Abstract
The Covid-19 pandemic has increased the vulnerability of cancer patients to psychological symptoms, in addition to treatment modality issues. The present study has aimed to determine the psychological state of Arab cancer patients during the COVID-19 pandemic and to explore the contributing factors. A cross-sectional, descriptive, correlational design with the Hospital Anxiety and Depression Scale (HADS), Insomnia Severity Index (ISI), Functional Assessment of Cancer Therapy–Fatigue subscale (FACT-F), and the Functional Assessment of Cancer Therapy–General (FACT-G) were used to collect the data. Out of 291 participants, 60.5% were female; 22.7% were 51–60 years; 31.6% were diagnosed with breast cancer; 44.3% with stage 2 cancer; 23% had contracted COVID-19; and 43.3% had received their first dose of the vaccine. The main study findings are: 74.9% had anxiety, 64.3% experienced depression, 68% suffered from insomnia, and 69.8% had fatigue. Quality of life (QoL) was low among cancer patients who had marked anxiety, depression, insomnia, or fatigue, and these findings were statistically significant (p < 0.05). Predictive factors showed males were 5.09 times more likely to report depression; gynecological cancer patients were 40.4 times more likely to experience insomnia, and patients who had COVID-19 were 5.13 times more likely to report fatigue. The study findings reveal that the COVID-19 pandemic affected the psychological state of cancer patients and had a significant effect on their quality of life. Hence, there is a need to develop a holistic cancer health care approach, which is often limited in Arab countries, to help patients manage these symptoms effectively and to decrease the prevalence of mental health morbidity.
Similar content being viewed by others
Introduction
Coronavirus (COVID-19) causes severe acute respiratory syndrome, which has escalated into a global pandemic since 2019 (Kumar et al., 2021). COVID-19 was initially identified in China in late 2019, and to date, the pandemic has affected more than 290 million people globally and caused more than 5 million deaths (WHO COVID- 19 dashboard, 2021). Cancer patients are more susceptible to COVID-19 (Moujaess et al., 2020) and are 2–3 times more likely to experience serious symptoms, distress, and death (Tian et al., 2020). In Saudi Arabia, up until January 2022, 562,437 individuals tested positive for the virus, and 8883 deaths have been attributed to the virus (Saudi MOH COVID-19 dashboard, 2021). The Saudi Health Ministry spokesman, Dr. Mohammed Al-Abd Al-Aly recently indicated that the number of confirmed COVID-19 daily cases has increased rapidly because of the Omicron variant, with infection rates doubling each week. He has urged people to follow the precautionary measures, which were first introduced at the start of the pandemic (Rashid, 2022). The prevalence of cancer in people with COVID-19 varies widely from study to study. It is reported that COVID-19 patients in the New York City region had a higher prevalence of cancer (of 5700 in-patients with COVID-19, 6% also had cancer) (Richardson et al., 2020). In a further study, 20% of COVID-19 patients who died also had active cancer (Onder et al., 2020), and 30% in the UKCCMP cohort who died also had active cancer (Lee et al., 2020; Saini et al., 2020) concluded that cancer patients who develop COVID-19 have a high probability of mortality. Considering a large number of undiagnosed COVID-19 infections and the lack of mortality statistics in many countries, the significance of the relationship between COVID-19, cancer, and mortality may be more significant than currently reported (Johannesen et al., 2021). Furthermore, Solano et al. (2016) found that individuals sought information and news regarding suicide more often during pandemics. Therefore, psychological distress related to COVID-19 might also significantly increase the risk of suicide. Wu et al. (2022) found that 45.4% of participants (n = 2094) experienced loneliness and stress related to COVID-19, which increased the levels of suicide in Taiwan. In addition, Wu et al. (2022) reported affective temperaments were independent and more strongly associated with lifelong suicide attempts than with the diagnosis of major mood disorders (Baldessarini et al., 2017). Interestingly, the Islamic population was found to have lower suicide rates than individuals of other religions. Also, religious individuals recovered faster from suicidal ideation, suggesting that religious affiliations may prevent attempted suicide. Nevertheless, Muslim cancer patients are not immune to the mental health problems posed by the COVID-19 pandemic (Hajiyousouf & Bulut, 2022).
The literature review has identified several studies undertaken in developed countries to assess the psychological status of cancer patients during the COVID-19 pandemic. (Ye et al., 2022; Chen et al., 2021; Momenimovahed et al., 2021). The majority of these studies have well documented the devastating effects of the pandemic on the mental health of not only cancer patients but also on the general population due to the increased uncertainties experienced in day-to-day living. Moreover, the health care services were forced to give priority to COVID-19 patients rather than to other cases. Normally, cancer care involves long-term support, which requires regular follow-up; however, during the pandemic, there was considerable disruption noted in this area. If the described situation can arise in developed countries, cancer patients in Middle Eastern countries, such as Saudi Arabia, where cancer care services are often limited, would experience significant negative impacts on their psychological state during the pandemic. Hence, the researcher has chosen this area of research for the current study, as no published research is yet available on this topic. By conducting this study, the researcher aims to bring new and substantial evidence regarding the psychological impacts of COVID-19 on cancer patients.
The following research objectives were developed for the study: (1) To examine the point prevalence of depression, anxiety, sleep disturbance, fatigue, and quality of life of cancer patients during the recent COVID-19 pandemic in Jazan, Saudi Arabia; (2) To assess patient distress in relation to depression, anxiety, insomnia, fatigue, and quality of life in terms of demographic characteristics; and (3) To evaluate the relationship between depression, anxiety, insomnia, fatigue, and quality of life of cancer patients during the recent COVID-19 pandemic in Jazan, Saudi Arabia.
Methods
Design, setting, and Data Collection Procedure
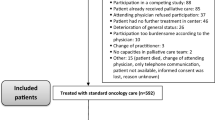
The study employed a large-scale cross-sectional, descriptive, correlational design. The survey was developed using an online platform (Qualtrics®) and a paper platform. Participants were recruited from the Mohammed bin Nasser hospital and the secondary analysis of data within the Oncology Center at the Mohammed bin Nasser hospital in Jazan, Saudi Arabia. Secondary analysis of existing data within the Oncology Center included a review of medical records and an assessment of the eligibility criteria of potential participants. Data was carefully evaluated along with the eligibility criteria, with 761 potential participants being excluded from the study, as detailed in Fig. 1. The Jazan region consists of a large agricultural heartland, which covers an area of 13,457 km² with a population of 1, 365,110 (Salam, 2010). Jazan is the most deprived region of KSA, with 34% of all families living in poverty (Dohman, 2012).
The sample size was determined using the Raosoft software calculator (Raosoft, 2004). It is based on a confidence level of 95%, with a margin of error of 5%, with a target population of 285 required to be statistically acceptable (as per cancer patient population).
The data set included standardized interviews with Nursing Directors and Head Nurses, as well as information obtained from the medical records of the cancer patients. The study was conducted during the period from August 2021 to December 2021; the eligibility criteria are presented in Table 1. Inclusion criteria for participation were as follows: adult patients over 18 years of age, able to speak and write in Arabic, and with no known psychiatric or neurological disorders that could interfere with study participation. In addition, they must be diagnosed with any type of cancer. The exclusion criterion for the participants was any cancer patient aged under 18 years. Project nurses and nursing students were responsible for data collection. Before data collection, both groups participated in a two-day workshop, delivered by the principal investigator. The workshop aimed to orientate participants to the study aim and objectives, including how to use the mapping instruments, and standardized interviews. Data collection involved registering information from each patient’s medical records, including demographic details and background history. The standardized instruments were distributed by preferred mode, either a paper copy or online form; participants were provided with sufficient time to complete the study instruments.
Measurement
Questionnaires obtained the following information: demographic characteristics, background history, and several psychometric scales - the Arabic versions of the Hospital Anxiety and Depression Scale (HADS), Insomnia Severity Index (ISI), the Functional Assessment of Cancer Therapy–Fatigue subscale (FACT-F), and the Functional Assessment of Cancer Therapy–General (FACT-G).
-
a)
Demographic characteristics:
Information obtained related to the demographic characteristics of participants and background history information.
-
b)
Depression and Anxiety:
The HADS questionnaire includes 14 items and assesses anxiety (7 items) and depression (7 items). All items are rated using a 4-point Likert-type response (0 to 3) (Zigmond & Snaith, 1983). The Arabic version of HADS demonstrated good internal consistency (Cronbach’s α = 0.83) (Terkawi et al., 2017).
-
c)
Insomnia:
The Insomnia Severity Index (ISI) is a 7-item self-report questionnaire assessing the nature, severity, and impact of insomnia (Morin et al., 2011). A 5-point Likert scale is used to rate each item (e.g., 0 = no problem; 4 = very severe problem) yielding a total score ranging from 0 to 28. A previous study reported acceptable psychometric properties for the Arabic version of this questionnaire (Cronbach’s α = 0.82) (Suleiman & Yates, 2011).
-
d)
Fatigue:
To measure fatigue, the Functional Assessment of Chronic Therapy-Fatigue subscale (FACT-F) was used in the study. This is a 13-item questionnaire that assesses self-reported fatigue in the past seven days (Yellen et al., 1997). Response options use a 5-point Likert scale for each item. Van Belle et al. (2005) suggested that the diagnosis of fatigue in patients with cancer should be 34. This study suggested that a score equal to or less than 34 indicates clinically significant fatigue. The Arabic version of FACT-F demonstrated good internal consistency (Cronbach’s α = 0.92) (Al Maqbali et al., 2020).
-
e)
Quality of life:
Quality of life (QoL) is an important aspect of the care of cancer patients. The Functional Assessment of Cancer Therapy General and Fatigue (FACT-G) self-administration questionnaire was used in the study (Cella et al., 1993; Webster et al., 2003). FACT-G measures QoL with 27 items divided into four domains: physical well-being (PWB) (7 items), social/family well-being (SWB) (7 items), emotional well-being (EWB) (6 items), and functional well-being (FWB) (7 items). The Arabic version of FACT-G revealed good internal consistency of 0.92 (Al Maqbali et al., 2020).
Statistical analysis
Data were entered into the Statistical Package for Social Sciences (SPSS) version 25. To address the research objectives, descriptive statistics were used to calculate the mean, standard deviation, standard errors, frequency, percentages of all scales and subscales, and the demographic characteristics of the participants. Chi-square (or Fisher’s exact test) was used to test whether the levels of depression, anxiety, insomnia, and fatigue differed in terms of demography and clinical characteristics. An independent t-test was used for the continuous variables of the quality-of-life subscale.
Logistic regression analysis was used to identify the predictive risk factors for depression, anxiety, fatigue, and QoL, and the independent variables (age, sex, marital status, education, occupation, having confirmed COVID-19, and vaccine status). A (p < 0.05) was considered to demonstrate statistical significance for all analyses.
Results
344 face-to-face surveys were conducted and a total of 291 valid questionnaires were returned online or as paper forms (See Fig. 1). Demographic characteristics of subjects (Table 1) showed the majority of the participants were female (60.5%, n = 176); belonged to the age group 51–60 years (22.7%, n = 66); were married (71.1%, n = 207); had basic education (50.9%, n = 148); unemployed (63.2%, n = 184). Clinical characteristics revealed (Table 1) the majority had breast cancer (31.6%, n = 92); stage 2 cancer (44.3%, n = 129); time since diagnosis was within 12 months in 39.2% (n = 114) of patients; the majority (76.6%, n = 223) were receiving chemotherapy; 23.4% ( n = 68) had more than two morbidities; only 23% (n = 67) had a confirmed COVID-19 infection; and 43.3% (n = 126) had received their first dose of the COVID-19 vaccine.
The psychological state of the cancer patients in this study refers to the percentage of depression, anxiety, insomnia, and fatigue they experienced, which was measured with standardized tools. From the assessment (Table 1), it was revealed that out of 291 participants, the prevalence of anxiety was 74.9% (n = 218), depression was reported by 64.3% (n = 187) respondents, and 68% (n = 198) suffered from insomnia, while fatigue was experienced by 69.8% (n = 203).
There was a significant difference in reported depression among male participants and those with hypertension/heart failure, and more than two comorbidities (p < 0.05). The depression group had significantly lower mean (SD) scores for QoL (61.57[15.33]) on the total scale as well as in the subscales of physical well-being (15.44 [6.46]), social well-being (18.03[6.3]), emotional well-being (14.12[3.67]), and functional well-being (13.98[5.79]) compared to the non-depression group. There were significant differences in reported anxiety in participants who had more limited educational opportunities, those undergoing chemotherapy, individuals with hypertension/heart failure, more than two comorbidities, and participants who had not taken any COVID-19 vaccines (p < 0.05). Participants in the anxiety group reported lower mean scores in the QoL (61.50[15.37]) total scale and the subscales of physical well-being (14.95 [6.20]), social well-being (18.08[6.23]), emotional well-being (13.96[3.57]), and functional well-being (14.51[6.06]) compared with non-anxiety patients. The insomnia group had significance (p < 0.05) for single participants, those with stage 4 cancer, individuals undergoing chemotherapy, those with hypertension/heart failure, asthma, and more than two comorbidities when compared to the non-insomnia group. Participants with insomnia reported lower mean scores on the QoL total scale (62.29[15.27]) and the subscales of physical well-being (14.87 [6.00]), social well-being (18.61[5.35]), emotional well-being (13.88[3.63]), and functional well-being (14.93[5.80]) when compared with non-insomnia patients (Table 1). Female participants, those who were single, unemployed, and who had not taken the COVID-19 vaccines were found to be significantly more likely to experience fatigue. There were significant differences in the reporting of fatigue, (p < 0.05), according to the site of cancer; participants with breast, thyroid, lymphoma, leukemia, gynecological, and others sites (lung) were more likely to experience fatigue when compared to the non-fatigue group. Participants with stages 3, 4, and unspecified stages of cancer were more likely to report fatigue. The fatigue group had significantly lower mean (SD) scores for QoL (60.17[14.4]) total scale as well as for the subscales: physical well-being (13.92 [5.83]), social well-being (18.1[6.2]), emotional well-being (13.55[3.52]), and functional well-being (14.6[5.81]) when compared to the non-fatigue group.
Predictive factors associated with Depression, anxiety, Insomnia, and fatigue
Four logistic regressions were completed to identify predictors of depression, anxiety, insomnia, and fatigue (Table 2). The logistic regression model for depression highlighted that patients with anxiety; insomnia, and low QoL were significantly more likely to experience depression (p < 0.5). However, the strongest predictor of depression was gender; male participants were 5.09 times more likely to report depression (95% CI: 1.94–13.32; p = 0.001) (Table 3).
In the anxiety logistic regression model, participants with secondary education, gynecological cancer, depression, and low QoL were predictors for reporting anxiety (p < 0.05). Furthermore, those who had depression were 1.36 times more likely to report anxiety (95% CI: 1.16–1.6; p = 0.001). In the insomnia logistic regression model, gynecological cancer was the strongest predictor, with participants being 40.4 times more likely to report insomnia (95% CI: 1.88–868; p < 0.05). The second predictor for insomnia was patients receiving radiotherapy, who was 17.69 times more likely to report insomnia (95% CI: 1.35–239; p = 0.03). The models demonstrated that patients experiencing anxiety, fatigue, diabetes, and other comorbidities were significantly more likely to suffer insomnia. Four independent variables were found to be significantly associated with fatigue (Table 2). The strongest predictor of fatigue were patients with a COVID-19 infection, who were 5.13 times more likely to report fatigue (95% CI: 1.64–16.1; p = 0.01). The second predictor of fatigue was found in patients diagnosed between 25 and 36 months previously, who were 3.66 times more likely to report fatigue (95% CI: 1.02–13.16; p = 0.05). Male participants were also 3.28 times (95% CI: 1-10.7; p < 0.05) more likely to experience fatigue. The QoL score was also found to be a significant predictor of fatigue (p < 0.05).
Discussion
The present study demonstrates that the Covid-19 pandemic has caused and continues to cause undesirable effects on the psychological state of cancer patients in Arab countries. The results of this study show that point prevalence of anxiety, depression, insomnia, and fatigue resulting from the pandemic in cancer patients in KSA is 74.9%, 64.3%, 68%, and 69.8% respectively. These findings are consistent with the study conducted by Chen et al. in China, where 74.5% of cancer patients suffered from depression, and 67.5% had anxiety (Chen et al., 2020). However, a lower rate of anxiety (17.7%) and depression (23.4%) was noted in another study (Wang et al., 2020) when compared to the present findings.
The study participants experienced 69.8% of clinically significant fatigue. In contrast, a study conducted by Cui et al. (2020) showed only 51.2% of fatigue among study participants. However, a slightly higher rate (74.8%) was reported in an earlier study conducted by Nugusse et al. (2021), which found that age, stage of cancer, presence of infection, type of cancer, and type of treatment were significantly associated with reported fatigue. Apart from cancer patients, even in the general population, a recent survey by Morgul et al. (2020), which examined the relationship between the COVID-19 pandemic and psychological fatigue in Turkey, reported that 64.1% of participants (n = 4700) were categorized as psychologically fatigued and had a positive correlation with psychological distress. Furthermore, Taylor et al. (2019) reported that anxiety and distress, isolation, and lack of physical movement were factors that could lead to fatigue in the general population.
Depression, anxiety, insomnia, and fatigue all had a significant association (p < 0.05) with QoL on the total scale and with lower scores in subscales, namely, physical, emotional, spiritual, and functional well-being. The lower scores in QoL may be due to fears associated with the COVID-19 pandemic in cancer patients. Fear of susceptibility to infection, lockdown measures imposed, restricted social activities, mass media information overload, uncertainty about the pandemic situation, rumors about vaccination effects, and the fear of losing loved ones to COVID-19 are some of the fears expressed by the participants, all of which may act as contributory factors to their poor psychological state. Similarly, previous studies have indicated the significant negative influence that depression, anxiety, insomnia, and fatigue have on reducing QoL and causing sleep disturbances in cancer patients (Rochmawati et al., 2020; Strik et al., 2021; Yeo et al., 2021).
Emotional distress in cancer patients can manifest as the mental symptoms of anxiety and depression, with changes in sleep pattern (Insomnia), and feelings of tiredness (Fatigue) being physical symptoms. Further, the COVID-19 pandemic has disrupted and altered normal routine hospital visits and follow-up care. Ciążyńska et al. (2020) found that of the cancer patients who participated in their study, 87% (n = 260) highlighted that the COVID-19 pandemic reduced their feelings of security and had a severe negative impact on their daily life activities, while 5% decided to discontinue treatment during the pandemic. Edge et al., (2021) reported that the COVID-19 pandemic has had a dramatic negative impact on cancer care globally. Disruption to services has been observed in all aspects of cancer care and the long-term effects of COVID-19 remain unclear. Nevertheless, the immediate effects on cancer patients and their care have become increasingly apparent (Edge et al., 2021). For example, 42% of cancer patients (n = 683) reported experiencing some disruption to their care (Edge et al., 2021) while others reported experiencing delayed treatment (Ciążyńska et al., 2020; Yildirim et al., 2021). In addition, 43% of healthcare workers (n = 150) within cancer care settings, reported atypical delays in delivering appropriate cancer care (Edge et al., 2021).
In the present study, predictive factors showed that Arab males were 5.09 times more likely to report depression. Gender identity differences exist in terms of the prevalence and severity of depression during the COVID-19 pandemic, which might reflect the dominant masculine and feminine discourses in addition to social and cultural patterns. This result is supported by a previous review that used data from two waves of the Wisconsin Longitudinal Study (n = 8,054), which showed that older white men with cancer may be particularly vulnerable to depression, emphasizing the significance of screening for depression (Pudrovska, 2010). However, the rate of major depression in women is 6.7 higher than in men globally; in 2010, the annual global prevalence was 5.5% and 3.2%, respectively, representing a 1.7-fold higher incidence in women (Albert, 2015).
In the present study, a logistic regression model was employed, which demonstrated that cancer patients with anxiety, insomnia, fatigue, and low QoL were at significant risk of experiencing depression (p ˃0.05). In cancer care, quality of life has become an important health outcome that should constantly be evaluated. Aside from cancer and its treatment, which may impact patients’ QoL, the current context of COVID-19 affects QoL in various ways, depending on virus circulation during the pandemic (Baffert et al., 2021). Zomerdijk et al.’s survey (2021) showed that the high psychological burden and unmet needs experienced by cancer patients (n = 394) during the COVID-19 pandemic highlight the urgent need for innovative solutions to rapidly identify these issues during and beyond the COVID-19 pandemic. Indeed, the lack of formal and virtual psychological support for cancer patients has brought additional challenges to their progress, recovery, and care outcomes during this period of the pandemic (Banaser & Alshammary, 2021).
In KSA, mass vaccination programs have been established that include AstraZeneca, Pfizer, and Moderna COVID vaccines offered free of charge to all citizens, residents, or holders of visitor visas. However, among cancer patients, there appears to be some vaccine hesitancy, as only 43.3% of participants in the study had taken up the first dose of the vaccine, and only 27% had received the second dose of the COVID-19 vaccination, with 29.6% remaining unvaccinated. Therefore, a COVID-19 vaccination promotion program should be considered for increasing vaccine uptake among cancer patients.
Altogether, anxiety, depression, insomnia, and fatigue are significant problems for cancer patients. The results of this study have several implications for service delivery structures for improving the psychological well-being of cancer patients. Health care organizations need to provide counseling support services or online workshops and training materials to enable patients to be better prepared to meet their psychological health needs. There is some evidence that highlights providing appropriate psychosocial care to cancer patients and their families as part of standard service delivery reduces distress and psychosocial morbidity associated with cancer, fosters a better quality of life during and after treatment, and eventually increases survival (Grassi et al., 2017). The most common forms of effective evidence-based interventions for this population are self-management education, support, and mindfulness. These approaches have been found to have a significant impact on reducing psychological symptoms in patients, and several researchers recommend their use (ElMokhallalati et al., 2018; Cillessen et al., 2019).
Limitations
The study was limited to a single region in Saudi Arabia, which may limit the generalizability of the reported findings to other regions or countries. Even within the Jazan region, data collection for the study was limited to a single hospital due to the lack of cancer centers in the region. The study utilized a cross-sectional design, which evaluated anxiety, depression, insomnia, and fatigue at one point in time, without any longitudinal observation of these issues for participants. Purposive sampling used to recruit the subjects might affect the generalizability of the results. The study purely relied on the use of participants’ self-reporting questionnaires to measure the incidence of psychological problems.
Recommendations
Routine assessments of the psychological state of cancer patients are recommended to identify early symptoms of psychological issues to plan for appropriate interventions and management to improve their quality of life in relation to COVID-19. Gender identity differences exist in terms of the prevalence and severity of depression during the COVID-19 pandemic, highlighting the significance of incorporating self-identified gender identity in nursing research, clinical practice, and policy. Further research to identify challenges and barriers faced by healthcare providers in implementing holistic health care for cancer patients requires exploration. Gain comprehensive, in-depth knowledge to understand the factors affecting mental health can be well elicited through qualitative studies. Although cancer patients had higher mortality and morbidity during the COVID-19 pandemic, this study has identified the low rate of vaccination among the respondents; therefore, it is recommended that the reasons for the low uptake are identified in future research. A theoretical framework applied in this area of research is recommended. The present study has focused only on the prevalence of mental health issues in cancer patients; future studies are recommended to identify the various fears affecting cancer patients and their preference for support systems in the face of the present and future pandemics. In addition, this study suggests that an important direction for future research is to compare gender patterns of cancer-related suffering among Arabs, especially given the traditional ideals of masculinity and femininity in Arab culture.
Conclusions
Depression, anxiety, insomnia, fatigue, and poor quality of life are common problems for cancer patients in KSA during the 18 months since the start of the COVID-19 pandemic. This study provides an understanding of the psychological well-being of cancer patients exposed to a rapidly spreading, life-threatening infectious disease, and helps provide evidence to assist preparedness for future outbreaks or pandemics of infectious diseases. Furthermore, it provides a foundation for the next stage of the study, which aims to identify appropriate interventions to improve the psychological well-being of cancer patients. Lessons learned during the COVID-19 pandemic will enable health care providers, especially nurses, to better face the challenges of the current and future pandemics, especially in ensuring a patient-centered approach to cancer care within a local context, particularly within health care systems where holistic health care, including psychosocial support, is poorly developed.
Data Availability
The data that support the findings of this study is available from the author upon any reasonable request.
References
Al Maqbali, M., Hughes, C., Gracey, J., Rankin, J., Hacker, E., & Dunwoody, L. (2020). Psychometric properties of the Arabic version of the Functional Assessment of Chronic Illnesses Therapy–Fatigue in Arabic cancer patients. Journal of Pain and Symptom Management, 59(1), 130–138. https://doi.org/10.1016/j.jpainsymman.2019.10.008
Albert, P. R. (2015). Why is depression more prevalent in women? Journal of Psychiatry & Neuroscience: JPN, 40(4), 219. https://doi.org/10.1503/jpn.150205
Baffert, K. A., Darbas, T., Lebrun-Ly, V., Pestre-Munier, J., Peyramaure, C., Descours, C., Mondoly, M., Latrouite, S., Bignon, E., Nicouleau, S., Geyl, S., Leobon, S., & Deluche, E. (2021). Quality of life of patients with cancer during the COVID-19 pandemic. In vivo, 35(1), 663–670. https://doi.org/10.21873/invivo.12306
Baldessarini, R. J., Innamorati, M., Erbuto, D., Serafini, G., Fiorillo, A., Amore, M., & Pompili, M. (2017). Differential associations of affective temperaments and diagnosis of major affective disorders with suicidal behavior. Journal of Affective Disorders, 210, 19–21. https://doi.org/10.1016/j.jad.2016.12.003
Banaser, M., & Alshammary, S. (2021). Psychological Support and Telehealth Options for Patients with Cancer during the Covid-19 Pandemic in Saudi Arabia. Integrative Journal of Medical Sciences, 8. https://doi.org/10.15342/ijms.2021.487
Cella, D. F., Tulsky, D. S., Gray, G., Sarafian, B., Linn, E., Bonomi, A., Silberman, M., Yellen, S. B., Winicour, P., & Brannon, J. (1993). The Functional Assessment of Cancer Therapy scale: development and validation of the general measure. Journal of Clinical Oncology, 11(3), 570–579. https://doi.org/10.1200/jco.1993.11.3.570
Chen, X., Wang, L., Liu, L., Jiang, M., Wang, W., Zhou, X., & Shao, J. (2021). Factors associated with psychological distress among patients with breast cancer during the COVID-19 pandemic: a cross-sectional study in Wuhan, China. Supportive Care in Cancer, 29(8), 4773–4782. https://doi.org/10.1007/s00520-021-05994-4
Chen, G., Wu, Q., Jiang, H., Zhang, H., Peng, J., Hu, J., Chen, M., Zhong, Y., & Xie, C. (2020). Fear of disease progression and psychological stress in cancer patients under the outbreak of COVID-19. Psycho-Oncology. https://doi.org/10.1002/pon.5451
Ciążyńska, M., Pabianek, M., Szczepaniak, K., Ułańska, M., Skibińska, M., Owczarek, W., Narbutt, J., & Lesiak, A. (2020). Quality of life of cancer patients during coronavirus disease (COVID-19) pandemic. Psycho-Oncology. https://doi.org/10.1002/pon.5434
Cillessen, L., Johannsen, M., Speckens, A. E., & Zachariae, R. (2019). Mindfulness-based interventions for psychological and physical health outcomes in cancer patients and survivors: a systematic review and meta‐analysis of randomized controlled trials. Psycho‐Oncology, 28(12), 2257–2269. https://doi.org/10.1002/pon.5214
Cui, Q., Cai, Z., Li, J., Liu, Z., Sun, S., Chen, C., & Wang, G. (2020). The psychological pressures of breast cancer patients during the COVID-19 outbreak in China - a comparison with frontline female nurses. Frontiers in Psychiatry, 1462. https://doi.org/10.3389/fpsyt.2020.559701
Dohman, A. (2021). Poverty in the Kingdom of Gold. http://www.almonitor.com/pulse/culture/2012/10/poverty-rising-issue-in-saudi-society.html#. Accessed 04 Dec 2021
Edge, R., Meyers, J., Tiernan, G., Li, Z., Schiavuzzi, A., Chan, P. , Vassallo, A., Morrow, A., Mazariego, C., Wakefield, C. E., Canfell, k., & Taylor, N. (2021). Cancer care disruption and reorganization during the COVID-19 pandemic in Australia: A patient, carer and healthcare worker perspective. PloS one, 16(9), e0257420. https://doi.org/10.1371/journal.pone.0257420
ElMokhallalati, Y., Mulvey, M. R., & Bennett, M. I. (2018). Interventions to support self-management in cancer pain. Pain Reports, 3(6), e690. https://doi.org/10.1097/pr9.0000000000000690
Grassi, L., Spiegel, D., & Riba, M. (2017). Advancing psychosocial care in cancer patients. F1000Research, 6. https://doi.org/10.12688/f1000research.11902.1
Hajiyousouf, I. I., & Bulut, S. (2022). Mental health, religion, and suicide. Open Journal of Medical Psychology. https://doi.org/10.4236/ojmp.2022.111002
Johannesen, T. B., Smeland, S., Aaserud, S., Buanes, E. A., Skog, A., Ursin, G., & Helland, Å. (2021). COVID-19 in cancer patients, risk factors for disease and adverse outcome, a population-based study from Norway. Frontiers in Oncology, 11, 1010. https://doi.org/10.3389/fonc.2021.652535
Kumar, A., Singh, R., Kaur, J., Pandey, S., Sharma, V., Thakur, L., Sati, S., Mani, S., Asthana, S., Sharma, T. K., Chaudhuri, S., Bhattacharyya, S., & Kumar, N. (2021). Wuhan to World: The COVID-19 Pandemic. Frontiers in Cellular and Infection Microbiology. https://doi.org/10.3389/fcimb.2021.596201
Lee, L. Y., Cazier, J. B., Starkey, T., Briggs, S. E., Arnold, R., Bisht, V., Booth, S., Campton, N. A., Collins, C. V. W. T., Curley, H., Earwaker, M., Fittall, P., Gennatas, M. W., Goel, S., Hartley, A., Hughes, S., FMedScii, D., Lee, D. K., ... UK Coronavirus Cancer Monitoring Project Team (2020). COVID-19 prevalence and mortality in patients with cancer and the effect of primary tumour subtype and patient demographics: a prospective cohort study. The Lancet Oncology, 21(10), 1309–1316. https://doi.org/10.1016/s1470-2045(20)30442-3
Momenimovahed, Z., Salehiniya, H., Hadavandsiri, F., Allahqoli, L., Günther, V., & Alkatout, I. (2021). Psychological Distress among Cancer Patients during COVID-19 Pandemic in the World: A Systematic Review. Frontiers in Psychology, 12. https://doi.org/10.3389/fpsyg.2021.682154
Morgul, E., Bener, A., Atak, M., Akyel, S., Aktaş, S., Bhugra, D., & Jordan, T. R. (2021). COVID-19 pandemic and psychological fatigue in Turkey. International Journal of Social Psychiatry, 67(2), 128–135. https://doi.org/10.1177/0020764020941889
Morin, C. M., Belleville, G., Bélanger, L., & Ivers, H. (2011). The Insomnia Severity Index: psychometric indicators to detect insomnia cases and evaluate treatment response. Sleep, 34(5), 601–608. https://doi.org/10.1093/sleep/34.5.601
Moujaess, E., Kourie, H. R., & Ghosn, M. (2020). Cancer patients and research during COVID-19 pandemic: A systematic review of current evidence. Critical Reviews in Oncology/Hematology, 150, 102972. https://doi.org/10.1016/j.critrevonc.2020.102972
Nugusse, T., Lemlem, S. B., Deressa, J., & Kisa, S. (2021). Prevalence of fatigue and associated factors among cancer patients attending Tikur Anbessa Specialized Hospital, Addis Ababa, Ethiopia. Cancer Management and Research, 13, 1909. https://doi.org/10.2147/cmar.s291298
Onder, G., Rezza, G., & Brusaferro, S. (2020). Case-Fatality Rate and Characteristics of Patients Dying in Relation to COVID-19 in Italy. JAMA,323(18), 1775–1776. https://doi.org/10.1001/jama.2020.4683
Pudrovska, T. (2010). Why is cancer more depressing for men than women among older white adults? Social Forces, 89(2), 535–558
Raosoft (2004). Raosoft Sample Size Calculator. Raosoft, Inc., Seattle. http://www.raosoft.com/samplesize.html. Accessed 04 Jun 2021
Rashid, H. (2022). Saudi Health Ministry rules out stricter lockdown amid COVID-19 case surge. https://www.arabnews.com/node/1997861/saudi-arabia. Accessed 04 January 2022
Richardson, S., Hirsch, J. S., Narasimhan, M., Crawford, J. M., McGinn, T., Davidson, K. W., & Northwell COVID-19 Research Consortium. (2020). Presenting characteristics, comorbidities, and outcomes among 5700 patients hospitalized with COVID-19 in the New York City area. Journal Of The American Medical Association, 323(20), 2052–2059. https://doi.org/10.1001/jama.2020.6775
Rochmawati, E., Wiksuarini, E., & Rahmah, R. (2020). Depression and quality of life among cancer patients undergoing chemotherapy. Palliative Medicine in Practice, 14(1), 1–6. https://doi.org/10.5603/PMPI.2020.0002
Saini, K. S., Tagliamento, M., Lambertini, M., McNally, R., Romano, M., Leone, M., Curigliano, G., & de Azambuja, E. (2020). Mortality in patients with cancer and coronavirus disease 2019: a systematic review and pooled analysis of 52 studies. European Journal of Cancer, 139, 43–50. https://doi.org/10.1016/j.ejca.2020.08.011
Salam, A. A. (2013). Population and household census, Kingdom of Saudi Arabia 2010: facts and figures. International Journal of Humanities and Social Science, 3(16), 258–263
Saudi MOH Coronavirus (COVID 19) Dashboard (2022). https://covid19.moh.gov.sa/. Accessed 04 January 2022
Solano, P., Ustulin, M., Pizzorno, E., Vichi, M., Pompili, M., Serafini, G., & Amore, M. (2016). A Google-based approach for monitoring suicide risk. Psychiatry research, 246, 581–586. https://doi.org/10.1016/j.psychres.2016.10.030
Strik, H., Cassel, W., Teepker, M., Schulte, T., Riera-Knorrenschild, J., Koehler, U., & Seifart, U. (2021). Why Do Our Cancer Patients Sleep So Badly? Sleep Disorders in Cancer Patients: A Frequent Symptom with Multiple Causes. Oncology Research and Treatment, 44(9), 469–475. https://doi.org/10.1159/000518108
Suleiman, K. H., & Yates, B. C. (2011). Translating the insomnia severity index into Arabic. Journal of Nursing Scholarship, 43(1), 49–53. https://doi.org/10.1111/j.1547-5069.2010.01374.x
Taylor, S. (2019). The Psychology of Pandemics: Preparing for the Next Global Outbreak of Infectious Disease. Cambridge Scholars Publishing
Terkawi, A. S., Tsang, S., AlKahtani, G. J., Al-Mousa, S. H., Musaed, A., AlZoraigi, S., U. S., & Altirkawi, K. A. (2017). Development and validation of Arabic version of the Hospital Anxiety and Depression Scale. Saudi Journal of Anaesthesia, 11(Suppl 1), S11–S18. https://doi.org/10.4103/sja.sja_43_17
Tian, Y., Qiu, X., Wang, C., Zhao, J., Jiang, X., Niu, W., Huang, J., & Zhang, F. (2021). Cancer associates with risk and severe events of COVID-19: A systematic review and meta‐analysis. International journal of cancer, 148(2), 363–374. https://doi.org/10.1002/ijc.33213
Van Belle, S., Paridaens, R., Evers, G., Kerger, J., Bron, D., Foubert, J., Ponnet, G., Vander Steichel, D., Heremans, C., & Rosillon, D. (2005). Comparison of proposed diagnostic criteria with FACT-F and VAS for cancer-related fatigue: proposal for use as a screening tool. Supportive Care in Cancer, 13(4), 246–254. https://doi.org/10.1007/s00520-004-0734-y
Wang, Y., Duan, Z., Ma, Z., Mao, Y., Li, X., Wilson, A., Qin, H., Ou, J., Peng, K., Zhou, F., Li, C., Liu, Z., & Chen, R. (2020). Epidemiology of mental health problems among patients with cancer during COVID-19 pandemic. Translational Psychiatry, 10(1), 1–10. https://doi.org/10.1038/s41398-020-00950-y
Webster, K., Cella, D., & Yost, K. (2003). Functional Assessment of Chronic Illness Therapy (FACIT) Measurement System: properties, applications, and interpretation. Health and Quality Life Outcomes, 1, 79. https://doi.org/10.1186/1477-7525-1-79
WHO Coronavirus (COVID 19) Dashboard (2021). https://covid19.who.int/. Accessed 04 January 2022
Wu, C. Y., Lee, M. B., Huong, P. T. T., Chan, C. T., Chen, C. Y., & Liao, S. C. (2022). The impact of COVID-19 stressors on psychological distress and suicidality in a nationwide community survey in Taiwan. Scientific Reports, 12(1), 1–10. https://doi.org/10.1038/s41598-022-06511-1
Ye, Y., Wang, J., Cai, S., Fu, X., & Ji, Y. (2022). Psychological distress of cancer patients caused by treatment delay during the COVID-19 pandemic in China: A cross‐sectional study. Psycho‐Oncology. https://doi.org/10.1002/pon.5946
Yellen, S. B., Cella, D. F., Webster, K., Blendowski, C., & Kaplan, E. (1997). Measuring fatigue and other anemia-related symptoms with the Functional Assessment of Cancer Therapy (FACT) measurement system. Journal of Pain and Symptom Management, 13(2), 63–74. https://doi.org/10.1016/s0885-3924(96)00274-6
Yeo, S., Lee, J., Kim, K., Kim, H. J., & Chung, S. (2021). Depression, Rather Than Cancer-Related Fatigue or Insomnia, Decreased the Quality of Life of Cancer Patients. Cancer Research and Treatment: Official Journal of Korean Cancer Association, 53(3), 641. https://doi.org/10.4143/crt.2020.1212
Yildirim, O. A., Poyraz, K., & Erdur, E. (2021). Depression and anxiety in cancer patients before and during the SARS-CoV-2 pandemic: association with treatment delays. Quality of Life Research, 30(7), 1903–1912. https://doi.org/10.1007/s11136-021-02795-4
Zigmond, A. S., & Snaith, R. P. (1983). The hospital anxiety and depression scale. Acta Psychiatrica Scandinavica, 67(6), 361–370. https://doi.org/10.1111/j.1600-0447.1983.tb09716.x
Zomerdijk, N., Jongenelis, M., Short, C. E., Smith, A., Turner, J., & Huntley, K. (2021). Prevalence and correlates of psychological distress, unmet supportive care needs, and fear of cancer recurrence among haematological cancer patients during the COVID-19 pandemic. Supportive Care in Cancer, 29(12), 7755–7764. https://doi.org/10.1007/s00520-021-06369-5
Acknowledgements
The authors’ team would like to thank the oncology centre at Mohammed Bin Nasser Hospital for their support to help complete this work. In addition, we would like to thank nursing students AbdulRahman Hammad Masmali, Atayaf Muhammed Gasem, and Amal Mohammed Hadadi for their participation and input into data collection. Finally, the authors wish to thank ' study participants, their relatives, and nursing staff for their willingness and motivation which made this study possible.
Funding
The authors have no funding to declare.
Author information
Authors and Affiliations
Contributions
Conceptualization: Norah Madkhali; methodology: Mohammed Al Meqbali; Material preparation and data collection: AbdulRahman Ameri, Mohammed Madkhali; formal analysis and investigation: Mohammed Al Meqbali, Norah Madkhali; writing original draft preparation: Norah Madkhali; Zakariya Al-Naamani, Bushra Alshammari; review and editing: Norah Madkhali; Zakariya Al-Naamani.
Corresponding author
Ethics declarations
Ethical approval
The study was approved by Jazan Health Ethics Committee at the Ministry of Health, Saudi Arabia (H-10-Z-073).
Consent to participate
All participants consented to participate in this study.
Consent for publication
All individual participants consented to having their data published.
Conflict of interest
The authors declare no competing interests.
Additional information
Publisher’s Note
Springer Nature remains neutral with regard to jurisdictional claims in published maps and institutional affiliations.
Rights and permissions
About this article
Cite this article
Madkhali, N.A., Ameri, A., Al-Naamani, Z.Y. et al. Has the COVID-19 pandemic affected the psychological state of arab cancer patients?. Curr Psychol 43, 13829–13840 (2024). https://doi.org/10.1007/s12144-022-03414-2
Received:
Revised:
Accepted:
Published:
Issue Date:
DOI: https://doi.org/10.1007/s12144-022-03414-2