Abstract
Interoception, a multifaceted concept defined as the perception of internal bodily signals, is crucially involved in mental health in general and in emotion regulation in particular, being interoceptive sensibility (IS) one of the most studied interoceptive processes. The main objective of this study was to explore the relationships between IS and emotion regulation processes, analyzing the role of the eight IS dimensions assessed by the Multidimensional Assessment of Interoceptive Awareness-2 (MAIA-2) in alexithymia, emotion dysregulation, and depression. Additionally, this study also aimed to validate the MAIA-2 in a Spanish sample. To do so, 391 healthy adults, native Peninsular Spanish speakers (61.0% women, Mage = 29.00, SDage = 11.40), completed the MAIA-2 and other self-reported questionnaires to measure alexithymia, emotion dysregulation, and depressive symptoms. Results showed that lower scores on the IS dimensions that involve an accepting attitude toward the bodily signals (e.g., not-worrying) were related to alexithymia and emotion dysregulation, which, in turn, predicted depression. Moreover, the eight-factor structure of the MAIA-2 was confirmed with acceptable fit indices. This study highlights the multidimensional nature of the IS and the relevance of IS dimensions that involve a positive appraisal of the body in regulating emotions.
Similar content being viewed by others
Avoid common mistakes on your manuscript.
Interoception refers to the sense of internal (physiological) bodily signals (Craig, 2002), and it has been considered a multifaceted construct (Khalsa et al., 2018). Interoceptive awareness is the most widely studied set of interoceptive processes, and it is commonly referred to as “any (or all) of the different interoception features accessible to conscious self-report” (Khalsa et al., 2018). Different procedures have been used to assess this construct. Performance-based tasks, such as the Heartbeat Detection Task (Schandry, 1981), allow us to measure several interoceptive features, such as interoceptive accuracy (i.e., the ability to monitor internal bodily signals precisely) (Khalsa et al., 2018).
A more comprehensive conceptualization of the subjective interoceptive experience is provided by self-report instruments. Specifically, they capture aspects such as autobiographical memories of interoceptive states, judgments, beliefs, attitudes, thoughts, and feelings about the individual’s perception of interoceptive signals (Craig, 2002; Khalsa et al., 2018). These subjective aspects of interoceptive awareness are encompassed by the term “interoceptive sensibility” (IS) (Khalsa et al., 2018). One of the most widely used self-report questionnaires to measure IS is the “Multidimensional Assessment of Interoceptive Awareness” (MAIA) (Mehling et al., 2012), which includes several dimensions: (1) Noticing (i.e., the self-reported tendency to be aware of one’s body sensations, regardless of how comfortable or uncomfortable they are); (2) Not-Distracting (i.e., the tendency to not ignore pain or uncomfortable body sensations; (3) Not-Worrying (i.e., the tendency to not worry or feel distress about pain or uncomfortable sensations; (4) Attention Regulation (i.e., the ability to pay attention to bodily sensations; (5) Emotional Awareness (i.e., the extent to which emotional states are perceived as connected to bodily sensations; (6) Self-Regulation (i.e., the ability to use attention to bodily sensations -e.g., breathing- as a regulatory pathway of distress); (7) Body Listening (i.e., listening actively to the body for insight); and (8) Trusting (i.e., the extent to which the body is experienced as trustworthy).
An increasing body of research supports the relevance of interoception in mental health, showing strong associations with emotion regulation (Füstös et al., 2013), alexithymia (Trevisan et al., 2019), and, ultimately, psychopathology and mental disorders (Bonaz et al., 2021; Khalsa et al., 2018). Many emotion theories postulate a close association between interoception and the emotional experience. Specifically, in these theoretical frameworks, the perception of bodily signals is usually considered an underlying mechanism of the ability to recognize and regulate emotions (Damasio, 1994; Smith & Lane, 2015).
In this vein, the extended emotion regulation model by Gross (2015) considers the relevance of interoceptive awareness in the first stage of this process, that is, the identification of the emotion to be regulated (or not). Füstös et al. (2013) revealed that lower interoceptive accuracy was associated with less successful reappraisal in down-regulating negative affect. Moreover, deficits in IS have also been associated with difficulties in emotion regulation in several populations, such as obesity (Willem et al., 2019) and alcohol use disorder (Jakubczyk et al., 2020), as well as in healthy individuals (Zamariola et al., 2019).
Another emotional construct, alexithymia, has also been linked to IS. Alexithymia refers to difficulties in identifying and expressing feelings, and an externally oriented thinking style (Bagby et al., 1994). A recent meta-analysis by Trevisan et al. (2019) showed that alexithymia is associated with several interoceptive components, including IS. However, these authors found that the valence of this relationship differed depending on the specific interoceptive measures. For example, lower scores on the Noticing and Emotional Awareness subscales of the MAIA were associated with higher alexithymia. In contrast, studies that measured self-reported IS with the Body Perception Questionnaire (BPQ) (Porges, 1993) found positive associations with alexithymia (i.e., higher IS was related to higher alexithymia). Thus, the MAIA and the BPQ might reflect different interoceptive constructs (Trevisan et al., 2019). In this regard, Mehling (2016) proposed that the BPQ items represent an interoceptive style characterized by the awareness of bodily symptoms related to anxiety (e.g., hypochondria, somatization) rather than adaptive and healthy interoceptive skills, as intended by the MAIA. Although other dimensions of the MAIA were not included in the meta-analytic review by Trevisan et al. (2019), several studies have found negative relationships between all the MAIA dimensions and alexithymia in different samples (Brown et al., 2017; Zamariola et al., 2018).
Additionally, alexithymia and emotional regulation are related. Some authors have postulated that emotion labelling (an aspect included in the conceptualization of alexithymia) is an emotion regulatory strategy per se (Burklund et al., 2014). Furthermore, the Difficulties in Emotion Regulation Scale (DERS) (Gratz & Roemer, 2004), a widely used measure of emotion dysregulation, includes two dimensions that seem to overlap with the concept of alexithymia, namely, emotional awareness and emotional clarity. In contrast, other approaches view emotion recognition as the first step in regulating emotions. For instance, Izard et al. (2011) postulated that emotion recognition and emotion regulation are two consecutive steps in emotion processing. The Gross extended process model of emotion regulation (Gross, 2015) also identifies the detection and acknowledgement of emotions as the first of three consecutive stages: identification, selection of the regulatory strategy, and its implementation. Thus, alexithymia would represent a dispositional tendency to fail in the identification stage of the extended process model of emotion regulation, leading to low emotion regulation success (i.e., emotion dysregulation).
Given that there is empirical support for both premises, it is unclear whether alexithymia is a precursor or a marker of maladaptive emotional regulation. Although both alexithymia and difficulties in regulating emotions have been widely related to dysfunctional mental health outcomes such as depression (Joormann & Stanton, 2016; Li et al., 2015), their relationships with psychopathological symptoms have been examined separately.
Hence, based on the theoretical assumptions presented above, two different scenarios for the relationships between alexithymia, emotion dysregulation, and mental health can be proposed: 1) alexithymia and emotion dysregulation are two different (related) predictors of poorer mental health, such as depressive symptomatology; and 2) emotion dysregulation could mediate the relationship between alexithymia and depression. The empirical evidence in this regard is limited. There has only been one previous attempt to elucidate the mediating effect of emotion regulation between alexithymia and depressive symptoms (Van Beveren et al., 2018). Specifically, this study applied structural equation modelling analysis and found that the relationship between emotional awareness and depressive symptoms in youth was not direct; instead, it was mediated by the use of adaptive regulatory strategies. However, this indirect effect was not found for the use of maladaptive emotion regulation strategies. In this regard, it should be noted that the distinction between adaptive and maladaptive regulatory strategies has been widely criticized because successful emotion regulation does not only depend on the strategy used, but rather on the interaction between the strategy, the person, and the situation (Doré et al., 2016). Therefore, examining the ability to regulate emotions per se, independently of the strategy used, would help to better understand these associations.
All these findings seem to indicate that IS disturbances might be the initial variable in a whole cascade of variables that lead to depressive symptoms through alexithymia and emotional dysregulation. Although theories of embodied emotion and emotion regulation and the existing empirical research support this assumption, a comprehensive model that simultaneously includes all these psychological variables has not yet been empirically investigated.
The general aim of this study was to examine the relationships between IS and emotion regulation processes in healthy individuals. Based on the literature reviewed, the main objective was to test two models that include the eight IS dimensions of the MAIA-2, alexithymia, and emotion dysregulation in accounting for depressive symptoms. To do so, two hypothetical models are tested. The first model proposes that alexithymia and emotion dysregulation are mediators at the same level in the relationship between IS and depression, whereas the second model reflects the assumption that alexithymia is a precedent of emotion dysregulation.
Additionally, this study was aimed to adapt the MAIA-2 to Spanish and evaluate its psychometric properties. Although there is already a previous Spanish validation in the Chilean population (Valenzuela-Moguillansky & Reyes-Reyes, 2015), this instrument showed some limitations. Specifically, the Not-Worrying and Not-Distracting subscales have shown unsatisfactory internal consistency and estimation problems, similar to the original English form (Mehling et al., 2012). To overcome these limitations, Mehling et al. (2018) included five additional items in these two factors, thus creating the MAIA-2. However, this new version has not yet been validated in Spanish. In this regard, it was hypothesized that the eight-factor original model would show an adequate fit in the Spanish sample, and that dimensions of the Spanish MAIA-2 would show appropriate internal reliability.
Methods
Participants
A convenience sample consisting of native Spanish (Castilian) speakers over 18 years old was recruited using two different methods. First, the study was advertised on different social media, as well as on several bulletin boards in the Faculty of Psychology at the University of Valencia (Spain). A raffle for four gift cards worth 20 euros each was offered to encourage participation. Second, a polling company was hired to recruit additional participants. Individuals with a history of neurological disease or psychiatric disorders and those who were taking psychotropic drugs were excluded from participation.
A total of 530 individuals signed the informed consent and completed the screening questionnaire. Of them, 94 individuals were excluded for the following reasons: (1) 39 participants reported a history of mental disorder; (2) 32 participants were not native Spanish speakers; (3) 16 participants reported a history of neurological disease; and (4) seven participants reported taking psychotropic drugs. Additionally, 45 participants were also excluded due to giving wrong answers on the control items. Hence, the final sample included 391 participants (61.0% women; Mage = 29.00, SDage = 11.40). Demographic characteristics of the sample are shown in Table 1.
Measures
Interoceptive Sensibility (IS)
IS was assessed using a custom Spanish translation of the MAIA-2 (Mehling et al., 2018). Two authors (LD and MM, both native Spanish speakers and proficient in English) each carried out an initial independent translation based on the first Spanish translation of the original MAIA scale (Valenzuela-Moguillansky & Reyes-Reyes, 2015). The new items added with the MAIA-2 (i.e., items #8, #9, #10, #14, and #15) were also included in their translations. The two translations were compared, and minor discrepancies were identified and resolved by a short discussion. The version that was more comprehensible and closer to the original version was chosen. Specifically, only four of the 32 items included in the first Spanish version of the MAIA were slightly modified: items #5, #8, #11, and #18 (corresponding to items #5, #11, #16, and #23, according to the numbering of the 37-item MAIA-2 version). Finally, a native English-speaking bilingual translator performed the back-translation into English. No substantial differences between the new back-translated items of the MAIA-2 and those of the original English MAIA-2 were found. Any other discrepancies in other items were resolved with the insights provided by the first Spanish translation of the original MAIA (Valenzuela-Moguillansky & Reyes-Reyes, 2015). Therefore, the initial Spanish translation of the MAIA-2 was considered appropriate. As in the original version, the resulting translation of the MAIA-2 used in this study consisted of 37 items rated on a Likert scale, with values ranging from 0 (never) to 5 (always). The eight-factor structure showed appropriate fit indices in the original MAIA-2 (Mehling et al., 2018). Furthermore, six of the eight dimensions showed adequate internal consistency, ranging from α = .74 to α = .83. However, two dimensions (i.e., Noticing and Not-Worrying showed a questionable internal consistency (α = .64 and α = .67, respectively) (Mehling et al., 2018).
Alexithymia
Alexithymia was measured using the Toronto Alexithymia Scale-20 (TAS-20) (Bagby et al., 1994). The TAS-20 is a self-reported 20-item questionnaire consisting of three dimensions of alexithymia: Difficulties in Identifying Feelings (DIF) (7 items), Difficulties in Describing Feelings (DDF) (5 items), and Externally Oriented Thinking (EOT) (8 items). Items are scored on a 5-point Likert-type scale (1 = “strongly disagree”, 5 = “strongly agree”) according to the degree of agreement with each statement. DIF scores range from 7 to 35, DDF scores range from 5 to 25, and EOT scores range from 8 to 40. In addition, an overall score ranging from 20 to 100 can be computed. Higher scores indicate more severe alexithymia. In this study, internal consistency for the total scale was also considered appropriate (α = .85), as well as for DIF (α = .85) and DDF (α = .84). However, it was questionable for EOT (α = .64). These reliability coefficients are similar to those estimated in a recent meta-analysis that included 62 studies examining the factor structure of the TAS-20 (ωDIF = .84; ωDDF = .75; ωEOT = .62) (Schroeders et al., 2021).
Emotion Dysregulation
Emotion dysregulation was assessed using the Lack of Emotional Control subscale of the Spanish version of the Difficulties in Emotion Regulation Scale (DERS) (Gratz & Roemer, 2004; Hervás & Jódar, 2008). The Spanish DERS is composed of 28 items that measure the degree of difficulty in optimal emotion regulation, rated on a 5-point Likert scale (1 = “almost never / 0-10% of the time”; 5 = “almost always / 90-100% of the time”). Although the original English version showed a six-factor structure, five factors were found in the Spanish adaptation, namely: Lack of Emotional Awareness, Nonacceptance of Emotional Responses, Lack of Emotional Clarity, Difficulties Engaging in Goal-Directed Behavior, and Lack of Emotional Control. The latter refers to difficulties in controlling one’s behavior when experiencing negative emotions and the belief that little can be done to regulate emotions effectively when feeling upset. Lack of Emotional Control (9 items) includes items from two different factors from the original scale (impulse control difficulties and limited access to emotion regulation strategies) that were merged into a single factor in the Spanish validation (Hervás & Jódar, 2008). Scores for this factor range from 9 to 45. In this study, this dimension showed excellent internal consistency (α = .90), similar to what was found by Hervás and Jódar (2008) (α = .91).
Depressive Symptomatology
The presence of depressive symptoms was measured with the Beck Depression Inventory-II (BDI-II) (Beck et al., 1996). The BDI-II consists of 21 items rated on a 4-point Likert scale, ranging from 0 to 3. The total score ranges from 0 to 63. Scores from 14 to 19 indicate mild depression, scores from 20 to 28 indicate moderate depression, and scores from 29 to 63 indicate severe depression. Numerous studies have shown good psychometric properties of the BDI-II (e.g., Dozois et al., 1998; Osman et al., 1997), and English and Spanish BDI-II versions have presented high and comparable reliability and validity (Wiebe & Penley, 2005). In this sample, the internal consistency was adequate (α = .90).
Procedure
Participants were provided with a link to an online survey developed through an institutional application. The survey included different sections, which included a screening questionnaire that collected information about the eligibility criteria and sociodemographic data, the MAIA-2, the TAS-20, the DERS, and the BDI-II, in that order.
To ensure the quality of the participants’ responses, four control items (e.g., Please, if you are reading this, check option #2 for this item) were included throughout the survey to detect and exclude potential non-attentive respondents. Participants were excluded if they failed to answer all the control items correctly.
All the participants signed an online informed consent before being included in the study. The study was conducted following the principles stated in the Declaration of Helsinki. The Ethics Committee at the University of Valencia approved the study (register number: 1284353).
Statistical Analyses
First, descriptive analyses of all the demographic characteristics were computed. Second, we analyzed the psychometric properties of the Spanish adaptation of the MAIA-2. Descriptive statistics for all the MAIA-2 items, including means, standard deviations, 95% confidence intervals (CI), skewness, and kurtosis were calculated. To investigate the latent structure of the Spanish MAIA-2, we conducted a confirmatory factor analysis (CFA) with the well-known eight-factor structure of the MAIA-2 using the lavaan package (Rosseel, 2012). The model was estimated with Weighted Least Squares Mean and Variance corrected (WLSMV), given the ordered categorical nature of the items and the violation of multivariate normality (see Supplementary Material).
The goodness of fit between the model and the data was evaluated using the following conventional criteria for overall goodness-of-fit-indices: a) the Comparative Fit Index (CFI), with cut-off criteria ≥ .90 indicating good fit (≥ .95 indicating very good fit); b) the Tucker–Lewis index (TLI), with cut-off criteria ≥ .90 indicating good fit (≥ .95 indicating very good fit); c) the Root Mean Square Error of Approximation (RMSEA), with values ≤ .08 indicating good fit (≤ .05 indicates very good fit), as well as its 90% confidence interval (CI), ideally with the lower bound close to .00 and the upper bound not exceeding .10; and d) the Standardized Root Mean Square Residual (SRMR) ≤ .08, indicating that the model fits the data well.
Then, the internal consistency of the eight dimensions of the MAIA-2 was analyzed using Cronbach’s alpha (α) and McDonald’s omega (ω) coefficients with the semTools package (Jorgensen et al., 2021). In addition, item-total correlations for the Spanish MAIA-2 factors and if-item-deleted alphas were computed using the multilevel package (Bliese, 2016).
Finally, two structural equation models were tested using the lavaan package (Rosseel, 2012). The first model included a sequence in which the IS dimensions (MAIA-2) predicted both alexithymia (TAS-20 Total score) and emotion dysregulation (Lack of Emotional Control subscale of the DERS) entered as correlated, which in turn led to depressive symptoms (BDI-II) (Model 1). The second model included a sequence in which the IS dimensions predicted alexithymia, which in turn led to emotion dysregulation, and emotion dysregulation predicted depressive symptomatology (Model 2). All the variables were entered as manifest variables. Indirect effects were estimated, and the CIs around the estimated effects were computed using a bootstrap resampling method, given that it produces more accurate CIs than other methods (Mackinnon et al., 2007). The models were estimated using the robust maximum likelihood method (MLR). The criteria used to assess the goodness of fit were the χ2, the CFI, and the SRMR, with the same cut-off values as the ones used in the CFA described above. However, TLI and RMSEA were not considered because they are not recommended as fit indices for models with small degrees of freedom (Kenny et al., 2014; Shi et al., 2019). To control for the inflated probability of type I error, p values were adjusted with the stats package (R Core Team, 2016) using the false discovery rate method (Benjamini & Hochberg, 1995), as recommended by Cribbie (2007) for structural equation models.
Data management and statistical analyses were conducted using SPSS v.26 and R 4.1.1.
Results
Spanish Adaptation of the Multidimensional Assessment of Interoceptive Awareness-2
Descriptive statistics for all the items on the Spanish MAIA-2 are shown in Table S1. Skewness ranged from −1.00 to .35, and kurtosis ranged from 2.00 to 4.00. Fit indices for the CFA indicated an acceptable fit with the original eight-factor structure (Table 2).
Items, standardized factor loadings, and communalities of the Spanish MAIA-2 items are shown in Table 3. All item communalities had values above .30, except items #5 and #6, which showed very low communalities (.028 and .002, respectively). The standardized factor loadings of items #5 and #6 were also low (.169 and .041, respectively), whereas the standardized factor loadings of the rest of the items were above .40, ranging from .493 to .860. All the standardized factor loadings were significant (p < .001), except the one for item 5 (p < .493).
Table 4 shows means, standard deviations, internal consistency, ranges of item-total correlations, and correlations between the Spanish MAIA-2 dimensions. All Cronbach’s alphas and McDonald’s omega coefficients ranged between .68 and .87, which were similar or, in some cases, higher than reliability indices obtained by (Mehling et al., 2018) for the English MAIA-2. Internal consistency for the total scale was adequate (α = .87). All item-scale correlations were greater than .40, except for Not-Distracting, where item-scale correlations for items #5 and #6 were r = .13 and r = .05, respectively (Table S2). It should be noted that the if-item-deleted alpha for the Not-Distracting subscale increased if these items were deleted (after removing only item #5: α = .75; after removing only item #6: α = .79: after removing both items #5 and #6: α = .88). Moreover, modification indices showed cross-loadings of these items on the factor Noticing.
Interoceptive Awareness, Alexithymia, Emotion Dysregulation, and Depressive Symptomatology
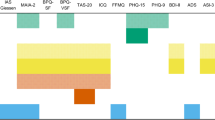
Pearson’s correlations between the IS dimensions, alexithymia, lack of emotional control, and depression are shown in Table S3. Based on theoretical assumptions, two hypothesized structural equation models were specified, tested, and evaluated (Models 1 and 2). Model 1 included a sequence that tested whether the IA dimensions of the MAIA-2 predicted depressive symptoms through the same-level mediating effects of alexithymia and emotion dysregulation, whereas in Model 2, alexithymia was entered as a predictor of emotion dysregulation. The standardized parameter estimates for Models 1 and 2 are shown in Fig. 1, except for covariances between the exogenous variables (i.e., the MAIA-2 dimensions), which are presented in Table S4.
Standardized coefficients of the hypothesized structural equation models 1 (a) and 2 (b). Standardized coefficients of the covariances between the exogenous variables have been omitted for clarity, but they are shown in Table S3. The squared multiple regression coefficients (R2) represent the amount of factor variance related to variance in its predictor variables. Continuous lines represent significant paths (p ≤ .05), whereas dashed lines represent non-significant paths (p > .05). *p ≤ .05, **p ≤ .01, ***p ≤ .001
Model 1
The overall fit indices for Model 1 indicated an adequate fit (Table 2). Alexithymia and emotion dysregulation, which were moderately and positively correlated, positively predicted higher scores on depression, explaining 31% of its variance.
Regarding relationships between the IS dimensions and alexithymia in Model 1, Not-Distracting, Not-Worrying, and Trusting were significant negative predictors (p ≤ .05), indicating that lower levels of these interoceptive dimensions were related to higher levels of alexithymia. Attention Regulation was a marginally significant negative predictor (p = .068). Moreover, alexithymia mediated the relationships between Not-Distracting (β = −.050, p = .003, 95% CI [−.083, −.017]), Not-Worrying (β = −.044, p = .004, 95% CI [−.074, −.014]), Attention Regulation (β = −.037, p = .043, 95% CI [−.073, −.001]), and Trusting (β = −.044, p = .020, 95% CI [−.080, −.007]), and depressive symptoms. In contrast, Noticing, Self-Regulation, and Body Listening did not show significant associations with alexithymia (p > .05) or statistically significant indirect effects on depressive symptomatology through alexithymia (Noticing: β = .009, p = .585, 95% CI [−.024, .042]; Emotional Awareness: β = −.020, p = .234, 95% CI [−.053, .013]; Self-Regulation: β = .014, p = .431, 95% CI [−.021, .048]; and Body Listening: β = −.019, p = .325, 95% CI [−.057, .019]). Overall, the IS dimensions of the MAIA-2 explained 15% of the variance in alexithymia.
Regarding the relationships between the IS dimensions and emotion dysregulation in Model 1, Not-Worrying, and Emotional Awareness were significant predictors. These two IS dimensions also showed indirect effects on depressive symptoms through emotion dysregulation (Not-Worrying: β = −.104, p < .001, 95% CI [−.150, −.059]; Emotional Awareness: β = .066, p = .011, 95% CI [.015, .117]). It should be noted that Emotional Awareness was positively associated with emotion dysregulation. No other MAIA-2 dimensions showed significant paths to emotion dysregulation (p > .05) or indirect effects on depressive symptomatology (Noticing: β = .028, p = .252, 95% CI [−.020, .077]; Not-Distracting: β = −.020, p = .330, 95% CI [−.061, .020]; Attention Regulation: β = −.033, p = .202, 95% CI [−.084, .018]; Self-Regulation: β = −.055, p = .070, 95% CI [−.115, .005]; Body Listening: β = .004, p = .894, 95% CI [−.051, .058], and Trusting: β = −.039, p = .126, 95% CI [−.089, .011]). The amount of variance explained by difficulties in emotion regulation was 17%.
Model 2
The overall fit indices for Model 2 indicated a substantially poorer fit than those for Model 1 (Table 2). According to this model, alexithymia led to emotion dysregulation, explaining 19% of the variance, which in turn led to higher depression, explaining 25% of the variance. Regarding the relationships between the IS dimensions and alexithymia in Model 2, similar to Model 1, Not-Distracting, Not-Worrying, Attention Regulation, and Trusting negatively predicted alexithymia, indicating that lower levels of these interoceptive dimensions were related to higher levels of alexithymia. Moreover, these interoceptive dimensions showed indirect effects on depressive symptoms through alexithymia and, subsequently, emotion dysregulation, in the expected direction (Not-Distracting: β = −.042, p = .002, 95% CI [−.068, −.015]; Not-Worrying: β = −.037, p = .010, 95% CI [−.065, −.009]; Attention Regulation: β = −.031, p = .040, 95% CI [−.061, −.001], and Trusting: β = −.037, p = .016, 95% CI [−.066, −.007]). In contrast, Noticing, Emotional Awareness, Self-Regulation, and Body Listening did not show significant associations with alexithymia (p > .05) or significant indirect effects (Noticing: β = .008, p = .589, 95% CI [−.020, .036]; Emotional Awareness: β = −.017, p = .240, 95% CI [−.045, .011]; Self-Regulation: β = .012, p = .419, 95% CI [−.017, .040]; Body Listening: β = −.016, p = .323, 95% CI [−.048, .016]). Overall, the IS dimensions of the MAIA-2 explained 15% of the variance in alexithymia.
Discussion
The current study aimed to test two alternative models in which lower scores on the IS dimensions of the MAIA-2 predict higher alexithymia and emotion dysregulation, which in turn lead to higher depressive symptomatology. Additionally, this study aimed to investigate the psychometric properties of the MAIA-2 in a Spanish sample. Following the order of the analyses, we start by discussing the results of the MAIA-2 validation, and then we discuss the results of the structural equation models.
The eight-factor structure of the original version of the MAIA (and MAIA-2) was confirmed by the results obtained from the CFA. Although the eight-factor model showed a good fit, items #5 and #6 (corresponding to the Not-Distracting factor) presented problematic factor loadings, and the if-deleted-alpha for Not-Distracting was higher than the internal consistency when including these items. Mehling et al. (2018) also found that item #5 showed the poorest factor loading, item-total correlation, and contribution to the internal consistency of the Not-Distracting subscale. Moreover, in the first Spanish version of the MAIA developed by Valenzuela-Moguillansky and Reyes-Reyes (2015), items #5 and #6 initially showed comprehension difficulties in cognitive debriefing interviews. After discussion with the first author of the original scale (Wolf Mehling), the authors reformulated item #5 to remove the negation, and item #6 was maintained. This is the way in which these items were included in the current Spanish version of the MAIA-2. It should be noted that these items (i.e., “Noto la tensión física o el malestar solamente cuando se vuelve más fuerte”[“I notice physical tension or discomfort only when they become more severe”], and “No me doy cuenta de las sensaciones de malestar”[“I do not realize the sensations of discomfort”]) might not accurately reflect the voluntary distractibility (and thus avoidance) component of bodily sensations of discomfort, unlike the rest of the items on the Not-Distracting subscale (e.g., “Intento ignorar el dolor” [“I try to ignore pain”]). Thus, these items could be more related to “noticing” the body sensations rather than to being distracted from them or not. This would explain why the modification indices suggested improving the goodness-of-fit by entering items #5 and #6 as indicators of the Noticing subscale. Future studies should reformulate these items to represent the Not-Distracting dimension more accurately. Despite this issue, we found acceptable reliability indices for almost all subscales (α ranging from .71 to .87), as well as for the total scale (α = .87). Indeed, this MAIA-2 Spanish version showed substantially higher reliability indices for the Not-Distracting and Not-Worrying subscales (α = .71 and α = .75, respectively) than the first Spanish version of the MAIA (α = .487 and α = .402, respectively). Therefore, the inclusion of the new items improved the psychometric properties of the questionnaire by increasing the reliability of both Not-Distracting and Not-Worrying, as occurred in the English version of the MAIA-2 (Mehling et al., 2018). However, the internal consistency for Noticing remained questionable (α = .68, ω = .68), similar to what was found in the original version (α = .69) by Mehling et al. (2012) and slightly higher than what was obtained by Valenzuela-Moguillansky and Reyes-Reyes (2015) in the first Spanish version of the MAIA (α = .64). Taking all of this into account, the Spanish adaptation of the MAIA-2 can be considered an appropriate measure to assess IS in the Spanish population.
Regarding the main objective of this study, the results showed that: (1) Not-Distracting, Not-Worrying, and Trusting negatively predicted alexithymia, and Attention Regulation showed a marginally significant tendency in this direction; (2) Not-Worrying and Trusting negatively predicted emotion dysregulation, whereas Emotional Awareness positively predicted emotion dysregulation; (3) all of these IS dimensions were indirectly related to depressive symptoms through the mediating effect of alexithymia and emotion dysregulation (considered same-level mediators, rather than consecutive), explaining 31% of the variance in depressive symptoms.
Therefore, not avoiding physical sensations and not worrying about them even if they are experienced as uncomfortable, as well as trusting the body and being able to voluntarily focus on bodily sensations, appeared to be adaptive for identifying emotions, leading to lower depressive symptomatology. Additionally, not worrying about bodily signals and trusting them appeared to underlie a higher ability to regulate negative emotions, also contributing to lower depression. These findings are consistent with previous research that reveals beneficial effects of mindfulness-based interventions on emotion processing (Wu et al., 2019) and depression (Goldberg et al., 2018). These interventions focus on paying attention to the present experience (even if it is not comfortable) and having a non-judgmental attitude, and these mindful components seem to permeate the IS dimensions with positive emotional correlates in this study, i.e., Not-Distracting, Not-Worrying, Attention Regulation, and Trusting.
Nevertheless, the Emotional Awareness subscale of the MAIA-2 performed in the opposite way to what was hypothesized: higher awareness of the link between body and emotions was related to a poorer emotion regulation outcome and, thus, higher depressive symptoms. In addition, Noticing and Body Listening, which involve the self-reported awareness of interoceptive signals and their emotional meaning, respectively, did not show significant relationships with alexithymia or difficulties in regulating emotions, contrary to our expectations. Similarly, the Self-Regulation subscale, which reflects the tendency to use attention towards one’s own body to regulate unpleasant emotions, was not a significant predictor of alexithymia or difficulties in emotion regulation.
These findings suggest that an accurate perception of the internal bodily signals might be necessary but not sufficient for awareness of the emotional experience and the deployment of an adaptive emotion regulation process, as found in previous literature (Lane & Schwartz, 1987; Mcrae & Gross, 2020). Specifically, our results indicate that what people do with interoceptive cues (i.e., how they interpret and manage them), rather than the self-perceived tendency to feel or not feel bodily sensations, plays a crucial role in emotional processing and psychopathology. This is consistent with approaches that suggest the existence of maladaptive and adaptive forms of IS. Maladaptive IS would be characterized by catastrophizing and hypervigilance of the body, whereas adaptive IS would be characterized by acceptance and attention regulation, respecting bodily sensations, as highlighted in mindfulness practices (Mehling, 2016).
Therefore, the multidimensional construct of interoception involves not only the perception of bodily states, but also their evaluative interpretation or appraisal (Farb et al., 2015; Mehling, 2016). Although the MAIA was initially designed to assess a healthy attentional style towards the body (Mehling, 2016), not all the MAIA dimensions include explicit notions of this adaptive appraisal of bodily signals because some are largely neutral (e.g., Noticing, Emotional Awareness). In this regard, the findings about the role of Not-Worrying and Trusting in both alexithymia and emotion dysregulation highlight the relevance of non-judgmental, accepting attitudes towards bodily sensations for healthy emotional functioning, rather than the extent to which internal cues are subjectively perceived (e.g., Noticing, Emotional Awareness, Body Listening).
It should be noted that self-reported perceptions of one’s interoceptive abilities (as captured by Noticing and Body Listening) do not necessarily match performance-based interoceptive abilities such as interoceptive accuracy (Schandry, 1981). Indeed, they are widely considered different features that might not correlate with each other (Khalsa et al., 2018). In addition, they can also relate differently to other emotional processes such as alexithymia (Trevisan et al., 2019). As mentioned above, (Trevisan et al., 2019) found that the interoceptive components and the methods used to measure IS strongly influenced the strength and directionality of the relationship between interoception and IS and alexithymia. Therefore, future studies should incorporate a comprehensive, multidimensional measurement of interoception by including both self-reported and behavioral instruments to disentangle the role of each interoceptive component in the processes of awareness and regulation of emotions.
This study initially supports the theories of embodied emotion that highlight the role of body awareness in emotional processes, namely, alexithymia, emotion dysregulation, and depressive symptoms. However, our findings extend these approaches by highlighting the role of evaluative appraisals of bodily signals, beyond the perception of the body state per se. According to our results, the interoceptive dimensions that are embedded in adaptive interpretations of the sensations felt in the body seem to trigger alexithymia and, partially, emotional dysregulation, leading to increased depressive symptomatology. Furthermore, our findings suggest that alexithymia is a predictor of depressive symptoms at the same level as difficulties in regulating one’s emotions, rather than a precedent for this dysregulation, which is consistent with findings from neuroimaging studies showing their common neural networks (Burklund et al., 2014). However, these results should be considered carefully due to the cross-sectional nature of this study. In addition, this study supports the multidimensionality not only of the interoception construct in general, but also, and especially, of IS in particular.
Finally, we must emphasize that the role of other variables cannot be ruled out because they could be modulating the relationships between interoceptive and emotional processes. For example, (Pollatos et al., 2009) found that anxiety moderated the relationship between interoceptive accuracy and depression. Their results showed that in individuals with high anxiety, there was a negative correlation between interoceptive accuracy and depression, whereas this association became non-significant and positive at low anxiety levels. Therefore, further studies are needed to fill the current gaps in our knowledge about the interoceptive system and disentangle its functions, including those involved in the emotional experience (Quigley et al., 2021).
This study might also have clinical implications, given that the findings suggest that manipulating interoceptive processing could modify a sequence through which higher awareness of one’s own emotions and more successful emotion regulation flow into decreased depressive symptoms. Several interoceptive interventions have been proposed, such as mindfulness, neural stimulation (e.g., vagus nerve stimulation, transcranial direct current stimulation), and pharmacological interventions (e.g., blockade of the ghrelin receptor) (Weng et al., 2021). Moreover, other embodiment techniques, such as manipulating the body posture, seem to enhance interoceptive accuracy on the Heartbeat Detection Task (Weineck et al., 2020). However, no empirical research has explored its effects on different aspects of IS measured with the MAIA. Given the specific IS dimensions that have been linked to positive emotional outcomes in the current study, mindfulness-based interventions seem to be especially promising for this purpose. Although some studies have explored the positive effects of mindfulness-based interventions on IS (Fissler et al., 2016), none have explored whether this enhancement of interoception is the mechanism that leads to improving emotional skills typically associated with mindfulness practices. Future research should confirm these assumptions.
The present study has some limitations that should be mentioned. First, it was conducted with a non-clinical sample, which limits the generalization of these results to clinical populations. Therefore, more research is needed to replicate these findings in clinically depressed individuals and other clinical populations with alexithymia and difficulties in regulating their emotions, such as patients with borderline personality disorder and brain damage. Second, this study included only a multifaceted approach to IS, but no performance-based interoceptive facets were considered. As previously mentioned, studies investigating the relationships between interoception and emotional skills should consider both self-reported and behavioral measurements of interoceptive awareness. Finally, this study included a cross-sectional design, and so no causal or temporal relationships can be established. Future research should implement experimental and longitudinal designs to provide stronger empirical support for the relationships hypothesized in embodiment and emotion regulation theoretical frameworks.
Conclusions
This study shows that: (1) the Spanish version of the MAIA-2 is an adequate tool to measure IS in Spanish individuals and (2) not ignoring uncomfortable sensations and not worrying about them, as well as trusting one’s bodily signals and being able to voluntarily focus on them, seem to be key interoceptive processes in recognizing emotions (i.e., low alexithymia), leading to lower depressive symptomatology. Furthermore, not worrying and trusting the body were also related to a higher ability to regulate emotions, which also contributed to lower depression. These findings highlight the relevance of the way bodily sensations are appraised in the emotional experience of healthy individuals.
Data Availability
The dataset generated and analyzed is available at the Open Science Framework repository: https://osf.io/cqfek/
References
Bagby, R. M., Parker, J. D. A., & Taylor, G. J. (1994). The twenty-item Toronto alexithymia scale-I. item selection and cross-validation of the factor structure. Journal of Psychosomatic Research, 38(1), 23–32. https://doi.org/10.1016/0022-3999(94)90005-1
Beck, A. T., Steer, R. A., & Brown, G. K. (1996). Beck depression inventory manual. The Psychological Corporation.
Benjamini, Y., & Hochberg, Y. (1995). Controlling the false discovery rate: A practical and powerful approach to multiple testing. Journal of the Royal Statistical Society: Series B (Methodological), 57, 289–300. https://doi.org/10.1111/J.2517-6161.1995.TB02031.X
Bliese, P. (2016). Package “multilevel”: Multilevel functions (Version 2.7). https://CRAN.R-project.org/package=multilevel
Bonaz, B., Lane, R. D., Oshinsky, M. L., Kenny, P. J., Sinha, R., Mayer, E. A., & Critchley, H. D. (2021). Diseases, disorders, and comorbidities of interoception. Trends in Neurosciences, 44(1), 39–51. https://doi.org/10.1016/J.TINS.2020.09.009
Brown, T. A., Berner, L. A., Jones, M. D., Reilly, E. E., Cusack, A., Anderson, L. K., Kaye, W. H., & Wierenga, C. E. (2017). Psychometric evaluation and norms for the multidimensional assessment of interoceptive awareness (MAIA) in a clinical eating disorders sample. European Eating Disorders Review, 25(5), 411–416. https://doi.org/10.1002/ERV.2532
Burklund, L. J., Creswell, J. D., Irwin, M., & Lieberman, M. (2014). The common and distinct neural bases of affect labeling and reappraisal in healthy adults. Frontiers in Psychology, 5(221). https://doi.org/10.3389/FPSYG.2014.00221
Craig, A. D. (2002). How do you feel? Interoception: The sense of the physiological condition of the body. Nature Reviews Neuroscience, 3(8), 655–666. https://doi.org/10.1038/nrn894
Cribbie, R. A. (2007). Multiplicity control in structural equation modeling. Structural Equation Modeling: A Multidisciplinary Journal, 14(1), 98–112. https://doi.org/10.1080/10705510709336738
Damasio, A. (1994). Descartes’s error: Emotion, rationality and the human brain. G. P. Putnam.
Doré, B. P., Silvers, J. A., & Ochsner, K. N. (2016). Toward a personalized science of emotion regulation. Social and Personality Psychology Compass, 10(4), 187. https://doi.org/10.1111/SPC3.12240
Dozois, D. J. A., Dobson, K. S., & Ahnberg, J. L. (1998). A psychometric evaluation of the Beck depression inventory-II. Psychological Assessment, 10(2), 83–89. https://doi.org/10.1037/1040-3590.10.2.83
Farb, N., Daubenmier, J., Price, C. J., Gard, T., Kerr, C., Dunn, B. D., Klein, A. C., Paulus, M. P., & Mehling, W. E. (2015). Interoception, contemplative practice, and health. Frontiers in Psychology, 6, 763. https://doi.org/10.3389/fpsyg.2015.00763
Fissler, M., Winnebeck, E., Schroeter, T., Gummersbach, M., Huntenburg, J. M., Gaertner, M., & Barnhofer, T. (2016). An investigation of the effects of brief mindfulness training on self-reported interoceptive awareness, the ability to decenter, and their role in the reduction of depressive symptoms. Mindfulness, 7(5), 1170–1181. https://doi.org/10.1007/s12671-016-0559-z
Füstös, J., Gramann, K., Herbert, B. M., & Pollatos, O. (2013). On the embodiment of emotion regulation: Interoceptive awareness facilitates reappraisal. Social Cognitive and Affective Neuroscience, 8(8), 911–917. https://doi.org/10.1093/scan/nss089
Goldberg, S. B., Tucker, R. P., Greene, P. A., Davidson, R. J., Wampold, B. E., Kearney, D. J., & Simpson, T. L. (2018). Mindfulness-based interventions for psychiatric disorders: A systematic review and meta-analysis. Clinical Psychology Review, 59, 52–60. https://doi.org/10.1016/J.CPR.2017.10.011
Gratz, K. L., & Roemer, L. (2004). Multidimensional assessment of emotion regulation and dysregulation: Development, factor structure, and initial validation of the difficulties in emotion regulation scale. Journal of Psychopathology and Behavioral Assessment, 26(1), 41–54. https://doi.org/10.1023/B:JOBA.0000007455.08539.94
Gross, J. J. (2015). Emotion regulation: Current status and future prospects. Psychological Inquiry, 26(1), 1–26. https://doi.org/10.1080/1047840X.2014.940781
Hervás, G., & Jódar, R. (2008). The Spanish version of the difficulties in emotion regulation scale. Clínica y Salud, 19(2), 139–156.
Izard, C. E., Woodburn, E. M., Finlon, K. J., Krauthamer-Ewing, E. S., Grossman, S. R., & Seidenfeld, A. (2011). Emotion knowledge, emotion utilization, and emotion regulation. Emotion Review, 3(1), 44–52. https://doi.org/10.1177/1754073910380972
Jakubczyk, A., Trucco, E. M., Klimkiewicz, A., Skrzeszewski, J., Suszek, H., Zaorska, J., Nowakowska, M., Michalska, A., Wojnar, M., & Kopera, M. (2020). Association between interoception and emotion regulation in individuals with alcohol use disorder. Frontiers in Psychiatry, 10, 1028. https://doi.org/10.3389/FPSYT.2019.01028/BIBTEX
Joormann, J., & Stanton, C. H. (2016). Examining emotion regulation in depression: A review and future directions. Behaviour Research and Therapy, 86, 35–49. https://doi.org/10.1016/J.BRAT.2016.07.007
Jorgensen, T. D., Pornprasertmanit, S., Miller, P., Schoemann, A., & Rosseel, Y. (2021). Package “semTools”. Useful tools for structural equation modeling (Version 0.5-5). https://CRAN.R-project.org/package=semTools
Kenny, D. A., Kaniskan, B., & McCoach, D. B. (2014). The performance of RMSEA in models with small degrees of freedom. Sociological Methods & Research, 44(3), 486–507. https://doi.org/10.1177/0049124114543236
Khalsa, S. S., Adolphs, R., Cameron, O. G., Critchley, H. D., Davenport, P. W., Feinstein, J. S., Feusner, J. D., Garfinkel, S. N., Lane, R. D., Mehling, W. E., Meuret, A. E., Nemeroff, C. B., Oppenheimer, S., Petzschner, F. H., Pollatos, O., Rhudy, J. L., Schramm, L. P., Simmons, W. K., Stein, M. B., et al. (2018). Interoception and mental health: A roadmap. Biological Psychiatry: Cognitive Neuroscience and Neuroimaging, 3(6), 501–513. https://doi.org/10.1016/j.bpsc.2017.12.004
Lane, R. D., & Schwartz, G. E. (1987). Levels of emotional awareness: A cognitive-developmental theory and its application to psychopathology. The American Journal of Psychiatry, 144(2), 133–143. https://doi.org/10.1176/AJP.144.2.133
Li, S., Zhang, B., Guo, Y., & Zhang, J. (2015). The association between alexithymia as assessed by the 20-item Toronto alexithymia scale and depression: A meta-analysis. Psychiatry Research, 227(1), 1–9. https://doi.org/10.1016/j.psychres.2015.02.006
Mackinnon, D. P., Fairchild, A. J., & Fritz, M. S. (2007). Mediation analysis. Annual Review of Psychology, 58, 593–614. https://doi.org/10.1146/annurev.psych.58.110405.085542
Mcrae, K., & Gross, J. J. (2020). Emotion regulation. Emotion, 20(1), 1–9. https://doi.org/10.1037/emo0000703
Mehling, W. (2016). Differentiating attention styles and regulatory aspects of self-reported interoceptive sensibility. Philosophical transactions of the Royal Society of London. Series B, Biological Sciences, 371(1708), 20160013. https://doi.org/10.1098/RSTB.2016.0013
Mehling, W. E., Price, C., Daubenmier, J. J., Acree, M., Bartmess, E., & Stewart, A. (2012). The multidimensional assessment of interoceptive awareness (MAIA). PLoS One, 7(11), e48230. https://doi.org/10.1371/journal.pone.0048230
Mehling, W. E., Acree, M., Stewart, A., Silas, J., & Jones, A. (2018). The multidimensional assessment of interoceptive awareness, version 2 (MAIA-2). PLoS One, 13(12). https://doi.org/10.1371/journal.pone.0208034
Osman, A., Downs, W. R., Barrios, F. X., Kopper, B. A., Gutierrez, P. M., & Chiros, C. E. (1997). Factor structure and psychometric characteristics of the beck depression inventory-II. Journal of Psychopathology and Behavioral Assessment 1997 19:4, 19(4), 359–376. https://doi.org/10.1007/BF02229026
Pollatos, O., Traut-Mattausch, E., & Schandry, R. (2009). Differential effects of anxiety and depression on interoceptive accuracy. Depression and Anxiety, 26(2), 167–173. https://doi.org/10.1002/DA.20504/
Porges, S. (1993). Body Perception Questionnaire. In stephenporges.com. Department of Psychology, University of Maryland.
Quigley, K. S., Kanoski, S., Grill, W. M., Barrett, L. F., & Tsakiris, M. (2021). Functions of interoception: From energy regulation to experience of the self. Trends in Neurosciences, 44(1), 29–38. https://doi.org/10.1016/J.TINS.2020.09.008
R Core Team. (2016). Package “stats” (Version 4.3.0). https://stat.ethz.ch/R-manual/R-devel/library/stats/html/00Index.html
Rosseel, Y. (2012). Lavaan: An R package for structural equation modeling. Journal of Statistical Software, 48(2), 1–36. https://doi.org/10.18637/jss.v048.i02
Schandry, R. (1981). Heart beat perception and emotional experience. Psychophysiology, 18(4), 483–488. https://doi.org/10.1111/j.1469-8986.1981.tb02486.x
Schroeders, U., Kubera, F., & Gnambs, T. (2021). The structure of the Toronto Alexithymia Scale (TAS-20): A meta-analytic confirmatory factor analysis: Assessment. https://doi.org/10.1177/10731911211033894.
Shi, D., Lee, T., & Maydeu-Olivares, A. (2019). Understanding the model size effect on SEM fit indices. Educational and Psychological Measurement, 79(2), 310–334. https://doi.org/10.1177/0013164418783530
Smith, R., & Lane, R. D. (2015). The neural basis of one’s own conscious and unconscious emotional states. Neuroscience and Biobehavioral Reviews, 57, 1–29. https://doi.org/10.1016/j.neubiorev.2015.08.003
Trevisan, D. A., Altschuler, M. R., Bagdasarov, A., Carlos, C., Duan, S., Hamo, E., Kala, S., McNair, M. L., Parker, T., Stahl, D., Winkelman, T., Zhou, M., & McPartland, J. C. (2019). A meta-analysis on the relationship between interoceptive awareness and alexithymia: Distinguishing interoceptive accuracy and sensibility. Journal of Abnormal Psychology, 128(8), 765–776. https://doi.org/10.1037/abn0000454
Valenzuela-Moguillansky, C., & Reyes-Reyes, A. (2015). Psychometric properties of the multidimensional assessment of interoceptive awareness (MAIA) in a Chilean population. Frontiers in Psychology, 6, 120. https://doi.org/10.3389/FPSYG.2015.00120/FULL
Van Beveren, M.-L., Goossens, L., Volkaert, B., Grassmann, C., Wante, L., Vandeweghe, L., Verbeken, S., & Braet, C. (2018). How do I feel right now? Emotional awareness, emotion regulation, and depressive symptoms in youth. European Child & Adolescent Psychiatry, 28(3), 389–398. https://doi.org/10.1007/S00787-018-1203-3
Weineck, F., Schultchen, D., Hauke, G., Messner, M., & Pollatos, O. (2020). Using bodily postures to reduce anxiety and improve interoception: A comparison between powerful and neutral poses. PLoS One, 15(12), e0242578. https://doi.org/10.1371/JOURNAL.PONE.0242578
Weng, H. Y., Feldman, J. L., Leggio, L., Napadow, V., Park, J., & Price, C. J. (2021). Interventions and manipulations of interoception. Trends in Neurosciences, 44(1), 52–62. https://doi.org/10.1016/J.TINS.2020.09.010
Wiebe, J. S., & Penley, J. A. (2005). A psychometric comparison of the Beck depression inventory - II in English and Spanish. Psychological Assessment, 17(4), 481–485. https://doi.org/10.1037/1040-3590.17.4.481
Willem, C., Gandolphe, M. C., Roussel, M., Verkindt, H., Pattou, F., & Nandrino, J. L. (2019). Difficulties in emotion regulation and deficits in interoceptive awareness in moderate and severe obesity. Eating and Weight Disorders, 24(4), 633–644. https://doi.org/10.1007/S40519-019-00738-0/TABLES/2
Wu, R., Liu, L. L., Zhu, H., Su, W. J., Cao, Z. Y., Zhong, S. Y., Liu, X. H., & Jiang, C. L. (2019). Brief mindfulness meditation improves emotion processing. Frontiers in Neuroscience, 13, 1074. https://doi.org/10.3389/FNINS.2019.01074
Zamariola, G., Vlemincx, E., Luminet, O., & Corneille, O. (2018). Relationship between interoceptive accuracy, interoceptive sensibility, and alexithymia. Personality and Individual Differences, 125, 14–20. https://doi.org/10.1016/j.paid.2017.12.024
Zamariola, G., Frost, N., Van Oost, A., Corneille, O., & Luminet, O. (2019). Relationship between interoception and emotion regulation: New evidence from mixed methods. Journal of Affective Disorders, 246, 480–485. https://doi.org/10.1016/J.JAD.2018.12.101
Acknowledgements
We would like to thank CIBERObn, an initiative of the Instituto de Salud Carlos III (ISC III CB06 03/0052).
Funding
Open Access funding provided thanks to the CRUE-CSIC agreement with Springer Nature. This work was supported by Excellence Research Program PROMETEO (PROMETEO/2018/110, Conselleria d’Educació, Investigació, Cultura I Esport, Generalitat Valenciana). LD is supported by a grant FPU18/01690 funded by Ministerio de Ciencia e Innovación/Agencia Estatal de Investigación/10.13039/501100011033 and by “European Social Fund - Investing in your future”. The funding sources were not involved in the study design, in the collection, analysis and interpretation of data, in the writing of the report, or in the decision to submit the article for publication.
Author information
Authors and Affiliations
Contributions
Conceptualization: Lorena Desdentado, Marta Miragall, Roberto Llorens, and Rosa M. Baños; Data curation: Lorena Desdentado and Marta Miragall; Formal Analysis: Lorena Desdentado and Marta Miragall; Funding acquisition: Rosa M. Baños; Investigation: Lorena Desdentado; Methodology: Lorena Desdentado, Marta Miragall, Roberto Llorens, and Rosa M. Baños; Project administration: Rosa M. Baños; Resources: Rosa M. Baños; Supervision: Marta Miragall, Roberto Llorens, and Rosa M. Baños; Validation: Lorena Desdentado, Marta Miragall, Roberto Llorens, and Rosa M. Baños; Visualization: Lorena Desdentado and Marta Miragall; Writing – original draft: Lorena Desdentado; Writing – review & editing: Lorena Desdentado, Marta Miragall, Roberto Llorens, and Rosa M. Baños.
Corresponding author
Ethics declarations
Ethical Approval
This study was performed in accordance with the ethical standards of the 1964 Declaration of Helsinki and was approved by the Ethics Committee of the University of Valencia (register number: 1284353).
Consent to Participate
All participants provided informed consent to participate in this study.
Conflict of Interest
The authors report no conflicts of interest.
Additional information
Publisher’s note
Springer Nature remains neutral with regard to jurisdictional claims in published maps and institutional affiliations.
Supplementary Information
ESM 1
(43.4 KB (44,522 bytes))
Rights and permissions
Open Access This article is licensed under a Creative Commons Attribution 4.0 International License, which permits use, sharing, adaptation, distribution and reproduction in any medium or format, as long as you give appropriate credit to the original author(s) and the source, provide a link to the Creative Commons licence, and indicate if changes were made. The images or other third party material in this article are included in the article's Creative Commons licence, unless indicated otherwise in a credit line to the material. If material is not included in the article's Creative Commons licence and your intended use is not permitted by statutory regulation or exceeds the permitted use, you will need to obtain permission directly from the copyright holder. To view a copy of this licence, visit http://creativecommons.org/licenses/by/4.0/.
About this article
Cite this article
Desdentado, L., Miragall, M., Llorens, R. et al. Disentangling the role of interoceptive sensibility in alexithymia, emotion dysregulation, and depression in healthy individuals. Curr Psychol 42, 20570–20582 (2023). https://doi.org/10.1007/s12144-022-03153-4
Accepted:
Published:
Issue Date:
DOI: https://doi.org/10.1007/s12144-022-03153-4