Abstract
Autism Spectrum Disorder (ASD) and Attention Deficit Hyperactivity Disorder (ADHD) are two often co-occurring neurodevelopmental conditions. Nevertheless, there is limited research about symptom differences between ASD and ASD + ADHD groups. This study examined differences in social interaction and communication between children and adolescents with ASD and with ASD + ADHD. A total of 112 participants were identified from two clinical trials. Fifty-six children and adolescents with ASD aged 8–17 years were matched for age, gender and general intelligence quotient with fifty-six children and adolescents with ASD + ADHD. Group differences in scores on the Autism Diagnostic Observation Schedule were analysed. Our results showed that participants with ASD and with ASD + ADHD had similar profiles of social communication interaction challenges and restricted behaviour. However, items assessing gestures: Conventional, Instrumental or Informational Gestures and Empathic or Emotional gestures showed significant differences between the groups suggesting that the ASD + ADHD group used descriptive gestures to communicate to a greater extent than the ASD group. These findings suggest that children and adolescents in both groups have similar difficulties in social communication and interaction with observed differences in the use of gestures. Possible reasons and implications for the differences in the use of gestures are discussed.
Similar content being viewed by others
Avoid common mistakes on your manuscript.
Autism Spectrum Disorder (ASD) and Attention Deficit Hyperactivity Disorder (ADHD) are two neurodevelopmental conditions of common heredity and overlapping difficulties, but also distinct differences (Bölte et al., 2018; Antshel & Russo, 2019). Prior to Diagnostic and Statistical Manual of Mental Disorders, 5th Edition (DSM-5; American Psychiatric Association [APA], 2013) research mainly focused on if inattention, hyperactivity, and impulsivity in individuals with autism were considered secondary to autism or main characteristics of ADHD (Antshel & Russo, 2019). When the DSM-5 (APA) was released in 2013, the mutual exclusion criterion for ADHD and ASD in DSM-IV (APA, 2000) was abandoned. The same is true for ICD-11 (World Health Organization, 2019). Meta-analytical findings show that the prevalence rate of ADHD in ASD is 39.4% among children (6–11 years) and 38.8% among adolescents (12–17 years; Rong et al., 2021), and is today one of the most commonly diagnosed co-occurring conditions in ASD (Lugo-Marín et al., 2019).
Despite the fact that an understanding of how ASD and ADHD symptoms interact is emerging, larger conclusive studies are lacking (Antshel & Russo, 2019). One area that has been studied extensively in ASD with co-occurring ADHD is executive functions (EF) such as working memory, inhibition, cognitive flexibility, and planning (Antshel & Russo, 2019). There are also implications that EF affects social communication in ASD (Hull et al., 2021; Livingston et al., 2019). Children with ASD + ADHD seem to have a combination of difficulties in EF from both conditions: directing attention and inhibiting impulses from ADHD and dealing with competing stimuli and shifting focus associated with ASD (Tye et al., 2014; Unterrainer et al., 2016) have shown that children with ASD + ADHD perform significantly better than children with only ASD on tests that require multi-step planning. They suggest that the impulsivity from ADHD increases flexibility in ASD, and disrupts the behavioural rigidity. In this type of task ADHD symptoms seem beneficial (Unterrainer et al., 2016). Few studies focus on the impact of co-occurring ADHD symptoms on social interaction in individuals with ASD. Facial emotion recognition ability is mainly affected in children with ADHD and ADHD + ASD compared to those with only ASD (Sinzig et al., 2008). A higher degree of ADHD symptoms seems to be associated with a higher degree of social problems, rule-breaking behaviour, and aggressive behaviour in children with ASD + ADHD (Mansour et al., 2017). Little is known about how ADHD related symptoms affect non-verbal communication such as eye contact, directing facial expressions, the use of gestures and taking social initiatives or interpreting social situations. When autistic symptoms are assessed, these socio communicative skills are evaluated.
Diagnosing ASD in individuals with co-occurring ADHD may be challenging (Gargaro et al., 2011), and the diagnosis of ASD may be delayed or initially diagnosed as only ADHD (Kentrou et al., 2019; Stevens et al., 2016) when there is a behavioural overlap between ASD and ADHD. Consequently, the lack of knowledge about the symptom differences between ASD and ASD + ADHD may lead to incorrect or delayed diagnosis, which leads to a delay in adequate intervention (e.g., societal support and health care). Further, the individuals may not get optimal interventions, such as psychoeducation adapted to this group.
To date, it is unclear to what extent standardised diagnostic measures can effectively capture the ASD and ADHD symptoms of children that meet the criteria for both conditions. Previous studies show that semi-structured observations, such as The Autism Diagnostic Observation Schedule (ADOS; Lord et al., 2000, 2009, 2014), commonly used with neurodevelopmental assessments can discern ADHD from ASD + ADHD sufficiently (Harkins et al., 2022; Ng et al., 2019; Salley et al., 2015). Only one of these studies (Harkins et al., 2022) was based on a larger sample, but their study focused on diagnostic evaluation. Still, little is known of what differentiates ASD + ADHD from ASD in regard to symptoms. The objective of this study was to investigate whether there are symptom differences between children and adolescents with ASD and those with ASD + ADHD when using common clinical instruments for measuring ASD symptoms in a larger sample and in a naturalistic clinical setting.
Method
Participants
The participants were selected from a previously collected sample from two randomised controlled trials focusing on the efficacy of social skills group training KONTAKT® (Choque Olsson et al., 2017; Jonsson et al., 2019). Inclusion criteria in the prior studies were: clinical ASD diagnosis; assessed with ADOS-Generic (ADOS-G; Lord et al., 2000, 2009) and in some cases the ADOS-2 (Lord et al., 2014); age between 8 and 17 years; full-scale IQ scores > 70 according to the Wechsler Intelligence Scale for Children, third or fourth edition (Wechsler, 1991, 2004); at least one co-occurring psychiatric condition such as ADHD, anxiety and depression according to International Classification of Diseases and Related Health Problems-tenth revision, ICD-10 (WHO, 2016). Exclusion criteria were: clinically assessed self-injury, an ICD-10 diagnosis of conduct disorder, antisocial or borderline personality disorder, any psychotic disorder that would interfere with participation or require alternative treatment, and insufficient Swedish language capacities.
For the purpose of the present study, only the participants with a complete baseline measure and a complete ADOS-G algorithm were selected and divided into two groups according to the presence or absence of ADHD. The groups were matched on age, gender and Full Scale Intelligence Quotient. The final sample consisted of 112 children and adolescents with ASD: n = 56 with ASD without ADHD (ASD), and n = 56 with ASD and co-occurring ADHD (ASD + ADHD). See Table 1.
There were no significant gender, age or general intelligence differences between the groups due to the matched sample (Table 1). ADOS-G module 3 was used to assess children and younger adolescents, while Module 4 was used on older adolescents. There were no significant differences between the groups on which the ADOS-G module was used χ2(1) = 1.76, p = .18. Although there were group differences in regard to co-occurring anxiety (ASD: 50%, AD + ADHD: 2%) ad depression (ASD: 54%, AD + ADHD: 9%) cnditions, there were no significant differences between the groups in regard to other co-occurring conditions (Table 1). Written consent from participants and their parents (or custodians) was obtained. The studies from which the participants were selected were approved by the ethical committee board in Stockholm (2012 / 385 − 31 / 4) (Choque Olsson et al., 2017; Jonsson et al., 2019).
Procedure
Participants were recruited from the Child and Adolescent Psychiatric outpatient clinics (CAP) in Stockholm. The data collection was conducted between August 2012 and October 2015 for the first trial (Choque Olsson et al., 2017) and between January 2013 and December 2015 for the second trial (Jonsson et al., 2019). All participants had a clinical ASD spectrum diagnosis after a child neuropsychiatric examination. Neuropsychiatric investigations in CAP in Stockholm are carried out by multidisciplinary teams consisting of at least one psychologist and one child psychiatrist (Choque Olsson et al., 2010, 2012). Differential diagnoses and co-occurring conditions are included in the assessment. ADOS is included along with intelligence testing (Choque Olsson et al., 2010, 2012) and is conducted by clinically trained examiners (Zander et al., 2016). The neurodevelopmental diagnosis was confirmed by requesting the child and adolescent psychiatric report from the clinic. Participants’ co-occurring conditions, which also included ADHD, were confirmed with information from the Child and Adolescent Psychiatric Report, medical records, or through a supplemental interview using the Kiddie Schedule of Affective Disorders and Schizophrenia (Kaufman et al., 1997).
Measurement
The Autism Diagnostic Observation Schedule (ADOS; Lord et al., 2000, 2009, 2014) is a clinician-rated semi-structured observation of social interaction, social communication, and restricted and repetitive behaviour. ADOS is viewed as a gold standard diagnostic method used for the evaluation of ASD symptoms and is recommended in international guidelines and research (Lord et al., 2018; Ozonoff et al., 2005; Vllasaliu et al., 2016). The version used in this study was ADOS-Generic (ADOS-G; Lord et al., 2000, 2009) which is based on ASD diagnoses in both DSM-IV and ICD-10 (Lord et al., 2000). There are differences in the algorithm that is used, especially in Module 3. ADOS-2 uses a total score where the subscales Social communication and Stereotyped behaviours, and restricted interests are added together (Lord et al., 2014; Appendix). ADOS-G has no total score, only the subscales Communication + Reciprocal social interaction, and Stereotyped behaviours, and restricted interests (Lord et al., 2000, 2009; Appendix). We focus our analyses on item level, and the analysed items are those that are used in both ADOS-G and ADOS-2 in order to make our study relevant now when ADOS-2 is mainly used. ADOS-G has excellent interrater reliability (ICC = 0.92), internal consistency (Cronbach’s alpha = 0.91-0.94), and test-retest reliability (ICC = 0.82) when it comes to specifying between ASD and non-ASD in social communication total index (Lord et al., 2000). The interrater reliability is 74.5% when ADOS-G is performed by trained clinicians that are not expert assessors, and the clinical sample also includes individuals with co-occurring ASD and ADHD as well as individuals with the DSM-IV diagnosis Pervasive Developmental Disorder (PDD NOS) used for mild symptoms (Zander et al., 2016). Interrater reliability is lower when restricted and repetitive behaviours are assessed (Lord et al., 2000; Zander et al., 2014, 2016).
ADOS-G consists of four modules (Modules 1–4), one of which is administered based on the assessed expressive language and chronological or developmental age. Module 3 consists of 28 items, and Module 4 of 31 items. These items are grouped in domains: Communication, Reciprocal Social Interaction, Imagination, Stereotyped Behaviours and Restricted Interests, Other Abnormal Behaviours. The assessor rates 0–2, where 0 means that nothing deviates from expected behaviour and 2 means that the behaviour deviates clearly. The assessment is based on an algorithm with the items that are the most diagnostically informative (Lord et al., 2000; Zander et al., 2016). In the current study, we included participants who were administered Module 3 or 4 designed for children and adolescents with fluent speech. Due to the fact that the participants included in the original studies had a prior clinical and multidisciplinary assessment, the majority of participants were assessed with ADOS-G, but some of the participants were assessed with the newer version, ADOS-2 (Lord et al., 2014). In those cases, the algorithm was converted to ADOS-G. The total index scores for Communication + Reciprocal Social Interaction, and Stereotyped Behaviours, and Restricted Interests were used to analyse group differences. The algorithms in ADOS include different sets of items in different modules and versions. There are 12 items that were used in Modules 3 and 4 in both ADOS-G and ADOS-2 (Appendix). These items were also analysed in order to study more detailed differences between the two groups.
Data analysis
The demographic data and group comparisons were analysed using the χ2-test and Student’s t-test. Group differences in ADOS (total index score of Communication + Reciprocal Social Interaction; Stereotyped Behaviours and Restricted Interest, and 12 selected items from the algorithm) were analysed using the non-parametric test Kruskal-Wallis test for pairwise comparisons. All analyses were done using two-tailed probabilities (α = 0.05). The test statistic was adjusted for ties and the multiple comparisons test was not performed because the comparison groups numbered less than three (Perneger, 1998).
Effect size for t-test was calculated by using Hedges’s g analysis, by using the group means divided with the pooled standard deviation.
All analysis was performed with IBM SPSS Statistics 27.0.0.0.
Results
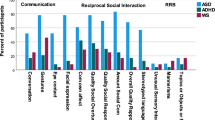
There were no significant differences between the groups in total scores for Communication + Reciprocal Social Interaction, H(1) = 0.57, p = .45, nor for Stereotyped Behaviours and Restricted Interest, H(1) = 0.01, p = .91. In contrast, a significant difference between groups was found for item Descriptive, Conventional, Instrumental or Informational Gestures, H(1) = 6.54, p = .01, indicating that the ASD + ADHD group used descriptive gestures to communicate to a greater extent than the ASD group (Table 2).
As the item Descriptive, conventional, instrumental or informative gestures in ADOS showed significant group differences, H(1) = 6.54, p = .01, we also analysed the item Empathic or Emotional Gestures. In addition to Descriptive, Conventional, Instrumental or Informative Gestures the item Empathic or Emotional Gestures is the only item that assesses gestures. This item occurs only in Module 4. Module 4 was used on 61 participants. The ASD group (n = 27, M = 1.30, SD = 0.61) and the ASD + ADHD group (n = 34, M = 0.82, SD = 0.80) had an average difference of 0.47, 95% CI [0.10, 0.84]. A t-test analysis showed that this difference was significant t(59) = 2.55, p = .01, with an effect size of g = 0.66.
Discussion
The aim of this study was to investigate whether there are autism symptom differences between children and adolescents with ASD and ASD + ADHD as operationalized by ADOS. No significant differences were found between the groups regarding the scores for Communication + Reciprocal Social Interaction or Stereotyped Behaviours and Restricted Interests in ADOS. The results indicate that children and adolescents with ASD and ASD + ADHD have similar qualitative difficulties with social communication and restricted and repetitive behaviours. In search of areas that could shed light on the behavioural phenotype of individuals with co-occurrent ASD and ADHD, we also chose to study ADOS on the item level. Interestingly, we found significant results in item Descriptive, Conventional, Instrumental or Informational Gestures, suggesting that the rater coded that children and adolescents with ASD + ADHD more often used descriptive gestures spontaneously together with other kinds of gestures (such as nodding, pointing, shaking the head or shrugging the shoulders). ADOS contains only one other item related to gestures: Emphatic or Emotional Gestures in Module 4. When we analysed this item, we found a significant difference between the groups, indicating that the ASD + ADHD group used empathic or emotional gestures more adequately than the ASD group. Despite observed possible differences in the use of gestures in our study, it is unclear whether the difference between ASD + ADHD and ASD applies to frequency, quality, or both. The main focus in the observation of gestures in ADOS is on spontaneous occurrence or frequency, but some attention is paid to the quality and timing (Lord et al., 2009). While individuals with ADHD are characterised as rarely being still (APA, 2013), those with ASD have been linked to motoric passivity (Leary & Hill, 1996; Wing & Gould, 1979). According to de Marchena and Eigsti (2010), children with ASD make fewer emphatic gestures (beats) than typically developed children. Otherwise, they make as many gestures as typically developed children, but their gestures are not as well synchronised with co-occurring speech. The item Descriptive, Conventional, Instrumental or Informational Gestures in ADOS intends to measure whether descriptive gestures are made spontaneously (Lord et al., 2009). Both Descriptive, Conventional, Instrumental or Informational Gestures and Emphatic or Emotional Gestures include assessment of both quality and frequency (Lord et al., 2009).
Two previous studies (Harkins et al., 2022; Ng et al., 2019) had similar results with no significant differences between the ASD group and the ASD + ADHD group on social communication in ADOS-2, while Salley et al. (2015) found significant differences in the total score for Communication + Reciprocal Social Interaction in ADOS-G between ASD and ASD + ADHD groups. Adolescents with ASD showed greater difficulties with communication and social interaction than adolescents with ASD and ADHD. Additionally, Ng et al. (2019) found no significant difference on Stereotyped Behaviours and Restricted Interests between ASD and ASD + ADHD. Both Salley et al. (2015) and Ng et al. (2019) included smaller sample sizes included in their analyses focusing on the difference between ASD and ASD + ADHD groups than in our study. Harkins et al. (2022) use groups where their smallest group is comparable to our two groups. In their study, there were significant differences between the ASD and the ASD + ADHD group in general intelligence and age, where the ASD group was younger and had lower general intelligence. Our sample size (n = 112: ASD = 56, ASD + ADHD = 56) is based on matched groups from a larger sample of N = 255 in order to minimise confounding factors (age, gender and general intelligence) and to define the differences between the groups related to social interaction.
In previous studies, most group differences between ADHD and ASD were larger than the group differences between ASD + ADHD and ASD (Harkins et al., 2022; Ng et al., 2019; Salley et al., 2015). This refers to, e.g., intelligence, executive functions and social communication. Since the ASD + ADHD group will have symptoms both from ASD and ADHD, it is likely that this group differs less from both the ADHD group and the ASD group than what ASD differs from ADHD.
Individuals with ADHD that are hyperactive and impulsive could be assumed to show an increased frequency of communication attempts during the ADOS observation. Since successful social interactions involve others and their reactions, it is precarious to only measure the Amount of Reciprocal Social Communication as in ADOS-G. The frequency of social initiatives does not require others to maintain the interaction in the same way as conversations do and could theoretically be linked to impulsivity. ADOS-2 has added the item Amount of Social Overtures/Maintenance of Attention but is not included in the algorithm that is the base for diagnostics in ADOS-2 (Lord et al., 2014). In combined ADHD, the lack of inhibition leads to more associative and divergent thought processes (Boot, Nevicka & Baas, 2017; Ten et al., 2020; White & Shah, 2016), which can result in both hyperactive talking and the tendency to interrupt others (APA, 2013). These traits could possibly affect this new item, Amount of Social Overtures/Maintenance of Attention (Lord et al., 2014).
Some limitations of the current study should be considered. Firstly, the participants were assessed and diagnosed by a multidisciplinary team in clinical settings, and the opportunity for assessment of inter-rater agreement or consensus scoring of ADOS was therefore not included. Secondly, there is a risk of selection bias because the fact that the participants were selected from another treatment effect study focusing on social skills training (Choque Olsson et al., 2017; Jonsson et al., 2019). The participants were recruited from mental health services, where it is routine to admit children and adolescents with co-occurring psychiatric symptoms and other neurodevelopmental conditions such as ADHD, but not those with no co-occurring conditions. Thirdly, the participants’ co-occurring psychiatric conditions were evaluated when they were recruited for the trials, but there was no information about whether the co-occurring condition already existed when the neuropsychiatric evaluation and ADOS observation were performed. Still, it is not possible to rule out the influence of co-occurring anxiety and depression, and it could be a confounder. On the other hand, the differences between the groups were few, implying that co-occurring conditions did not have a large impact on our results. According to prior studies, depression (Lai et al., 2017; Sterling et al., 2008) and anxiety (Livingston et al., 2019) in ASD are associated with compensatory social behaviour and consequently lower scores on ADOS (Lai et al., 2017; Livingston et al., 2019; Sterling et al., 2008). In addition, it has been suggested that autistic individuals with higher cognitive abilities and better social skills may be more aware of their social difficulties and their differences from peers and hence are more prone to depression (Sterling et al., 2008). Since our participants have chosen to participate in social skills training and are likely interested in social interaction and accept group treatment, they might fit this earlier mentioned group that are eager to fit in and are aware of their shortcomings. If this is the case, the difference between ASD and ASD + ADHD on gestures might be larger in a group without co-occurring psychiatric disorders. Fourthly, our study has an exploratory approach with many comparisons due to the lack of prior research, this increased the risk of making a Type I error. To avoid this, we could have chosen to set the significance level at 0.01 instead. In turn, this would have increased the risk of making a Type II error. Since the points on every item in the ADOS algorithm range from 0 to 2 the possible range of the mean is limited, which also would increase the risk of Type II errors. However, the coincidence that the two only items in the ADOS assessing gestures would be significant by chance would likely have a low probability. Our results need to be taken with caution and be replicated with a larger sample and with less skewed distribution on co-occurring conditions.
The co-occurrence of ADHD is a factor that complicates diagnostic assessment of ASD (Zander et al., 2016). Many characteristics of ASD and ADHD seem contradictory, especially in the combined form of ADHD. Difficulties with social reciprocity and developing and maintaining relationships (APA, 2013) get a different quality when they are paired with, for instance, hyperactive talking (APA, 2013) and extraversion (Knouse et al., 2013; Martel et al., 2010). Low social attention in ASD can be caused by unusually high interest in limited areas (Bölte et al., 2018), and this might make it harder to notice further inattention caused by ADHD. Impulsivity (APA, 2013) and novelty seeking (Anckarsäter et al., 2006) in ADHD is contrasted to the repetitive behaviour and adherence to routines in ASD (APA, 2013). When these traits are mixed, they might seem both less impulsive and less rigid, but they could possibly still cause considerable difficulties with everyday life in some areas. The obscuring trait of “impulsivity” might not reach the diagnostic threshold but would nonetheless make the autistic rigidity less obvious. Stereotyped or repetitive motor movements are more challenging to detect when they are mixed with fidgeting and hyperactive movements (APA, 2013). Both ASD (Van Den Huntjens et al., 2020) and ADHD (Petrovic & Castellanos, 2016) can cause emotional dysregulation, and together they are likely to combine the emotional volatility from ADHD (Petrovic & Castellanos, 2016) with associated difficulty in processing emotions (Milosavljevic et al., 2016) and the tendency to misunderstand social contexts common in ASD (Schall & McDonough, 2010). This enhances the risk of developing self-harming and suicidal ideation (Van Den Huntjens et al., 2020; Petrovic, & Castellanos, 2016) and can resemble borderline personality disorder and become misdiagnosed. Since the accuracy of diagnostic measures could be affected by the training and experience of the assessor in difficult diagnostic decisions (Charman & Gotham, 2013), it is essential to know how ASD appears in the presence of ADHD.
Children with ASD + ADHD are diagnosed later than those with only ASD. The delay appears to be due to ASD symptoms raising parental concern later (Stevens et al., 2016) and ASD being discovered later once they have sought psychological and/or psychiatric care (Kentrou et al., 2019; Stevens et al., 2016). To detect these children earlier, increased awareness of the signs of ASD + ADHD is required. The sensitivity of the diagnostic measures seems to be influenced by whether the parents rating their child’s symptoms are specifically concerned about ASD or if they have a more general concern (Havdahl et al., 2017). Existing instruments mainly measure the quality of social interaction and not, for example, the frequency of initiatives that could, to a greater extent, be linked to impulsivity and might be a better measure of differences between the groups. The relationship between the frequency and quality of social initiatives could be an area of development for measuring instruments. Taking many social initiatives can be advantageous but can also potentially make the difficulties with social interaction less obvious and possibly delay diagnosis. The analysis of the included ADOS items from the algorithm indicated a difference in the use of gestures between the groups. The presence of spontaneous gestures in the ASD + ADHD group (e.g., livelier body language) could conceal the presence of ASD and possibly delay the ASD diagnosis. Knowledge of the presence of spontaneous gestures in the ASD + ADHD group would be useful for detecting ASD earlier in children and adolescents with ASD + ADHD. From a clinical perspective, it is problematic if parents and children with co-occurring ASD and ADHD don’t recognize that their difficulties derive from those diagnoses. As a result, it becomes difficult for them to accept the diagnosis and the help offered. Psychoeducational treatment is then also not perceived as relevant. Psychoeducational programs improve social interaction in ASD (DaWalt et al., 2018) and emotional and social functioning in ADHD (Ferrin et al., 2014). Parents improve their ability to differentiate their children’s symptoms from other non-adaptive behaviours (Ferrin et al., 2014). They learn to problem solve and to further necessary adaptation of their children’s environment (DaWalt et al., 2018). Adolescents get an improved awareness of their strengths and difficulties (Gordon et al., 2015). This becomes difficult if the child or the parent does not accept the diagnoses because they or the youth do not recognise their difficulties in the description they are presented with. Consequently, more knowledge is needed about the features of the behavioural phenotype for individuals with ASD + ADHD.
Conclusion
We conclude that children and adolescents with ASD + ADHD have similar qualitative difficulties with social communication and restricted and repetitive behaviours to those with ASD. Our findings may indicate some differences between the groups in the use of gestures. This needs to be further studied specifically addressing the impact of the frequency of social initiatives in social interaction. Such information may be important in the earlier detection of individuals with ASD + ADHD as well as offering them better tailored psychoeducation.
Data availability
The data used for the current study are available from the corresponding author on reasonable request.
References
American Psychiatric Association (2000). Diagnostic and Statistical Manual of Mental Disorders (4th ed., text rev.)
American Psychiatric Association (2013). Diagnostic and Statistical Manual of Mental Disorders: DSM-5. (1st ed.).
Antshel, K. M., & Russo, N. (2019). Autism spectrum disorders and ADHD: Overlapping phenomenology, diagnostic issues, and treatment considerations. Current Psychiatry Reports, 21(5). https://doi.org/10.1007/s11920-019-1020-5
Anckarsäter, H., Stahlberg, O., Larson, T., Hakansson, C., Jutblad, S. B., Niklasson, L., Nydén, A., Wentz, E., Westergren, S., Cloninger, C. R., Gillberg, C., & Rastam, M. (2006). The impact of ADHD and autism spectrum disorders on temperament, character, and personality development. American Journal of Psychiatry, 163(7), 1239–1244. https://doi.org/10.1176/ajp.2006.163.7.1239
Boot, Nevicka, B., & Baas, M. (2017). Subclinical symptoms of attention-deficit/hyperactivity disorder (ADHD) are associated with specific creative processes. Personality and Individual Differences, 114, 73–81. https://doi.org/10.1016/j.paid.2017.03.050
Bölte, S., Poustka, L., & Geurts, H. (2018). Cooccurringity: Autism Spectrum Disorder. In T. Banaschewski, D. Coghill, & A. Zuddas (Eds.), Oxford Textbook of attention deficit hyperactivity disorder (pp. 227–234). University Press.
Charman, T., & Gotham, C. (2013). Measurement issues: Screening and diagnostic instruments for autism spectrum disorders - lessons from research and practise. Child and Adolescent Mental Health, 18(1), 52–64. https://doi.org/10.1111/j.1475-3588.2012.00664.x
Choque Olsson, N., Engström, A. C., Malm, E., Malmberg, K., Hedfors Moretti, Å., Nigam, I., Marsk, E., Borell, N., Larsson, J. O., Bölte, S., & Kadesjö, B. (2010). Autismspektrumtillstånd. I Barn och ungdomspsykiatrin, Stockholms läns landsting. Riktlinjer till stöd för bedömning och behandling [ASD Spectrum Disorder. In Child and Adolescent Psychiatry, Stockholm Region. Guidelines for evaluation and treatment]. Stockholms läns landsting.
Choque Olsson, N., Engström, A. C., Malm, E., Malmberg, K., Hedfors Moretti, Å., Nigam, I., Marsk, E., Borell, N., Larsson, J. O., Bölte, S., & Kadesjö, B. (2012). Autismspektrumtillstånd. I Barn och ungdomspsykiatrin, Stockholms läns landsting. Riktlinjer till stöd för bedömning och behandling 2012 [ASD Spectrum Disorder. In Child and Adolescent Psychiatry, Stockholm Region. Guidelines for evaluation and treatment 2012]. Stockholms läns landsting.
Choque Olsson, N., Flygare, O., Coco, C., Görling, A., Råde, A., Chen, Q., Lindstedt, K., Berggren, S., Serlachius, E., Jonsson, U., Tammimies, K., Kjellin, L., & Bölte, S. (2017). Social skills training for children and adolescents with autism spectrum disorder: A randomized controlled trial. Journal of the American Academy of Child & Adolescent Psychiatry, 56(7), 585–592. https://doi.org/10.1016/j.jaac.2017.05.001
DaWalt, L. S., Greenberg, J. S., & Mailick, M. R. (2018). Transitioning together: A multi-family group psychoeducation program for adolescents with ASD and their parents. Journal of Autism and Developmental Disorders, 48(1), 251–263. https://doi.org/10.1007/s10803-017-3307-x
de Marchena, A., & Eigsti, I. M. (2010). Conversational gestures in autism spectrum disorders: Asynchrony but not decreased frequency. Autism Research, 3(6), 311–322. https://doi.org/10.1002/aur.159
Ferrin, M., Moreno-Granados, J. M., Salcedo-Marin, M. D., Ruiz-Veguilla, M., Perez-Ayala, V., & Taylor, E. (2014). Evaluation of a psychoeducation programme for parents of children and adolescents with ADHD: Immediate and long-term effects using a blind randomized controlled trial. European Child & Adolescent Psychiatry, 23(8), 637–647. https://doi.org/10.1007/s00787-013-0494-7
Gargaro, B. A., Rinehart, N. J., Bradshaw, J. L., Tonge, B. J., & Sheppard, D. M. (2011). Autism and ADHD: How far have we come in the cooccurringity debate? Neuroscience and Biobehavioral Reviews, 35(5), 1081–1088. https://doi.org/10.1016/j.neubiorev.2010.11.002
Gordon, K., Murin, M., Baykaner, O., Roughan, L., Livermore-Hardy, V., Skuse, D., & Mandy, W. (2015). A randomised controlled trial of PEGASUS, a psychoeducational programme for young people with high-functioning autism spectrum disorder. Journal of Child Psychology and Psychiatry, 56(4), 468–476. https://doi.org/10.1111/jcpp.12304
Harkins, C. M., Handen, B. L., & Mazurek, M. O. (2022). The impact of the comorbidity of ASD and ADHD on social impairment. Journal of Autism and Developmental Disorders, 52(6), 2512–2522. https://doi.org/10.1007/s10803-021-05150-1
Havdahl, K. A., Bishop, S. L., Surén, P., Øyen, A. S., Lord, C., Pickles, A., von Tetzchner, S., Schjølberg, S., Gunnes, N., Hornig, M., Lipkin, W. I., Susser, E., Bresnahan, M., Magnus, P., Stenberg, N., Reichborn-Kjennerud, T., & Stoltenberg, C. (2017). The influence of parental concern on the utility of autism diagnostic instruments. Autism Research, 10(10), 1672–1686. https://doi.org/10.1002/aur.1817
Hull, L., Petrides, K. V., & Mandy, W. (2021). Cognitive predictors of self-reported camouflaging in autistic adolescents. Autism Research, 14(3), 523–532. https://doi.org/10.1002/aur.2407
Hus, V., & Lord, C. (2014). The autism diagnostic observation schedule, module 4: Revised algorithm and standardized severity scores. Journal of Autism and Developmental Disorders, 44(8), 1996–2012. https://doi.org/10.1007/s10803-014-2080-3
Jonsson, U., Olsson, N. C., Coco, C., Görling, A., Flygare, O., Råde, A., Chen, Q., Berggren, S., Tammimies, K., & Bölte, S. (2019). Long-term social skills group training for children and adolescents with autism spectrum disorder: A randomized controlled trial. European Child and Adolescent Psychiatry, 28(2), 189–201. https://doi.org/10.1007/s00787-018-1161-9
Kaufman, K., Birmaher, B., Brent, D., Rao, U., Flynn, C., Moreci, P., Williamson, D., & Ryamn, N. (1997). Schedule for affective disorders and schizophrenia for school-age children-present and lifetime version (K-SADS-PL): Initial reliability and validity data. Journal of the American Academy of Child and Adolescent Psychiatry, 36(7), 980–988. https://doi.org/10.1097/00004583-199707000-00021
Kentrou, V., de Veld, D. M. J., Mataw, K. J. K., & Begeer, S. (2019). Delayed autism spectrum disorder recognition in children and adolescents previously diagnosed with attention-deficit/hyperactivity disorder. Autism, 23(4), 1065–1072. https://doi.org/10.1177/1362361318785171
Knouse, L. E., Traeger, L., O’Cleirigh, C., & Safren, S. A. (2013). Adult attention deficit hyperactivity disorder symptoms and five-factor model traits in a clinical sample: A structural equation modeling approach. The Journal of nervous and mental disease, 201(10), 848–854. https://doi.org/10.1097/NMD.0b013e3182a5bf33e
Lai, M. C., Lombardo, M. V., Ruigrok, A. N. V., Chakrabarti, B., Auyeung, B., Szatmari, P., Happé, F., & Baron-Cohen, S. (2017). Quantifying and exploring camouflaging in men and women with autism. Autism, 21(6), 690–702. https://doi.org/10.1177/1362361316671012
Leary, M. R., & Hill, D. A. (1996). Moving on: Autism and movement disturbance. Mental Retardation, 34(1), 39–53.
Livingston, L. A., Colvert, E., Bolton, P., & Happé, F. (2019). Good social skills despite poor theory of mind: exploring compensation in autism spectrum disorder. Journal of Child Psychology and Psychiatry, and Allied Disciplines, 60(1), 102–110. https://doi.org/10.1111/jcpp.12886
Lord, C., Elsabbagh, M., Baird, G., & Veenstra-Vanderweele, J. (2018). Autism spectrum disorder. The Lancet, 392(10146), 508–520. https://doi.org/10.1016/S0140-6736(18)31129-2
Lord, C., Risi, S., Lambrecht, L., Cook Jr, E., Leventhal, B., DiLavore, P., Pickles, A., & Rutter, M. (2000). The Autism diagnostic observation schedule-generic: A standard measure of social and communication deficits associated with the spectrum of autism. Journal of Autism and Developmental Disorders, 30(3), 205–223. https://doi.org/10.1023/A:1005592401947
Lord, C., Rutter, M., Di Lavore, P., & Risi, S. (2009). Autism diagnostic observation schedule. ADOS. Manual (6th ed). Western Psychological Services. (Original work published 1999).
Lord, C., Rutter, M., Di Lavore, P., & Bishop, S. (2014). ADOS-2. Autism diagnostic observation schedule. Second edition. Manual (Part 1). Swedish Version Hoegrefe.
Lugo-Marín, Magán-Maganto, M., Rivero-Santana, A., Cuellar-Pompa, L., Alviani, M., Jenaro-Rio, C., Díez, E., & Canal-Bedia, R. (2019). Prevalence of psychiatric disorders in adults with autism spectrum disorder: A systematic review and meta-analysis. Research in Autism Spectrum Disorders, 59, 22–33. https://doi.org/10.1016/j.rasd.2018.12.004
Mansour, R., Dovi, A. T., Lane, D. M., Loveland, K. A., & Pearson, D. A. (2017). ADHD severity as it relates to comorbid psychiatric symptomatology in children with autism spectrum disorders (ASD). Research in Developmental Disabilities, 60, 52–64. https://doi.org/10.1016/j.ridd.2016.11.009
Martel, M. M., Goth-Owens, T., Martinez-Torteya, C., & Nigg, J. T. (2010). A person-centered personality approach to heterogeneity in Attention-Deficit/Hyperactivity disorder (ADHD). Journal of Abnormal Psychology, 119(1), 186–196. https://doi.org/10.1037/a0017511
Milosavljevic, B., Leno, C., Simonoff, V., Baird, E., Pickles, G., Jones, A., Erskine, C. R. G., Charman, C., & Happé, F. (2016). Alexithymia in adolescents with autism spectrum disorder: Its relationship to internalising difficulties, sensory modulation and social cognition. Journal of Autism and Developmental Disorders, 46(4), 1354–1367. https://doi.org/10.1007/s10803-015-2670-8
Ng, R., Heinrich, K., & Hodges, E. K. (2019). Brief report: Neuropsychological testing and informant-ratings of children with autism spectrum disorder, attention-deficit/hyperactivity disorder, or cooccurring diagnosis. Journal of Autism and Developmental Disorders, 49(6), 2589–2596. https://doi.org/10.1007/s10803-019-03986-2
Ozonoff, S., Goodlin-Jones, B., & Solomon, M. (2005). Evidence-based assessment of autism spectrum disorders in children and adolescents. Journal of Clinical Child and Adolescent Psychology, 34(3), 523–540. https://doi.org/10.1207/s15374424jccp3403_8
Petrovic, & Castellanos, F. X. (2016). Top-down dysregulation-from ADHD to emotional instability. Frontiers in Behavioral Neuroscience, 10, 70–70. https://doi.org/10.3389/fnbeh.2016.00070
Perneger. (1998). What’s wrong with Bonferroni adjustments. BMJ, 316(7139), 1236–1238. https://doi.org/10.1136/bmj.316.7139.1236
Rong, Y., Yang, C. J., Jin, Y., & Wang, Y. (2021). Prevalence of attention-deficit/hyperactivity disorder in individuals with autism spectrum disorder: A meta-analysis. Research in Autism Spectrum Disorders, 83, 101759. https://doi.org/10.1016/j.rasd.2021.101759
Salley, B., Gabrielli, J., Smith, C. M., & Braun, M. (2015). Do communication and social interaction skills differ across youth diagnosed with autism spectrum disorder, attention-deficit/hyperactivity disorder, or dual diagnosis? Research in Autism Spectrum Disorders, 20, 58–66. https://doi.org/10.1016/j.rasd.2015.08.006
Schall, C. M., & McDonough, J. T. (2010). Autism spectrum disorders in adolescence and early adulthood: Characteristics and issues. Journal of Vocational Rehabilitation, 32(2), 81–88. https://doi.org/10.3233/JVR-2010-0503
Sinzig, J., Morsch, D., & Lehmkuhl, G. (2008). Do hyperactivity, impulsivity and inattention have an impact on the ability of facial affect recognition in children with autism and ADHD? European Child and Adolescent Psychiatry, 17(2), 63–72. https://doi.org/10.1007/s00787-007-0637-9
Sterling, L., Dawson, G., Estes, A., & Greenson, J. (2008). Characteristics associated with presence of depressive symptoms in adults with autism spectrum disorder. Journal of Autism and Developmental Disorders, 38(6), 1011–1018. https://doi.org/10.1007/s10803-007-0477-y
Stevens, T., Peng, L., & Barnard-Brak, L. (2016). The comorbidity of ADHD in children diagnosed with autism spectrum disorder. Research in Autism Spectrum Disorders, 31, 11–18. https://doi.org/10.1016/j.rasd.2016.07.003
Ten, W., Tseng, C. C., Chiang, Y. S., Wu, C. L., & Chen, H. C. (2020). Creativity in children with ADHD: Effects of medication and comparisons with normal peers. Psychiatry Research, 284, 112680–112680. https://doi.org/10.1016/j.psychres.2019.112680
Tye, C., Asherson, P., Ashwood, K. L., Azadi, B., Bolton, P., & McLoughlin, G. (2014). Attention and inhibition in children with ASD, ADHD and co-morbid ASD + ADHD: An event-related potential study. Psychological Medicine, 44(5), 1101–1116. https://doi.org/10.1017/S0033291713001049
Unterrainer, J. M., Rauh, R., Rahm, B., Hardt, J., Kaller, C. P., Klein, C., Paschke-Müller, M., & Biscaldi, M. (2016). Development of planning in children with high-functioning Autism Spectrum Disorders and/or attention Deficit/Hyperactivity disorder. Autism Research, 9(7), 739–751. https://doi.org/10.1002/aur.1574
Van Den Huntjens, L. M. C. W., Sizoo, B., Kerkhof, A., Huibers, M. J., & Van Der Gaag, M. (2020). The effect of dialectical behaviour therapy in autism spectrum patients with suicidality and/or self-destructive behaviour (DIASS): Study protocol for a multicentre randomised controlled trial. BMC Psychiatry, 20(1), 1–11. https://doi.org/10.1186/s12888-020-02531-1
Vllasaliu, L., Jensen, K., Hoss, S., Landenberger, M., Menze, M., Schütz, M., Ufniarz, K., Kieser, M., & Freitag, C. (2016). Diagnostic instruments for autism spectrum disorder (ASD). Cochrane Library. https://doi.org/10.1002/14651858.CD012036
Wechsler, D. (1991). The Wechsler Intelligence Scale for Children. Third Edition. Psychological Corporation.
Wechsler, D. (2004). The Wechsler intelligence scale for children, fourth edition. Pearson Assessment.
White, H. A., & Shah, P. (2016). Scope of semantic activation and innovative thinking in college students with ADHD. Creativity Research Journal, 28(3), 275–282. https://doi.org/10.1080/10400419.2016.1195655
Wing, L., & Gould, J. (1979). Severe impairments of social interaction and associated abnormalities in children: Epidemiology and classification. Journal of Autism and Developmental Disorders, 9(1), 11–29. https://doi.org/10.1007/BF01531288
World Health Organization (2016). International statistical classification of diseases and related health problems (10th ed.). https://icd.who.int/browse10/2016/en
World Health Organization (2019). 6A02 Autism spectrum disorder. In ICD-11 for Mortality and Morbidity Statistics (ICD-11 MMS) https://icd.who.int/browse11/l-m/en#/http://id.who.int/icd/entity/437815624
Zander, E., Willfors, C., Bejerot, S., & Bölte, S. (2014). Utvecklingen av ADOS-2 och psykometriska studier. Del 1. Lord, C., Rutter, M., Di Lavore, P., & Bishop, S. L (2014). ADOS-2. Autism diagnostic observation schedule (2nd Edition, Manual Swedish version, pp. 155–181). Hoegrefe.
Zander, E., Willfors, C., Berggren, S., Choque-Olsson, N., Coco, C., Elmund, A., Moretti, Å, Holm, H., Jifält, A., Kosieradzki, I., Linder, R., Nordin, J., Olafsdottir, V., Poltrago, K., & Bölte, L. (2016). The objectivity of the autism diagnostic observation schedule (ADOS) in naturalistic clinical settings. European Child & Adolescent Psychiatry, 25(7), 769–780. https://doi.org/10.1007/s00787-015-0793-2
Acknowledgements
We thank the children, adolescents, and parents who participated in the study. Oskar Flygare, MSc, Anders Görling MSc, Christina Coco MSc, Steve Berggren, PhD. and Kerstin Andersson MSc are acknowledged for their work in collecting the data and samples during the RCT. The authors are also thankful to the leads of child and adolescent psychiatry (Olav Bengtsson, MD, Paula Liljeberg, MD, Charlotta Wiberg Spangenberg, MSc, Peter Ericson, MSc, Karin Forler, MSc, Alkisti Nikolayidis Linderholm, MSc, all of Stockholm County Council), PRIMA Järva child and adolescent psychiatry (MaiBritt Giacobini, MD, PhD), and child and adolescent habilitation services (Lars Kjellin, PhD, Moa Pellrud, MSc, of Örebro County Council) for organizational support; The Foundation Sunnerdahls Disability, Majblomman, Stockholm County Council, and the Pediatric Research Foundation at Astrid Lindgren Children’s Hospital; The Swedish Research Council, in partnership with the Swedish Research Council for Health, Working Life and Welfare, Formas and VINNOVA (cross-disciplinary research program concerning children’s and young people’s mental health, 259-2012-24, Dr. Bölte) Stockholm County Council (20130314 Dr. Bölte).
Funding
Open access funding provided by Stockholm University.
Author information
Authors and Affiliations
Contributions
V.J.P., N.C.O. and L.H. designed the study; N.C.O. and S.B. conceived the original clinical trial; V.J.P performed the analysis with supervision from N.C.O. and L.H.; M. J-F., A.F. and S.B. provided overall suggestion and discussion for the analyses; V.J.P., N.C.O. and L.H. wrote the paper with input from all authors. All authors approved the final version of the article.
Corresponding author
Ethics declarations
Informed consent
Informed consent was obtained from all individual participants included in the study.
Ethical approval
Approval for all study procedures was obtained from the local ethics committee in Stockholm, Sweden.
Conflict of interest
S.B. is an author of the German and Swedish KONTAKT manuals and receives royalties. N.C.O. is one of the co-authors of the Swedish KONTAKT manuals, but has no financial interest to disclose. The other authors have no relevant financial or non-financial interest or potential conflicts of interest.
Additional information
Publisher’s note
Springer Nature remains neutral with regard to jurisdictional claims in published maps and institutional affiliations.
Appendix Overview of the algorithms and indexes of different ADOS versions and modules
Appendix Overview of the algorithms and indexes of different ADOS versions and modules
ADOS G- algorithms | ADOS 2 - algorithms | ||||
|---|---|---|---|---|---|
Subscales in ADOS-G | Module 3- items | Module 4- items | Subscales in ADOS 2 | Module 3- items | Module 4a- items |
Communication | Stereotyped/idiosyncratic use of words or phrases Reporting of events Conversation Descriptive, conventional, instrumental or informational gestures | Stereotyped/idiosyncratic use of words or phrases Conversation Descriptive, conventional, instrumental or informational gestures Empathic or emotional gestures | Social communication, total | Reporting of events Conversation Descriptive, conventional, instrumental or informational gestures Unusual eye contact Facial expressions directed to others Shared enjoyment in interaction Quality of social overtures Quality of social response Amount of reciprocal social communication Overall quality of report | Conversation Empathic or emotional gestures Unusual eye contact Facial expressions directed to others Communication of own affect Empathy/Comments on others emotions Quality of social overtures Quality of social response Amount of reciprocal social communication Overall quality of report |
Total (cut-off, ASD: 2) | Total (cut-off, ASD: 2) | ||||
Reciprocal social interaction | Unusual eye contact Facial expressions directed to others Insights Responsibility Quality of social overtures Quality of social response Amount of reciprocal social communication Overall quality of report | Unusual eye contact Facial expressions directed to others Empathy/Comments on others emotions Responsibility Quality of social overtures Quality of social response Amount of reciprocal social communication | |||
Total (cut-off, ASD: 4) | Total (cut-off, ASD: 4) | ||||
Communication + reciprocal social interaction, total | Total (cut-off, ASD: 7) | Total (cut-off, ASD: 7) | |||
Imagination/Creativity | Imagination/Creativity | Imagination/Creativity | - | - | - |
Stereotyped behaviors and restricted interest | Unusual sensory interest in play material/person Hand and finger and other complex mannerism Unusually repetitive interests or stereotyped behavior Compulsions or rituals | Unusual sensory interest in play material/person Hand and finger and other complex mannerism Unusually repetitive interests or stereotyped behavior Compulsions or rituals | Stereotyped behaviors and restricted interest, total | Stereotyped/idiosyncratic use of words or phrases Unusual sensory interest in play material/person Hand and finger and other complex mannerism Unusually repetitive interests or stereotyped behavior | Stereotyped/idiosyncratic use of words or phrases Unusual sensory interest in play material/person Hand and finger and other complex mannerism Unusually repetitive interests or stereotyped behavior |
Total sum is not used | Total sum is not used | Social communication + Stereotyped behaviors and restricted interest, total | Total (cut-off ASD: 7) | Total (cut-off ASD: 8) | |
Rights and permissions
Open Access This article is licensed under a Creative Commons Attribution 4.0 International License, which permits use, sharing, adaptation, distribution and reproduction in any medium or format, as long as you give appropriate credit to the original author(s) and the source, provide a link to the Creative Commons licence, and indicate if changes were made. The images or other third party material in this article are included in the article's Creative Commons licence, unless indicated otherwise in a credit line to the material. If material is not included in the article's Creative Commons licence and your intended use is not permitted by statutory regulation or exceeds the permitted use, you will need to obtain permission directly from the copyright holder. To view a copy of this licence, visit http://creativecommons.org/licenses/by/4.0/.
About this article
Cite this article
Piltz, V.J., Halldner, L., Markus, JF. et al. Symptom similarities and differences in social interaction between autistic children and adolescents with and without ADHD. Curr Psychol 43, 3503–3513 (2024). https://doi.org/10.1007/s12144-023-04499-z
Accepted:
Published:
Issue Date:
DOI: https://doi.org/10.1007/s12144-023-04499-z