Abstract
There is increasing need to identify factors that contribute to poor work ability with an aim to prevent work related problems such as sick leave and disability pension. In the Metacognitive Control System model, dysfunctional metacognitive beliefs are seen as an underlying factor in psychological vulnerability beyond disorder, and recent studies have reported that metacognitions are associated with work ability and work status. In the present study, we set out to test if there is a prospective relationship between dysfunctional metacognitions and self-assessed work ability. Individuals in working age (M = 37.19; SD = 10.31) participated in a four-timepoint self-report survey (N = 528; 75% females) separated by six weeks between each timepoint. Baseline gender differences and differences between participants by job status were conducted using t-test and one-way ANOVA, respectively. Latent growth curve with covariates assessed the impact of dysfunctional metacognitions on work ability across the four timepoints. Males reported higher work ability. Participants in fulltime job also reported higher work ability followed by those in part-time job, jobseekers, sick leave up to 12 months, and sick leave > 12 months, respectively. Dysfunctional metacognitions predicted work ability over time when controlling for gender, age, physical health status, and three common categories of emotional distress symptoms. This finding suggest that dysfunctional metacognitions are a prospective predictor of work ability beyond health status and implies that these beliefs should be targeted with a view to increasing work ability and thus potentially reduce risk for sick leave and other work-related problems.
Similar content being viewed by others
Avoid common mistakes on your manuscript.
Introduction
Work ability is the balance between human resources and work demands and is related, but not equivalent to health status. Work ability reflects workers’ own judgement of their state of health in relation to job demands (Ilmarinen et al., 1991). There is research evidence that dysfunctional metacognitions (e.g., about the controllability and effectiveness of cognition) is correlated with self-reported work ability (Nordahl & Wells, 2019a, b, 2020). However, no longitudinal studies have examined the relationship between dysfunctional metacognitions and work ability. Longitudinal studies which show how dysfunctional metacognitions and work ability are temporarily related can overcome severe design issues in cross-sectional studies and can contribute information for targeted interventions to preserve good work ability or improve poor work ability. In response, this study investigates the relationship between dysfunctional metacognition and work ability over four timepoints. Given the obvious gaps in this area of research, this study seems fully warranted.
Work ability predicts risk of disability pension, welfare benefits, sickness absence, work participation, and income from regular employment (Bethge et al., 2018; Lundin et al., 2017; Notenbomer et al., 2015; Reeuwijk et al., 2015; Roelen et al., 2014). Furthermore, it is a prospective predictor of return to work (RTW) for example in employees with common mental disorders (Nigatu et al., 2017), cancer survivors (Wolvers et al., 2018), those on sick leave for long-term neck/shoulder and/or back pain (Rashid et al., 2021), and has been suggested as a common factor underlying RTW after common mental disorders and common physical illnesses (Gragnano et al., 2018). Work ability is also a significant predictor of early retirement from the labour market (Sell, 2009). Thus, work ability is important not only for workers themselves as being employed is associated with better quality of life and mental health (Carlier et al., 2013; Curnock et al., 2016), but also for employers because of demands put on them related to absenteeism such as economic costs and loss of competent/experienced workers (Nagata et al., 2018).
Work ability can be assessed using self-report assessment tools such as the Work Ability Index (WAI; Ilmarinen et al., 1991; Tuomi et al., 1997). The WAI assesses seven components intended to form a single dimension of work ability. Several studies (e.g., Kinnunen & Nätti, 2018; Leijon et al., 2017; Lindberg et al., 2009; Lundin et al., 2017) have shown support for using a single item from the WAI with comparable predictive validity to the whole scale. This is the first item of the scale and is referred to as the Work Ability Scale (WAS). The WAS assess individuals’ own evaluation of their work ability compared with lifetime best on a single scale ranging from 0 (“completely unable to work”) to 10 (“present work ability at its best”).
As subjective judgements of work ability indicated by the WAS is related to short- and long-term absence from work, there is a need to identify factors that contribute to work ability with a view to increase occupational functioning and facilitate return to work. Work ability can be affected by a number of factors including health status, cognitive abilities, social and behavioural functioning, workplace factors, and factors outside the workplace (Fadyl et al., 2010). In addition, psychological factors such as sense of control also seem to be associated with work ability (McGonagle et al., 2015). Psychological factors underlying work ability that is amenable to change is of particular interest as they may be targeted in interventions with the aim to preserve good- or improve poor work ability. According to the Metacognitive Control System Model (MCS; Wells, 2019) which is an extension of the Self-Regulatory Executive Function (S-REF) model (Wells & Matthews, 1994), metacognitive knowledge (e.g., beliefs about cognition) is central to psychological disorder but also to psychological vulnerability and self-regulation in general. Dysfunctional metacognitive beliefs (e.g., “Worrying is uncontrollable”, or “I have a poor memory”) give rise to a maladaptive cognitive style called the Cognitive Attentional Syndrome (CAS; Wells, 2009) consisting of perseverative negative thinking, maladaptive coping strategies, and strategic attention towards perceived threats. The CAS and its underlying metacognitions cause ineffective mental management strategies which are unable to reduce distress or improve performance confidence. Thus, dysfunctional metacognitions may contribute to poorer work ability by undermining the expectation of mastery and ability to cope with job demands.
In a recent cross-sectional study, Nordahl and Wells (2019a) reported a positive correlation between dysfunctional metacognitions and self-reported work ability and showed that metacognitive beliefs in the form of judgements of memory confidence accounted for independent variance in work ability even when controlling for the effects of physical health status and emotional distress symptoms in individuals with a diagnosed common mental disorder. Other studies have indicated that dysfunctional metacognitive beliefs correlate with work status (Nordahl & Wells, 2019b, 2020) and that, dysfunctional metacognitions are prospective predictors of return-to-work (RTW) in patients with chronic pain, chronic fatigue, and emotional disorders (Jacobsen et al., 2020). There is also evidence suggesting that Metacognitive therapy (Wells, 2009), which aims to modify dysfunctional metacognitive knowledge is associated with RTW in patients with Major Depressive Disorder (Solem et al., 2019). It is therefore possible that metacognitive change underlie change in work ability and RTW. However, the relation between dysfunctional metacognitive beliefs and subjective judgements of work ability has not previously been investigated in longitudinal data.
Following from the studies above, the aim of the present study was to test the effect of metacognitions on work ability consistent with a causal role of metacognitions to self-assessed work ability using latent growth curve modelling (LGCM). To provide a more stringent test of the unique contribution of dysfunctional metacognitions, we controlled for the effects of several covariates relevant to work ability. For age and gender, previous studies show that older participants and females report lower work ability (Kooij et al., 2008; Stansfeld & Candy, 2006). In addition, the effect of physical health was taken into account since it has a direct impact on work ability and predicts sickness absence (Lundin et al., 2017). Emotional distress symptoms (generalised anxiety-, social anxiety-, and depression symptoms) were included as covariates because they have been routinely used as markers of psychopathology associated with lower work ability (Leijon et al., 2017), and to control for the expected overlap between dysfunctional metacognitions and psychopathology symptoms (Wells, 2009). In line with the metacognitive perspective (Wells, 2009), we hypthesised that dysfunctional metacognition will predict work ability over and above all relevant covariates included.
Method
Procedure and participants
Data for this study was collected using “Select Survey” provided by the Norwegian University of Science and Technology. Participants were invited through advertisement on various social media platforms and assisted by several Norwegian voluntary organizations for mental health. Participants that were required had to be 18 years or older and to be able to read Norwegian language. Participants responded to the survey at four different time points separated by six weeks between each measurement occasion. The research was conducted in accordance with the Declaration of Helsinki and was approved by the Norwegian Regional Committee for Medical and Health Research Ethics (REC; reference: REK-Midt, 2016/705). A total of 868 participants responded to the survey. Participants who were students (n = 299; 81% females) or retired (n = 37; 41% females) were removed prior to the analyses, leaving five hundred and twenty-eight eligible participants (N = 528; 75% females) with a mean age of 37.19 (SD = 10.31) years in timepoint one (T1). Four hundred and thirteen participated in T2, 330 in T3, and 293 in T4. Regarding work status, 312 (59.1%) reported to be in a fulltime job, 55 (10.4%) reported to be working part-time, 25 (4.7%) reported to be jobseekers, 26 (4.9%) reported to be on sick leave for up to twelve months, and 110 (20.8%) reported to be on long term sick leave (more than 12 months) or on disability pension. Four participants did not report their job status and were excluded from further analyses.
Measures
The single item Work Ability Scale (WAS) of the Work Ability Index (WAI; Ilmarinen et al., 1991; Tuomi et al., 1991, 1997) was used. The WAS assesses participants self-reported present work ability compared to their lifetime best was used as the dependent variable in the current study. The WAS is measured on an 11-point Likert-type scale from 0 (cannot currently work at all) to 10 (work ability at its best) and thus reflect individual judgements of present work ability. The WAS item is “Assume that your work ability at its best has a value of 10 points. How many points would you give your current work ability?” For assessing physical health status, we used Scale 3 of the WAI which measures the number of current diseases diagnosed by a physician.
The Generalized Anxiety Disorder Questionnaire (GAD-7; Spitzer et al., 2006) scale is a seven item self-report measure that assesses anxiety related symptoms. All items (e.g., Being so restless that it is hard to sit still) are answered using a 4-point Likert scale with higher scores indicating more anxiety symptoms. In the current study the internal consistency at baseline was α = 0.91.
Liebowitz Social Anxiety Scale (LSAS; Fresco et al., 2001; Liebowitz, 1987) is a 24-item self-report scale assessing social anxiety severity where the respondent is asked to rate the degree of fear and avoidance in 24 different social situations during the past week. Each item (e.g., Going to a party) is rated on a 4-point scale, indicating degree of fear from 0 (none) to 3 (severe) and avoidance, from 0 (never) to 3 (usually) separately. In the current study the internal consistency at baseline was α = 0.98.
The Patient Health Questionnaire (PHQ-9; Kroenke et al., 2001) is a nine item self-report measure that assesses the frequency of depressive symptoms. All items (e.g., Feeling down, depressed, or hopeless) are answered using a 4-point Likert scale with higher scores indicating more depressive symptoms. In the current study the internal consistency at baseline was α = 0.93.
The Metacognitions Questionnaire-30 (MCQ-30; Wells & Cartwright-Hatton, 2004)) is a measure of dysfunctional metacognitive beliefs. Each item (e.g., “Worrying helps me to avoid problems in the future”) is assessed in a scale from 1 (Do not agree) to 4 (Agree very much), and a higher total score indicate higher levels of dysfunctional metacognitive beliefs. In the current study the internal consistency for the total score at baseline was α = 0.93.
Data analyses
Preliminary analyses at baseline to examine gender differences and difference between participants by job status were conducted using t-test and one-way analyses of variance, respectively. A well-fitting latent growth curve model (LGCM) was used to determine the overall trajectory of work ability over time. Since scores were nonnormally distributed (Mardia’s multivariate skewness = 141.25, p < 0.001; Mardia’s multivariate kurtosis = 16.39, p < 0.001), the full information maximum likelihood estimation with robust standard errors in Mplus 8.6 was used (Muthén & Muthén, 1998–2021). Specifically, the LGCM was used to examine the overall initial status and the rate of change of work ability through two latent variables, intercept and slope. Known baseline time-invariant covariates (e.g., age, gender, physical health status, generalised- and social anxiety symptoms, and depression symptoms) and the time varying effect of metacognitions were used to determine predictors of the growth factors and variation in work ability over time. Growth factors and known baseline time-invariant covariates represent level 2 effects (or between person variations) while the exogenous time-varying effect of metacognitive beliefs represent level 1 effects (or time level variations). The following fit indices determined adequate fit: Standardized Root Mean Square Residual (SRMSR < 0.08), Root Mean Square Error of Approximation (RMSEA ≤ 0.06) (Browne & Cudeck, 1993) Comparative Fit Index (CFI ≥ 0.90) and a non-Normed Fit index (NNFI; aka TLI ≥ 0.90) (Hu & Bentler, 1999).
Results
Preliminary results
Table 1 displays descriptive statistics and correlations for all variables in the study. An independent samples t-test analysis at baseline showed that males reported higher work ability (Mean difference, MD = 0.89, BCa 95% CI 0.272, 1.514, t(234) = 2.834, p < 0.01, d = 0.288). Similarly, significant baseline differences F (4, 414) = 138.38, p < 0.001, partial η2 = 0.57, were found such that, participants in fulltime job reported higher work ability than participants in the following job statuses: part-time job (MD = 1.68, BCa 95% CI 0.660, 2.700, p < 0.001), jobseekers (MD = 1.97, BCa 95% CI 0.500, 3.450, p < 0.01), (MD = 1.68, BCa 95% CI 0.660, 2.700, p < 0.001), individuals on sick leave up to twelve months (MD = 4.89, BCa 95% CI 3.480, 6.300, p < 0.001), and those on longer sick leave/disability pension (MD = 5.79, BCa 95% CI 4.980, 6.590, p < 0.001). Participants in part-time job reported higher work ability than individuals on sick leave up to twelve months (MD = 3.21, BCa 95% CI 1.560, 4.860, p < 0.001) and than those on longer sick leave/disability pension (MD = 4.11, BCa 95% CI 2.940, 5.280, p < 0.001). Jobseekers reported higher work ability than those on sick leave up to twelve months (MD = 2.92, BCa 95% CI 0.960, 4.880, p < 0.001) and than those on longer sick leave/disability pension (MD = 3.82, BCa 95% CI 2.240, 5.400, p < 0.001). There were no significant differences in work ability between individuals reporting to be on sick leave up to twelve months and those on longer term sick leave/disability pension (MD = 0.89, BCa 95% CI -0.620, 2.42, p = 0.504) as well as between part-time workers and jobseekers (MD = 0.29, BCa 95% CI -1.410, 1.990, p = 0.550).
Latent growth curve modelling (LGCM)
Unconditional LGCM
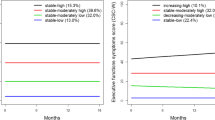
The model to data correspondence for the linear growth model showed adequate fit (χ2 = 13.533, df = 5; p < 0.05; SRMR = 0.016; RMSEA = 0.060, [90% CI = 0.023, 0.100]; CFI = 0.980; TLI = 0.975). The average intercept or initial status was significant (I = 5.840, p < 0.001), and the slope was stable over time (S = 0.030, p = 0.473). The variance of the intercept growth factor was significant (8.262, p < 0.001), but not the slope growth factor (0.146, p = 0.066), which indicated that, although there were significant individual differences in the initial levels of work ability, the rate of change in work ability over time was stable and identical for all the participants. The covariance between the intercept and slope growth factors was also not significant (-0.263, p = 0.081). The R2 values (i.e., explained variance) in work ability ranged between 79.50% to 83.00% in the unconditional LGCM model.
Conditional LGCM with time-invariant and time-varying covariates
The model with the baseline time-invariant covariates (LGCM-TIC) showed an adequate fit to the data (χ2 = 37.584, df = 17; p < 0.01; SRMR = 0.025; RMSEA = 0.054, [90% CI = 0.030, 0.077]; CFI = 0.977; TLI = 0.960), as was the model with the time-varying effect of metacognitive beliefs included (LGCM-TIC and TVC) (χ2 = 46.428, df = 21; p < 0.01; SRMR = 0.014; RMSEA = 0.048, [90% CI = 0.029, 0.067]; CFI = 0.976; TLI = 0.947). To account for the short time intervals between measurement points, equality constraints were imposed on the effect of metacognitive beliefs on work ability. The resulting test did not show significant worsening in model fit (χ2 = 4.407, df = 3; p = 0.221), as such it was retained as the final model with the following fit indices (χ2 = 50.471, df = 24; p < 0.01; SRMR = 0.013; RMSEA = 0.046, [90% CI = 0.028, 0.063]; CFI = 0.975; TLI = 0.952). Parameter estimates for both LGCM – TIC and LGCM – TIC and TVC models are shown in Table 2. Figure 1 shows the final LGCM – TIC and TVC model. The average intercept (I = 10.518, p < 0.001) and the variance of the intercept (4.040, p < 0.001) were all significant. The rate of change showed a stable trajectory over time (S = 0.362, p = 0.096), whereas the variance showed significant difference (0.166, p < 0.05), indicating significant inter-individual differences in the initial status and rate of change as a function of the covariates.
The explained variance in work ability (at Time 1 = 85.6%; Time 2 = 81.4%; Time 3 = 79.00%; Time 4 = 85.80%) indicate that the variation in work ability is well explained by the growth factors and metacognitive beliefs. Controlling for the time-varying effect of metacognitive beliefs, the time-invariant covariates explained (R2 = 42.10%, p < 0.001) in the intercept growth factor, but the explained variance in the slope was not significant (R2 = 15.20%, p = 0.085). High number of physical disorders/injuries/illnesses, depression symptoms and social anxiety symptoms all predicted low level of work ability. Gender (i.e., female) negatively predicted the rate of change in work ability over time. Interestingly, higher metacognitive beliefs longitudinally predicted significant lower work ability whiles controlling for the known covariates.
Discussion
The primary aim of this study was to test the prospective relationship between dysfunctional metacognitions and self-assessed work ability over four timepoints separated by six weeks between each measurement occasion while controlling for the effects of gender, age, number of diagnosed physical disorders, illnesses or injuries, and emotional distress in the form of generalized- and social anxiety symptoms, and depression symptoms.
In exploring basic correlations between the variables at T1, we found that gender was significantly correlated with work ability (females reported poorer work ability), while age did not significantly correlate with work ability. Number of physical disorders diagnosed by a physician and domains of emotional distress symptoms (generalized anxiety, social anxiety, and depression symptoms) significantly and negatively correlated with work ability. Furthermore, higher levels of dysfunctional metacognitions significantly and negatively correlated with work ability. These results are in line with our hypothesis and previous research as outlined in the introduction with the exception that age did not significantly correlate with work ability. This finding may be explained by the relatively young age of the participants in the present study.
When controlling for the overlap between the predictors, number of physical diagnoses, social anxiety- and depression symptoms accounted for individual variance in the intercept growth factor. Gender was the only significant predictor of the slope growth factor among the covariates. However, dysfunctional metacognitions had a significant and consistent effect on work ability over time when controlling for the effects of the covariates. These results indicate that dysfunctional metacognitions have a prospective effect on work ability even when controlling for gender, age, number of physical disorders, and emotional distress symptoms, and that higher levels of dysfunctional metacognitions is associated with poorer work ability.
To the authors’ knowledge, this is the first study testing and indicating that metacognitions are prospective predictors of work ability. This finding fits well with the MCS model (Wells, 2019) which emphasize metacognitive knowledge and the regulation of cognition as central to psychological functioning and self-regulation in general. It suggests dysfunctional metacognitions cause mental management strategies that are ineffective in reducing distress and in enhancing confidence in performance. The effect from metacognition does not appear to be an artefact of the association between anxiety- and depression symptoms and dysfunctional metacognition (e.g., Sun et al., 2017) as we were able to control for emotional distress symptoms and also number of physical diagnosed disorders in our analyses. Thus, there seem to be a role for metacognitions to work ability beyond more objective indicators such as health status. This finding is in line with a previous cross-sectional study that reported an association between metacognitions and work ability beyond physical health status and emotional distress symptoms (Nordahl & Wells, 2019b), but our findings add to this study by demonstrating a prospective effect from metacognitions to work ability. Furthermore, our modeling approach incorporates a within-person effect of metacognitions, such that its effect alters an individual’s work ability change trajectory.
These results add to previous studies that have indicated an association between dysfunctional metacognitions and work status. Dysfunctional metacognitions are associated with work status when controlling for the presence of a mental disorder and trait-anxiety (Nordahl & Wells, 2019a) above distress severity and cognitive-behavioral factors in socially anxious individuals (Nordahl & Wells, 2020). Furthermore, one study reported that metacognitions prospectively predicted return to work among individuals with chronic pain, fatigue, and common mental disorders (Jacobsen et al., 2020). It is possible that metacognitive change underlie change in perceived work ability and thus impacts on return to work independent from physical- and emotional disorders and distress.
The implication of our finding is that targeting and modifying dysfunctional metacognitions can impact on perceived work ability and therefore reduce the risk for negative consequences of poor work ability such as short- and long-term sickness absence, and early retirement. Metacognitive therapy (Wells, 2009) was specifically designed to modify metacognitive knowledge and to improve self-regulation, and is a highly effective treatment for emotional disorders (Normann & Morina, 2018). In addition, some studies indicate that MCT has a positive effect on work ability and return to work (De Dominicis et al., 2021; Solem et al., 2019), but this should be more specifically evaluated. According to the MCS model (Wells, 2019), dysfunctional metacognitions are transdiagnostic factors and underlie a range of difficulties related to psychological functioning. We may therefore speculate that targeting dysfunctional metacognitions can have a broad impact on occupational functioning as these beliefs cause both emotional distress symptoms and subjective judgement of poor work ability beyond health status.
There are several limitations that must be acknowledged. Convenience sampling was used, so there is relatively little control over who participated in the study. Further, the sample consisted of substantially more females and the mean age of the sample indicated that there were many relatively young participants which might compromise the generalizability of our findings. All the data relied on self-report, and the WAI Scale 3 was used to assess physical health status which may be unreliable. Moreover, we had no control over physical illness severity which may be more important to work ability than the presence of a diagnosis. Further research should take these limitations into account and include more specific information about health status. Furthermore, further studies should investigate the relation between metacognition and work ability in different populations (e.g., different disorders) and under different levels of workplace factors such as type and demands of work (e.g., high versus low responsibility).
Conclusion
Our findings suggest that dysfunctional metacognitions cause poorer work ability over time, even when controlling for the effect of physical health problems and common types of emotional distress symptoms. The implication of this finding is that modifying dysfunctional metacognitions may have a positive effect on work ability and thus create resilience among workers as their ability to deal with occupational stress and demands will increase or contribute to return to work among those out of work. Metacognitive therapy may be particularly effective in this context as it specifically aims to modify dysfunctional metacognitions.
Data availability
The data and materials, including codes will be made available by the authors without undue reservation to any qualified researcher.
References
Bethge, M., Spanier, K., Peters, E., Michel, E., & Radoschewski, M. (2018). Self-reported work ability predicts rehabilitation measures, disability pensions, other welfare benefits, and work participation: Longitudinal findings from a sample of German employees. Journal of Occupational Rehabilitation, 28(3), 495–503. https://doi.org/10.1007/s10926-017-9733-y
Browne, M. W., & Cudeck, R. (1993). Alternative ways of assessing model fit. In K. A. Bollen & J. S. Long (Eds.), Testing structural equation models (pp. 136–162). Sage.
Carlier, B. E., Schuring, M., Lötters, F. J., Bakker, B., Borgers, N., & Burdorf, A. (2013). The influence of re-employment on quality of life and self-rated health, a longitudinal study among unemployed persons in the Netherlands. BMC Public Health, 13(1), 1–7. https://doi.org/10.1186/1471-2458-13-503
Curnock, E., Leyland, A. H., & Popham, F. (2016). The impact on health of employment and welfare transitions for those receiving out-of-work disability benefits in the UK. Social Science & Medicine, 162, 1–10. https://doi.org/10.1016/j.socscimed.2016.05.042
De Dominicis, S., Troen, M. L., & Callesen, P. (2021). Metacognitive Therapy for work-related stress: A feasibility study. Frontiers in Psychiatry, 12, 668245. https://doi.org/10.3389/2Ffpsyt.2021.668245
Fadyl, J. K., McPherson, K. M., Schlüter, P. J., & Turner-Stokes, L. (2010). Factors contributing to work-ability for injured workers: Literature review and comparison with available measures. Disability and Rehabilitation, 32(14), 1173–1183. https://doi.org/10.3109/09638281003653302
Fresco, D., Coles, M., Heimberg, R. G., Liebowitz, M., Hami, S., Stein, M. B., & Goetz, D. (2001). The Liebowitz Social Anxiety Scale: A comparison of the psychometric properties of self-report and clinician-administered formats. Psychological Medicine, 31(6), 1025–1035. https://doi.org/10.1017/s0033291701004056
Gragnano, A., Negrini, A., Miglioretti, M., & Corbière, M. (2018). Common psychosocial factors predicting return to work after common mental disorders, cardiovascular diseases, and cancers: A review of reviews supporting a cross-disease approach. Journal of Occupational Rehabilitation, 28(2), 215–231. https://doi.org/10.1007/s10926-017-9714-1
Hu, L.-t, & Bentler, P. M. (1999). Cutoff criteria for fit indexes in covariance structure analysis: Conventional criteria versus new alternatives. Structural Equation Modeling: A Multidisciplinary Journal, 6(1), 1–55. https://doi.org/10.1080/10705519909540118
Ilmarinen, J., Tuomi, K., Eskelinen, L., Nygård, C.-H., Huuhtanen, P., & Klockars, M. (1991). Summary and recommendations of a project involving cross-sectional and follow-up studies on the aging worker in Finnish municipal occupations (1981—1985). Scandinavian Journal of Work, Environment & Health, 135–141.
Jacobsen, H. B., Glette, M., Hara, K. W., & Stiles, T. C. (2020). Metacognitive beliefs as predictors of return to work after intensive return-to-work rehabilitation in patients with chronic pain, chronic fatigue and common psychological disorders: Results from a prospective trial. Frontiers in Psychology, 11, 70. https://doi.org/10.3389/fpsyg.2020.00070
Kinnunen, U., & Nätti, J. (2018). Work ability score and future work ability as predictors of register-based disability pension and long-term sickness absence: A three-year follow-up study. Scandinavian Journal of Public Health, 46, 321–330. https://doi.org/10.1177/1403494817745190
Kooij, D., De Lange, A., Jansen, P., & Dikkers, J. (2008). Older workers’ motivation to continue to work: Five meanings of age: A conceptual review. Journal of Managerial Psychology, 23, 364–394. https://doi.org/10.1108/02683940810869015
Kroenke, K., Spitzer, R. L., & Williams, J. B. (2001). The PHQ-9: Validity of a brief depression severity measure. Journal of General Internal Medicine, 16, 606–613. https://doi.org/10.1046/j.1525-1497.2001.016009606.x
Leijon, O., Balliu, N., Lundin, A., Vaez, M., Kjellberg, K., & Hemmingsson, T. (2017). Effects of psychosocial work factors and psychological distress on self-assessed work ability: A 7-year follow-up in a general working population. American Journal of Industrial Medicine, 60, 121–130. https://doi.org/10.1002/ajim.22670
Liebowitz, M. R. (1987). Social phobia. Modern Problems in Pharmacopsychiatry, 22, 141–173.
Lindberg, P., Josephson, M., Alfredsson, L., & Vingård, E. (2009). Comparisons between five self-administered instruments predicting sick leaves in a 4-year follow-up. International Archives of Occupational and Environmental Health, 82, 227. https://doi.org/10.1007/s00420-008-0326-0
Lundin, A., Leijon, O., Vaez, M., Hallgren, M., & Torgén, M. (2017). Predictive validity of the Work Ability Index and its individual items in the general population. Scandinavian Journal of Public Health, 45, 350–356. https://doi.org/10.1177/1403494817702759
McGonagle, A. K., Fisher, G. G., Barnes-Farrell, J. L., & Grosch, J. W. (2015). Individual and work factors related to perceived work ability and labor force outcomes. Journal of Applied Psychology, 100(2), 376–398. https://psycnet.apa.org/doi/10.1037/a0037974.
Muthén, L. K., & Muthén, B. O. (1998 - 2021). Mplus: Statistical analysis with latent variables (Version 8.6). Los Angeles, CA.
Nagata, T., Mori, K., Ohtani, M., Nagata, M., Kajiki, S., Fujino, Y., ... & Loeppke, R. (2018). Total health-related costs due to absenteeism, presenteeism, and medical and pharmaceutical expenses in Japanese employers. Journal of Occupational and Environmental Medicine, 60(5), e273-e280. https://doi.org/10.1097/2FJOM.0000000000001291
Nigatu, Y. T., Liu, Y., Uppal, M., McKinney, S., Gillis, K., Rao, S., & Wang, J. (2017). Prognostic factors for return to work of employees with common mental disorders: A meta-analysis of cohort studies. Social Psychiatry and Psychiatric Epidemiology, 52(10), 1205–1215. https://doi.org/10.1007/s00127-017-1402-0
Nordahl, H., & Wells, A. (2019a). In or out of work: A preliminary investigation of mental health, trait anxiety and metacognitive beliefs as predictors of work status. Clinical Psychologist, 23(1), 79–84. https://doi.org/10.1111/cp.12153
Nordahl, H., & Wells, A. (2019b). Predictors of work ability in individuals with a common mental disorder: Is there an effect of metacognitive beliefs among poor physical health and emotional distress? Behaviour Change, 36(4), 252–262. https://doi.org/10.1017/bec.2019.15
Nordahl, H., & Wells, A. (2020). Social anxiety and work status: The role of negative metacognitive beliefs, symptom severity and cognitive-behavioural factors. Journal of Mental Health, 29(6), 1665–1669. https://doi.org/10.1080/09638237.2017.1340622
Normann, N., & Morina, N. (2018). The efficacy of metacognitive therapy: A systematic review and meta-analysis. Frontiers in Psychology, 9, 2211. https://doi.org/10.3389/fpsyg.2018.02211
Notenbomer, A., Groothoff, J. W., van Rhenen, W., & Roelen, C. A. M. (2015). Associations of work ability with frequent and long-term sickness absence. Occupational Medicine, 65, 373–379. https://doi.org/10.1093/occmed/kqv052
Rashid, M., Heiden, M., Nilsson, A., & Kristofferzon, M. L. (2021). Do work ability and life satisfaction matter for return to work? Predictive ability of the work ability index and life satisfaction questionnaire among women with long-term musculoskeletal pain. BMC Public Health, 21(1), 1–9. https://doi.org/10.1186/s12889-021-10510-8
Reeuwijk, K. G., Robroek, S. J., Niessen, M. A., Kraaijenhagen, R. A., Vergouwe, Y., & Burdorf, A. (2015). The prognostic value of the work ability index for sickness absence among office workers. PLoS ONE, 10(5), e0126969. https://doi.org/10.1371/journal.pone.0126969
Roelen, C. A., Heymans, M. W., Twisk, J. W., van der Klink, J. J., Groothoff, J. W., & van Rhenen, W. (2014). Work Ability Index as tool to identify workers at risk of premature work exit. Journal of Occupational Rehabilitation, 24, 747–754. https://doi.org/10.1007/s10926-014-9505-x
Sell, L. (2009). Predicting long-term sickness absence and early retirement pension from self-reported work ability. International Archives of Occupational and Environmental Health, 82(9), 1133–1138. https://doi.org/10.1007/s00420-009-0417-6
Solem, S., Kennair, L. E. O., Hagen, R., Havnen, A., Nordahl, H. M., Wells, A., & Hjemdal, O. (2019). Metacognitive therapy for depression: A 3-year follow-up study assessing recovery, relapse, work force participation, and quality of Life. Frontiers in Psychology, 10, 2908. https://doi.org/10.3389/fpsyg.2019.02908
Spitzer, R. L., Kroenke, K., Williams, J. B., & Löwe, B. (2006). A brief measure for assessing generalized anxiety disorder: The GAD-7. Archives of Internal Medicine, 166(10), 1092–1097. https://doi.org/10.1001/archinte.166.10.1092
Stansfeld, S., & Candy, B. (2006). Psychosocial work environment and mental health—a meta-analytic review. Scandinavian Journal of Work, Environment & Health, 443–462. http://www.jstor.org/stable/40967597
Sun, X., Zhu, C., & So, S. H. W. (2017). Dysfunctional metacognition across psychopathologies: A meta-analytic review. European Psychiatry, 45, 139–153. https://doi.org/10.1016/j.eurpsy.2017.05.029
Tuomi, K., Ilmarinen, J., Eskelinen, L., Järvinen, E., Toikkanen, J., & Klockars, M. (1991). Prevalence and incidence rates of diseases and work ability in different work categories of municipal occupations. Scandinavian Journal of Work, Environment & Health, 67-74. https://doi.org/10.1037/t58607-000
Tuomi, K., Ilmarinen, J., Seitsamo, J., Huuhtanen, P., Martikainen, R., Nygård, C.-H., & Klockars, M. (1997). Summary of the Finnish research project (1981—1992) to promote the health and work ability of aging workers. Scandinavian Journal of Work, Environment & Health, 66–71. https://www.jstor.org/stable/40966693
Wells, A. (2009). Metacognitive therapy for anxiety and depression. Guilford press.
Wells, A. (2019). Breaking the cybernetic code: Understanding and treating the human metacognitive control system to enhance mental health. Frontiers in Psychology, 10, 2621. https://doi.org/10.3389/fpsyg.2019.02621
Wells, A., & Cartwright-Hatton, S. (2004). A short form of the metacognitions questionnaire: Properties of the MCQ-30. Behaviour Research and Therapy, 42(4), 385–396. https://doi.org/10.1016/s0005-7967(03)00147-5
Wells, A., & Matthews, G. (1994). Attention and Emotion: A clinical perspective. Erlbaum.
Wolvers, M. D. J., Leensen, M. C. J., Groeneveld, I. F., Frings-Dresen, M. H. W., & De Boer, A. G. E. M. (2018). Predictors for earlier return to work of cancer patients. Journal of Cancer Survivorship, 12(2), 169–177. https://doi.org/10.1007/s11764-017-0655-7
Funding
Open access funding provided by NTNU Norwegian University of Science and Technology (incl St. Olavs Hospital - Trondheim University Hospital)
Author information
Authors and Affiliations
Contributions
FA and HN conceived the study and contributed equally to writing. FA led the analysis. OH provided guidance and comments on the manuscript.
Corresponding author
Ethics declarations
Conflicts of interest
All authors declare no conflict of interest.
Additional information
Publisher's note
Springer Nature remains neutral with regard to jurisdictional claims in published maps and institutional affiliations.
Rights and permissions
Open Access This article is licensed under a Creative Commons Attribution 4.0 International License, which permits use, sharing, adaptation, distribution and reproduction in any medium or format, as long as you give appropriate credit to the original author(s) and the source, provide a link to the Creative Commons licence, and indicate if changes were made. The images or other third party material in this article are included in the article's Creative Commons licence, unless indicated otherwise in a credit line to the material. If material is not included in the article's Creative Commons licence and your intended use is not permitted by statutory regulation or exceeds the permitted use, you will need to obtain permission directly from the copyright holder. To view a copy of this licence, visit http://creativecommons.org/licenses/by/4.0/.
About this article
Cite this article
Anyan, F., Hjemdal, O. & Nordahl, H. Testing the longitudinal effect of metacognitive beliefs on the trajectory of work ability. Curr Psychol 42, 28086–28094 (2023). https://doi.org/10.1007/s12144-022-03912-3
Accepted:
Published:
Issue Date:
DOI: https://doi.org/10.1007/s12144-022-03912-3