoms that act as a link to other symptom clusters. To this end, the present study uses a novel network methodology to identify symptoms that function as a link between the different domains (bridge symptoms) and detect the most relevant symptoms within the network (centrality).
This study aims to provide new information about which symptoms play a key role in the coexistence of EDs using a heterogeneous sample of PC patients with symptoms of EDs from a multicenter, randomized controlled trial (Cano-Vindel et al., 2021). We believe that our research is important because it analyzes certain system components (symptoms) and their interactions, which allows for a more detailed explanation of comorbidity. Thus, the objectives of the exploratory study are: (1) to study the associations between depressive, anxious, and somatic symptoms; (2) to explore the possible clustering of symptoms (communities); and (3) to identify the most central nodes of the network and the bridge symptoms using network analysis in PC individuals with EDs.
Methods
Participants
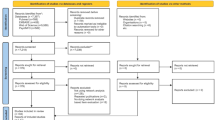
This study is part of a larger, randomized controlled trial (PsicAP) carried out in a total of 22 PC centers in eight regions of Spain (Andalusia, Basque region, Cantabria, Castilla la Mancha, Galicia, Madrid, Navarra, and Valencia) (for a detailed description see, Cano-Vindel et al., 2016). All individuals who visited their general practitioners (GPs) with signs or symptoms of negative emotional problems, i.e., depressive, anxious, or somatic symptomatology without a clear biological basis were considered candidates for participation in the study. The total sample consisted of 1704 participants. The sociodemographic and clinical characteristics of the sample are shown in Table 1.
Procedures
Individuals with symptoms of EDs were recruited in the PC setting by their GPs during a routine clinical visit. In this first phase, the candidates received detailed information about the study from their GPs. In addition, all those who chose to participate were given a patient information sheet and asked to sign an informed consent form. In a second phase, the participants included in the trial completed a battery of questionnaires in a first session with a clinical psychologist. The questionnaires included measures of clinical symptoms that were evaluated using the Patient Health Questionnaire (PHQ; Spitzer et al., 2006). Were also evaluated other emotional regulation strategies with the Penn State Worry Questionnaire-Abbreviated (PSWQ-A; Meyer et al., 1990), the Ruminative Responses Scale-Brooding (RRS-B, Nolen-Hoeksema & Morrow, 1991); the Metacognitions Questionnaire–Negative Beliefs (MCQ-NB; Wells & Cartwright-Hatton, 2004) and the Emotion Regulation Questionnaire (ERQ, Gross and John, 2013). In addition to functional status by means of the Sheehan Disability Scale (SDS; Luciano et al., 2010) and quality of life through the World Health Organization Quality of life Instrument-Abbreviated version (WhoQoL-Bref; Lucas-Carrasco, 2012).
The inclusion criteria were: (a) age 18–65 years; (b) presence of emotional symptomatology (anxiety, depression, and/or somatization); and (c) willingness to voluntarily participate in the study. The exclusion criteria were: (a) diagnosis of a severe mental disorder (e.g., bipolar or eating disorders); (b) presence of substance abuse or dependence; (c) any individual with personality disorder; and (d) frequent or recent suicide attempt(s).
The study protocol (PsicAP) was approved by the CEIC-APCV—the national research ethics committee coordinator— and the Spanish Medicines and Health Products Agency and conducted in accordance with the Declaration of Helsinki (EUDRACT: 2013–001,955-11). The trial has also been registered (“http://www.isrctn.com/ISRCTN58437086”).
Measures
Depressive Symptoms
The PHQ-9 (Kroenke et al., 2001) is a 9-item self-report scale that assesses the frequency of depressive symptoms over the last 2 weeks. Response options are measured on a 4-point Likert scale (0 = not at all; 1 = several days; 2 = more than half the days; 3 = nearly every day). The cut-off point for major depressive disorder (MDD) is usually a score of 10 (at least 5 items scored 2 [item 9 also scores 1], with item 1 or 2 amongst them). A score of 10–14 indicates minor depression, moderate MDD, or dysthymia; 15–19, moderately severe MDD; and 20–27, severe MDD (see Table 1). We used the validated Spanish version of the scale (González-Blanch et al. 2018c; Muñoz-Navarro et al., 2017a). In the present study, the internal consistency was good (α = 0.86).
Anxiety Symptoms
The Generalized Anxiety Disorder-7 (GAD-7; Spitzer et al., 2006) is a 7-item self-report scale that assesses the frequency of anxiety symptoms over the past 2 weeks. The GAD-7 uses a 4-point Likert scale (0 = not at all; 1 = several days; 2 = more than half the days; 3 = nearly every day). Cut points of 5, 10, and 15 represent mild, moderate, and severe anxiety, respectively. The algorithm sets 10 as the most optimal cut-off point for GAD (Spitzer et al., 2006). We used the validated Spanish version of the scale (Moreno et al., 2019; Muñoz-Navarro et al., 2017b). In the present study, the internal consistency was good (α = 0.86).
Somatic Symptoms
The PHQ-15 (Kroenke et al., 2002) is a 15-item self-report scale that assesses the frequency of somatic symptoms during the past 4 weeks on a 3-point Likert scale (0 = not bothered; 1 = bothered a little; 2 = bothered a lot). Cut points 5, 10, and 15 represent low, medium, and high somatic symptom severity, respectively. To detect a probable diagnosis of somatization disorder, at least 3 of the first 13 symptoms must obtain the maximum score (2 points). We used the Spanish version that includes 13 somatic symptoms (Ros Montalbán et al., 2010). In the present study, the internal consistency showed acceptable psychometric properties (α = 0.76).
Analytic plan
Data Preparation
Prior to the network analysis, we used the na.omit () function in R to remove any incomplete cases. The results show that there is no missing data. Conversely, a data-driven approach was applied to rule out possible items that might be measuring the same psychological construct. Following previous research (see Blanchard et al., 2021), we checked that the matrix correlation was positively definite and then searched for pairs of highly correlated nodes (r > 0.50) that shared more than 75% of the same correlations with other variables. With this aim, we used the goldbricker function available in the R package networktools (version 1.2.3; Jones, 2018). Two pairs of nodes were identified (items S10/S11: feeling your heart pound or race/shortness of breath and items S1/S13: stomach pain/nauseas, gas, or indigestion) as redundant and were therefore combined into a new variable (Tachycardia or choking “S10” and Abdominal pain “S11”). The new variables were combined manually obtaining the average of the scores using the SPSS statistical software. In addition, item S3 (Menstrual cramps or other problems with your periods) was removed to avoid potential bias. Therefore, for the current analysis, we used a total of 26 nodes (see Table 2).
Network Estimation
We performed the network analyses in RStudio software (version 4.2.2). A graphical Gaussian model (GGM) was used to estimate a network where each of 26 symptoms (i.e., depressive, anxiety, and somatic symptoms) are represented by nodes (i.e., circles), and edges (i.e., lines linking nodes) represent a regularized partial correlation between two nodes after controlling for the influence of the other nodes (Epskamp & Fried, 2018). The regularization procedure was executed using the EBICglasso function available in the R package qgraph (Epskamp et al., 2012), which implements the graphical LASSO regularization technique in combination with the extended Bayesian information criterion (EBIC) to minimize spurious associations. We chose a hyperparameter γ value of 0.5 as suggested by Foygel and Drton (2011) to obtain fewer links and hence a more parsimonious model.
Community Detection
To detect whether symptoms are clustered in one or more subgroups (i.e., “communities”), we implemented the spinglass algorithm using the spinglass.community function of the R package igraph (Csardi & Nepusz, 2006). This method enables detecting communities in networks with positive and negative edge values (Traag & Bruggeman, 2009). The community structure was obtained by applying the following parameters (γ = 0.5, start temperature = 1, stop temperature = 0.01, cooling factor = 0.99).
Expected Influence Centrality and Bridge Expected Influence
To determine the importance of each node within the network, we computed the expected influence (EI) centrality (Robinaugh et al., 2016). The EI of a node is the sum weight of all its edges incident on a given node, considering positive and negative values. High values of EI indicate greater centrality. Two new measures proposed by Robinaugh et al. (2016) were used to identify nodes with high influence: One-step expected influence (EI1) and two-step expected influence (EI2). The first (EI1) evaluates the immediate influence of a node with its nodes neighbors in the network (i.e., "neighbors" refers to nodes that are close to each other in the network structure and with those which share an edge. Second, EI2 explains a node’s immediate influence within the network as well as its secondary influence on the network through its neighbors, that is, it incorporates information about the expected influence of a node’s neighbors (Robinaugh et al., 2016). We also identified nodes that might play an important role in linking two or more communities, also known as bridge symptoms (Jones et al., 2021). To do so, we estimated two indices of bridge expected influence: one-step bridge expected influence (Bridge EI1), which measures the sum of the edge weights connecting a given node to all nodes in the other community or communities and two-step bridge expected influence (Bridge EI2), which considers the secondary influence of a node on the other communities through the influence of its neighbors’ nodes. Higher values indicate that these nodes are likely to activate other nearby communities, that is, nodes that play a key role in connecting groups of nodes to one another (Jones et al., 2021). Bridge symptoms can be evaluated using the bridge function of the R package networktools (Jones, 2018). Following previous guidelines (Epskamp et al., 2018), we also assessed the stability of expected influence and bridge expected influence centrality indices (see a detailed description and results in the Supplementary Material).
Network stability
We assess the robustness of the estimated parameters following previous guidelines (Epskamp et al., 2018). To do so, we made two steps using R package bootnet. First, we estimated the accuracy of the edge weights (Fig. S1), by using non-parametric bootstrapping (nboots = 1000). As a result, a confidence interval (CI) is estimated which contains 95% of the cases with the true value of the parameter. Results are depicted in Figure S1. Second, we assess the stability of the centrality indexes by relying on a case-dropping bootstrap procedure (Costenbader & Valente, 2003). Results are depicted in Figure S2 and calculated a correlation stability coefficient. According to the literature, the correlation stability coefficient should not be < 0.25 and preferably be ≥ 0.50 (Epskamp et al., 2018). Moreover, to identify significant differences between edge weights, bootstrapped difference test was used (Figure S3, S4).
Results
Network Estimation
The network estimated from the 26 symptoms is depicted in Fig. 1. The mean and standard deviation of study variables were: PHQ-9 (M = 13.32, SD = 6.46), GAD-7 (M = 11.73, SD = 5.26) and PHQ-15 (M = 13.45, SD = 5.45). Overall, the network structure is positively connected, and the results show the strongest correlations between items belonging to the same measure. For instance, anhedonia (D1) and sad mood (D2) show the within strongest edge-weights the depression domain. Within the anxiety domain, the edges with the strongest edge-weights were found between uncontrollable worry (A2) and worry too much (A3), and between nervousness or anxiety (A1) and worry too much (A3). The 3 strongest edge-weights between items in different communities were found between restlessness (A5) and psychomotor agitation/retardation (D8), trouble sleeping (D3) and trouble relaxing (A4), and between dizziness (S6) and fainting spells (S7). Robustness analyses show that the edge weights were estimated accurately (see the Supplementary Material, Figure S1).
Network structure of the 26 symptoms from PHQ-9, GAD-7 and PHQ-15 constructed via the spinglass community. Note. Nodes are coloured according to the clusters derived from the communities analysis. Green edges represent positive regularized partial correlations. Red edges negative regularized partial correlations
Community Detection
Our results revealed three communities in the EDs network (Fig. 1). Community 1 (cognitive-affective depression symptoms) include 6 nodes belonging to the depression domain (shown in yellow in Fig. 1), Community 2 (neurovegetative symptoms) contains 11 nodes belonging to both the depression and somatization domains (shown in dark pink) and Community 3 (mainly anxiety symptoms) contains 9 nodes, two of which are somatic symptoms (shown in blue).
Expected Influence Centrality and Bridge Expected Influence
The results revealed that sad mood (D2; EI1 = 1.14; EI2 = 2.21) and low energy (D4; EI1 = 1.24; EI2 = 2.07) showed the highest centrality in the network (see Fig. 2), followed by control worry (A2; EI1 = 1.04; EI2 = 1.90) and relax (A4; EI1 = 1.02; EI2 = 1.83). The Bridge EI1 and Bridge EI2 values are plotted in Fig. 3. Four nodes were identified as bridge symptoms: low energy (D4) (Bridge EI1 = 0.43; Bridge EI2 = 0.81), fainting spells (S7) (Bridge EI1 = 0.35; Bridge EI2 = 0.54), sad mood (Bridge EI1 = 0.27; Bridge EI2 = 0.67) and restlessness (A5) (Bridge EI1 = 0.32; Bridge EI2 = 0.55). These results indicate that these bridge symptoms (D4, S7, D2 and A5) appear to be key in the association between depressive, anxious, and somatic symptoms (see the Supplementary Material, Figure S5). The stability analysis reveals that both the EI and Bridge EI centrality indices are stable after sub-setting cases (see the Supplementary Material, Figure S2).
Discussion
There is a high comorbidity between symptoms of depression, anxiety, and somatization, which is reflected in requests for help in PC (Whiteford et al., 2015). To disentangle the complex association between these manifestations, the present study conceptualized comorbidity using the network approach and examined potential specific associations that may link the three different emotional domains. This study highlights that the presence of certain specific symptoms (e.g., low energy, fainting spells, sad mood and restlessness) may contribute to the maintenance of co-occurrence between symptoms of EDs. These results contribute to identifying some specific pathways of interaction between anxiety, depression, and somatic symptoms, which could aid in determining future interventions to prevent the development of symptoms and help reduce comorbidity. Furthermore, we observe that the strongest relationships are established between symptoms belonging to the same domain (i.e., anhedonia and sad mood for depressive symptoms and uncontrollable worry and worrying too much for anxiety symptoms), which is also consistent with previous research (Beard et al., 2016; Garabiles et al., 2019), even when somatic symptoms are included. Previous studies with people diagnosed with EDs obtained very similar results (e.g., Beard et al., 2016; Bekhuis et al., 2016a; Kaiser et al., 2021).
The present study also examines the most relevant symptoms within the EDs network structure. Our results show that sad mood is the most influential symptom in the network. This result is consistent with both previous research (Beard et al., 2016; Kaiser et al., 2021; Schellekens et al., 2020) and with the main diagnostic classification systems that establish sad mood as one of the fundamental symptoms for diagnosing depression according to the Diagnostic and Statistical Manual of Mental Disorders (DSM-5) and the International Classification of Diseases (ICD-11). Moreover, our results highlight that several overlapping symptoms of some disorders (e.g., low energy, difficulty relaxing) also present a high centrality in the network. This is in line with the data reported in previous studies (Fried et al., 2016; Kaiser et al., 2021) suggesting that not all symptoms are equally important. In this regard, Cramer et al. (2010) posited that that the most influential nodes could be preferential therapeutic targets (centrality hypothesis), although previous research has only found moderate evidence to support this hypothesis (Castro et al., 2019; Rodebaugh et al., 2018). In this line, Spiller et al. (2020) found that, among the centrality indices, only expected influence proved to be a good predictor of a decrease in the severity of symptoms, after inhibiting the most influential nodes. In the applied context, the lack of a detailed assessment to detect preferential and specific symptoms in individuals with diverse clinical features and different levels of severity may lead to them being diagnosed with the same disorder and thus receiving the same treatment, usually pharmacological (Mitchell et al., 2009). An advantage of detecting the specific symptoms that an individual patient is experiencing is that we can adopt a symptom-based intervention strategy. This also applies to drug treatment. For example, fatigue and concentration are mainly regulated by norepinephrine and dopamine. Certain antidepressants, such as norepinephrine and dopamine reuptake inhibitors (NDRIs), regulate these neurotransmitters, so selecting a psychotropic drug with this principle of action may possibly help reduce specific symptoms more quickly and not require the use of without using randomized intervention strategies (Stahl, 2013).
On the other hand, the detection of communities identified three subgroups of symptoms within the EDs network. In this structure, we found four symptoms that showed the highest expected bridge influence values: low energy (D4), fainting spells (S7), sad mood (D2), and restlessness (A5). Two of these bridge symptoms (D4 and D2) seem to connect the cluster of depressive symptoms having a greater cognitive component (Cognitive-affective community, shown in yellow in Fig. 1) with the more physical or somatic symptoms (Neurovegetative community). The restlessness node (A5) also appears to play a key role in the connection between Cognitive-affective community and the other two communities, which is in line with the findings of a recent study by Kaiser et al. (2021). Fainting spells (S7) appears as a key symptom to link the three symptom clusters.
The strongest bridge symptoms between EDs detected in this study were predominantly physical. Specifically, these symptoms reflect low energy, restlessness, and fainting spells. Previous research has highlighted physical symptoms as important when comorbidity is present. For example, a study by Helgadóttir et al. (2015) showed that patients with comorbid anxiety and depression had greater physical activity than people with only one disorder. Interestingly, several authors have indicated the importance of detecting possible somatic symptoms in the assessment, since their presence predicts a worse prognosis for depressive disorder (Bekhuis et al., 2016b). Accordingly, De Waal et al. (2004) showed that if patients consider their problems as physical, they may be less motivated to start psychological treatment, thus highlighting the importance of identifying somatic symptoms in the context of PC to plan for a more adjusted intervention (De Waal et al., 2008). Therefore, including physiological measures in the network could be useful to elucidate comorbidity processes.
Our findings also have several implications. Overall, our results highlight the usefulness of adopting a symptom-specific approach and investigating the role each node plays within the network to gain a more complete idea of the interrelationship between symptoms of EDs. This conceptualization offers a complementary network model that emphasizes relationships at the symptom level (Jones et al., 2018). In this regard, knowing how the symptoms are related has implications in terms of patient evaluations, that is, detecting the presence of certain symptoms could help clinicians to assess the possibility that other symptoms are present or may develop. In particular, our results suggest that deactivating the symptoms of restlessness, low energy, fainting spells, and sad mood, could weaken the general activation of the network and improve the prognosis of people with comorbidity, although experimental studies would be necessary to validate this hypothesis.
Regarding the limitations, first, our study used cross-sectional data. Therefore, temporal relationships and the potential directionality of relationships among symptoms of EDs could not be identified. We encourage future research on temporal networks using intensive data to gain insight into the potential temporality between these associations. Second, the symptoms were assessed using self-report questionnaires, which could lead to desirability biases, although it should be noted that these are well-validated tests. Third, the questionnaires administered in the present study may not have covered all possible symptoms of EDs, thus precluding a holistic explanation of comorbidity mechanisms (Fried et al., 2017). Comorbidity was examined paying attention exclusively to symptoms, therefore it would be extremely beneficial that future research include non-symptomatic variables (e.g., cognitive mechanisms, socioeconomic factors) to avoid a reductionist approach. Finally, our results are supported by a sample of subjects with mild to moderate emotional disorders. Therefore, it would be of interest to obtain further results with more serious disorders or in other disorders.
Despite these limitations, the present study has several strengths. First, to the best of our knowledge, this is the first study that has used network analysis to examine the interrelationships between anxiety, depression, and somatic symptoms in PC patients with comorbidity. Second, we have used this network approach because we think that it can aid in revealing other important aspects of a complex phenomenon such as comorbidity that until now has only been investigated using more traditional methodologies. Finally, additional analyses have been applied to verify that the estimated data are robust.
In conclusion, and to our knowledge, this is the first study to examine symptom-level comorbidity in people with emotional disorders in a primary care setting using a network approach. Although these findings are preliminary, the present study adds new data to the existing literature on the comorbidity of EDs. Specifically, the results suggest that low energy (D4), fainting spells (S7), sad mood (D2), and restlessness (A5) may be symptoms to connect and activate other symptom clusters, suggesting possible pathways for the development and maintenance of comorbidity in EDs. This novel methodology offered the opportunity to observe some symptom-level mechanisms to understand comorbidity in EDs and, if replicated, may help us to better understand the onset and development of EDs comorbidity and, on the other hand, to improve intervention strategies to treat such emotional problems.
Data availability
The datasets generated during and/or analysed during the current study are available from the corresponding author on reasonable request.
References
Barthel, A. L., Pinaire, M., Curtiss, J., Baker, A., Brown, M. L., Hoeppner, S., Bui, E., Simon, N., & Hofmann, S. (2020). Anhedonia is central for the association between quality of life, metacognition, sleep, and affective symptoms in generalized anxiety disorder: A complex network analysis. Journal of Affective Disorders, 277, 1013–1021. https://doi.org/10.1016/j.jad.2020.08.077
Beard, C., Millner, A. J., Forgeard, M. J., Fried, E. I., Hsu, K. J., Treadway, M. T., Leonard, C. V., Kertz, S. J., & Björgvinsson, T. (2016). Network analysis of depression and anxiety symptom relationships in a psychiatric sample. Psychological Medicine, 46(16), 3359–3369. https://doi.org/10.1017/S0033291716002300
Bekhuis, E., Boschloo, L., Rosmalen, J. G., de Boer, M. K., & Schoevers, R. A. (2016a). The impact of somatic symptoms on the course of major depressive disorder. Journal of Affective Disorders, 205, 112–118. https://doi.org/10.1016/j.jad.2016.06.030
Bekhuis, E., Schoevers, R. A., van Borkulo, C. D., Rosmalen, J. G., & Boschloo, L. (2016b). The network structure of major depressive disorder, generalized anxiety disorder and somatic symptomatology. Psychological Medicine, 46(14), 2989–2998. https://doi.org/10.1017/S0033291716001550
Blanchard, M. A., Roskam, I., Mikolajczak, M., & Heeren, A. (2021). A network approach to parental burnout. Child abuse & neglect, 111, 104826. https://doi.org/10.1016/j.chiabu.2020.104826
Cano-Vindel, A., Muñoz-Navarro, R., Wood, C. M., Limonero, J. T., Medrano, L. A., Ruiz-Rodríguez, P., Gracia-Gracia, I., Dongil-Collado, E., Iruarrizaga, I., Chacón, F., & Santolaya, F. (2016). Transdiagnostic Cognitive Behavioral Therapy Versus Treatment as Usual in Adult Patients with Emotional Disorders in the Primary Care Setting (PsicAP Study): Protocol for a Randomized Controlled Trial. JMIR research protocols, 5(4), e246. https://doi.org/10.2196/resprot.6351
Cano-Vindel, A., Muñoz-Navarro, R., Moriana, J. A., Ruiz-Rodríguez, P., Medrano, L. A., González-Blanch, C. (2021). Transdiagnostic group cognitive behavioural therapy for emotional disorders in primary care: the results of the PsicAP randomized controlled trial. Psychological Medicine 1–13. https://doi.org/10.1017/S0033291720005498
Castro, D., Ferreira, F., de Castro, I., Rodrigues, A. R., Correia, M., Ribeiro, J., & Ferreira, T. B. (2019). The Differential Role of Central and Bridge Symptoms in Deactivating Psychopathological Networks. Frontiers in Psychology, 10, 2448. https://doi.org/10.3389/fpsyg.2019.02448
Costenbader, E., & Valente, T. W. (2003). The stability of centrality measures when networks are sampled. Social Networks, 25(4), 283–307. https://doi.org/10.1016/S0378-8733(03)00012-1
Cramer, A. O., Waldorp, L. J., van der Maas, H. L., & Borsboom, D. (2010). Comorbidity: A network perspective. The Behavioral and Brain Sciences, 33(2–3), 137–193. https://doi.org/10.1017/S0140525X09991567
Csardi, G., & Nepusz, T. (2006). The igraph software package for complex network research. InterJournal Complex Systems, 1695
de Waal, M. W., Arnold, I. A., Eekhof, J. A., & van Hemert, A. M. (2004). Somatoform disorders in general practice: Prevalence, functional impairment and comorbidity with anxiety and depressive disorders. The British Journal of Psychiatry: The Journal of Mental Science, 184, 470–476. https://doi.org/10.1192/bjp.184.6.470
de Waal, M. W., Arnold, I. A., Eekhof, J. A., Assendelft, W. J., & van Hemert, A. M. (2008). Follow-up study on health care use of patients with somatoform, anxiety and depressive disorders in primary care. BMC Family Practice, 9, 5. https://doi.org/10.1186/1471-2296-9-5
den Boeft, M., Twisk, J. W., Hoekstra, T., Terluin, B., Penninx, B. W., van der Wouden, J. C., Numans, M. E., & van der Horst, H. E. (2016). Medically unexplained physical symptoms and work functioning over 2 years: Their association and the influence of depressive and anxiety disorders and job characteristics. BMC Family Practice, 17, 46. https://doi.org/10.1186/s12875-016-0443-x
Dobson, E. T., Croarkin, P. E., Schroeder, H. K., Varney, S. T., Mossman, S. A., Cecil, K., & Strawn, J. R. (2021). Bridging Anxiety and Depression: A Network Approach in Anxious Adolescents. Journal of Affective Disorders, 280(Pt A), 305–314. https://doi.org/10.1016/j.jad.2020.11.027
Epskamp, S., & Fried, E. I. (2018). A tutorial on regularized partial correlation networks. Psychological Methods. https://doi.org/10.1037/met0000167
Epskamp, S., Cramer, A. O. J., Waldorp, L. J., Schmittmann, V. D., & Borsboom, D. (2012). qgraph: Network Visualizations of Relationships in Psychometric Data. Journal of Statistical Software, 48(4), 1–18. https://doi.org/10.18637/jss.v048.i04
Epskamp, S., Borsboom, D., & Fried, E. I. (2018). Estimating psychological networks and their accuracy: A tutorial paper. Behavior Research Methods, 50(1), 195–212. https://doi.org/10.3758/s13428-017-0862-1
Feinstein, A. R. (1970). The pre-therapeutic classification of co-morbidity in chronic disease. Journal of Chronic Diseases, 23(7), 455–468. https://doi.org/10.1016/0021-9681(70)90054-8
Fortunato, S., & Hric, D. (2016). Community detection in networks: A user guide. Physics Reports, 659, 1–44. https://doi.org/10.1016/j.physrep.2016.09.002
Foygel, R., & Drton, M. (2011). Bayesian model choice and information criteria in sparse generalized linear models. Arxiv Preprint ArXiv:1112.5635 1–37. https://doi.org/10.1038/srep05918
Frances, S., Shawyer, F., Cayoun, B., Enticott, J., & Meadows, G. (2020). Study protocol for a randomized control trial to investigate the effectiveness of an 8-week mindfulness-integrated cognitive behavior therapy (MiCBT) transdiagnostic group intervention for primary care patients. BMC Psychiatry, 20(1), 7. https://doi.org/10.1186/s12888-019-2411-1
Fried, E. I., Epskamp, S., Nesse, R. M., Tuerlinckx, F., & Borsboom, D. (2016). What are “good” depression symptoms? Comparing the centrality of DSM and non-DSM symptoms of depression in a network analysis. Journal of Affective Disorders, 189, 314–320. https://doi.org/10.1016/j.jad.2015.09.005
Fried, E. I., van Borkulo, C. D., Cramer, A. O., Boschloo, L., Schoevers, R. A., & Borsboom, D. (2017). Mental disorders as networks of problems: A review of recent insights. Social Psychiatry and Psychiatric Epidemiology, 52(1), 1–10. https://doi.org/10.1007/s00127-016-1319-z
Garabiles, M. R., Lao, C. K., Xiong, Y., & Hall, B. J. (2019). Exploring comorbidity between anxiety and depression among migrant Filipino domestic workers: A network approach. Journal of Affective Disorders. https://doi.org/10.1016/j.jad.2019.02.062
Gilbody, S., Bower, P., & Whitty, P. (2006). Costs and consequences of enhanced primary care for depression: Systematic review of randomised economic evaluations. The British Journal of Psychiatry: The Journal of Mental Science, 189, 297–308. https://doi.org/10.1192/bjp.bp.105.016006
González-Blanch, C., Hernández-de-Hita, F., Muñoz-Navarro, R., et al. (2018). The association between different domains of quality of life and symptoms in primary care patients with emotional disorders. Science and Reports, 8, 11180. https://doi.org/10.1038/s41598-018-28995-6
González-Blanch, C., Hernández-de-Hita, Fernando, Muñoz-Navarro, R., Ruíz-Rodríguez, P., Medrano, L. A., Moriana, J. A., Cano-Vindel, A., Psic AP ResearchGroup. (2018). Domain-specific associations between disability and depression, anxiety, and somatization in primary care patients. Psychiatry research, 269, 596–601. https://doi.org/10.1016/j.psychres.2018.09.007
González-Blanch, C., Medrano, L. A., Muñoz-Navarro, R., Ruíz-Rodríguez, P., Moriana, J. A., Limonero, J. T., Schmitz, F., Cano-Vindel, A., PsicAPResearchGroup. (2018). Factor structure and measurement invariance across various demographic groups and over time for the PHQ-9 in primary care patients in Spain. PloS one, 13(2), e0193356. https://doi.org/10.1371/journal.pone.0193356
Gross, James J.; John, O.P., 2013. Emotion Regulation Questionnaire (ERQ). J. Pers.
Helgadóttir, B., Forsell, Y., & Ekblom, Ö. (2015). Physical activity patterns of people affected by depressive and anxiety disorders as measured by accelerometers: a cross-sectional study. PloS one, 10(1), e0115894. https://doi.org/10.1371/journal.pone.0115894
Hüsing, P., Löwe, B., Piontek, K., & Shedden-Mora, M. (2018). Somatoform disorder in primary care: The influence of co-morbidity with anxiety and depression on health care utilization. Journal of Evaluation in Clinical Practice, 24(4), 892–900. https://doi.org/10.1111/jep.12898
Jones, P. J., Mair, P., Riemann, B. C., Mugno, B. L., & McNally, R. J. (2018). A network perspective on comorbid depression in adolescents with obsessive-compulsive disorder. Journal of Anxiety Disorders, 53, 1–8. https://doi.org/10.1016/j.janxdis.2017.09.008
Jones, P. J., Ma, R., & McNally, R. J. (2021). Bridge Centrality: A Network Approach to Understanding Comorbidity. Multivariate Behavioral Research, 56(2), 353–367. https://doi.org/10.1080/00273171.2019.1614898
Jones, P. J. (2018). Networktools: Tools for identifying important nodes in networks. (R package version 1.2, 1.). https://cran.r-project.org/package=networktools
Kaiser, T., Herzog, P., Voderholzer, U., & Brakemeier, E. (2021). Unraveling the comorbidity of depression and anxiety in a large inpatient sample: Network analysis to examine bridge symptoms. Depression and Anxiety., 38, 307–317. https://doi.org/10.1002/da.23136
Kessler, R. C., Chiu, W. T., Demler, O., Merikangas, K. R., & Walters, E. E. (2005). Prevalence, severity, and comorbidity of 12-month DSM-IV disorders in the National Comorbidity Survey Replication. Archives of General Psychiatry, 62(6), 617–627. https://doi.org/10.1001/archpsyc.62.6.617
Kroenke, K., Spitzer, R. L., & Williams, J. B. (2001). The PHQ-9: Validity of a brief depression severity measure. Journal of General Internal Medicine, 16(9), 606–613. https://doi.org/10.1046/j.1525-1497.2001.016009606.x
Kroenke, K., Spitzer, R. L., & Williams, J. B. (2002). The PHQ-15: Validity of a new measure for evaluating the severity of somatic symptoms. Psychosomatic Medicine, 64(2), 258–266. https://doi.org/10.1097/00006842-200203000-00008
Lucas-Carrasco, R. (2012). The WHO quality of life (WHOQOL) questionnaire: Spanish development and validation studies. Quality of Life Research : An International Journal of Quality of Life Aspects of Treatment, Care and Rehabilitation, 21(1), 161–165. https://doi.org/10.1007/s11136-011-9926-3
Luciano, J. V., Bertsch, J., Salvador-Carulla, L., Tomás, J. M., Fernández, A., Pinto-Meza, A., Haro, J. M., Palao, D. J., & Serrano-Blanco, A. (2010). Factor structure, internal consistency and construct validity of the Sheehan Disability Scale in a Spanish primary care sample. Journal of Evaluation in Clinical Practice, 16(5), 895–901. https://doi.org/10.1111/j.1365-2753.2009.01211.x
Mahmud, S., Hossain, S., Muyeed, A., Islam, M. M., & Mohsin, M. (2021). The global prevalence of depression, anxiety, stress, and insomnia and its changes among health professionals during COVID-19 pandemic: A rapid systematic review and meta-analysis. Heliyon, 7(7), e07393. https://doi.org/10.1016/j.heliyon.2021.e07393
McNally, R. J. (2021). Network Analysis of Psychopathology: Controversies and Challenges. Annual Review of Clinical Psychology, 17, 31–53. https://doi.org/10.1146/annurev-clinpsy-081219-092850
Meyer, T. J., Miller, M. L., Metzger, R. L., & Borkovec, T. D. (1990). Development and validation of the Penn State Worry Questionnaire. Behaviour Research and Therapy, 28(6), 487–495. https://doi.org/10.1016/0005-7967(90)90135-6
Mitchell, A. J., Vaze, A., & Rao, S. (2009). Clinical diagnosis of depression in primary care: A meta-analysis. Lancet (london, England), 374(9690), 609–619. https://doi.org/10.1016/S0140-6736(09)60879-5
Moreno, E., Muñoz-Navarro, R., Medrano, L. A., González-Blanch, C., Ruiz-Rodríguez, P., Limonero, J. T., Moretti, L. S., Cano-Vindel, A., & Moriana, J. A. (2019). Factorial invariance of a computerized version of the GAD-7 across various demographic groups and over time in primary care patients. Journal of Affective Disorders, 252, 114–121. https://doi.org/10.1016/j.jad.2019.04.032
Muñoz-Navarro, R., Cano-Vindel, A., Medrano, L. A., Schmitz, F., Ruiz-Rodríguez, P., Abellán-Maeso, C., Font-Payeras, M. A., & Hermosilla-Pasamar, A. M. (2017a). Utility of the PHQ-9 to identify major depressive disorder in adult patients in Spanish primary care centres. BMC Psychiatry, 17(1), 291. https://doi.org/10.1186/s12888-017-1450-8
Muñoz-Navarro, R., Cano-Vindel, A., Moriana, J. A., Medrano, L. A., Ruiz-Rodríguez, P., Agüero-Gento, L., Rodríguez-Enríquez, M., Pizà, M. R., & Ramírez-Manent, J. I. (2017b). Screening for generalized anxiety disorder in Spanish primary care centers with the GAD-7. Psychiatry Research, 256, 312–317. https://doi.org/10.1016/j.psychres.2017.06.023
Nolen-Hoeksema, S., & Morrow, J. (1991). A prospective study of depression and posttraumatic stress symptoms after a natural disaster: The 1989 Loma Prieta Earthquake. Journal of Personality and Social Psychology, 61(1), 115–121. https://doi.org/10.1037//0022-3514.61.1.115
Park, S. C., & Kim, D. (2020). The Centrality of Depression and Anxiety Symptoms in Major Depressive Disorder Determined Using a Network Analysis. Journal of Affective Disorders, 271, 19–26. https://doi.org/10.1016/j.jad.2020.03.078
Robinaugh, D. J., Millner, A. J., & McNally, R. J. (2016). Identifying highly influential nodes in the complicated grief network. Journal of Abnormal Psychology, 125(6), 747–757. https://doi.org/10.1037/abn0000181
Rodebaugh, T. L., Tonge, N. A., Piccirillo, M. L., Fried, E., Horenstein, A., Morrison, A. S., Goldin, P., Gross, J. J., Lim, M. H., Fernandez, K. C., Blanco, C., Schneier, F. R., Bogdan, R., Thompson, R. J., & Heimberg, R. G. (2018). Does centrality in a cross-sectional network suggest intervention targets for social anxiety disorder? Journal of Consulting and Clinical Psychology, 86(10), 831–844. https://doi.org/10.1037/ccp0000336
RosMontalbán, S., Comas Vives, A., & Garcia-Garcia, M. (2010). Validation of the Spanish version of the PHQ-15 questionnaire for the evaluation of physical symptoms in patients with depression and/or anxiety disorders: DEPRE-SOMA study. Actas Españolas De Psiquiatría, 38(6), 345–357.
Schellekens, M., Wolvers, M., Schroevers, M. J., Bootsma, T. I., Cramer, A., & van der Lee, M. L. (2020). Exploring the interconnectedness of fatigue, depression, anxiety and potential risk and protective factors in cancer patients: A network approach. Journal of Behavioral Medicine, 43(4), 553–563. https://doi.org/10.1007/s10865-019-00084-7
Spiller, T. R., Levi, O., Neria, Y., Suarez-Jimenez, B., Bar-Haim, Y., & Lazarov, A. (2020). On the validity of the centrality hypothesis in cross-sectional between-subject networks of psychopathology. BMC Medicine, 18(1), 297. https://doi.org/10.1186/s12916-020-01740-5
Spitzer, R. L., Kroenke, K., Williams, J. B., & Löwe, B. (2006). A brief measure for assessing generalized anxiety disorder: The GAD-7. Archives of Internal Medicine, 166(10), 1092–1097. https://doi.org/10.1001/archinte.166.10.1092
Stahl, S. M. (2013). Essential psychopharmacology. Neuroscientific basis and practical applications (4th ed.). Cambridge University Press.
Traag, V. A., & Bruggeman, J. (2009). Community detection in networks with positive and negative links. Physical Review E - Statistical, Nonlinear, and Soft Matter Physics, 80(3), 1–6. https://doi.org/10.1103/PhysRevE.80.036115
Vos, T., Barber, R. M., Bell, B., Bertozzi-Villa, A., Biryukov, S., Bolliger, I., et al. (2015). Global, regional, and national incidence, prevalence, and years lived with disability for 301 acute and chronic diseases and injuries in 188 countries, 1990–2013: A systematic analysis for the Global Burden of Disease study. Lancet, 386. https://doi.org/10.1016/S0140-6736(15)60692-4
Walters, K., Buszewicz, M., Weich, S., & King, M. (2011). Mixed anxiety and depressive disorder outcomes: Prospective cohort study in primary care. The British Journal of Psychiatry: The Journal of Mental Science, 198(6), 472–478. https://doi.org/10.1192/bjp.bp.110.085092
Wells, A., & Cartwright-Hatton, S. (2004). A short form of the metacognitions questionnaire: Properties of the MCQ-30. Behaviour Research and Therapy, 42(4), 385–396. https://doi.org/10.1016/S0005-7967(03)00147-5
Whiteford, H. A., Ferrari, A. J., Degenhardt, L., Feigin, V., & Vos, T. (2015). The global burden of mental, neurological and substance use disorders: an analysis from the Global Burden of Disease Study 2010. PloS one, 10(2), e0116820. https://doi.org/10.1371/journal.pone.0116820
Acknowledgements
The authors wish to thank to all the persons who participated in the study and all the physicians and psychologists who collaborated in the projects.
Funding
Funding for open access publishing: Universidad de Córdoba/CBUA. This work was supported by the Regional Government of Andalusia of European Regional Development Fund (ERDF) [1380654-F]. This research did not receive any specific grant from funding agencies in the public, commercial, or not-for-profit sectors.
Author information
Authors and Affiliations
Corresponding author
Ethics declarations
Ethical standards
The authors assert that all procedures contributing to this work comply with the ethical standards of the relevant national and institutional committees on human experimentation and with the Helsinki Declaration of 1975, as revised in 2008.
Conflict of interest
The authors declare that they have no conflict of interest.
Additional information
Publisher's note
Springer Nature remains neutral with regard to jurisdictional claims in published maps and institutional affiliations.
Supplementary Information
Below is the link to the electronic supplementary material.
Rights and permissions
Open Access This article is licensed under a Creative Commons Attribution 4.0 International License, which permits use, sharing, adaptation, distribution and reproduction in any medium or format, as long as you give appropriate credit to the original author(s) and the source, provide a link to the Creative Commons licence, and indicate if changes were made. The images or other third party material in this article are included in the article's Creative Commons licence, unless indicated otherwise in a credit line to the material. If material is not included in the article's Creative Commons licence and your intended use is not permitted by statutory regulation or exceeds the permitted use, you will need to obtain permission directly from the copyright holder. To view a copy of this licence, visit http://creativecommons.org/licenses/by/4.0/.
About this article
Cite this article
Jurado-González, F., García-Torres, F., Contreras, A. et al. Mapping bridges between anxiety, depression, and somatic symptoms in primary care patients: a network perspective. Curr Psychol 43, 4292–4304 (2024). https://doi.org/10.1007/s12144-023-04657-3
Accepted:
Published:
Issue Date:
DOI: https://doi.org/10.1007/s12144-023-04657-3