Abstract
Before herd immunity is reached, preventive practices still play an important role in controlling the COVID-19 pandemic. Adherence to preventive behaviors could be determined by individuals’ health beliefs, which would be influenced by antecedent factors such as previous exposure to pandemic stressors. Applying the health belief model (HBM), this study aims to examine the mediation association among COVID-19 stressors, HBM constructs, and preventive behaviors. Longitudinal data were collected from 1225 Chinese college students using web-based surveys at wave 1 (w1; between January 31 and February 11, 2020) and wave 2 (w2; between March 20 and April 3, 2020). Participants reported their COVID-19 stressors (w1), five HBM constructs (w2), and preventive behaviors (w1 and w2). Paired t-tests suggested that social distancing and self-quarantine behaviors decreased while precautionary behaviors increased from w1 to w2. Path analysis indicated that two HBM constructs (perceived barriers and self-efficacy) mediated the association between COVID-19 stressors and precautionary behaviors. These findings suggested that tailored prevention intervention for college students should attend to perceived barriers and self-efficacy. Individuals who exposed to multiple pandemic stressors merit particular attention and intervention should account for their early pandemic stress experiences.
Similar content being viewed by others
Avoid common mistakes on your manuscript.
Introduction
Preventive Practices in Controlling the COVID-19 Pandemic in China
Since the first case was reported in December 2019, the world has been suffering from the coronavirus disease 2019 (COVID-19) pandemic which has developed to a critical public health crisis (International Society for Infectious Diseases, 2020). COVID-19 is caused by severe acute respiratory syndrome coronavirus 2 (SARS-CoV-2), and individuals infected by the virus would experience various symptoms, such as fever, cough, fatigue, loss of taste or smell, and Diarrhea, which could be acute or persistent (Carfì et al., 2020). As of April 20, 2021, COVID-19 has led to global death tolls of 3,044,801 (Johns Hopkins University and Medicine, 2021), and the global number of new COVID-19 cases has continued to rise (World Health Organization, 2020). In addition to the influences on physical health, the pandemic has had detrimental impacts on economy, such as massive medical costs and high unemployment rates (Bartsch et al., 2020; Coibion et al., 2020). In response to this emergent public health crisis, Chinese government rapidly enforced numerous nationwide restrictions (e.g., city lockdown, school closure, and controls of cross-province travels) during January to February 2020 (China National Health Commission [CNHC], 2020a; Xinhua, 2020). In the individual level, several preventive behaviors including quarantine (e.g., stay at home, avoid going to public places), social distancing, and personal precautionary behaviors (e.g., masks wearing and hand washing) were strongly encouraged for controlling the COVID-19 transmission in communities (CNHC, 2020b; Gan et al., 2020). As the outbreak was initially suppressed after March 2020 in China (Tian et al., 2020; Sun et al., 2020), restriction policies have been gradually loosened and personal preventive behaviors become essential measures in controlling COVID-19. However, data from both China and the United States have shown an immediate increase of new COVID-19 cases after national restrictions were loosened (Beijing Municipal Health Commission, 2020; USA Today, 2021). Hence, adherence to preventive behaviors is critical in coping with such a long-lasting pandemic. It is important to understand factors contributing to preventive practices, especially when nationwide restrictions were being gradually loosened.
Health Belief Model: A Theoretical Framework to Understand Preventive Behaviors
Health belief model (HBM) provides a theoretical guidance to understand psychological influences on preventive behaviors in controlling the pandemic. This theory posits that individuals’ health action can be determined by numerous beliefs regarding illness or health behavior practice, including perceived susceptibility (i.e., a subjective evaluation of developing an illness), perceived severity (i.e., a subjective evaluation of the severity of the illness), perceived benefits (i.e., positive consequences of health behaviors), perceived barriers (i.e., costs of action), and self-efficacy (i.e., perceived confidence on individual’s ability to practice health behaviors). Previous review and meta-analysis studies have revealed that higher levels in perceived susceptibility, severity, benefits, and self-efficacy are associated with more preventive behavior practices, while a higher level in perceived barriers is associated with less practices (Carpenter, 2010; Sim et al., 2014).
Inspired by HBM, a number of global COVID-19 research has examined the role of health beliefs in prevention behaviors (e.g., wearing a mask) and documented consistent results with previous HBM research (Chen & Chen, 2020; Chen et al., 2020; Dai et al., 2020; Pan et al., 2020; Yan et al., 2020; Kim & Kim, 2020; Fathian-Dastgerdi et al., 2021). However, it is noteworthy that most of these studies were conducted at the early stage of the pandemic. The consideration of the pandemic stages is important because heath beliefs (e.g., perceived susceptibility) may change as the incidence of transmission has become lower (Leung et al., 2020), and the change of health beliefs could influence individuals’ subsequent preventive practices. Accordingly, it is worth examining health beliefs and their associations with preventive behaviors after the initial outbreak. Such an exploration would enrich the knowledge about the role of health beliefs in different phases of a pandemic.
COVID-19 Stressors as Antecedent Factors Affecting Health Beliefs and Preventive Behaviors
In addition to health beliefs, HBM literature has also suggested the distal influences from antecedent factors (Abraham & Sheeran, 2005). In a pandemic context, disease-related stressors (e.g., COVID-19 stressors) may be one of such antecedent factors. Since the outbreak of the pandemic, Chinese residents have exposed to numerous stressors such as daily disturbances, discussions about novel coronavirus, uncertainty towards media, massive COVID-19 negative news, and COVID-19-like symptoms in family or friends (Ye et al., 2020; Lin et al., 2020), and these stressors have been negatively influential to preventive behavior uptakes (Peng et al., 2021). In addition, disease-related stressors may influence health beliefs, and such influences may vary among different health beliefs. Several HBM studies on medication regimen or control of illness have shown that a higher level of perceived stress was associated with a higher level of perceived threat but lower levels of perceived benefits and self-efficacy (Im & Huh, 2017; Morton & Duck, 2001; Roddenberry & Renk, 2010). Accordingly, it is possible that individuals who expose to more COVID-19 stressors (e.g., negative COVID-19 news) would develop higher perceived threat (i.e., perceived susceptibility and severity) but establish lower protective beliefs (e.g., perceived benefits and self-efficacy) towards preventive behaviors.
Taken the stressors findings together with HBM, the mechanism of COVID-19 stressors on preventive behaviors may occur through a mediation role of health beliefs. That is, COVID-19 stressors, as antecedent factors, would be associated with health beliefs, and, in turn, health beliefs would be associated with preventive behaviors. It is important to examine this mediation role as it can contribute to theoretical insights of psychological influences on preventive behaviors during the COVID-19 pandemic on the utility of health belief model and potentially inform interventions to promote adherence to preventive measures in face of the long-term pandemic. However, scant COVID-19 studies have examined such a mediation model.
The Purpose of Present Study
The purpose of the current study was to examine the underlying mechanism among COVID-19 stressors, health beliefs (i.e., perceived susceptibility, perceived severity, perceived benefits, perceived barriers, and self-efficacy), and preventive behaviors (i.e., social distancing, self-quarantine, and precautionary behaviors) over time during the COVID-19 pandemic in China. Guided by HBM, the current study postulated a hypothesized mediation model. Specifically, we hypothesized that (1) health beliefs would be associated with preventive behaviors; (2) COVID-19 stressors would be associated with health beliefs and preventive behaviors; and (3) health beliefs would mediate the association between COVID-19 stressors and preventive behaviors.
Methods
Participants and Procedure
Two waves of longitudinal data were collected from 1225 college students via online survey using SO JUMP, a well-known Chinese online survey platform similar to Amazon Mechanical Turk (Wang et al., 2020). Wave 1 (w1) survey was conducted between January 31st and February 11th, 2020, which was considered as the peak period of the COVID-19 epidemic in China (CNHC, 2020c) and wave 2 (w2) survey was conducted between March 20th and April 4th, 2020, which was considered as the period in which the COVID-19 outbreak has been initially suppressed in China (CNHC, 2020d). College students were invited by email to participate in the survey and participants who were willing to participate in the follow up provided their email addresses during the w1 survey.
The inclusion criteria for participation were (1) currently enrolled in an academic program in China (i.e., bachelor’s, master’s, or doctoral); and (2) willing to provide online consent. Respondents were excluded if they had been already graduated or self-identified as prospective college students. Online consent was obtained before the survey. Details about data collection were presented in a previous study (Ye et al., 2020). The study protocol was approved by the Institutional Review Board of the Faculty of Psychology, Beijing Normal University.
Measures
Demographics
Participants were asked to provide their demographic information including gender, years of age, college years (e.g., freshmen or sophomore, junior or senior), major, and residence at w1. Given majority of participants were in health-related majors (i.e., Medicine), major was dichotomized into health-related (1) and non-health related (0). Considering that Hubei province was the epicenter of COVID-19 in China during the study, responses on w1 residence were categorized into Hubei province (1) and other regions in mainland China (0).
COVID-19 Stressors
Nine items from the SARS-related Stressors Scale (Main et al., 2011) were adapted to assess the potential stressors during the COVID-19 outbreak at w1. A checklist with two response options (1 = yes, 0 = no) was used to indicate if participants had been exposed to potential stressors related to COVID-19 in the past month. Stressors included confirmed or suspected infection among relatives or friends (e.g., “relatives or friends were suspected or confirmed with coronavirus infection”), the interruptions, inconvenience, and chaos in their daily life (e.g., “schedules for daily life, work, or school have been interrupted and messed up”), discussions on the severity and infectability of the virus (“heard or read discussions by others regarding the severity and infectability of the novel coronavirus”), negative news from authorities (“heard or read much negative news from the authoritative channels regarding the epidemic”), family conflicts (“conflict with family members due to the epidemic”), and information uncertainty (e.g., “difficult to tell the authenticity of much online information regarding the epidemic”). The responses to 9 items were summed as a compose score (ranging from 0 to 9), with a higher score indicating a higher level of exposure to COVID-19 stressors. Cronbach’s alpha was .57, McDonald’s Omega (ω) was .59.
Preventive Behaviors in Controlling COVID-19
Participants reported their preventive behaviors at both w1 and w2 using three measures adapted from the pandemic-related health behavior questionnaire developed by Lee-Baggley et al. (2004).
Precautionary Behaviors
Participants were asked to report their frequencies of four personal preventive practices recommended by governmental agencies in the previous two weeks, including “wearing a mask and replace a new one regularly”, “practicing hand hygiene”, “taking seriously care about personal cleanliness”, and “increasing indoor air circulation”. Responses ranged from 1 (never) to 4 (always) for each item. Responses to 4 items were summed as a composite score (ranging from 4 to 16), with a higher score indicating a higher level of daily precaution or taking preventive medications. Cronbach’s alphas are .73 for w1 and .77 for w2, McDonald’s Omegas (ω) were .77 for w1 and .79 for w2.
Self-Quarantine
Participants responded to 10 dichotomous questions (1 = yes, 0 = No) which asked whether they have ever engaged in the behaviors to avoid specific places at risk for COVID-19 infections, such as “avoid traveling to areas affected by the COVID-19 outbreak” in the past two weeks. The sum score (ranging from 0 to 10) was generated with higher scores indicating better practices of self-quarantine. Cronbach’s alphas for self-quarantine scale are .65 and .74 at w1 and w2, McDonald’s Omegas (ω) were .75 for w1 and .78 for w2, respectively.
Social Distancing
Participants responded to 6 dichotomous questions (1 = yes, 0 = No) which asked whether they have ever engaged in social distancing behavior to avoid contacting with people who were considered to have a high risk for COVID-19 (e.g., “avoid shaking hands with others”) in the previous two weeks. The sum score (ranging from 0 to 6) was generated, with higher scores indicating better practices of social distancing. Cronbach’s alphas of this scale were .75 at w1 and .86 at w2, while McDonald’s Omegas (ω) were .86 for w1 and .89 for w2.
Health Beliefs
Perceived Susceptibility and Perceived Severity
Perceived susceptibility and severity about COVID-19 were measured at wave 2 using a 6-item scale adapted from a perceived threat measure for SARS (Lee-Baggley et al., 2004). Participants were asked to evaluate the extent to which they agreed with statements describing threats of COVID-19 to their health in the previous two weeks. Response options ranged from 1 (totally disagree) to 4 (totally agree). Three items assessed perceived susceptibility (e.g., “I think it is possible to get infected with COVID-19 even if going out without a mask only once”) and the other three items assessed perceived severity (e.g., “I think COVID-19 could threaten my health”). Mean scores for two subscales were generated, with a higher score indicating a higher level of perceived susceptibility or perceived severity. Cronbach’s alphas were .67 for perceived susceptibility subscale and .90 for perceived severity subscale. McDonald’s Omegas (ω) were .68 and .90 for the two scales, respectively.
Perceived Benefits and Perceived Barriers
Perceived benefits and perceived barriers of practicing preventive behaviors were measured at w2 using a 6-item scale adapted from a measure for SARS (Cheng & Ng, 2006). Participants were asked to rate the extent to which they agreed with statements describing the potential consequences of adopting preventive behaviors in response to the COVID-19 pandemic in the previous two weeks. Response options ranged from 1 (totally disagree) to 4 (totally agree). Perceived benefits were assessed by three items (e.g., “If I adopt the preventive measures, I will be less vulnerable to COVID-19 infection”). Perceived barriers were measured by other three items (e.g., “Preventive measures will cause inconvenience to me”). Mean scores for two subscales were generated, with a higher score indicating a higher level of perceived benefits or perceived barriers. Cronbach’s alphas and McDonald’s Omegas (ω) were .93 and .93 for perceived benefits subscale and .80 and .81 for perceived barriers subscale.
Self-Efficacy
The 7-item scale of self-efficacy associated with COVID-19 was adapted from a 5-item self-efficacy measure which was developed for Ebola and influenza A (Cahyanto et al., 2016; Lee et al., 2012). Five items in the original scale were modified to assess participants’ beliefs in their capabilities to exercise preventive behaviors related to COVID-19 (e.g., “I am confident that I am able to take action to prevent contracting coronavirus”) and to control over the influences of the COVID-19 outbreak (e.g., “I know what to do if I suspect that I have been exposed to coronavirus”). Two new items were added to the scale “I am confident that I have enough resources (e.g., masks) to prevent coronavirus infection” and “I am confident that I will be taken good care of if I’m infected by coronavirus”. Participants rated items on a 4-point scale ranging from 1 (not at all) to 4 (a great deal). A total score from nine items was generated, with a higher score representing a greater level of self-efficacy (α = .91, McDonald’s Omega [ω] = .90).
Data Analysis
Multiple statistical analysis approaches were employed in the present study using SPSS version 22 and Mplus version 7.1. First, paired sample t test was conducted for examining the differences in preventive behaviors (precautionary behaviors, self-quarantine, and social distancing) between w1 and w2. Second, Spearman’s correlation was conducted to examine the bivariate associations among study variables, including COVID-19 stressors (w1), preventive behaviors (w2), and health beliefs (i.e., perceived benefits, perceived barriers, perceived susceptibility, perceived severity, and self-efficacy) (w2). Third, path analysis was employed to examine the hypothesized mediation model controlling for demographic variables and the baseline preventive behaviors. Several goodness-of-fit indices including the root mean square of approximation (RMSEA), the comparative fit index (CFI), and standardized root mean square of residual (SRMR) were used to evaluate the model fit, with RMSEA and SRMR below .08, and CFI above .90 indicating a good model fit (Hu & Bentler, 1999). The indirect effects were examined using the bootstrapping with 2000 samples (Muthen & Muthen, 2017). A significant mediating effect would be identified if the 95% confidence interval (CI) from bootstrap examination does not include zero.
To examine structural validity, all study scales (i.e., COVID-19 stressors, five HBM constructs, and three preventive behaviors) were tested using confirmatory factor analysis (CFA). Items in one scale (e.g., perceived benefits scale) were set to load into one latent factor (e.g., perceived benefits). Results revealed that factor loadings of items in each scale were all statistically significant (βs = .41–.92, ps < .001) and the CFA models showed good fits to data (CFIs = .94–.99, TLIs = .90–.99, RMSEAs = .03–.06, SRMRs = .01–.04), suggesting that study scales had generally good structural validity.
Results
Descriptive Statistics and Paired Sample T-Test of Preventive Behaviors
The demographic characteristics were shown in Table 1. Participants were mostly women (70.69%). The average age was 20.22 years (Standard Deviation [SD] = 2.02). Freshman accounted for the largest proportion (43.02%) among the sample. Over one in three (33.96%) of participants studied in health-related majors. About 2% of participants stayed in Hubei province during the outbreak of COVID-19.
The descriptive statistics of preventive behaviors at w1 and w2 were both shown in Table 2. Paired sample t tests were conducted for comparing preventive behaviors between w1 and w2. The results showed that precautionary behaviors increased from w1 to w2 (t = −3.46, df = 1224, p = .001, 95% CI [−.28–.08]). Self-quarantine (t = 2.28, df = 1224, p = .020, 95% CI [.02 .15]) and social distancing (t = 9.04, df = 1224, p = .001, 95% CI [.42 .63]) decreased from w1 to w2.
Bivariate Analyses
Results of bivariate analyses among various study variables were shown in Table 3. COVID-19 stressors was negatively correlated with precautionary behaviors (r = −.07, p = .014) and positively correlated with social distancing (r = .11, p < .001). Perceived benefits was positively correlated with precautionary behaviors (r = .19, p < .001), quarantine (r = .06, p = .027), and social distancing (r = .10, p = .001). Perceived barriers was negatively correlated with precautionary behaviors (r = −.14, p < .001). Perceived susceptibility was positively correlated with precautionary behaviors (r = .14, p < .001), self-quarantine (r = .13, p < .001), and social distancing (r = .22, p < .001). Perceived severity was negatively correlated with precautionary behaviors (r = −.09, p = .002) and positively correlated with social distancing (r = .07, p = .012). Self-efficacy was positively correlated with precautionary behaviors (r = .39, p < .001), self-quarantine (r = .08, p = .006), and social distancing (r = .10, p < .001).
Path Analysis of the Hypothesized Model
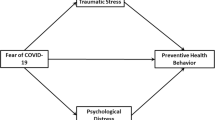
Results of path analysis on the mediation model among COVID-19 stressors, HBM constructs, and preventive behaviors were shown in Fig. 1. The model showed an overall good model fit to data (χ2 = 137.11, df = 36, RMSEA = .05, RMSEA 90% CI [.04, .06], CFI = .94, SRMR = .04). The direct effect of COVID-19 stressors on social distancing was statistically significant (β = .09, p < .001). In addition, COVID-19 stressors was negatively associated with perceived benefits (β = −.07, p = .013) and self-efficacy (β = −.06, p = .020), and positively associated with perceived barriers (β = .08, p = .002) and perceived severity (β = .12, p < .001). Moreover, perceived barriers (β = −.07, p = .003) was negatively associated with precautionary behaviors. Perceived susceptibility (β = .06, p = .025) and self-efficacy (β = .23, p < .001) were positively associated with precautionary behaviors. Perceived susceptibility was positively associated with self-quarantine (β = .11, p < .001) and social distancing (β = .16, p < .001).
Indirect Effects
As shown in Table 4, the indirect effects of perceived barriers (β = −.01, p = .033) and self-efficacy (β = −.02, p = .024) in the relationship between COVID-19 stressors and precautionary behaviors were statistically significant. Results of bootstrapping suggested that perceived barriers (95% CI = −.011 to −.001) and self-efficacy (95% CI = −.027 to −.002) mediated the associations of COVID-19 stressors with precautionary behaviors.
Discussion
The current study used longitudinal data from a sample of college students and examined the association among COVID-19 stressors, health beliefs (i.e., perceived benefits, perceived barriers, perceived susceptibility, perceived severity, and self-efficacy), and preventive behaviors (i.e., precautionary behaviors, self-quarantine, social distancing) in response to COVID-19 in China. Guided by HBM, the current study identified factors contributing to preventive behaviors over time during the COVID-19 pandemic. In particular, our findings suggested a serial stress-cognition-behavior association, revealing that the exposure to COVID-19 stressors at the beginning of the pandemic can influence preventive behavior uptakes, even at the phase when outbreak has been suppressed, and such influences occurred through health beliefs. To the best of our knowledge, the current study was one of the first attempts to examine COVID-19 stressors impacts on HBM constructs and preventive behaviors using longitudinal data during the pandemic.
Our findings suggested that preventive behaviors changed significantly after the initial outbreak of the pandemic. In particular, self-quarantine and social distancing significantly decreased. This may be related to the changes of national policy responses to COVID-19 pandemic. At the peak of the COVID-19 pandemic, Chinese government enforced various harsh restrictions in order to limit interpersonal contracts, such as stay-at-home and shelter-in-place orders. As the pandemic initially suppressed, these restrictions were loosened in many Chinese regions, allowing some activities to resume (e.g., return to work and dinning in a restaurant) (Gan et al., 2020). This would result in reductions of social distancing and self-quarantine practices. However, our data revealed that precautionary behaviors significantly increased even when the outbreak was suppressed. This is congruent with the longitudinal data (from February to March 2020) from a recent study in China (Peng et al., 2021). This seems to suggest that Chinese people’s prevention practices in the early phase of the pandemic have transformed to a personal habit, and such a habit was maintained in a later phase of the pandemic. The increased precautionary behavior uptakes may be also related to the increase of interpersonal contacts (e.g., school reopen) at wave 2, leading to more practices of wearing masks and personal hygiene. Such changes in personal precautionary behaviors have also been documented in an international study, revealing a significant increase of precautionary behaviors after the national governmental intervention among Western and Northern Europeans (Varga et al., 2021).
Our findings revealed that preventive behaviors were influenced by three health beliefs, including perceived susceptibility, self-efficacy, and perceived barriers. This implied that, when the outbreak of the COVID-19 pandemic has initially suppressed, Chinese college students’ health action decision making relied upon three cognitive appraisal processes. First, the influence of perceived susceptibility suggested that individuals who appraised their current situations to have high risk for COVID-19 infection exhibited strong adherence to numerous preventive behaviors, including social distancing, self-quarantine, and precautionary behaviors. The critical role of risk perception has been documented in health behavior literature, indicating that perceived susceptibility became particularly salient in the context of pandemic prevention (Bish & Michie, 2010; Dror et al., 2020; Graffigna et al., 2020; Janz & Becker, 1984). A recent COVID-19 study in China has also documented a similar finding (Peng et al., 2021). This could be explained by the transactional model of stress and coping, which depicts a stress response mechanism through two (primary and secondary) cognitive appraisal processes (Folkman et al., 1986). In particular, perceived susceptibility is associated with the primary appraisal, which states that individuals are strongly motivated to exhibit coping behaviors (e.g., preventive practices) if the current situation is evaluated as threatful. Second, the influence of self-efficacy revealed that precautionary behavior uptakes would be dependent on individuals’ assessments on their personal competencies or psychological assets associated with the behaviors. That is, individuals who perceived higher confidence or better control of behaviors would exhibit greater adherence to personal prevention practices. A systematic review on HBM research has documented a congruent finding, revealing that self-efficacy was a strong predictor specifically for influenza-related precautionary practices including hygiene behaviors, hand washing, and respiratory hygiene (Bish & Michie, 2010). The favorable influence of self-efficacy supports the secondary appraisal in the transactional model of stress and coping (Folkman et al., 1986), suggesting that individuals likely adopt proactive coping (e.g., precautionary behaviors) when they perceive sufficient psychological resources (e.g., self-efficacy). Third, the effects of perceived barriers suggested that adherence to preventive practices would be challenged by perceived negative consequences of the behaviors. Although HBM posits that perceived benefits and barriers jointly contribute to health behavior uptakes, perceived barriers were the stronger predictor when behavior outcomes were preventive behaviors (Carpenter, 2010; Janz & Becker, 1984). This may be due to the fact that some barriers are not addressable (e.g., preventive measures cause inconvenience), and that the persistent perception on negative consequences may induce cognition dissonance (Festinger, 1957), undermining self-control on adherence to preventive behaviors. Taken all together, our finding revealed that Chinese residents’ preventive behaviors uptakes were influenced by the cognitive appraisals on their contextual situations, personal competencies, and negative consequences of the behaviors during the COVID-19 phase when national restrictions were loosened.
One of important findings in the current study is that health beliefs can be influenced by previous COVID-19 stressor exposure (e.g., daily life interruptions, negative news about the pandemic, and uncertainty of information), suggesting stress experiences at the beginning of the COVID-19 pandemic could shape health beliefs and impact behaviors in a long-term manner. Our path analysis revealed two mediation associations, indicating that more stressors exposure was associated with lower self-efficacy but higher perceived barriers, resulting in weaker adherence to precautionary behaviors. Such findings may be related to emotional burdens. Existing literature showed that individuals who exposed to a great amount of negative information or misinformation about the pandemic could induce high levels of anxiety (Banerjee & Rao, 2020; Lee et al., 2020). Individuals who suffered from anxiety would overestimate potential risk of the behaviors but underestimate the benefits (Bliss & Morrison, 2020; Dube et al., 2014; Karafillakis et al., 2017; Larson, 2018). Also, emotional burdens related to the pandemic would be associated with a lower perception on personal competencies, devastating self-efficacy. Indeed, previous research at the early phase of the COVID-19 pandemic has revealed that more COVID-19 stressor exposure was associated with greater levels of psychiatric symptoms (i.e., acute stress disorder) and lower levels of perception of personal competencies (e.g., psychological resilience) (Ye et al., 2020). These stress-induced detrimental impacts on health beliefs would be due to an information-processing bias for threatening information when individuals experience distress (Puleo et al., 2011). Given its longitudinal influences on cognitions and behaviors, stress experiences in early pandemic meritshigh attention.
Given that effective COVID-19 vaccines are not likely to be widely distributed until late 2021 (Hobson & Hagan, 2020), prevention practices, especially personal precautionary behaviors, would still play an essential role in coping with the COVID-19 pandemic. Our findings provide several implications for interventions and policy-making for promoting prevention behaviors. First, our results in terms of health beliefs imply that health communications should be tailored to these health beliefs. Existing intervention research has shown successes in adopting health-belief-framed messages for promoting influenza disease prevention (Payaprom et al., 2011). In the context of COVID-19, health messages could be framed to highlight the vulnerability and severe consequences of the pandemic (e.g., ‘We are all possible to be infected by COVID-19 and it may put you in a severe situation and strongly affect your health”). Messages based on autonomy motivations (e.g., supporting the sense of choices of the ways in practicing prevention behaviors) and exemplification (e.g., messages presented with an exemplar) would be helpful to promote self-efficacy of prevention behaviors (Valle et al., 2018). Prosocial-framed messages could shift attention from the barriers against prevention practices to prosocial benefits (e.g., the protection of significant others) (Chou & Budenz, 2020; Jordan et al., 2020). Second, our findings regarding the influences of COVID-19 stressors imply that preventive behavior promotion interventions should also attend to pandemic stress management. Such interventions may benefit from including cognitive behavioral strategies, such as mindfulness-based intervention, which have been effective in fostering adaptive coping skills (e.g., emotion regulation) and enhancing psycho-behavioral health (e.g., reducing depression and promoting self-care behaviors) (Garland et al., 2009; Gu et al., 2015; Soriano-Ayala et al., 2020). To address pandemic stressors such as media information uncertainty, government should develop policy to enhance media censorship in terms of misinformation. The accessibility to psycho-behavioral resources (e.g., mental health services and personal protective equipment) should be enhanced for individuals who have exposed to multiple COVID-19 stressors.
The present study has several methodological limitations. First, data were collected by online surveys and may be subject to the self-reporting bias (e.g., social desirability) and self-selection bias (only a small proportion of w1 participants completed the w2 survey). Second, the data were collected from a convenience sample of college students and our findings may not be generalized to all Chinese residents. Third, some measures (i.e., self-quarantine, and perceived susceptibility) were adapted from previous studies and showed low internal consistency (e.g., COVID-19 stressors). These measures needed further validation. Fourth, given that health beliefs were only measured at w2, the association between health beliefs and preventive behaviors cannot draw conclusions about causality. Fifth, the model was examined in a generally healthy population (college students). Compared to healthy population, individuals with medical conditions (e.g., chronic diseases) would be more vulnerable to the COVID-19 pandemic (e.g., more exposure to stressors) and preventive behaviors is particularly essential to protect their health. Hence, it is worth examining the model among people with medical conditions. Future research will benefit from using a random sampling approach, utilizing a multiple-wave longitudinal design, validating self-developed measures, and expanding study population to people with medical conditions.
Conclusions
In summary, our findings showed that prevention behavior uptakes among Chinese residents changed after the initial outbreak of the pandemic. The current study adds to HBM literature, finding that several health beliefs, including perceived susceptibility, self-efficacy, and perceived barriers, were associated with COVID-19-related preventive behaviors, such as personal precautionary behaviors. COVID-19 stressor exposure at the early phase of the pandemic can influence precautionary behaviors over time through self-efficacy and perceived barriers. Given that the pandemic seems to continue for a considerable period of time, preventive behavior promotion interventions are warranted, and such interventions would benefit from attending to health beliefs and being tailored for COVID-19 stressors.
Data Availability
The Datasets generated during and/or analyzed during the current study are available from the corresponding author on reasonable request.
References
Abraham, C., & Sheeran, P. (2005). The health belief model. In M. T. Conner & P. Norman (Eds.), Predicting health behaviour: Re- search and practice with social cognition models (2nd ed., pp. 28–80). Open University Press.
Banerjee, D., & Rao, T. S. (2020). Psychology of misinformation and the media: Insights from the COVID-19 pandemic. Indian Journal of Social Psychiatry, 36(5), 131. https://doi.org/10.4103/ijsp.ijsp_112_20.
Bartsch, S., Weber, E., Büttgen, M., & Huber, A. (2020). Leadership matters in crisis-induced digital transformation: how to lead service employees effectively during the covid-19 pandemic. Journal of Service Management, ahead-of-print(ahead-of-print). https://doi.org/10.1108/JOSM-05-2020-0160.
Beijing Municipal Health Commission. (2020). Beijing newly reported 36 confirmed cases of COVID-19 yesterday. http://wjw.beijing.gov.cn/wjwh/ztzl/xxgzbd/gzbdyqtb/202006/t20200614_1924537.html. Accessed 14 Jun 2020.
Bish, A., & Michie, S. (2010). Demographic and attitudinal determinants of protective behaviours during a pandemic: A review. British Journal of Health Psychology, 15, 797–824. https://doi.org/10.1348/135910710x485826.
Bliss, K., & Morrison, J. S. (2020). The Risks of Misinformation and Vaccine Hesitancy within the Covid-19 Crisis. https://www.csis.org/analysis/risks-misinformation-and-vaccine-hesitancy-within-covid-19-crisis
Cahyanto, I., Wiblishauser, M., Pennington-Gray, L., & Schroeder, A. (2016). The dynamics of travel avoidance: The case of Ebola in the U.S. Tourism Management Perspectives, 20, 195–203. https://doi.org/10.1016/j.tmp.2016.09.004.
Carfì, A., Bernabei, R., & Landi, F. (2020). Persistent symptoms in patients after acute COVID-19. JAMA, 324(6), 603–605. https://doi.org/10.1001/jama.2020.12603.
Carpenter, C. J. (2010). A meta-analysis of the effectiveness of health belief model variables in predicting behavior. Health Communication, 25(8), 661–669. https://doi.org/10.1080/10410236.2010.521906.
Chen, X. W., & Chen, H. L. (2020). Differences in preventive behaviors of COVID-19 between urban and rural residents: Lessons learned from a cross-sectional study in China. International Journal of Environmental Research and Public Health, 17(12), 14, Article 4437. https://doi.org/10.3390/ijerph17124437.
Chen, X. Y., Ran, L., Liu, Q., Hu, Q. K., Du, X. Y., & Tan, X. D. (2020). Hand hygiene, mask-wearing behaviors and its associated factors during the COVID-19 epidemic: A cross-sectional study among primary school students in Wuhan, China. International Journal of Environmental Research and Public Health, 17(8), 2893. https://doi.org/10.3390/ijerph17082893.
Cheng, C., & Ng, A. K. (2006). Psychosocial factors predicting SARS-preventive behaviors in four major SARS-affected regions. Journal of Applied Social Psychology, 36(1), 222–247. https://doi.org/10.1111/j.0021-9029.2006.00059.x.
China National Health Commission. (2020a). The prevention and control of the 2019 novel coronavirus infection (second edition). http://www.nhc.gov.cn/xcs/zhengcwj/202001/c67cfe29ecf1470e8c7fc47d3b751e88.shtml
China National Health Commission. (2020b). A letter of appleal directions for preventing COVID-19 infection. http://www.nhc.gov.cn/xcs/fkdt/202001/c7078e26e17b46168d7ddf3dbefcda26.shtml
China National Health Commission. (2020c). Update on novel coronavirus Epidemic Situation at 24 :00 on February 6. Retrieved from http://www.nhc.gov.cn/yjb/s7860/202002/3db09278e3034f289841300ed09bd0e1.shtml.
China National Health Commission. (2020d). Update on novel coronavirus Epidemic Situation at 24 :00 on March 30. Retrieved from http://www.nhc.gov.cn/yjb/s7860/202003/ec2689b0e716468fbfff7cf890c74bb7.shtml.
Chou, W., & Budenz, A. (2020). Considering emotion in COVID-19 vaccine communication: Addressing vaccine hesitancy and fostering vaccine confidence. Health Communication, 35(14), 1718–1722. https://doi.org/10.1080/10410236.2020.1838096.
Coibion, O., Gorodnichenko, Y., & Weber, M.. (2020). Does policy communication during covid-19 work?. Department of Economics, Working Paper Series.
Dai, B. B., Fu, D., Meng, G. T., Liu, B. S., Li, Q., & Liu, X. (2020). The effects of governmental and individual predictors on COVID-19 protective behaviors in China: A path analysis model. Public Administration Review, 8, 797–804. https://doi.org/10.1111/puar.13236.
Dror, A. A., Eisenbach, N., Taiber, S., Morozov, N. G., Mizrachi, M., Zigron, A., Srouji, S., & Sela, E. (2020). Vaccine hesitancy: The next challenge in the fight against COVID-19. European Journal of Epidemiology, 35(8), 775–779. https://doi.org/10.1007/s10654-020-00671-y.
Dube, E., Gagnon, D., Nickels, E., Jeram, S., & Schuster, M. (2014). Mapping vaccine hesitancy-country-specific characteristics of a global phenomenon. Vaccine, 32(49), 6649–6654. https://doi.org/10.1016/j.vaccine.2014.09.039.
Fathian-Dastgerdi, Z., Tavakoli, B., & Jaleh, M. (2021). Factors associated with preventive behaviors of COVID-19 among adolescents: Applying the health belief model. Research in Social and Administrative Pharmacy, 6. https://doi.org/10.1016/j.sapharm.2021.01.014.
Festinger, L. (1957). A theory of cognitive dissonance (Vol. 2). Stanford University Press.
Folkman, S., Lazarus, R. S., Dunkel-Schetter, C., DeLongis, A., & Gruen, R. J. (1986). Dynamics of a stressful encounter: Cognitive appraisal, coping, and encounter outcomes. Journal of Personality and Social Psychology, 50(5), 992–1003. https://doi.org/10.1037/0022-3514.50.5.992.
Gan, Y., Ma, J., Wu, J., Chen, Y., Zhu, H., & Hall, B. J. (2020). Immediate and delayed psychological effects of province-wide lockdown and personal quarantine during the COVID-19 outbreak in China. Psychological Medicine, 1–12. https://doi.org/10.1017/s0033291720003116.
Garland, E., Gaylord, S., & Park, J. (2009). The role of mindfulness in positive reappraisal. Explore-the Journal of Science and Healing, 5(1), 37–44. https://doi.org/10.1016/j.explore.2008.10.001.
Graffigna, G., Palamenghi, L., Boccia, S., & Barello, S. (2020). Relationship between citizens’ health engagement and intention to take the COVID-19 vaccine in Italy: A mediation analysis. Vaccines, 8(4). https://doi.org/10.3390/vaccines8040576.
Gu, J., Strauss, C., Bond, R., & Cavanagh, K. (2015). How do mindfulness-based cognitive therapy and mindfulness-based stress reduction improve mental health and wellbeing? A systematic review and meta-analysis of mediation studies. Clinical Psychology Review, 37, 1–12. https://doi.org/10.1016/j.cpr.2015.01.006.
Hobson, J., & Hagan, A. (2020). General Public Won't Receive COVID-19 Vaccine until Mid to Late 2021. Doctor Predicts. https://www.wbur.org/hereandnow/2020/09/14/covid-19-vaccine-distribution
Hu, L. T., & Bentler, P. M. (1999). Cutoff criteria for fit indexes in covariance structure analysis: Conventional criteria versus new alternatives. Structural Equation Modeling-a Multidisciplinary Journal, 6(1), 1–55. https://doi.org/10.1080/10705519909540118.
Im, H., & Huh, J. (2017). Does health information in mass media help or hurt patients? Investigation of potential negative influence of mass media health information on patients' beliefs and medication regimen adherence. Journal of Health Communication, 214, 214–222. https://doi.org/10.1080/10810730.2016.1261970.
International Society for Infectious Diseases. (2020). Undiagnosed pneumonia - China. https://promedmail.org/promed-post/?id=6864153%20#COVID19
Janz, N. K., & Becker, M. H. (1984). The health belief model - a decade later. Health Education Quarterly, 11(1), 1–47. https://doi.org/10.1177/109019818401100101.
Johns Hopkins University and Medicine. (2021). COVID-19 Dashboard by the Center for Systems Science and Engineering (CSSE) at Johns Hopkins University (JHU). https://coronavirus.jhu.edu/map.html
Jordan, J., Yoeli, E., & Rand, D. (2020). Don’t get it or don’t spread it? Comparing self-interested versus prosocially framed COVID-19 prevention messaging. https://doi.org/10.31234/osf.io/yuq7x.
Karafillakis, E., Larson, H. J., & Consortium, A. (2017). The benefit of the doubt or doubts over benefits? A systematic literature review of perceived risks of vaccines in European populations. Vaccine, 35(37), 4840–4850. https://doi.org/10.1016/j.vaccine.2017.07.061.
Kim, S., & Kim, S. (2020). Analysis of the impact of health beliefs and resource factors on preventive behaviors against the COVID-19 pandemic. International Journal of Environmental Research and Public Health, 17(22), 8666. https://doi.org/10.3390/ijerph17228666.
Larson, H. J. (2018). The biggest pandemic risk? Viral misinformation [editorial material]. Nature, 562(7727), 309–309. https://doi.org/10.1038/d41586-018-07034-4.
Lee, C. K., Song, H. J., Bendle, L. J., Kim, M. J., & Han, H. (2012). The impact of non-pharmaceutical interventions for 2009 H1N1 influenza on travel intentions: A model of goal-directed behavior. Tourism Management, 33(1), 89–99. https://doi.org/10.1016/j.tourman.2011.02.006.
Lee, J. J., Kang, K.-A., Wang, M. P., Zhao, S. Z., Wong, J. Y. H., O'Connor, S., Yang, S. C., & Shin, S. (2020). Associations between COVID-19 misinformation exposure and belief with COVID-19 knowledge and preventive behaviors: Cross-sectional online study. Journal of Medical Internet Research, 22(11), e22205. https://doi.org/10.2196/22205.
Lee-Baggley, D., DeLongis, A., Voorhoeave, P., & Greenglass, E. (2004). Coping with the threat of severe acute respiratory syndrome: Role of threat appraisals and coping responses in health behaviors. Asian Journal of Social Psychology, 7(1), 9–23. https://doi.org/10.1111/j.1467-839X.2004.00131.x.
Leung, K., Wu, J. T., Liu, D., & Leung, G. M. (2020). First-wave COVID-19 transmissibility and severity in China outside Hubei after control measures, and second-wave scenario planning: A modelling impact assessment. Lancet, 395(10233), 1382–1393. https://doi.org/10.1016/s0140-6736(20)30746-7.
Lin, D., Friedman, D. B., Qiao, S., Tam, C. C., Li, X., & Li, X. (2020). Information uncertainty: A correlate for acute stress disorder during the COVID-19 outbreak in China. BMC Public Health, 20(1), 1–9. https://doi.org/10.1186/s12889-020-09952-3.
Main, A., Zhou, Q., Ma, Y., Luecken, L. J., & Liu, X. (2011). Relations of SARS-related stressors and coping to Chinese college students’ psychological adjustment during the 2003 Beijing SARS epidemic. Journal of Counseling Psychology, 58(3), 410–423. https://doi.org/10.1037/a0023632.
Morton, T. A., & Duck, J. M. (2001). Communication and health beliefs mass and interpersonal influences on perceptions of risk to self and others. Communication Research, 28(5), 602–626. https://doi.org/10.1177/009365001028005002.
Muthen, L. K., & Muthen, B. O. (2017). Mplus user’s guide (8th ed.). Los Angeles: Author. https://doi.org/10.13155/29825.
Pan, A., Liu, L., Wang, C. L., Guo, H., Hao, X. J., Wang, Q., Huang, J., He, N., Yu, H. J., Lin, X. H., Wei, S., & Wu, T. C. (2020). Association of Public Health Interventions with the epidemiology of the COVID-19 outbreak in Wuhan, China. JAMA-Journal of the American Medical Association, 323(19), 1915–1923. https://doi.org/10.1001/jama.2020.6130.
Payaprom, Y., Bennett, P., Alabaster, E., & Tantipong, H. (2011). Using the health action process approach and implementation intentions to increase flu vaccine uptake in high risk Thai individuals: A controlled before-after trial. Health Psychology, 30(4), 492–500. https://doi.org/10.1037/a0023580.
Peng, S., Yang, X. Y., Yang, T., Zhang, W., & Cottrell, R. R. (2021). Uncertainty stress, and its impact on disease fear and prevention behavior during the COVID-19 epidemic in China: A panel study. American Journal of Health Behavior, 45(2), 334–341. https://doi.org/10.5993/AJHB.45.2.12.
Puleo, C. M., Settipani, C. A., Crawley, S. A., Beidas, R. S., & Kendall, P. C. (2011). Anxiety Disorders. In B. B. Brown & M. J. Prinstein (Eds.), Encyclopedia of adolescence (pp. 48–55). Academic Press. https://doi.org/10.1016/B978-0-12-373951-3.00099-5.
Roddenberry, A., & Renk, K. (2010). Locus of control and self-efficacy: Potential mediators of stress, illness, and utilization of health services in college students. Child Psychiatry and Human Development, 41(4), 353–370. https://doi.org/10.1007/s10578-010-0173-6.
Sim, S., Moey, K., & Tan, N. (2014). The use of facemasks to prevent respiratory infection: A literature review in the context of the health belief model. Singapore Medical Journal, 55(3). https://doi.org/10.11622/smedj.2014037.
Soriano-Ayala, E., Amutio, A., Franco, C., & Manas, I. (2020). Promoting a healthy lifestyle through mindfulness in university students: A randomized controlled trial. Nutrients, 12, 12(8) Article 2450. https://doi.org/10.3390/nu12082450.
Sun, Z., Zhang, H., Yang, Y., Wan, H., & Wang, Y. (2020). Impacts of geographic factors and population density on the covid-19 spreading under the lockdown policies of China. Science of the Total Environment, 746, 141347. https://doi.org/10.1016/j.scitotenv.2020.141347.
Tian, H., Liu, Y., Li, Y., Wu, C.-H., Chen, B., Kraemer, M. U. G., Li B., Cai J., Xu B., Yang Q., Wang B., Yang P., Cui Y., Song Y., Zheng P., Wang Q., Bjornstad O. N., Yang R., Grenfell B. T., Pybus O. G. Dye, C. (2020). An investigation of transmission control measures during the first 50 days of the COVID-19 epidemic in China. Science (New York, N.Y.), eabb6105. https://doi.org/10.1126/science.abb6105.
USA Today. (2021). Map of COVID-19 case trends, restrictions and mobility. Retrieved April 20 from https://www.usatoday.com/storytelling/coronavirus-reopening-america-map/
Valle, C. G., Queen, T. L., Martin, B. A., Ribisl, K. M., Mayer, D. K., & Tate, D. F. (2018). Optimizing tailored communications for health risk assessment: A randomized factorial experiment of the effects of expectancy priming, autonomy support, and exemplification. Journal of Medical Internet Research, 20(3), Article e63. https://doi.org/10.2196/jmir.7613.
Varga, T. V., Bu, F., Dissing, A. S., Elsenburg, L. K., Bustamante, J. J. H., Matta, J., van Zon, S. K. R., Brouwer, S., Bültmann, U., Fancourt, D., Hoeyer, K., Goldberg, M., Melchior, M., Strandberg-Larsen, K., Zins, M., Clotworthy, A., & Rod, N. H. (2021). Loneliness, worries, anxiety, and precautionary behaviours in response to the COVID-19 pandemic: A longitudinal analysis of 200,000 Western and northern Europeans. The Lancet Regional Health-Europe, 2, 100020. https://doi.org/10.1016/j.lanepe.2020.100020.
Wang, Y., Yang, Y. Y., Li, S., Lei, X. M., & Yang, Y. F. (2020). Investigation on the status of influencing factors for depression symptom of children and adolescents with home quarantine during the prevalence of novel coronavirus pneumonia. Chinese Journal of Child Health Care, 03(02), 18. Retrieved from http://kns.cnki.net/kcms/detail/61.1346.R.20200218.1248.002.html
World Health Organization. (2020). Coronavirus disease 2019 (COVID-19) Situation Report-75. https://www.who.int/docs/default-source/coronaviruse/situation-reports/20200404-sitrep-75-covid-19.pdf?sfvrsn=99251b2b_4
Xinhua. (2020). Prevention and control of the outbreak. http://www.xinhuanet.com/politics/leaders/2020-01/31/c_1125517278.htm
Yan, A. F., Sun, X., Zheng, J., Mi, B., Zuo, H., Ruan, G., Hussain, A., Wang, Y., & Shi, Z. (2020). Perceived risk, behavior changes and health-related outcomes during COVID-19 pandemic: Findings among adults with and without diabetes in China. Diabetes Research and Clinical Practice, 167, 108350. https://doi.org/10.1016/j.diabres.2020.108350.
Ye, Z., Yang, X. Y., Zeng, C. B., Wang, Y. Y., Shen, Z. J., Li, X. M., & Lin, D. H. (2020). Resilience, social support, and coping as mediators between COVID-19-related stressful experiences and acute stress disorder among college students in China. Applied Psychology-Health and Well Being, 21. https://doi.org/10.1111/aphw.12211.
Funding
Research reported in this manuscript is supported in part by the National Natural Science Foundation of China under award number 32071076.
Author information
Authors and Affiliations
Corresponding author
Ethics declarations
Conflict of Interest
The authors have no conflicts of interest to report.
Additional information
Publisher’s Note
Springer Nature remains neutral with regard to jurisdictional claims in published maps and institutional affiliations.
Rights and permissions
About this article
Cite this article
Tam, C.C., Li, X., Li, X. et al. Adherence to preventive behaviors among college students during COVID-19 pandemic in China: The role of health beliefs and COVID-19 stressors. Curr Psychol 42, 17280–17290 (2023). https://doi.org/10.1007/s12144-021-01942-x
Accepted:
Published:
Issue Date:
DOI: https://doi.org/10.1007/s12144-021-01942-x