Abstract
The limited material and human resources available in the Spanish public mental health system, combined with the high prevalence of emotional disorders nowadays, makes it necessary to search for and implement other more cost-effective formats. The versatility of the Unified Protocol (UP) for the transdiagnostic treatment of emotional disorders allows its application in group format, which could be a cost-effective solution for the system. The aim of the present study is to investigate the cost-effectiveness of the UP applied in group format in specialized care units compared to the Treatment as usual (TAU) in the Spanish public mental health system over a 15-month time period. The sample of this study consisted of 188 patients, diagnosed with an emotional disorder, randomized to the UP condition in group format or to the TAU condition in individual format. The findings of this study have shown the same beneficial results for the participants with symptoms of anxiety and depression in both conditions and greater improvements in quality of life in the UP condition. Regarding cost-effectiveness results, at the 15-month follow-up, participants in the UP condition received a greater number of sessions, with a lower total economic cost compared to the TAU condition. Finally, reductions in the number of participants using antidepressants and a reduction in medication burden were found in the UP condition over time. The results of this study show that UP applied in a group format can be a cost-effectiveness solution for the Spanish public mental health system. Trial registration number: NCT03064477 (March 10, 2017).
Similar content being viewed by others
Avoid common mistakes on your manuscript.
Introduction
The functional model of Emotional Disorders (EDs; Barlow et al., 2018), describe the three features that often occur across all EDs: frequent, intense emotions (i.e., sadness, guilt, anxiety, etc.), negative reactions to those emotions (i.e., “I am a weak person”) and avoidance of emotions strategies (i.e., avoiding social activities). The biological vulnerability factor shared by EDs is high neuroticism (and in some cases low extraversion), which has been associated with the etiology and maintenance of these disorders (Barlow et al., 2014; Bullis et al., 2019). These shared temperamental dimensions could explain the high comorbidity between EDs (Brown & Barlow, 2009), which has contributed to EDs being the most prevalent disorders nowadays.
Prevalence and cost of treatment of EDs
In Europe, it is estimated that 38.2% of the population suffers from a mental disorder, with anxiety disorders (14%) and depressive disorders (12%) being the most prevalent disorders (World Health Organization [WHO], 2017). In the case of Spain, in 2019, a total of 5.8% of the Spanish population had been diagnosed with an anxiety disorder and 5.2% with depression (National Statistics Institute [NSI], 2020), which shows that we are dealing with an important public health problem.
The high prevalence of EDs causes an increase in the demand for medical and psychological care. This situation, added to the limited resources (economic, material and human) available to the Spanish Health System (Gabilondo et al., 2011), often leads to the saturation of public health services. This situation is reflected in long waiting lists, as shown in the study by Díaz et al. (2017), who found a total delay of 74 days for the first mental health consultation.
The aforementioned high demand implies a high cost of treatment for the public health settings. According to the Organization for Economic Cooperation and Development (OECD/EU, 2018), the total cost of mental health problems represented about 4% of the gross domestic product (GDP) of European countries in 2018, estimating a total cost of 113,405 million euros (€3,406 per person per year) derived from mood disorders, and 65,995 million euros (€1,076 per person per year) for anxiety disorders (Gustavsson et al., 2011).
If we consider the data from Spain, it is estimated that the total cost of mental health problems accounted for 4.2% of GDP, and a total of 64,542 million euros in healthcare costs (OECD/EU, 2018). Of this amount, it is estimated that a total of 6,145 million euros (€3,402 per person per year) corresponds to the costs of mood disorders (Vieta et al., 2021) and 6,219 million euros (€997 per person per year) to the direct costs of anxiety disorders (Gustavsson et al., 2011). Within these direct costs, the high usage of anxiolytics and antidepressants stands out. According to data from the Ministry of Health, (2022), during 2021 a total of 59 million packages of anxiolytics, at a cost of 107 million euros, and 49 million packages of antidepressants, at a cost of 607 million euros, were prescribed, making Spain the second largest consumer of anxiolytics and the fourth for antidepressants in the European Union (Estrela et al., 2020).
Cost-effective interventions
However, despite the high demand for psychological assistance and the high costs associated with the treatment, the services mainly used in Mental Health Units are interventions in individual format, even though it is not the most cost-effective format (Norton, 2012). Individual face-to-face intervention is the most commonly used treatment format and the one that the National Health System users prefer to receive. This is reflected in the study by Osma et al. (2019), which analyzed the intervention format preferences of 267 users of mental health units with a primary diagnosis of EDs. The results of this study showed that the majority of the participants (85.4%) preferred psychological treatment in an individual format and only 14.2% of users preferred the group format. The arguments against the group format were lack of privacy, difficulties of expression and low efficacy. Similarly, the results of the study conducted by Bryde Christensen et al. (2022) in the Danish health service on patients' experience of group treatment, showed that most participants, before starting the group intervention, were skeptical about the effectiveness of the group treatment. However, after completion of the treatment, the participants were pleasantly surprised by the treatment received, and by the care, understanding and support received by the group and the therapist. Contrary to what patients seem to think, especially before starting group treatment, group treatments have proven to be equally or even more effective than individual treatments, as well as being more cost-effective (Ruiz-Rodríguez et al., 2018).
In addition to the group format, another way to reduce the costs of treating EDs in public mental health settings may be to use transdiagnostic psychological interventions. These interventions focus on addressing the etiological and maintenance mechanisms shared by different disorders (Brown & Barlow, 2009). With this approach, transdiagnostic psychological interventions could be a cost-effective alternative for public mental health settings because it facilitates their application in a group format, since they allow the inclusion of people with different diagnoses, but who share common vulnerability mechanisms (Newby et al., 2015). This allows a greater number of people to be cared for in a shorter period of time, with the consequent economic and time savings, which will reduce the long waiting lists of public mental health settings. Additionally, through a single treatment protocol, we can treat users with different diagnoses and symptomatology thus reducing the costs of training each therapist in specific treatment protocols (Wilamowska et al., 2010), and the structured and protocolized format of these treatments facilitates the dissemination of the treatment, reducing the costs derived from the implementation of evidence-based treatments (McHugh & Barlow, 2010).
Finally, another solution to reduce costs may be related to the reduction of pharmacological doses. Several systematic reviews have found that therapies such as Cognitive Behavioral Therapy (CBT) facilitate the reduction of doses and consumption of antidepressants and anxiolytics without increasing the risk of relapse (van Dis et al., 2020).
Intervention needs and opportunities
Our research group is conducting a multicenter randomized clinical trial with the aim of analyzing the efficacy and cost-effectiveness of the Unified Protocol for the Transdiagnostic Treatment of Emotional Disorders (UP; Barlow et al., 2018), applied in group format in the Spanish public mental health system (Osma et al., 2018). The UP is a cognitive-behavioral treatment based on a transdiagnostic approach, which focuses on addressing the vulnerability mechanisms shared by people suffering from EDs, specifically in targeting neuroticism (Bullis et al., 2019).
So far, several systematic reviews and meta-analysis studies have shown that UP is a highly effective treatment for EDs, applied mainly in an individual format, but also when applied in a group format (Carlucci et al., 2021; Sakiris & Berle, 2019). Regarding the efficacy of the UP applied in group format in SPMH settings, the efficacy results obtained by our team showed that, at the six-month follow-up, the improvements obtained by the UP condition are statistically superior compared to the treatment as usual (TAU) condition (non-structured CBT specific for each disorder in individual format); specifically, changes in symptoms of depression, anxiety and improvements in quality of life were higher (Cohen’s d 0.69 to 0.87) (Osma et al., 2022). In addition, we have found that there were statistically significant reductions in personality outcomes such as neuroticism and negative affect, as well as increases in extraversion and positive affect after the UP intervention. Moreover, these changes were greater when initial scores in neuroticism and negative affect were high, or low in extraversion and positive affect (Osma et al., 2021).
Despite the good efficacy outcomes found, to our knowledge, there is currently no data published about the different costs derived by the application of the UP in specialized care units in international or national public mental health systems. For example, although studies such as the one carried out by Steele et al. (2018) propose the reduction of costs associated with the training of therapists, since a single treatment could address a large number of disorders, there are no other studies that have analyzed the cost-efficacy of the group UP for transdiagnostic treatment of EDs. The need and relevance of this knowledge could have relevant implications for mental health managers working in public mental health settings in Spain.
Purpose of the current study
The aim of the present study is to investigate the cost-effectiveness of the UP applied in group format in specialized care units in the Spanish public mental health system during a 15-month time period. For this purpose, we will analyze the efficacy of the UP applied in a group setting for the improvement of symptoms of depression, anxiety and quality of life and we will calculate the cost associated with the treatment sessions compared to the TAU condition in an individual format. We hypothesize that an intensive UP intervention applied in group format in two-hour sessions held weekly for 12 weeks will be more cost-effective for the Spanish public mental health system in comparison with TAU over a 15-month period of time.
Method
Participants
The participants of this study were selected from the sample of a main study, who were part of a multicenter randomized clinical trial (Osma et al., 2018). This subsample consisted of 188 specialized care users randomized in two conditions, UP applied in group format (n = 96) and TAU condition (n = 92). Participants in the UP condition had a mean age of 42.73 years (SD = 12.15, range 18–65) and 77.1% (n = 74) were female. For TAU condition, the mean age of users was 43.08 (SD = 13.42, range 18–72) and 78.3% of them (n = 72) were female. 78.1% of the participants in the UP condition (n = 75), and 78.3% (n = 72) in the TAU condition, were taking psychotropic medication at the beginning of the intervention. Regarding the main diagnoses of the participants, and as can be seen in Table 1, 43.6% of the participants (n = 82) had a main anxiety disorder, being generalized anxiety disorder (8.5%), unspecified anxiety disorder (6.4%) or panic disorder without agoraphobia (6.4%) the most prevalent. Meanwhile, 31.4% of the participants (n = 31.4%) had a mood disorder, being major depressive disorder the most prevalent (20.7%). Finally, 25% of the participants (n = 47) presented a mixed disorder, specifically an adjustment disorder. Table 1 shows the remaining sociodemographic characteristics of the participants.
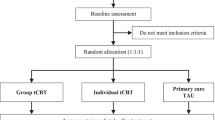
This subsample of the main study was selected based on whether they presented data on the number of treatment sessions received (at least 8 treatment sessions in the UP condition and at least 4 in the TAU condition, throughout the 15-month period) and data on pharmacological treatment in at least two of the evaluation time points in order to have as much complete information as possible to carry out an estimate of the cost of both experimental conditions. The flow diagram can be viewed in Fig. 1.
Measures
Anxiety Disorders Interview Schedule for DSM-IV (ADIS-IV-L; Di Nardo et al., 1994) is the Spanish version (Botella & Ballester, 1997). This semi-structured interview, based on the DSM-IV diagnostic criteria (American Psychiatric Association [APA], 1994), was used to assess whether the study participants met diagnostic criteria for an emotional disorder (generalized anxiety disorder, panic disorder, obsessive–compulsive disorder, agoraphobia, adjustment disorders, major depression disorder, dysthymic disorder, among others).
Sociodemographic data questionnaire
This questionnaire was developed ad hoc and was completed by the therapist. It collected the sociodemographic information of the participants, specifically: age, educational level, marital status, employment status and primary and secondary clinical diagnosis.
Clinical information
The main and secondary diagnosis, the number of treatment sessions received and whether the participant was receiving pharmacological treatment, the name of the pharmacological treatment and dosage were collected at each evaluation point by the patients' referring therapists.
Beck Depression Inventory (BDI-II; Beck et al., 1996; Sanz et al., 2003). It consists of 21 items and evaluates the presence and severity of depressive symptomatology. The response scale is a four-point Likert-type scale ranging from 0 "absence of depressive symptoms" to 3 "total or severe presence of depressive symptoms", the maximum score that can be obtained in the questionnaire is 63 points. The internal consistency in the present sample is Cronbach's alpha 0.89.
Beck Anxiety Inventory (BAI; Beck & Steer, 1993; Sanz et al., 2012). This instrument consists of 21 items and evaluates the presence and severity of anxiety symptoms. This instrument uses a four-point Likert-type response scale ranging from 0 "absence of anxiety symptoms" to 3 "total or severe presence of anxiety symptoms". The maximum score that can be obtained on the instrument is 63 points. The Cronbach's alpha in the present sample is 0.92.
Quality of Life Index (QLI; Ferrans & Powers, 1985; Mezzich et al., 2000). This questionnaire consists of 10 items assessing 10 domains related to quality of life, specifically: 1) physical well-being; 2) psychological and emotional well-being; 3) independent functioning; 4) occupational functioning; 5) interpersonal functioning; 6) social-emotional support; 7) sociocommunity and service support; 8) personal fulfillment; 9) spiritual fulfillment; and 10) global perception of quality of life. The response scale is a 10-point Likert-type scale ranging from 1 "Bad" to 10 "Excellent". In the present sample, a Cronbach's alpha of 0.83 was obtained.
Client Satisfaction Questionnaire (CSQ-8, Larsen et al., 1979). This instrument consists of 8 questions about client satisfaction with the service received. A Likert-type 5-point response format is used, ranging from 0 "Not at all" to 4 "Very much". In the present study only one of the items referring to "To what extent has this treatment program caused you discomfort?" has been included in order to assess the degree of discomfort generated by the intervention program.
Procedure
The public mental health system users who attended the centers participating in the study were evaluated by their referral psychologist to see if they met the inclusion criteria for participation in the study. The inclusion criteria were: a) Main diagnosis of emotional disorder (includes anxiety disorders, unipolar mood disorders, and related disorders, such as somatoform and dissociative disorders; Bullis et al., 2019); b) To be over 18 years of age; c) To understand perfectly the language in which the therapy is carried out; d) Be able to participate in the evaluation and treatment sessions and sign the informed consent, and e) If receiving pharmacological treatment,, no changes had taken place in the three months before the start of the treatment and they accepted to not have any changes made during the treatment if possible. As for the exclusion criteria, these were: a) The patient presents a severe mental disorder, current risk of suicide or substance abuse in the previous 3 months, and b) The patient has received, in the last 5 years, 8 or more sessions of psychological treatment clearly based on the principles of CBT.
Once assessed, and after confirming that they met the inclusion criteria, the participants were invited to enroll in the study. Following the signing of the informed consent form, participants completed the pre-treatment assessment, were stratified according to their anxiety and depression scores and randomized to the two treatment conditions: UP in group format, which consisted of 8 treatment modules applied intensively in 12 weekly sessions, each 2 h long (3 months approximately), and carried out by a trained therapist and co-therapist. All therapists who applied the UP intervention followed the guidelines of the therapist manual (Barlow et al., 2011b) and were previously trained in the management of UP through group workshops with an average duration of 15 h (range 10—20 h). In addition, once they started the first treatment group, they received individualized supervision throughout the 12 treatment sessions, with the aim of ensuring treatment fidelity. This supervision was carried out by an expert supervisor in UP. Finally, the client workbook (Barlow et al., 2011a) was given to all participants in this condition.
The other condition was the TAU, which consisted of a CBT non-protocolized intervention, in individual format and specific for each disorder, with a duration and frequency determined by the availability of the therapist and the public mental health center where the treatment was carried out.
The psychological intervention was combined with the prescribed pharmacological treatment, if the patient was receiving it, in both conditions. For more information about the procedure, please consult (Osma et al., 2018).
Over a time period of 15 months, we conducted 5 evaluations of both conditions at the following time points: Time1: pre-treatment; Time2: 3 months after treatment onset (coinciding with the end of the UP treatment condition); Time3: 6 months after treatment onset; Time4: 9 months after treatment onset; and Time5: 15 months after treatment onset.
In addition, in order to analyze the direct costs of treatments, the study's collaborating therapists recorded: a) number of treatment sessions received at each evaluation time; b) name and dose of the pharmacological treatment at each evaluation time, where applicable.
The direct costs associated with each psychological treatment session were calculated on the basis of the data available in Conselleria de Sanitat de la Comunitat Valenciana (Conselleria de Sanitat, Universal i Salut Pública, 2021), since most of the sample was recruited in that autonomous community of Spain (48.4%). This public document describes the annual salaries of each professional according to their seniority, that is to say, the number of years they have been working in the same position, and with the same responsibilities, within the health organization’s hierarchy (e.g., clinical psychologist or director of the mental health unit). In addition, this document also informed about the working hours per year of each health professional. Considering this information, we could establish which amount of money one hour of each clinical psychologist’s time cost to the health organization and, therefore, the cost of each treatment session. The mean from the salary without supplements up to the salary with the highest number of specific supplements was calculated and divided by the number of working hours established for the personnel of the health care institutions (Decreto 38/2016, de 8 de abril). As a result, an average cost of €23.98 (per patient and session) was obtained for the TAU condition. The cost of the UP session was obtained by multiplying that value by the cost per session of the 2 therapists needed to carry out the treatment group and the two-hour duration, divided by the average number of patients seen in the group (average of 8 participants), thus resulting in a cost of €11.99 (per patient and session) for the UP condition.
Finally, regarding pharmacological treatment, pharmacological usage was recorded and classified into antidepressants, antiepileptics, antipsychotics and anxiolytics. Next, the total medication burden was calculated by recoding the doses consumed of each drug from 1 to 4, according to the minimum and maximum recommended doses for each drug, where 1 was "minimum recommended dose or non-habitual consumption (use on demand or as a rescue dose)" and 4 "maximum recommended doses", as stated in the literature (Sackeim, 2001), and the mean score of medication doses taken by each participant was calculated.
Data analysis
First, descriptive statistical analyses were carried out for the analysis of the sociodemographic data of the participants. Furthermore, mean comparison analysis between participants in the UP and TAU condition was carried out through analysis of variance (ANOVA) and Chi-square test.
Next, differences in the percentage of pharmacological usage between treatment conditions were analyzed through a Chi-square test and over time through a Cochran's Q Test (for categorical variables). Differences in medication burden were also calculated between treatment conditions and at each time point through the linear mixed model using the SPSS program (version 26, IBM Corp, 2019).
Finally, for the cost-effectiveness analyses, the data were analyzed with linear mixed effects models using the lme4 package (version lme4_1.1–13; Bates et al., 2015) for R statistical software (version 4.1.2; R Core Team, 2021). Five different models were fitted for each dependent measure: Depression (BDI), Anxiety (BAI), Quality of life (ICV), Number of sessions and Treatment cost. For each model, Time (Time1 vs. Time2 vs. Time3 vs. Time4 vs. Time5), Condition (TAU vs. UP) and their interaction term were entered as fixed effects. Time was dummy coded, with Time1 being the baseline. Condition was also dummy coded, with TAU being the baseline. Random intercepts for center and participants were included in the random part of the nested models [i.e., Dependent measure ~ Time × Condition + (1|Center/Participant)].
Results
Descriptive statistical results, number of sessions of treatment received, psychotropic medication usage and degree of discomfort generated by the intervention program
Descriptive statistics for the five dependent measures as a function of condition and time are provided in Table 2. In terms of differences between treatment conditions, no statistically significant differences were found (p > 0.05) between treatment conditions in the sociodemographic variables (gender, age, primary and secondary diagnosis), neither in the baseline Time1 (pretreatment) scores of depressive symptoms, anxiety nor quality of life (p > 0.05).
Regarding the number of sessions received (see Table 2), the average number of treatment sessions received during the first 3 months (T2) was 10.20 (SD = 2.17, range 8–16). Over the 15 months of follow-up (Time5), the number of sessions received was 13.49 sessions (SD = 2.84, range 8–20) in the UP condition. Throughout this period, 17.71% (n = 17) of the participants in the UP condition required extra treatment sessions in individual format, with a mean of 2.06 sessions (SD = 1.08, range 1–5).
Concerning the TAU condition, the average number of treatment sessions received during the first three months was 2.24 (SD = 1.16, range 1–5), and a total of 7.65 sessions (SD = 3.23, range 4–14) over the 15-month follow-up.
Regarding psychotropic medication usage, differences were found in the number of participants who consumed the following types of psychotropic medication throughout the treatment, specifically: antiepileptics in Time1 (pre-treatment) (χ2 (1) = 6. 75, p = 0.009), Time4 (χ2 (1) = 5.425, p = 0.020) and Time5 (χ2 (1) = 3.811, p = 0.044), and antipsychotics in Time3 (χ2 (1) = 7.88, p = 0.005). In all of them, the highest consumption was in the TAU condition. Finally, we also found a reduction in the number of participants taking antidepressants over time in the UP condition (χ2 (4) = 11.83, p = 0.019), but not the other types of psychotropic medication or in the TAU condition (p > 0.05). The frequencies of the total number of participants who consumed psychotropic medication at each time point are shown in Table 2.
Regarding the evolution of psychotropic medication doses used throughout the course of treatment, a statistically significant effect of time on medication burden was found in the UP condition (F = 2.54, p = 0.042, dof = 168.15, Cohen’s d = 0.23), but not in the TAU condition (F = 0.93, p = 0.447, dof = 172.19, Cohen’s d = 0.14).
Finally, if we consider the degree of discomfort generated by the intervention programs, the results have shown low values in both treatment conditions. Specifically, a mean value of 1.88 out of 4 (SD = 0.88, range 1—4) in the UP condition and a mean value of 1.64 out of 4 (SD = 0.78, range 1—4) in the TAU condition. No statistically significant differences were found in the discomfort generated by the interventions (F = 1.57, p = 0.214).
Number of sessions measure model and effectiveness analyses on symptoms of depression, anxiety and quality of life
In terms of the number of sessions measure model (see Table 3), the results showed a statistically significant interaction between Condition (UP) and Time (Time2, Time3, Time4, Time5) in all the time segments (b ranged from 7.96 to 5.84; t ranged from 29.04 to 21.30), which means that participants in the UP condition received a higher amount of sessions within the same time segments than participants in the TAU condition, and also that the majority of these sessions occurred in earlier time segments for the participants in the UP condition (approximately within the first three months of treatment), as shown in Fig. 2.
Evolution of the number of sessions during the course of the unified protocol and treatment as usual. Note: Model Estimates for Number of sessions as a function of Condition (TAU vs. UP) and Time (Time1 vs. Time2 vs. Time3 vs. Time4 vs. Time5). Error bars represent 95% CIs. Time1 = Pre treatment time, Time2: 3 months after treatment onset (coinciding with the end of the UP treatment condition); Time3: 6 months after treatment onset; Time4: 9 months after treatment onset; and Time5: 15 months after treatment onset, UP = Unified protocol, TAU = Treatment as usual
Regarding the model for Depression, and as can be seen on Table 3 (and Figure 1 in the supplementary material), the model showed a significant effect of Time in the five time segments for both Conditions (b ranged from -6.41 to -8.10; t ranged from -5.79 to -6.09), which points to lower levels of depression as the sessions for both treatments (UP and TAU) progressed, with both interventions achieving statistically significant reductions in depression scores over time. In addition, the model did not show a significant main effect of Condition, which means no significant differences in depression for both conditions, neither a significant interaction between Condition (UP) and Time (Time2, Time3, Time4, Time5), so the scores evolved over time in a similar way in both conditions. However, the effect sizes were larger in the UP condition, despite the fact that large effect sizes were obtained in both conditions when comparing Time1 to Time5: Cohen's d = -0.94 for the UP condition and Cohen's d = -0.71 for the TAU condition.
According to the model for Anxiety, and as shown in Table 3 (and Figure 2 in the supplementary material), results showed a significant effect of Time in the five time segments for both Conditions (b ranged from -3.34 to -7.79; t ranged from -2.79 to -5.51), which points again to lower levels of anxiety as the sessions for both treatments (TAU and UP) progressed, with both interventions achieving statistically significant reductions in anxiety scores over time. In addition, the model also did not show a significant main effect of Condition, which means no significant differences in anxiety for both conditions, neither a significant interaction between Condition (UP) and Time (Time2, Time3, Time4, Time5), with scores evolving over time in a similar way in both conditions. Again, when comparing Time1 to Time5, moderate effect sizes were obtained in the UP condition (Cohen's d = -0.71) and medium-moderate in the TAU condition (Cohen's d = -0.60), being higher in the UP condition.
Finally, as can be checked on Table 3 (and Figure 3 supplementary material), the model for Quality of life also showed a significant effect of Time in the five time segments for both Conditions (b ranged from 0.38 to 0.81; t ranged from 2.44 to 4.44), pointing to higher levels of quality of life as the sessions for both treatments (TAU and UP) progressed. In addition, the model did not show a significant main effect of Condition, but it showed a significant interaction between Condition (UP) and Time (Time2, Time3, Time4, Time5) in all the time segments (b ranged from 0.55 to 0.66; t ranged from 2.52 to 2.72), which means that although both treatments were beneficial for quality of life, the UP produced significantly higher improvements than the TAU. Large effect sizes were obtained when comparing Time1 to Time5 for the UP condition (Cohen's d = 0.85), and moderate effect sizes for the TAU condition (Cohen's d = 0.51).
Note that the results presented for each model consider the variability due to the different centers where the treatments where applied, as random intercepts for Center and Participants were included in the random part of the nested models. It was found that the variability due to the center did not modify the results obtained.
Costs of the treatments
The cost of treatment sessions received can be seen in Table 2, the mean cost of treatment at 15-month follow-up (Time5) was €161.74 for the UP condition (SD = 34.09, range €95.92—€299.75), and €183.50 for the TAU condition (SD = 77.52, range €71.94—€335.72).
Taking into account the model for the treatment cost measure, Table 4 and Fig. 3 show a significant interaction between Condition (UP) and Time (Time2, Time3, Time4, Time5) in all the time segments (b ranged from 68.58 to -21.76; t ranged from 12.81 to -4.06), pointing that, although the UP condition starts being more expensive than the TAU condition within the first months of treatment, at the end of both conditions (Time5), the TAU ends up being significantly more expensive than the UP.
Evolution of the cost over the course of treatment. Note: Model Estimates for Treatment cost as a function of Condition (TAU vs. UP) and Time (Time1 vs. Time2 vs. Time3 vs. Time4 vs. Time5). Error bars represent 95% CIs. Time1 = Pre treatment time, Time2: 3 months after treatment onset (coinciding with the end of the UP treatment condition); Time3: 6 months after treatment onset; Time4: 9 months after treatment onset; and Time5: 15 months after treatment onset, UP = Unified protocol, TAU = Treatment as usual
Discussion
The aim of this study was to analyze the cost-effectiveness associated with the application of two different psychological interventions for EDs in the Spanish public mental health system, the UP applied in group format compared to the TAU applied in individual face-to-face format. The hypothesis was that the UP would be more cost-effective than the TAU, that is, that it would be effective in reducing emotional symptomatology and that it would do so at a lower associated cost in comparison with the TAU. The results of this study have demonstrated it.
Summarizing the block for the effectiveness analyses, it can be concluded that, for Depression and Anxiety measures, the UP condition shows at least the same beneficial results for the participants than the TAU condition, and both interventions generate low discomfort in the patients who receive them. However, for the Quality of life outcome, the UP condition shows to be significantly more effective in comparison with the TAU condition. These results are similar to those found in other studies (Carlucci et al., 2021; Sakiris & Berle, 2019) and by our team (Osma et al., 2022). Finally, it was found that the variability due to the center did not modify the results obtained. Therefore, the possible variability in the application of the intervention by therapists did not influence the outcomes in each center.
Concerning the results of the cost-effectiveness block and regarding the number of sessions received, we found a large difference in the number of sessions received by each treatment condition, especially in the first 3 months of intervention. Participants in the UP condition received an average of 10 sessions, compared to 2 sessions in the TAU condition. This outcome was expected because we implemented the UP over 12 weekly 2-h sessions in group format, which allows clinicians to treat a greater number of patients at the same time and with greater frequency (Barlow et al., 2018).
If we consider the total number of sessions received over 15 months, we found that the UP had an average of 13 sessions, an average of 3 more sessions than those carried out during the first 3 months. This is mainly due to the design of the UP implementation, in which we can distinguish two phases. The first consists of the 12 treatment sessions in which the therapist explains and instructs patients in the training of adaptive emotional regulation skills. This phase takes place during the first three months of treatment. The number of sessions we applied is the same of those used in other studies that have adapted and applied the UP in group format (Bullis et al., 2015; de Ornelas Maia et al., 2015), although lower than the 14 sessions of the study of Laposa et al. (2017) or the 15 treatment sessions of Reinholt et al. (2017). The second part involves the patients' autonomous practice of the techniques and skills learned, with supervision through follow-up sessions at 3, 6, and 12 months post-treatment. This structure facilitated patients hardly requiring extra treatment sessions; in our study, only 17.7% required an average of 2 extra sessions in individual format.
In contrast, we find that, in the TAU condition, the number of sessions during the first 3 months of treatment is only about 2 sessions on average, which again highlights the difficulties and consequences of the situation in our national mental health system, which results in a shortage of resources, long waiting lists, and the frequency of sessions being greatly delayed over time (Díaz et al., 2017; Gabilondo et al., 2011). In fact, in this treatment condition, an average of one psychological treatment session is carried out approximately every month and a half. If we look at the total number of sessions received over the time period of 15 months, we found that, in the TAU condition, participants have received between 7 and 8 treatment sessions. This outcome is especially concerning if we consider the recommendations of the NICE guideline (National Collaborating Centre for Mental Health, 2011), who state that, for a psychological treatment to be effective, it should consist of approximately 8 sessions (depending on the disorder) and should be applied on a weekly basis. In this case, we find that these 8 sessions have taken place over 15 months, a period of time in which people have had to live with the discomfort generated by suffering from an ED (Bullis et al., 2019).
In addition, individuals with EDs often feel an impact on their work life, as can be seen in the study carried out by Salvador-Carulla et al. (2011) in Catalonia (Spain), where researchers found that the average number of days of sick leave for a person diagnosed with depression is 103.5 days. This also translates into an estimated productivity loss of €6,013 per person, with an estimated total productivity loss of 200 million euros per year as a result of work days lost due to temporary disability caused by depression (Salvador-Carulla et al., 2011). These outcomes highlight the urgent need to find new ways of applying cost-effective psychological evidence-based treatments in the SPMH to cover the great demands of society in relation to mental health care and will also lead to an improvement in factors related to work performance (Ihara et al., 2021; Mahmud et al., 2022).
The second result obtained in this study is related to reductions of medication burden over time in the UP condition. Several investigations have shown that with CBT-based interventions, the number of relapses in patients is reduced (van Dis et al., 2020), which could result, in the long term, in a lower need for pharmacological doses. It should be mentioned that this statistically significant reduction was only found in the UP condition. In this sense, it should be noted that many of the patients of the UP condition drastically decreased their emotional symptomatology in the first 3 months of treatment (corresponding to the 12 sessions of active treatment), as shown in the study carried out by our research team (Osma et al., 2022). However, some of the participants in the TAU condition continued to receive active treatment due to the presence of symptomatology throughout the 15-month time period of the study. This could explain why the pharmacological treatment was maintained in the TAU condition.
The final result obtained in this study is related to the cost of treatment sessions. Although the initial cost of the UP treatment is high (€122.27 per person, compared to €53.69 for the TAU condition), in the long term, individual face-to-face treatment is more expensive (€163.74 per person for the UP condition, compared to €183.50 for the TAU condition). This result shows that other forms of treatment, such a transdiagnostic group treatment, are possible to treat a greater number of people, in a shorter time, at a lower cost (Ruiz-Rodríguez et al., 2018), and ensuring its effectiveness (Osma et al., 2022). In addition, transdiagnostic treatments make it possible to reduce training costs for therapists, as they do not have to specialize in different protocols for each of the diagnoses (Wilamowska et al., 2010), and would reduce implementation and dissemination costs, since it is a structured and protocolized treatment (McHugh & Barlow, 2010). This would have benefits both in terms of people's health and in terms of public administrations' accounting.
Limitations
This study also has a number of limitations. The characteristics of the context where the study was carried out, that is, the Spanish mental health system, prevent us from generalizing the results to other contexts, such as the private sector or to public contexts in other countries that function differently from ours. Also, the characteristics of the context has made it difficult to collect a greater number of additional costs, for example indirect costs (days of sick leave, costs of other therapists, costs derived from the space where the intervention takes place, among others), that usually are mentioned in the literature and that allow to perform more specific analysis (e.g., quality-adjusted life years, Prieto and Sacristán (2003). Another limitation to take into account is that the sample of this study was selected from a larger sample of which the project is a part, depending on whether they had the necessary information to be able to carry out the cost-effective analyses needed for this study. This may result in a bias effect derived from the exclusion of the rest of the participants, then the results obtained in the present study should be interpreted with caution. The assessment of the degree of fidelity to the treatment is another limitation present in the study. Since this was a naturalistic setting, it was not possible to record the treatment sessions, so we could not guarantee that all the collaborating therapists in the study applied the treatment in the same way. However, all therapists in the UP condition were trained and supervised in order to ensure as much fidelity to the treatment as possible and it was found that the variability concerning the center did not modify the results obtained. Finally, this is a multicenter randomized control trial and we have chosen the financial information available only from the autonomous community which has provide the largest percentage of the sample, slight differences in the costs of psychological treatment sessions in both conditions could emerge if we consider the data of all autonomous communities represented.
Conclusions
In summary, the current situation of our national mental health system makes it necessary to search for more cost-effective psychological treatment formats. A possible solution to this problem could be a treatment based on the UP which, given its transdiagnostic nature, allows its application in group format, thus increasing the number of patients who can benefit from treatment at the same time, increasing the frequency of sessions and reducing waiting lists at a lower cost than individual treatment. This is the first study that has analyzed the cost-effectiveness of the UP when it is applied in a group format in a public mental health setting. The results of this study have contributed to increasing the information available on the efficacy of the UP for the reduction of depressive and anxious symptomatology and the increase in quality of life; as well as that, the group format has allowed the participants of the UP condition to receive a greater number of sessions, in a shorter period of time and with a lower economic cost per treatment session. We hope that future studies will explore the cost-effectiveness of this treatment in other contexts and in other countries, since the results of this study have shown that the UP is an efficient solution when applied in group format in specialized care that will improve the cost-effectiveness of our national mental health system.
Data availability statement
The datasets generated during and/or analyzed during the current study are available from the corresponding author on reasonable request.
References
American Psychiatric Association. (1994). Diagnostic and statistical manual of mental disorders. Author.
Barlow, D. H., Ellard, K. K., Fairholme, C. P., Farchione, T. J., Boisseau, C. L., Allen, L. B., & May, J. T. E. (2011a). Unified protocol for transdiagnostic treatment of emotional disorders Client workbook. Oxford University Press.
Barlow, D. H., Farchione, T. J., Fairholme, C. P., Ellard, K. K., Boisseau, C. L., Allen, L. B., & Ehrenreich-May, J. (2011b). The Unified Protocol for Transdiagnostic Treatment of Emotional Disorders: Therapist Guide. Oxford University Press.
Barlow, D. H., Farchione, T. J., Sauer-Zavala, S., Latin, H. M., Ellard, K. K., Bullis, J. R., Bentley, K. H., Boettcher, H. T., & Cassiello-Robbins, C. (2018). Unified protocol for transdiagnostic treatment of emotional disorders: Therapist guide (2nd ed.). Oxford University Press.
Barlow, D. H., Sauer-Zavala, S., Carl, J. R., Bullis, J. R., & Ellard, K. K. (2014). The nature, diagnosis, and treatment of neuroticism. Clinical Psychological Science, 2(3), 344–365. https://doi.org/10.1177/2167702613505532
Bates, D., Mächler, M., Bolker, B., & Walker, S. (2015). Fitting Linear Mixed-Effects Models Using using lme4. Journal of Statistical Software, 67(1). https://doi.org/10.18637/jss.v067.i01
Beck, A. T., & Steer, R. A. (1993). Beck Anxiety Inventory Manual (vol. 2). Psychological Corporation.
Beck, A. T., Steer, R. A., & Brown, G. K. (1996). BDI-II, Beck depression inventory: manual (2nd ed.). Psychological Corporation.
Botella, C., & Ballester, R. (1997). Trastorno de pánico, evaluación y tratamiento [Panic disorder, evaluation and treatment] (4ed., text). Martínez Roca.
Brown, T. A., & Barlow, D. H. (2009). A proposal for a dimensional classification system based on the shared features of the DSM-IV anxiety and mood disorders: Implications for assessment and treatment. Psychological Assessment, 21(3), 256–271. https://doi.org/10.1037/a0016608
Bryde Christensen, A., Pavlo, A. J., Davidson, L., Poulsen, S., Reinholt, N., Hvenegaard, M., Simonsen, E., & Arnfred, S. (2022). Does one treatment benefit all? Patients’ experiences of standardized group CBT for anxiety and depression. Current Psychology. https://doi.org/10.1007/s12144-022-02820-w
Bullis, J. R., Boettcher, H., Sauer-Zavala, S., & Barlow, D. H. (2019). What is an emotional disorder? A transdiagnostic mechanistic definition with implications for assessment, treatment, and prevention. Clinical Psychology: Science and Practice, 1–19. https://doi.org/10.1111/cpsp.12278
Bullis, J. R., Sauer-Zavala, S., Bentley, K. H., Thompson-Hollands, J., Carl, J. R., & Barlow, D. H. (2015). The unified protocol for transdiagnostic treatment of emotional disorders: Preliminary exploration of effectiveness for group delivery. Behavior Modification, 39(2), 295–321.
Carlucci, L., Saggino, A., & Balsamo, M. (2021). On the efficacy of the unified protocol for transdiagnostic treatment of emotional disorders: A systematic review and meta-analysis. Clinical Psychology Review, 87, 101999.
Conselleria de Sanitat Universal i Salut Pública (2021). Memòria de gestió de la Conselleria de Sanitat Universal i Salut Pública. Retrieved from: https://www.san.gva.es/conselleria-sanitat-universal-i-salut-publica/inicio. Accessed 30 Nov 2021.
de Ornelas Maia, A. C. C., Nardi, A. E., & Cardoso, A. (2015). The utilization of unified protocols in behavioral cognitive therapy in transdiagnostic group subjects: A clinical trial. Journal of Affective Disorders, 172, 179–183. https://doi.org/10.1016/j.jad.2014.09.023
DECRETO 38/2016, de 8 de abril, por el que se modifica el Decreto 137/2003, de 18 de julio, por el que se regula la jornada y horario de trabajo, permisos, licencias y vacaciones del personal al servicio de instituciones sanitarias de la Generalitat dependientes de la Conselleria de Sanitat. Diario oficial de la Generalitat Valenciana, 7760, de 14 de abril de 2016. https://dogv.gva.es/es/eli/es-vc/d/2016/04/08/38/
di Nardo, P. A., Brown, T. A., & Barlow, D. H. (1994). Anxiety Disorders Interview Schedule for DSM-IV: Lifetime Version (ADIS-IV-L). In Psychological Corporation.
Díaz, J., Díaz-de-Neira, M., Jarabo, A., Roig, P., & Román, P. (2017). Estudio de derivaciones de Atención Primaria a centros de Salud Mental en pacientes adultos en la Comunidad de Madrid. Clínica y Salud, 28(2), 65–70. https://doi.org/10.1016/j.clysa.2017.03.001
Estrela, M., Herdeiro, M. T., Ferreira, P. L., & Roque, F. (2020). The use of antidepressants, anxiolytics, sedatives and hypnotics in Europe: Focusing on mental health care in portugal and prescribing in older patients. International Journal of Environmental Research and Public Health, 17(22), 8612. https://doi.org/10.3390/ijerph17228612
Ferrans, C. E., & Powers, M. J. (1985). Quality of life index: Development and psychometric properties. Advances in Nursing Science, 8, 15–24.
Gabilondo, A., Rojas-Farreras, S., Rodráguez, A., Ferníndez, A., Pinto-Meza, A., Vilagut, G., Haro, J. M., & Alonso, J. (2011). Use of primary and specialized mental health care for a major depressive episode in Spain by ESEMeD respondents. Psychiatric Services, 62(2), 152–161. https://doi.org/10.1176/ps.62.2.pss6202_0152
Gustavsson, A., Svensson, M., Jacobi, F., Allgulander, C., Alonso, J., Beghi, E., Dodel, R., Ekman, M., Faravelli, C., Fratiglioni, L., Gannon, B., Jones, D. H., Jennum, P., Jordanova, A., Jönsson, L., Karampampa, K., Knapp, M., Kobelt, G., Kurth, T., …, & Olesen, J. (2011). Cost of disorders of the brain in Europe 2010. European Neuropsychopharmacology, 21(10), 718–779. https://doi.org/10.1016/j.euroneuro.2011.08.008
IBM Corp. (2019). IBM SPSS Statistics for Windows, Version 26.0. IBM Corp.
Ihara, Y., Kurosawa, T., Matsumoto, T., & Takizawa, R. (2021). The effectiveness of preventive group cognitive-behavioral interventions on enhancing work performance-related factors and mental health of workers: A systematic review. Current Psychology. https://doi.org/10.1007/s12144-021-01562-5
Instituto Nacional de Estadística (INE). (2020). Encuesta Europea de Salud en España (EESE). https://www.ine.es/dyngs/INEbase/es/operacion.htm?c=Estadistica_C&cid=1254736176784m&menu=resultados&idp=1254735573175.
Laposa, J. M., Mancuso, E., Abraham, G., & Loli-Dano, L. (2017). Unified protocol transdiagnostic treatment in group format: A preliminary investigation with anxious individuals. Behavior Modification, 41(2), 253–268. https://doi.org/10.1177/0145445516667664
Larsen, D. L., Attkisson, C. C., Hargreaves, W. A., & Nguyen, T. D. (1979). Assessment of client/patient satisfaction: Development of a general scale. Evaluation and Program Planning, 2(3), 197–207.
Mahmud, S., Mohsin, M., Dewan, Md. N., & Muyeed, A. (2022). The global prevalence of depression, anxiety, stress, and insomnia among general population during COVID-19 pandemic: A systematic review and meta-analysis. Trends in Psychology. https://doi.org/10.1007/s43076-021-00116-9
McHugh, R. K., & Barlow, D. H. (2010). The dissemination and implementation of evidence-based psychological treatments: A review of current efforts. American Psychologist, 65(2), 73–84. https://doi.org/10.1037/a0018121
Mezzich, J. E., Ruipérez, M. A., Pérez, C., Yoon, G., Liu, J., & Mahmud, S. (2000). The Spanish version of the quality of life index: Presentation and validation. Journal of Nervous and Mental Disease, 188(5), 301–305. https://doi.org/10.1097/00005053-200005000-00008
Ministry of Health, S. of S. for Health. G. of S. (2022). Estadística del Consumo Farmacéutico a través de Recetas Médicas del Sistema Nacional de Salud [Statistics on Pharmaceutical Consumption through Prescription Drugs in the National Health System].
National Collaborating Centre for Mental Health. (2011). Common mental health problems: Identification and pathways to care. RCPsych Publications.
National Statistics Institute (NSI). (2020). European Health Survey in Spain (EESE). Retrieved from: https://www.ine.es/dyngs/INEbase/es/operacion.htm?c=Estadistica_C&cid=1254736176784&menu=resultados&idp=1254735573175. Accessed 3 Nov 2021.
Newby, J. M., McKinnon, A., Kuyken, W., Gilbody, S., & Dalgleish, T. (2015). Systematic review and meta-analysis of transdiagnostic psychological treatments for anxiety and depressive disorders in adulthood. Clinical Psychology Review, 40, 91–110. https://doi.org/10.1016/j.cpr.2015.06.002
Norton, P. J. (2012). Group cognitive-behavioral therapy of anxiety: A transdiagnostic treatment manual. Guilford Press.
OECD/EU. (2018). Health at a glance: Europe 2018: State of health in the EU cycle. OECD. https://doi.org/10.1787/health_glance_eur-2018-en
Osma, J., Suso-Ribera, C., García-Palacios, A., Crespo-Delgado, E., Robert-Flor, C., Sánchez-Guerrero, A., Ferreres-Galán, V., Pérez-Ayerra, L., Malea-Fernández, A., & Torres-Alfosea, M. A. (2018). Efficacy of the unified protocol for the treatment of emotional disorders in the Spanish public mental health system using a group format: study protocol for a multicenter randomized non-inferiority controlled trial. Health and Quality of Life Outcomes, 16, 46. https://doi.org/10.1186/s12955-018-0866-2
Osma, J., Peris-Baquero, Ó., Suso-Ribera, C., Sauer-Zavala, S., & Barlow, D. H. (2021). Predicting and moderating the response to the unified protocol: Do baseline personality and affective profiles matter? Cognitive Therapy and Research, 45(4), 817–830. https://doi.org/10.1007/s10608-021-10208-6
Osma, J., Peris-Baquero, Ó., Suso-Ribera, C., Farchione, T. J., & Barlow, D. H. (2022). Effectiveness of the Unified Protocol for transdiagnostic treatment of emotional disorders in group format in Spain: Results from a randomized controlled trial with 6-months follow-up. Psychotherapy Research, 32(3), 329–342. https://doi.org/10.1080/10503307.2021.1939190
Osma, J., Suso-Ribera, C., Peris-Baquero, Ó., Gil-Lacruz, M., Pérez-Ayerra, L., Ferreres-Galan, V., Torres-Alfosea, M. Á., López-Escriche, M., & Domínguez, O. (2019). What format of treatment do patients with emotional disorders prefer and why? Implications for public mental health settings and policies. PLoS One, 14(6), e0218117. https://doi.org/10.1371/journal.pone.0218117
Prieto, L., & Sacristán, J. A. (2003). Problems and solutions in calculating quality-adjusted life years (QALYs). Health and Quality of Life Outcomes, 1(1), 80.
R Core Team. (2021). R: A language and environment for statistical computing. In R Foundation for Statistical Computing. R foundation for statistical computing Vienna, Austria.
Reinholt, N., Aharoni, R., Winding, C., Rosenberg, N., Rosenbaum, B., & Arnfred, S. (2017). Transdiagnostic group CBT for anxiety disorders: The unified protocol in mental health services. Cognitive Behaviour Therapy, 46(1), 29–43. https://doi.org/10.1080/16506073.2016.1227360
Ruiz-Rodríguez, P., Cano-Vindel, A., Muñoz-Navarro, R., Wood, C. M., Medrano, L. A., Moretti, L. S., Castillo, M. D. G., Tomás, P. T., Cabré, G. J., Moriana, J. A., Bonet, A. C., Pizà, M. R., Ramírez-Manent, I., Agüero, L., Rodríguez-Enríquez, M., Kvedaras, E. S., González, J. P., Schmitz, F., Maeso, C. A., …, Hidalgo, L. Y. (2018). Cost-effectiveness and cost-utility analysis of the treatment of emotional disorders in primary care: PsicAP clinical trial. Description of the sub-study design. Frontiers in Psychology, 9(MAR). https://doi.org/10.3389/fpsyg.2018.00281
Sackeim, H. A. (2001). The definition and meaning of treatment-resistant depression. Journal of Clinical Psychiatry, 62, 10–17.
Sakiris, N., & Berle, D. (2019). A systematic review and meta-analysis of the Unified Protocol as a transdiagnostic emotion regulation based intervention. Clinical Psychology Review, 72, 101751. https://doi.org/10.1016/j.cpr.2019.101751
Salvador-Carulla, L., Bendeck, M., Fernández, A., Alberti, C., Sabes-Figuera, R., Molina, C., & Knapp, M. (2011). Costs of depression in Catalonia (Spain). Journal of Affective Disorders, 132(1–2), 130–138. https://doi.org/10.1016/j.jad.2011.02.019
Sanz, J., García-Vera, M. P., & Fortún, M. (2012). The Beck Anxiety Inventory (BAI): Psychometric properties of the Spanish version in patients with psychological disorders. Behavioral Psychology/ Psicologia Conductual, 20(3), 563–583.
Sanz, J., Navarro, M. E., & Vázquez, C. (2003). Adaptación española del Inventario para la Depresión de Beck-II (BDI-II): 1. Propiedades psicométricas en estudiantes universitarios. Análisis y Modificación de Conducta, 29(124), 239–288.
Steele, S. J., Farchione, T. J., Cassiello-Robbins, C., Ametaj, A., Sbi, S., Sauer-Zavala, S., & Barlow, D. H. (2018). Efficacy of the Unified Protocol for transdiagnostic treatment of comorbid psychopathology accompanying emotional disorders compared to treatments targeting single disorders. Journal of Psychiatric Research, 104, 211–216. https://doi.org/10.1016/j.jpsychires.2018.08.005
van Dis, E. A. M., van Veen, S. C., Hagenaars, M. A., Batelaan, N. M., Bockting, C. L. H., van den Heuvel, R. M., Cuijpers, P., & Engelhard, I. M. (2020). Long-term outcomes of cognitive behavioral therapy for anxiety-related disorders. JAMA Psychiatry, 77(3), 265. https://doi.org/10.1001/jamapsychiatry.2019.3986
Vieta, E., Alonso, J., Pérez-Sola, V., Roca, M., Hernando, T., Sicras-Mainar, A., Sicras-Navarro, A., Herrera, B., & Gabilondo, A. (2021). Epidemiology and costs of depressive disorder in Spain: The EPICO study. European Neuropsychopharmacology, 50, 93–103. https://doi.org/10.1016/j.euroneuro.2021.04.022
Wilamowska, Z. A., Thompson-Hollands, J., Fairholme, C. P., Ellard, K. K., Farchione, T. J., & Barlow, D. H. (2010). Conceptual background, development, and preliminary data from the unified protocol for transdiagnostic treatment of emotional disorders. Depression and Anxiety, 27(10), 882–890. https://doi.org/10.1002/da.20735
World Health Organization. (2017). Depression and Other Common Mental Disorders: Global Health Estimates. World Health Organization. Retrieved from: https://apps.who.int/iris/handle/10665/254610. Accessed 30 Oct 2021.
Acknowledgements
We would like to thank all the participants, health professionals and collaborating centers that have made this study possible.
Funding
Open Access funding provided thanks to the CRUE-CSIC agreement with Springer Nature. This work was supported by Gobierno de Aragon and FEDER 2014–2020 “Construyendo Europa desde Aragon” [Grant Number Research team S31_20D]; Plan Estatal de I + D + I 2013–2016 and co-funded by the “ISCIII-Subdireccion General de Evaluacion y Fomento de la investigacion del Fondo Europeo de Desarrollo Regional (FEDER). Otra manera de hacer Europa” [Grant Number PI17/00320].
Author information
Authors and Affiliations
Contributions
All authors contributed to the study conception and design. Material preparation and data collection were performed by Óscar Peris-Baquero and Jorge Osma. Data analysis were performed by Óscar Peris-Baquero and José David Moreno. The first draft of the manuscript was written by Óscar Peris-Baquero and Jorge Osma, and all authors commented on previous versions of the manuscript. All authors read and approved the final manuscript.
Corresponding author
Ethics declarations
Ethics approval
This study was performed in line with the principles of the Declaration of Helsinki. Approval was granted by the Ethics Committee of all collaborating centers.
Consent to participate
Informed consent was obtained from all individual participants included in the study.
Competing interests
The authors have no financial or proprietary interests in any material discussed in this article.
Additional information
Publisher's note
Springer Nature remains neutral with regard to jurisdictional claims in published maps and institutional affiliations.
Supplementary Information
Below is the link to the electronic supplementary material.
Rights and permissions
Open Access This article is licensed under a Creative Commons Attribution 4.0 International License, which permits use, sharing, adaptation, distribution and reproduction in any medium or format, as long as you give appropriate credit to the original author(s) and the source, provide a link to the Creative Commons licence, and indicate if changes were made. The images or other third party material in this article are included in the article's Creative Commons licence, unless indicated otherwise in a credit line to the material. If material is not included in the article's Creative Commons licence and your intended use is not permitted by statutory regulation or exceeds the permitted use, you will need to obtain permission directly from the copyright holder. To view a copy of this licence, visit http://creativecommons.org/licenses/by/4.0/.
About this article
Cite this article
Peris-Baquero, Ó., Moreno, J.D. & Osma, J. Long-term cost-effectiveness of group unified protocol in the Spanish public mental health system. Curr Psychol 42, 22462–22477 (2023). https://doi.org/10.1007/s12144-022-03365-8
Accepted:
Published:
Issue Date:
DOI: https://doi.org/10.1007/s12144-022-03365-8