Abstract
Anorexia Nervosa (AN) is a psychological disorder involving body manipulation, self-inflicted hunger, and fear of gaining weight.We performed an overview of the existing literature in the field of AN, highlighting the main intrafamilial risk factors for anorexia. We searched the PubMed database by using keywords such as “anorexia” and “risk factors” and “family”. After appropriate selection, 16 scientific articles were identified. The main intrafamilial risk factors for AN identified include: increased family food intake, higher parental demands, emotional reactivity, sexual family taboos, low familial involvement, family discord, negative family history for Eating Disorders (ED), family history of psychiatric disorders, alcohol and drug abuse, having a sibling with AN, relational trauma. Some other risk factors identified relate to the mother: lack of maternal caresses, dysfunctional interaction during feeding (for IA), attachment insecurity, dependence. Further studies are needed, to identify better personalized intervention strategies for patients suffering from AN.
Highlights:
This systematic review aims at identifying the main intrafamilial risk factors for anorexia nervosa, including maternal ones.
Intrafamilial risk factors identified mostly regard family environment and relational issues, as well as family history of psychiatric diseases.
Family risk factors identified may interact with genetic, environmental, and personal risk factors.
These findings may help develop tailored diagnostic procedures and therapeutic interventions.
Similar content being viewed by others
Avoid common mistakes on your manuscript.
Introduction
Eating behavior encompasses all responses associated with the act of eating and is influenced by social conditions, individual perception, previous experiences, and nutritional status. Additional influencing factors include mass media and idealization of thinness. Anorexia nervosa (AN) is a psychological disorder concerning body manipulation, including fear of becoming fat and self-inflicted hunger. This disorder is interpreted as a response to the social context and a woman’s rejection of fat to deny mature sexuality (Gonçalves et al., 2013; Korb, 1994) and it was once supposed to have “hysterical” causes (Valente, 2016). The current definition of AN provided by the DSM-5 describes it as “a restriction of energy intake relative to requirements such as to lead to a significantly low body weight […]; intense fear of gaining weight or becoming fat, or persistence in behaviors that interfere with weight gain […]; alteration in the way weight or body shape are experienced […]” (Cuzzolaro, 2014). The lifetime prevalence of AN is estimated being of 1.4% (0.1–3.6%) in women and 0.2% (0-0.3%) in men (Galmiche et al., 2019). The lifetime prevalence rates of anorexia nervosa might be up to 4% among females and 0.3% among males (Van Eeden et al., 2021). AN finds its roots in biological, psychological, social, and familial risk factors.
More precisely, heritable risk factors for AN can be found in 48–74% of cases (Baker et al., 2017): for example, it has a higher prevalence in female relatives of individuals with AN (Bulik et al., 2019). The presence of genetic correlations between AN and metabolic and anthropometric traits may explain why people with AN achieve very low BMIs and may even maintain and relapse to low body weight despite clinical improvement (Bulik et al., 2019). On the other hand, psychological risk factors include excessive concerns about weight and figure, low self-esteem, and depression; while social risk factors are related to peer diet, peer criticism, and poor social support (Haynos et al., 2016). As far as family is concerned, it has been observed that anorexic girls’ families are often characterized by poor communication with one another, overprotection, conflicts, and hostility (Emanuelli et al., 2003; Horesh et al., 2015; Sim et al., 2009).
Overall, the puzzle of AN risk factors is still obscure and needs deeper investigations as far as some predisposing aspects are concerned, such as intrafamilial risk factors, which have been extensively analyzed but not properly clarified for clinical applications. Because of the multifactorial etiology of AN, intrafamilial risk factors identification can help to establish preventive interventions in at-risk individuals, and to provide tailored treatments from the earliest stages of the disorder. Our main hypothesis is that intrafamilial as well as maternal risk factors play an essential role in the development of the disease.
Therefore, the main objective of this work is to provide a scientific review of the existing literature about familial relational risk factors involved in the development of AN, with the aim of improving: prevention, establishment of an early diagnosis, and development of a tailored treatment.
Methodology
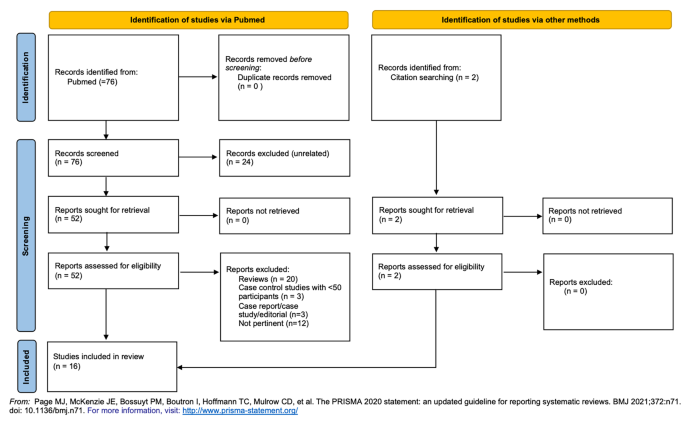
On February the 16th, 2022, a first research was conducted on PubMed with the title/abstract filter, using the terms “anorexia AND risk factors AND family” in the search bar. For eligibility, we included only randomized controlled studies and case-control studies focused on the issue, as well as case-control studies with at least 50 participants. We excluded reviews, single case studies, case reports, other types of articles and other studies that did not focus on the main topic. The system provided 76 articles, of which 24 were ignored for low relevance. Hence, 52 were assessed for eligibility, from which 26 articles were excluded for not respecting the inclusion criteria, and 12 were excluded for not analyzing the research subject specifically. To the remaining 14 articles, 2 were added from citation search.
In the PRISMA diagram below (Fig. 1), the articles identified for the review (76) are reported schematically: screened (76), assessed for eligibility (52) and included (16).
Results
The main results of the studies analyzed are summarized in Table 1.
Discussion
Despite anorexia having been usually considered an expression of age-specific conflicts intensified by constrictive cultural ideas and certain kinds of familial constellations (Bemporad et al., 1988), having our review included studies from 1990 to 2021 and conducted across many countries (i.e. US, Japan, Poland, UK, etc.) we can hypothesize that such a condition just evolves with culture and time, still maintaining certain background issues that we are aiming to emphasize in order to recognize certain red flags.
Eating disorders mark deficits in the ability to be nourished and to symbolize embodied experience. Psychoanalytic theories suggest that mothers who are insufficiently developed leave the child either austerely avoiding intrusion or struggling to digest maternal provisions without becoming lost in them. (Charles, 2021). Infantile Anorexia (IA) has been defined as a child’s refusal of food for more than 1 month, between 6 months and 3 years of age; acute and/or chronic malnutrition; parental concern about the child’s eating; mother-child conflict, talk, and distraction during mealtime (Chatoor et al., 1998). Maternal risk factors for (IA) we have identified across the review can confirm this widely accepted theory, specifically lack of maternal caresses (Mangweth et al., 2005), dysfunctional interaction during feeding in IA (Ammaniti et al., 2010), and attachment insecurity (Chatoor et al., 2000). Regarding maternal history of psychiatric diseases, it has been noted that maternal depression has an influence on the development of conflicts during mother-child interaction in younger children, while maternal psychoticism predicts mother-child conflict during feeding in older children (Ammaniti et al., 2010). This means that depressed mothers engage in less positive interactions with their infants while breastfeeding, with difficulties in empathically recognizing their infant’s affective states at mealtimes (Ammaniti, Ambruzzi et al., 2004; Feldman et al., 2004).
In addition to the relational risk factors, maternal diet seems to play a role in the development of AN (Haynos et al., 2016). This mechanism seems to find its roots early during childhood, since the infant’s weight appears to be inversely related to the mother’s degree of concern about her body shape (Ammaniti, Lucarelli et al., 2004). The “modelling theory of AN” (Pike & Rodin, 1991) argues that adolescent girls begin the diet by mimicking their dieting mothers. It seems that family concerns about weight and appearance are directly linked to the development of low satisfaction with one’s body, and therefore directly or indirectly related to eating problems (Leung et al., 1996).
Maternal risk factors are synthesized in Table 2.
Enlarging our highlight from the mother to the whole family nucleus, the onset and maintenance of AN seems to be closely related to familial risk factors, and knowing them is crucial to identify the best therapeutic approach in order to target the unhealthy family environment as well as the needs of the patient. In addition, being aware of the familiar background may help in strengthening the hypothesis of genetic correlates within Eating Disorders (ED). Intrafamilial risk factors for the development of ED seem to have a greater impact when they occur early in adolescence (Field et al., 2008), but most of them are chronic in time and one can suppose they can be found in a family at any time during the life of the patient.
The major intrafamilial risk factors identified in this review are summarized in the following Table 3.
Increased food intake in the family (Hilbert et al., 2014) seems to play a role in the development of ED. This seems counterintuitive, but the discrepancy between one’s family food intake and peer and media influences on body ideals may contribute to triggering a subtle mechanism by which diet represents a way to affirm oneself in front of the family and reestablish social acceptance.
Perfectionism (Hilbert et al., 2014; Pike et al., 2008, 2021) is widely recognized as a familiar risk factor across many studies, and it can be assimilated to higher parental demands (Pike et al., 2008). It surely contributes to creating a tense family environment in which the development of oneself is more difficult, therefore inhibiting progressive differentiation of self from other (Charles, 2021). Perfectionism itself will become a personal risk factor for the outcome and severity of disease (Longo, Aloi et al., 2021) in a way that could be mimicking the family environment.
In general, unhealthy family functioning is predictive of adolescence problems (Lyke & Matsen, 2013). General family malfunction is predictive for AD onset during adolescence, and the level of affective expression of the family seems to be relate to ED risk during adolescence (Felker & Stivers, 1994), but our review has highlighted that all those features of what could be described as a “toxic” family environment in the common sense play a role in the development of AN. Emotional reactivity (Lyke & Matsen, 2013), as well as family taboos regarding nudity and sexuality (Mangweth et al., 2005), low familial involvement (Haynos et al., 2016), negative affectivity (Pike et al., 2008, 2021), and family discord (Pike et al., 2008) may lie in the background in the lives of a future AN patient, and should be recognized as environmental risk factors in order to develop a tailored psychotherapeutic intervention that may involve the family as well as the patient, since it seems clear that the quality of family functioning influences the development (McGrane & Carr, 2002) and maintenance of EDs (North et al., 1997; Strober et al., 1997; Wewetzer et al., 1996).
As far as the presence of other disorders in family members is concerned, our review established that a familiar history of almost any psychiatric disorder (Longo, Marzola et al., 2021; Pike et al., 2021), including depression (Lyon et al., 1997), affective disorders (Steinhausen et al., 2015), alcohol and drug abuse (Lyon et al., 1997) plays a role in the development of AN. Nevertheless, having a sibling with AN increases the risk of developing AN (Machado et al., 2014; Steinhausen et al., 2015). We can hypothesize that the role of genetics in this mechanism is crucial yet still obscure, and nevertheless, talking about the presence of these diseases in members of the family nucleus, having to cope and live with the difficulties of others’ conditions is what can predispose to AN. In addition, the opposite may happen as well: there is an increased risk for relatives of patients with AN and BN to develop subclinical forms of ED, major depressive disorder, obsessive-compulsive disorder, and anxiety disorders (Lilenfeld et al., 1998). What is curious to note is that, on the one hand, having a sibling with AN predisposes to the development of AN (Felker & Stivers, 1994; Machado et al., 2014; Steinhausen et al., 2015), probably because of shared intrafamilial risk factors, therefore underlining the importance of the aim of this review; but, on the other hand, negative family history for ED predicts poor outcome (Ackard et al., 2014), probably because of the familiar unpreparedness to cope with such a difficult condition and the discrepancy created between the healthy members and the patient, which remains alone and uncapable of sharing certain issues with the others, so close yet so far from them.
Another risk factor identified is having suffered a relational trauma (Longo, Marzola et al., 2021). In general, individuals who have suffered from traumatic events (physical violence, being threatened with a weapon, sexual violence, being a victim of robbery) more frequently develop maladaptive eating behaviors (Field et al., 2008). Some evidence also suggests an increase of severe life events in the year preceding the onset of AN (Råstam & Gillberg, 1991). Children of mothers who have experienced the loss of a vital member of their family (i.e. older child or partner) in the six months prior to pregnancy have a higher risk of ED than children and infants who have not been exposed to this risk factor (Su et al., 2015). Further confirming the possible role of relational trauma as a red flag not only in the development of AN, but also in determining the severity of the disease, patients with AN and comorbid Post Traumatic Stress Disorder (PTSD) show more severe concerns about body shape and weight (Field et al., 2008). Having suffered physical and sexual abuse during childhood appears to be related to the onset of psychiatric pathologies in general, and not specifically to the onset of EDs in the young adult (Bruch, 1977; McGrane & Carr, 2002; Smith et al., 1995): therefore, this risk factor needs further investigation to confirm its specific role in the development of AN.
Strength and limits
The strength of this work lies in the comparison between different studies regarding AN showing high level of evidence and providing a complete picture of the constellation of intrafamilial risk factors of anorexia nervosa. There main limit of this study is that few articles from those included are from the very last years, while many other studies were conducted and published earlier (1990–2014), underlining the need of further investigations.
Conclusions
The main intrafamilial risk factors for AN identified from this study are: increased food intake in the family, perfectionism, higher parental demands, emotional reactivity, family taboos regarding nudity and sexuality, low familial involvement, negative affectivity, family discord, dependence, negative family history for ED (as a predictor of poor outcome), family history of depression, positive family history for psychiatric disorders, affective disorders in family members, alcohol and drug abuse, having a sibling with AN, relational trauma. Some other risk factors identified may relate to the role of the mother during childhood especially, and are as follows: lack of maternal caresses, dysfunctional interaction during feeding (for IA), attachment insecurity, dependence, maternal diet.
Complex interactions occur between intrafamilial risk factors and other personal aspects and symptoms, including perfectionism, individual body image issues, social concerns, excessive preoccupation with weight control, stress and adjustment problems, lack of close friends, social prejudice.
In conclusion, further studies are needed to understand more clearly how intrafamilial risk factors for AN interact with other environmental, personal and genetic ones, in order to connect the dots that can lead to an improvement of diagnostic and therapeutic procedures, and to the development of tailored intervention strategies that may target multiple issues in the life of the patient, including intrafamilial mechanisms that may be identified precociously and addressed through familial therapy, for the sake of the whole family nucleus.
Data availability
Data sharing is not applicable to this article as no datasets were generated or analyzed during the current study.
References
Ackard, D. M., Richter, S., Egan, A., & Cronemeyer, C. (2014). Poor outcome and death among youth, young adults, and midlife adults with eating disorders: An investigation of risk factors by age at assessment. International Journal of Eating Disorders, 47(7), 825–835. https://doi.org/10.1002/eat.22346
Ammaniti, M., Ambruzzi, A. M., Lucarelli, L., Cimino, S., & D’Olimpio, F. (2004). Malnutrition and dysfunctional mother-child feeding interactions: clinical assessment and research implications. Journal of the American College of Nutrition, 23(3), 259–271. https://doi.org/10.1080/07315724.2004.10719369
Ammaniti, M., Lucarelli, L., Cimino, S., & D’Olimpio, F. (2004). Transmission intergénérationnelle: troubles alimentaires de l’enfance et psychopathologie maternelle. Devenir, 16(3), 173. https://doi.org/10.3917/dev.043.0173
Ammaniti, M., Lucarelli, L., Cimino, S., D’Olimpio, F., & Chatoor, I. (2010). Maternal psychopathology and child risk factors in infantile anorexia. International Journal of Eating Disorders, 43(3), 233–240. https://doi.org/10.1002/eat.20688
Baker, J. H., Schaumberg, K., & Munn-Chernoff, M. A. (2017). Genetics of Anorexia Nervosa. Current Psychiatry Reports, 19(11), 84. https://doi.org/10.1007/s11920-017-0842-2
Bemporad, J. R., Ratey, J. J., O’Driscoll, G., & Daehler, M. L. (1988). Hysteria, Anorexia and the Culture of Self-Denial. Psychiatry (New York), 51(1), 96–103. https://doi.org/10.1521/00332747.1988.11024383
Bruch, H. (1977). Patologia del comportamento alimentare. Italian Tr). Feltrinelli.
Bulik, C. M., Flatt, R., Abbaspour, A., & Carroll, I. (2019). Reconceptualizing anorexia nervosa. Psychiatry and Clinical Neurosciences, 73(9), 518–525. https://doi.org/10.1111/pcn.12857
Charles, M. (2021). Meaning, metaphor, and metabolization: the case of eating disorders. American Journal of Psychoanalysis, 81(4), 444–466. https://doi.org/10.1057/s11231-021-09324-9
Chatoor, I., Hirsch, R., Ganiban, J., Persinger, M., & Hamburger, E. (1998). Diagnosing infantile anorexia: the observation of mother-infant interactions. Journal of the American Academy of Child and Adolescent Psychiatry, 37(9), 959–967. https://doi.org/10.1097/00004583-199809000-00016
Chatoor, I., Ganiban, J., Hirsch, R., Borman-Spurrell, E., & Mrazek, D. A. (2000). Maternal characteristics and toddler temperament in infantile anorexia. Journal of the American Academy of Child and Adolescent Psychiatry, 39(6), 743–751. https://doi.org/10.1097/00004583-200006000-00013
Cuzzolaro, M. (2014). Anoressie e bulimie. Il Mulino.
Emanuelli, F., Ostuzzi, R., Cuzzolaro, M., Watkins, B., Lask, B., & Waller, G. (2003). Family functioning in anorexia nervosa: British and Italian mothers’ perceptions. Eating Behaviors, 4(1), 27–39. https://doi.org/10.1016/s1471-0153(02)00097-1
Feldman, R., Keren, M., Gross-Rozval, O., & Tyano, S. (2004). Mother-Child touch patterns in infant feeding disorders: relation to maternal, child, and environmental factors. Journal of the American Academy of Child and Adolescent Psychiatry, 43(9), 1089–1097. https://doi.org/10.1097/01.chi.0000132810.98922.83
Felker, K. R., & Stivers, C. (1994). The relationship of gender and family environment to eating disorder risk in adolescents. Adolescence, 29(116), 821–834. http://www.ncbi.nlm.nih.gov/pubmed/7892793
Field, A. E., Javaras, K. M., Aneja, P., Kitos, N., Camargo, C. A., Taylor, C. B., & Laird, N. M. (2008). Family, peer, and media predictors of becoming eating disordered. Archives of Pediatrics & Adolescent Medicine, 162(6), 574–579. https://doi.org/10.1001/archpedi.162.6.574
Galmiche, M., Déchelotte, P., Lambert, G., & Tavolacci, M. P. (2019). Prevalence of eating disorders over the 2000–2018 period: A systematic literature review. American Journal of Clinical Nutrition, 109(5), 1402–1413. https://doi.org/10.1093/ajcn/nqy342
Gonçalves, J. A., Moreira, E. A. M., de Trindade, E. B. S. M., & Fiates, G. M. R. (2013). Eating disorders in childhood and adolescence.Revista Paulista de Pediatria: Orgao Oficial Da Sociedade de Pediatria de Sao Paulo, 31(1),96–103. https://doi.org/10.1590/s0103-05822013000100016
Haynos, A. F., Watts, A. W., Loth, K. A., Pearson, C. M., & Neumark-Stzainer, D. (2016). Factors Predicting an Escalation of Restrictive Eating During Adolescence. The Journal of Adolescent Health: Official Publication of the Society for Adolescent Medicine, 59(4), 391–396. https://doi.org/10.1016/j.jadohealth.2016.03.011
Hilbert, A., Pike, K. M., Goldschmidt, A. B., Wilfley, D. E., Fairburn, C. G., Dohm, F. A., Walsh, B. T., & Weissman, S., R (2014). Risk factors across the eating disorders. Psychiatry Research, 220(1–2), 500–506. https://doi.org/10.1016/j.psychres.2014.05.054
Horesh, N., Sommerfeld, E., Wolf, M., Zubery, E., & Zalsman, G. (2015). Father-daughter relationship and the severity of eating disorders. European Psychiatry: The Journal of the Association of European Psychiatrists, 30(1), 114–120. https://doi.org/10.1016/j.eurpsy.2014.04.004
Korb, M. (1994). Anorexia as Symbolic Expression of a Woman’s Rejection of Her Mother’s Life. Western Journal of Nursing Research, 16(1), 69–80. https://doi.org/10.1177/019394599401600106
Leung, F., Schwartzman, A., & Steiger, H. (1996). Testing a dual-process family model in understanding the development of eating pathology: a structural equation modeling analysis. The International Journal of Eating Disorders, 20(4), 367–375. https://doi.org/10.1002/(SICI)1098-108X(199612)20:4%3C367::AID-EAT4%3E3.0.CO;2-L
Lilenfeld, L. R., Kaye, W. H., Greeno, C. G., Merikangas, K. R., Plotnicov, K., Pollice, C., Rao, R., Strober, M., Bulik, C. M., & Nagy, L. (1998). A controlled family study of anorexia nervosa and bulimia nervosa: Psychiatric disorders in first-degree relatives and effects of proband comorbidity. Archives of General Psychiatry, 55(7), 603–610. https://doi.org/10.1001/archpsyc.55.7.603
Longo, P., Aloi, M., Delsedime, N., Rania, M., Garcia, S., Abbate-Daga, C., G., & Marzola, E. (2021). Different clusters of perfectionism in inpatients with anorexia nervosa and healthy controls. Eating Disorders. https://doi.org/10.1080/10640266.2021.1938937
Longo, P., Marzola, E., De Bacco, C., Demarchi, M., & Abbate-Daga, G. (2021). Young patients with anorexia nervosa: The contribution of post-traumatic stress disorder and traumatic events. Medicina (Lithuania), 57(1), 1–10. https://doi.org/10.3390/medicina57010002
Lyke, J., & Matsen, J. (2013). Family functioning and risk factors for disordered eating. Eating Behaviors, 14(4), 497–499. https://doi.org/10.1016/j.eatbeh.2013.08.009
Lyon, M., Chatoor, I., Atkins, D., Silber, T., Mosimann, J., & Gray, J. (1997). Testing the hypothesis of the multidimensional model of anorexia nervosa in adolescents. Adolescence, 32(125), 101–111.
Machado, B. C., Gonçalves, S. F., Martins, C., Hoek, H. W., & Machado, P. P. (2014). Risk factors and antecedent life events in the development of anorexia nervosa: A Portuguese case-control study. European Eating Disorders Review, 22(4), 243–251. https://doi.org/10.1002/erv.2286
Mangweth, B., Hausmann, A., Danzl, C., Walch, T., Rupp, C. I., Biebl, W., Hudson, J. I., & Pope, H. G. (2005). Childhood body-focused behaviors and social behaviors as risk factors of eating disorders. Psychotherapy and Psychosomatics, 74(4), 247–253. https://doi.org/10.1159/000085149
McGrane, D., & Carr, A. (2002). Young Women at Risk for Eating Disorders: Perceived Family Dysfunction and Parental Psychological Problems. Contemporary Family Therapy, 24, 385–395.
North, C., Gowers, S., & Byram, V. (1997). Family functioning and life events in the outcome of adolescent anorexia nervosa. The British Journal of Psychiatry: The Journal of Mental Science, 171, 545–549. https://doi.org/10.1192/bjp.171.6.545
Pike, K. M., Hilbert, A., Wilfley, D. E., Fairburn, C. G., Dohm, F. A., Walsh, B. T., & Striegel-Moore, R. (2008). Toward an understanding of risk factors for anorexia nervosa: A case-control study. Psychological Medicine, 38(10), 1443–1453. https://doi.org/10.1017/S0033291707002310
Pike, K. M., & Rodin, J. (1991). Mothers, daughters, and disordered eating. Journal of Abnormal Psychology, 100(2), 198–204. https://doi.org/10.1037//0021-843x.100.2.198
Pike, K. M., So, M., Hilbert, A., Maekawa, H., Shimanouchi, T., Wilfley, D., Dohm, F. A., Fairburn, C. G., & Weissman, R. S. (2021). Risk factors for anorexia nervosa and bulimia nervosa in Japan and compared to a U.S. sample. International Journal of Eating Disorders, 54(2), 155–167. https://doi.org/10.1002/eat.23442
Råstam, M., & Gillberg, C. (1991). The family background in anorexia nervosa: a population-based study. Journal of the American Academy of Child and Adolescent Psychiatry, 30(2), 283–289. https://doi.org/10.1097/00004583-199103000-00018
Sim, L. A., Homme, J. H., Lteif, A. N., Voort, V., Schak, J. L., K. M., & Ellingson, J. (2009). Family functioning and maternal distress in adolescent girls with anorexia nervosa. The International Journal of Eating Disorders, 42(6), 531–539. https://doi.org/10.1002/eat.20654
Smith, L. M., Mullis, R. L., & Hill, E. W. (1995). Identity Strivings within the Mother-Daughter Relationship. Psychological Reports, 76(2), 495–503. https://doi.org/10.2466/pr0.1995.76.2.495
Steinhausen, H. C., Jakobsen, H., Helenius, D., Munk-Jørgensen, P., & Strober, M. (2015). A nation-wide study of the family aggregation and risk factors in anorexia nervosa over three generations. International Journal of Eating Disorders, 48(1), 1–8. https://doi.org/10.1002/eat.22293
Strober, M., Freeman, R., & Morrell, W. (1997). The long-term course of severe anorexia nervosa in adolescents: survival analysis of recovery, relapse, and outcome predictors over 10–15 years in a prospective study. The International Journal of Eating Disorders, 22(4), 339–360. https://doi.org/10.1002/(sici)1098-108x(199712)22:4%339::aid-eat1%3.0.co;2-n
Su, X., Xu, B., Liang, H., Olsen, J., Yuan, W., Cnattingius, S., László, K. D., & Li, J. (2015). Prenatal maternal bereavement and risk of eating disorders in infants and toddlers: a population-based cohort study. Bmc Psychiatry, 15, 229. https://doi.org/10.1186/s12888-015-0612-9
Valente, S. (2016). The hysterical anorexia epidemic in the French nineteenth century. Dialogues in Philosophy Mental and Neuro Sciences, 9(1), 22–23.
Van Eeden, A. E., Van Hoeken, D., & Hoek, H. W. (2021). Incidence, prevalence and mortality of anorexia nervosa and bulimia nervosa. Current Opinion in Psychiatry, 34(6), 515–524. https://doi.org/10.1097/YCO.0000000000000739
Wewetzer, C., Deimel, W., Herpertz-Dahlmann, B., Mattejat, F., & Remschmidt, H. (1996). Follow-up investigation of family relations in patients with anorexia nervosa. European Child & Adolescent Psychiatry, 5(1), 18–24. https://doi.org/10.1007/BF00708210
Acknowledgement
None.
Funding
Open access funding provided by Università degli Studi di Roma La Sapienza within the CRUI-CARE Agreement.
Author information
Authors and Affiliations
Contributions
Conceptualization: ADC, SV; Data curation ADC, GP; Investigation: SV, BA, MNM, AV, GP; Methodology: ADC; MNM; Supervision: ADC, AMS; Roles/Writing - original draft: ADC, SV, BA, MNM; Writing - review & editing: ADC, MNM.
Corresponding author
Ethics declarations
Conflict of interest statement
On behalf of all authors, the corresponding author states that there is no conflict of interest.
Informed consent
Not applicable.
Conflict of interest
None.
Additional information
Publisher’s note
Springer Nature remains neutral with regard to jurisdictional claims in published maps and institutional affiliations.
Rights and permissions
Open Access This article is licensed under a Creative Commons Attribution 4.0 International License, which permits use, sharing, adaptation, distribution and reproduction in any medium or format, as long as you give appropriate credit to the original author(s) and the source, provide a link to the Creative Commons licence, and indicate if changes were made. The images or other third party material in this article are included in the article’s Creative Commons licence, unless indicated otherwise in a credit line to the material. If material is not included in the article’s Creative Commons licence and your intended use is not permitted by statutory regulation or exceeds the permitted use, you will need to obtain permission directly from the copyright holder. To view a copy of this licence, visit http://creativecommons.org/licenses/by/4.0/.
About this article
Cite this article
Del Casale, A., Adriani, B., Modesti, M.N. et al. Anorexia nervosa and familial risk factors: a systematic review of the literature. Curr Psychol 42, 25476–25484 (2023). https://doi.org/10.1007/s12144-022-03563-4
Received:
Revised:
Accepted:
Published:
Issue Date:
DOI: https://doi.org/10.1007/s12144-022-03563-4