Abstract
The Covid-19 pandemic has had a major impact on migrants and ethnic minorities (MEMs). Socio-economic factors and legal, administrative and language barriers are among the reasons for this increased susceptibility. The aim of the study is to investigate the impact of Covid-19 on MEMs compared to the general population in terms of serious outcomes. We conducted a systematic review collecting studies on the impact of Covid-19 on MEMs compared to the general population in the WHO European Region regarding hospitalisation, intensive care unit (ICU) admission and mortality, published between 01/01/2020 and 19/03/2021. Nine researchers were involved in selection, study quality assessment and data extraction. Of the 82 studies included, 15 of the 16 regarding hospitalisation for Covid-19 reported an increased risk for MEMs compared to the white and/or native population and 22 out of the 28 studies focusing on the ICU admission rates found an increased risk for MEMs. Among the 65 studies on mortality, 43 report a higher risk for MEMs. An increased risk of adverse outcomes was reported for MEMs. Social determinants of health are among the main factors involved in the genesis of health inequalities: a disadvantaged socio-economic status, a framework of structural racism and asymmetric access to healthcare are linked to increased susceptibility to the consequences of Covid-19. These findings underline the need for policymakers to consider the socio-economic barriers when designing prevention plans.
Similar content being viewed by others
Avoid common mistakes on your manuscript.
Background
With more than 600 million cases and over 6 million deaths, as of 7th October 2022, the Covid-19 pandemic represents an unprecedented challenge for countries and health systems worldwide (WHO, 2022a, 2022b). Along with a high toll in terms of death and health outcomes in the population as a whole, the Covid-19 pandemic has also had a recognised impact in widening health inequalities, both between and within countries (Bambra, 2020; Lau, 2020; Marmot & Allen, 2020). Socially disadvantaged population groups have experienced particular vulnerability to the pandemic (Patel JA, 2020).
Migrants and ethnic minorities (MEMs) in particular have been shown to suffer a higher burden both in terms of risk of infection and in terms of negative health outcomes (Greenway, 2020; Hayward, 2021; Phiri, 2021; Sze, 2020). The mechanisms underlying the higher susceptibility of MEMs to worse health outcomes of Covid-19 include factors already known to create health inequity, such as socio-economic difficulty barriers to accessing healthcare such as legal, administrative, linguistic and cultural barriers, in addition to a higher prevalence of pre-existing conditions, often neglected (Greenway, Marceca, 2017; Shaaban, 2020; Stevens, 2021; Woodward, 2014).
While there is growing evidence on the differential impact of diseases on MEMs worldwide, data specific to the WHO European Region is scarce, partly due to the difficulty of retrieving data on ethnicity and migration background for public health purposes (Bozorgmehr, 2019; Corvacho, 2021; Melchior, 2021). The issue of the health of MEMs in the region, however, is pressing, since the WHO European Region is a very ethnically diverse territory and it is estimated that almost 10% of the population living in the WHO European Region is made up of migrants, therefore making clearer that there is no public health without refugee and migrant health (WHO, 2010; WHO, 2018; Abubakar et al., 2018).
In a previously published systematic review (Jaljaa, 2022), we have analysed the higher risk of infection for MEMs in the WHO European Region. The aim of this paper is to collect and synthesise evidence on the differential impact of Covid-19 on MEMs compared to the general population in the WHO European Region, in terms of negative health outcomes, considering risk of hospitalisation and risk of severe disease and mortality.
Methods
This systematic review is the second one of a project registered on PROSPERO (CRD42021247326), carried out according to the Preferred Reporting Items for Systematic Reviews and Meta-Analyses (PRISMA) (Liberati, 2009). The first review focused on the risk of SARS-CoV-2 infection by MEMs compared to the general population of the EU WHO region (Jaljaa, 2022).
The following databases were searched: Medline, Embase, SciSearch, BIOSIS, and ESBIOBASE. PubMed database (which includes medRxiv, bioRxiv, ChemRxiv, arXiv, Research Square, and SSRN) was also searched for preprints.
After receiving the instructions of the working group, the documentation centre developed a preliminary pilot search aimed at balancing recall (sensitivity) and precision (specificity), using the following keywords: migrants, ethnic minorities, mortality, hospitalisation, complications, intensive care unit, SARS-CoV-2, and Covid-19. Later on, a tailored search strategy was performed, including both Medline and Embase subject headings (i.e., Mesh and Emtree terms, respectively) as well as free-text words related to the subject of the review. The complete search strategy is available as supplementary material. The last database search was carried out on the 19th of March 2021. During the query session, duplicate citations due to databases overlap were removed and the results were exported to Microsoft Excel to facilitate further data analysis and management. Additional duplicates, not automatically intercepted, were manually removed based on a review of the titles.
Inclusion and Exclusion Criteria
We included studies reporting differential impact/clinical consequences of Covid-19 on MEMs compared to the general population, in the 53 countries belonging to the WHO European Region. International studies reporting data on WHO European Countries were also included. In particular, eligible studies reported quantitative data on outcomes of Covid-19, including negative health consequences, hospitalisation, access to intensive care unit (ICU) and mortality due to SARS-CoV-2 infection. For the definition of ‘migrant’, we referred to the International Organisation for Migration (IOM) glossary (IOM, 2019; sAppendix 3). We sourced the definition of ‘refugee’ from the convention and protocol relating to the status of refugees of the United Nations High Commissioner for Refugees (UNHCR, 2010; sAppendix 3). At last, we defined ‘ethnic minorities’ according to the European Centre for Disease Prevention and Control (ECDC, 2022; sAppendix 3). However, it must be noted that there is no universally accepted definition of such terms and that the differences between migrants and ethnic minorities are nuanced and dependent on the country context.
We collected studies published from January 1, 2020, to March 19, 2021, in English, Italian, French and Spanish. In our review, we included primary and secondary quantitative and quali-quantitative studies (cross-sectional, case-control, cohort, intervention, case-series, prevalence or ecological studies); purely qualitative studies were excluded. Regarding the publication type, comments, opinions, editorials and news were excluded; letters were included if containing original quantitative data. The selected reviews were excluded if their primary studies had already been taken into consideration. Nine researchers, appropriately trained and constantly monitored, were involved in the study selection and assessment and in data extraction. Two at a time screened, independently, title and abstract against eligibility criteria and, later, assessed eligibility for inclusion by reading the full texts. Any disagreements were resolved by discussion between the two reviewers. If it was not possible, an assessment group intervened to solve the disagreement.
Critical Appraisal, Data Extraction and Synthesis
The study quality was assessed independently by two researchers, using the appropriate Joanna Briggs Institute Critical Appraisal Tools (Critical Appraisal, 2022) for each study design. Quality scores were calculated as the number of positive answers out of the number of applicable questions and converted into percentages. Studies with a score of 80–100% were considered ‘high quality’, 60–79% ‘medium quality’ and 0–59% ‘low quality’. Low-quality studies were not excluded but contributed to the final synthesis.
Data were sought for the following outcomes: hospital admission, severe Covid-19 and ICU admission and mortality. The extraction of relevant information from the included documents was carried out by one researcher, using an appropriate extraction form. Then, another researcher checked the information collected. The items extracted included the following: bibliographic reference, publication country, language, type of study, study period, objectives, population, comparison population if available, diagnostic methods, observation setting, outcomes, results, conclusions, limits, comments and study quality.
Disagreements both in quality assessment and in data extraction were resolved by discussion between the two researchers. If it was not possible, an assessment group stepped in for a final decision.
Data of the included studies were narratively described and gathered according to the three main outcomes (hospital admission, severe Covid-19 and ICU admission and mortality). In Table 1, the following dimensions were collected: study period, study design, study population, sample size, main outcomes and their measures of effect (in terms of incidence, prevalence, morbidity rates, rate ratios, odds ratios, relative risks and hazard ratios); the study quality in terms of risk of bias was also included in the table.
Results
Literature Search and Selection
The systematic search of the literature concerning the study question identified 5,321 records on databases; after the removal of 2,439 duplicates (2,045 automatically intercepted and 394 by title review), 2,882 records were screened by title and abstract. Two hundred fifty-three were found eligible for full text reading, and 6 more studies were added from the reference lists of the eligible studies. From the resulting 253 studies, 82 records met all the inclusion criteria and were analysed for a quality appraisal. Figure 1 shows the flow diagram of identified studies.
Sixty-two studies were considered ‘high quality’, 17 ‘medium quality’ and only three studies (3.6%) had a ‘low quality’ level. Table 1 shows the characteristics of the included studies.
No studies specifically concerning refugees were found. The studies investigating the migrant population compared to the native one, referred to migrants as persons born outside the country in object.
The findings have been reported according to the outcome taken into consideration as follows: hospital admission, severe Covid-19 and ICU admission and mortality.
Hospital Admission
We found 16 sources reporting the hospital admission rate and risk for Covid-19 among MEMs, including 10 from the UK, 1 from Norway, 3 from Italy and 2 international studies. Two of these regarded the paediatric population, 2 specific groups of patients with comorbidities and 12 the general adult population.
Fifteen studies out of 16 reported that MEMs had a higher risk of hospital admission for Covid-19 compared to native/White ethnicity. The hospitalisation rate varied markedly depending on ethnicity and country of birth. A cohort study from the UK (Sapey, 2020) reported a standardised admission ratio (SAR) for South Asian women 74% higher (SAR 1.7, 95% CI [1.5–2.0]) and for South Asian men 63% higher (SAR 1.6, 95% CI [1.4–1.9]) than the standard population (2011 census data by age and sex), while admission rates were similar to the expected rates of the standard population for Black ethnicity. Conversely, a second cohort study from the UK (Singh, 2021) found that the South Asian ethnic group was less likely to be hospitalised for Covid-19 compared with the White ethnic reference category (adjusted OR 0.56, 95% CI [0.44 to 0.70]), whereas the Black ethnic group had an increased risk (adjusted OR 2.08, 95% CI [1.70 to 2.57]). These findings were partially confirmed by two cohort studies (Atkins, 2020; Zakeri, 2020), where only Black ethnicity was associated with higher odds of admission (adjusted OR 2.85, 95% CI [1.71–4.74] and 3.1, 95% CI [2.6–3.7], respectively), whereas no increase in admission risk was associated with Asian ethnicity.
Two studies, that used the UK Biobank cohort as data source, reported that both Black (OR 3.1, 95% CI [2.0–4.8] [30] and 4.32, 95% CI [3.00–6.23] [31]) and Asian participants (OR 2.0, 95%CI [1.2–3.1] and 2.12, 95% CI [1.37–3.28]) were at increased risk of hospitalisation when compared to White participants.
A further cohort study (Clift, 2020), that used the UK Qresearch database, reported a higher adjusted hazard ratio (HR) of hospital admission for Covid-19 in the BAME (Black, Asian and minority ethnic) population compared to the White population, especially for the Caribbean (adjusted HR women 2.01, 95% CI [1.71–2.35] and men 2.29, 95% CI [1.99–2.63]) and the Black population (adjusted HR women 2.30, 95% CI [1.97–2.68] and men 2.59, 95% CI [2.27–2.97]).
These findings were also confirmed by an international cohort study (Lo, 2020): in the UK, the adjusted OR for Covid-19 requiring a hospital visit was elevated across ethnic minorities compared to non-Hispanic White participants (adjusted OR 2.11, 95% CI [1.81–2.46]).
Among the studies that described the immigrant population, a Norwegian register-based surveillance (Indseth, 2021) reported a higher number of hospitalisations relative to notified cases of Covid-19 in immigrants compared to non-immigrants, with an increased rate of hospitalisation in many immigrant groups when adjusted for age and sex, ranging from 7/100.000 (Polish-born immigrant group) to 354/100.000 (Somalian-born group) depending on the specific immigrant community, compared with the non-immigrant population that had a hospitalisation rate of 21 per 100.000.
In two Italian studies considering the adult population (Fabiani, 2021; Giorgi Rossi, 2020), immigration status was found to be associated with a higher risk of hospitalisation (adjusted RR 1.39, 95% CI [1.33–1.34] and HR 1.3, 95% CI [0.99 to 1.81], respectively), especially among non-Italian nationals from low Human Development Index (HDI) countries (adjusted RR 1.59, 95% CI [1.48–1.71]) (Fabiani, 2021).
Paediatric Population
The first of the two papers regarding the paediatric population (Felsenstein, 2020) found that, among 29 children admitted to tertiary paediatric centres in the English North West with a diagnosis of PIMS-TS (Paediatric Inflammatory Multisystem Syndrome Temporally associated with SARS-CoV-2), children of BAME background were overrepresented when compared to the composition of the general population in the region. The second one (Baronio, 2021) reported that among 111 children, the ratio of hospitalised foreign patients was significantly higher than expected when compared with the native Italian patients (OR 1.76, 95% CI [1.16–2.66]). Children from Africa had significant higher odds of being hospitalised with SARS-CoV-2 infection than Italian children (OR = 2.76, 95% CI [1.56–4.87]) and than all other foreign ethnicities combined (OR 2.03, 95% CI [1.00–4.13]).
Patients with Comorbidities
Among the studies that analysed patients with comorbidities, a study on a cohort of 39 patients with diabetes-related end stage renal disease (Corcillo, 2021) observed a high prevalence of patients of Afro-Caribbean ethnicity hospitalised with Covid-19 with a 73% and 54% prevalence in renal transplant and haemodialysis (HD) groups, respectively. This contrasted markedly with the much lower prevalence of Afro-Caribbean people in the renal transplant population attending the hospital for routine care (18% of renal transplant and 42% of HD patients of Afro-Caribbean origin).
Also, an international study (Mahil, 2021) on a total of 374 patients with psoriasis and confirmed or suspected Covid-19 from 25 countries stated that significant associations with increased hospitalisation rate were observed for non-White ethnicity (adjusted OR 3.15, 95% CI [1.24–8.03]) compared with the White one.
Only one UK study (Kakkar, 2020), on a cohort of 3,018 adult patients tested for Covid-19 at Sheffield Teaching Hospital, found no significant difference between BAME and White groups in terms of overall admissions (p=0.083).
Severe Covid-19 and ICU Admission
We retrieved 26 studies investigating severe consequences of Covid-19 and ICU admission rates among MEM population. Nineteen studies were conducted in the UK, two in Spain, two in Italy, and one in Ireland, Sweden and France, respectively.
Some studies conducted in the UK reported a higher ICU admission risk for Asian and Black (Lok, 2020) or overall BAME population (Bannaga, 2020; Baumer, 2020; Dennis, 2021; Galloway, 2020; Gopal-Rao, 2021; Harrison, 2020; Hippisley-Cox, 2020; Richards-Belle, 2020). On the other hand, among patients admitted to ICU with other viral pneumonias, the proportion of non-White patients was smaller (11.2% versus 32.6%) (Richards-Belle, 2020).
Regarding presenting symptoms and the need for invasive treatments, in a multicentre cohort study (Papageorgiu, 2020), Asian patients presented more frequently with deep vein thrombosis and/or pulmonary embolism (adjusted OR 4.10, 95% CI [1.49–11.27]) and had a higher rate of mechanical ventilation (p=0.007). Afro-Caribbeans required more frequently urgent renal replacement therapy (adjusted OR 2.11, 95% CI [1.15–3.86]), had a higher risk of cardiovascular consequences and resorted more often to ECMO (extracorporeal membrane oxygenation) (p=0.014). According to Apea et al. (Apea, 2021), both Asian and Black patients were more likely to receive invasive ventilation (OR 1.54, 95% CI [1.06–2.23] and OR 1.80, 95% CI [1.20–2.71], respectively). Dite et al. (Dite, 2021) found a 43% increased risk for severe Covid-19 among non-Whites (adjusted OR 1.43, 95% CI [0.99–2.05]), even though with marginal significance (p=0.06). Conversely, Harrison et al. (Harrison, 2020) found no significant differences in the distribution of severity scores at hospital admission between ethnic groups. However, abnormal liver function during hospitalisation for Covid-19 (Lok, 2020) was more common among Asian patients compared with White ones (59.0% vs 39.8%, p=0.026). Being from sub-Saharan African origin was independently associated with severe and critical forms of Covid-19 in patients living with HIV (Etienne, 2020). Compared with the French whole out-patient population, the proportion of Covid-19 patients in those from sub-Saharan African origin was higher (44.6 vs 29.7%) and these patients counted for 31.4% of those with moderate, 57.1% with severe and 100% with critical Covid-19 (p=0.08). According to a Swedish study (Svensson, 2021), among patients with a region of birth outside the EU15Footnote 1, diabetes had a stronger association with severe Covid-19 compared with patients born within EU15 (p=0.004). An Italian study (Fabiani, 2021) reported a higher ICU admission rate in non-Italian compared to Italian nationals (adjusted RR 1.19, 95% CI [1.07–1.32]), particularly in those from medium and low HDI countries (adjusted RR 1.25, 95% CI [1.11–1.42] and adjusted RR 1.16, 95% CI [0.93–1.44], respectively). A study conducted in Spain (Norman, 2021) underlines that ICU admission was more frequent in non-Europeans (OR 1.43, 95% CI [1.03–1.98]). Also, in another study from Ireland (Farrell, 2021), compared with White Irish patients, all other ethnic groups, including other White and BAME, had an approximately fourfold increased risk of ICU admittance after adjusting for age (adjusted HR=4.22, 95% CI [1.45–12.31] and 4.58, 95% CI [1.33, 15.84], respectively).
Paediatric Population
Two articles (Davies, 2020; Felsenstein, 2020) analysed cohorts of children under 18 years of age with PIMS-TS. Asian and Afro-Caribbean patients were over-represented (28% Asian and 47% Afro-Caribbean), despite accounting for 7% and 8% of the UK population, respectively. Out of 78 PIMS-TS children, 61 (78%) were of ethnic minorities (Davies, 2020). They were also more likely to present with clinical signs of hypoperfusion or shock (p=0.04) and abnormalities on echocardiogram (p=0.02) (Felsenstein, 2020). Moreover, BAME children were at higher risk of PIMS-TS (p=0.004), and children with this syndrome showed higher ICU admission rates (p<0.001) (Swann, 2020).
Six papers did not report any increased risk for people from ethnic minorities. Russell et al. (Russel, 2020) found no increased risk of severe Covid-19 in ethnic minorities compared to White patients, and Patel et al. (Patel A, 2020) and Staines et al. (Steines, 2021) delineated no difference for ICU admission risks. A study conducted in Spain (Guijarro, 2021) reported the unadjusted rate of ICU admission as being higher for Spaniards (63%) compared to migrants (33%). Canevelli et al. (Canevelli, 2020) found no significant difference between people with a migration background and native Italian individuals regarding admission to ICU, times to clinical milestones (all p>0.05) and proportion of development of ARDS (acute respiratory distress syndrome) (97.0% of natives and 96.9% of migrants). According to a UK study, ethnicity does not appear to be an independent risk factor for developing acute kidney failure (AKI) with Covid-19 either (p=0.443) (Kolhe, 2020).
Mortality
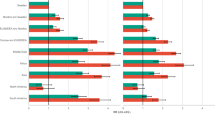
The research retrieved 65 studies investigating the difference in mortality risk between MEMs and non-ethnic-minority populations, of which 43 documented an association between mortality and being MEMs.
Several studies reported an overall increased mortality for BAME population after adjusting for age and sex (Apea, 2021), comorbidities (Alaa, 2020; Papageorgiu, 2020) and socio-economic characteristics (Batty, Deary et al., 2021; Nikoloudis, 2020; Perkin, 2020; Williamson, 2020). Among those observing a higher mortality rate in the BAME population, 9 found the Asian ethnicity to be at increased risk of mortality than other ethnic minorities, compared to the White population. A cohort study and an observational retrospective study from the UK reported that the Asian population had greater odds of death compared to White people (adjusted OR 1.99, 95% CI [1.22–3.25] (Patel A, 2020) and adjusted OR 1.21, 95% CI [1.13–1.30] (Navaratnam, 2021), respectively), compared to other ethnic minorities. This was also confirmed by Ferrando-Vivas (Ferrando-Vivas, 2021) and Cheng (Cheng, 2021), who, in a multivariable Cox proportional hazards model for death within 30 days of start of critical care, observed that patients with an Asian background had an adjusted HR of 1.27, 95% CI [1.15–1.40] and HR 1.40, 95% CI [1.08 to 1.81], respectively. This last result was corroborated by a sensitivity analysis conducted, restricted to PCR-confirmed Covid-19 patients, among which people of Asian ethnicity had higher mortality risk (HR 1.5, 95% CI [1.1 to 2.1]) (Cheng 2021). Other cohort studies from the UK analysed different Asian subgroups of population and found in multivariable models that South Asian ethnicity was associated with a significantly higher risk of death (adjusted HR 1.4, 95% CI [1.2 to 1.8] [26]; adjusted HR 1.19, 95% CI [1.05 to 1.36] (Harrison, 2020); adjusted HR 2.00, 95% CI [1.13–3.51] (Miles, 2020), respectively), compared to the White group. In other studies, the Black population was found to be at increased risk of death, with adjusted OR ranging from 1.17, 95% CI [1.03–1.33], to 3.44, 95% CI [1.48–8.00] (Atkins, 2020; de Lusignan, 2020; Elliott, 2021; Joy, 2020; Kuo, 2021; Perez-Guzman, 2021; Singh, 2021). Although Singh et al. (Singh, 2021) pointed out the non-significant association between in-hospital Covid-19 case fatality and ethnicity in general, the Black population showed higher absolute and adjusted mortality occurred in the Black population compared to White people and other ethnic minorities. Batty et al. (Batty, Gaye et al., 2021) reported a higher mortality risk adjusted for sex and age for both Black and Asian patients (age and sex adjusted OR 7.25; 4.65, 11.33 and 1.98; and 1.02 and 3.84, respectively). After a separate adjustment for lifestyle, socio-economic factors and comorbidities, the association resulted significant only in the Black population (adjusted OR 4.29, 95% CI [2.67–6.88]). Moreover, the risks across ethnic groups were analysed in detail. In a cross-sectional study conducted in the UK (Clough, 2021), Bangladeshi/Pakistani, Black and Indian ethnic groups (for both sexes) had increased adjusted odds of dying from Covid-19 when compared with a baseline White group. These findings were confirmed by Aldridge (2020) and Platt (2020), who reported an increased risk of death for Black Africans, Pakistanis, Black Caribbeans, Indians and Bangladeshi ranging from 1.7 to 4.1. In a cross-sectional study on 52 patients admitted to ICU in the Royal Gwent Hospital (Baumer, 2020), people of BAME minority ethnic descent represented 35% of deaths (6 of 17) and 72% (13 of 18) of BAME patients were found to reside in geographical areas representing the 20% most deprived in Wales. Findings of an ecological study confirmed that areas with higher percentages of Black and Asian (except Chinese) ethnic groups had higher mortality rates (Harris, 2020). According to Daras et al. (Daras, 2021), each standard deviation increase in the proportion of BAME population was associated with a 8% increase in the Covid-19 mortality rate (IRR 1.08, 95% CI 1.03 to 1.13). Likewise, each 1% increase in the proportion of BAME population was associated with a 1% increase in the Covid-19 mortality rate (IRR 1.01, 95% CI 1.01 to 1.02) (Rose, 2020) or an increase in Covid-19-related deaths by 5.12 (95% CI [4.00 to 6.24]), per million (Nazroo, 2020). Moreover, a negative association between the proportion of White people and rate of death related to Covid-19 was found (r=−0.6) (Bray, 2020). A fully adjusted model (Ayoubkhani, 2021) described the mortality HRs as higher for Black females (HR 1.29, 95% CI [1.18–1.42] and for Black (HR 1.76, 95% CI [1.63–1.90], Bangladeshi/Pakistani (HR 1.35, 95% CI [1.21 to 1.49] and Indian (HR 1.30, 95% CI [1.19 to 1.43]) males compared to the White counterparts (Ayoubkhani, 2021). In a UK cohort study of 13,500 consultant physicians aged 50–59 years (Verma, 2021), the authors highlighted the striking effects of ethnicity on the risk of Covid-19-related death for both BAME men (ranging from HR 1.59 to 2.35) and women (ranging from HR 1.33 to 1.48) compared to the White population. Similar observations were reported by another UK cohort study (Clift, 2020), according to which men and women of BAME background registered higher risks of Covid-19-related death compared to White counterparts. However, men of each ethnic group taken into consideration had a greater HR of death than women (women of Indian 1.89, 95% CI [1.43–2.51], Caribbean 1.68, 95% CI [1.29–2.20], Black African 1.98, 95% CI [1.39–2.83], and other ethnic groups 1.73, 95% CI [1.28–2.35] compared to white women; men of Indian 1.59, 95% CI [1.25–2.01], Pakistani 1.84, 95% CI [1.39–2.44], Bangladeshi 2.27, 95% CI [1.65–3.12], other Asian 2.02, 95% CI [1.49–2.74], Caribbean 2.06, 95% CI [1.6–2.57], Black African 3.03, 95% CI [2.42–3.80], Chinese 2.47, 95% CI [1.49–4.09] and other ethnic groups 2.04, 95% CI [1.60–2.58] compared to White men).
The research retrieved only four studies conducted outside the UK reporting an increased mortality risk for migrants compared to the native population, two from Sweden and two from Italy. Drefahl et al. (Drefahl, 2020) observed that immigrants from low- and middle-income countries (LIC and MIC) of the Middle East and Northern Africa displayed more than three times higher mortality among men (HR 3.13, 95% CI [2.51–3.90]) and two times higher among women (HR 2.09, 95% CI [1.52–2.89]), whereas immigrants from other LIC and MIC experienced a mortality risk more than doubled among men (HR 2.20, 95% CI [1.81–2.69]) and almost a 1.5 times higher among women (HR 1.45, 95% CI [1.12–1.90]), compared to those born in Sweden. Male immigrants from high-income countries displayed 19% higher mortality (HR 1.19, 95% CI [1.01–1.39]). Also, an Italian cross-sectional study (Fabiani, 2021) observed a higher fatality rate between non-Italian nationals from low HDI countries compared to Italian nationals (adjusted RR 1.32, 95% CI [1.01–1.75]). In the other Swedish study (Rostila, 2021), in a sample of people aged more than 21 years, the authors reported higher mortality rate ratios among migrants from the Middle East (adjusted RR 1.96, 95% CI [1.56–2.46]), Africa (adjusted RR 1.70, 95% CI [1.17–2.47]) and non-Sweden Nordic countries (adjusted RR 1.25, 95% CI [1.03–1.52]) than persons born in Sweden. These findings were confirmed by the sensitivity analysis.
An Italian ecological study (Di Girolamo, 2020) delineates a positive monotonic gradient for Covid-19 mortality by the percentage of foreign resident population, considered a proxy for social and economic disadvantage. All the ecological measures were grouped in population quintiles of the regional distribution. Mortality rate ratios (MRRs) were found to be significantly increased in the fourth and fifth quintiles for men (Q4: 1.34, 95% CI [1.16–1.54]; Q5: 1.57, 95% CI [1.37–1.80]) and in the fifth one for women (Q5: 1.20, 95% CI [1.02–1.42]), compared to the respective first quintile.
Patients with Comorbidities
In a population of cancer patients (Russell, 2020) being of Asian ethnicity had a positive association with risk of Covid-19 death as compared to White (HR 3.73, 95% CI [1.28–10.91]) and in a retrospective cohort study on patients in haemodialysis (Savino, 2020), Asian patients with Covid-19 were found to have a ‘borderline’ 16% higher mortality risk (HR 1.16 CI 0.94–1.44) than White patients. A strong significant interaction (p-interaction=0.002) was also found between the body mass index and non-Whites in increasing the risk of death for Covid-19 (Sattar, 2020). Concerning patients with a diagnosis of both type 1 and 2 diabetes, Covid-19-related mortality was found to be significantly higher in people of Black and Asian ethnicities than in those of White ethnicity (type 1 diabetes: adjusted HR 1.77, 95% CI [1.25–2.49] and adjusted HR 1.57, 95% CI [1.16–2.12], respectively, and type 2 diabetes: adjusted HR 1.63, 95% CI [1.51–1.77] and adjusted HR 1.08, 95% CI [1.01–1.15], respectively) (Holman, 2020). Barron et al. (Barron, 2020) reported higher odds for Covid-19-related death for BAME population both with and without diabetes, with a general adjusted OR of 1.35, 95% CI [1.28–1.42] for Asian people, 1.71, 95% CI [1.61–1.82] for Black people, 1.43, 95% CI [1.23–1.67] for mixed and 1.10, 95% CI [1.01–1.20] for other ethnic minorities. However, a study reported no increased mortality for non-White ethnicity compared to White in patients with type 2 diabetes (p=0.08) (Dennis, 2021).
Twenty-one studies did not report an increased mortality risk for people with an ethnic minority background (Aw, 2020; Bannaga, 2020; Canevelli, 2020; Davies, 2021; Dennis, 2021; Farrell, 2021; Galloway, 2020; Giorgi-Rossi, 2020; Gopal-Rao, 2021; Guijarro, 2021; Ken-Dror, 2020; Kolhe, 2020; Livingston, 2020; Moody, 2021; Norman, 2021; Santorelli, 2020; Staines, 2021; Saban & Wilf-Miron, 2020; Thompson, 2020; Zakeri, 2020), and although Thomson et al. (Thomson, 2020) found an association in the univariable analysis between Asian ethnicity and death (OR 2.57, 95% CI 1.02–6.57), in the multivariable model, this finding was not significant (Asian OR 2.94, 95% CI 0.94–9.78).
Discussion
This systematic review aims at investigating the differential risk of Covid-19 adverse outcomes between MEMs compared to the non-migrant population in the countries of the European Region of WHO. As stated in a previous systematic review (Jaljaa, 2022), this geographical restriction was an attempt to limit the heterogeneity of the target population among different countries.
The various outcomes that emerged from the research have been grouped and reported in the current study as follows: hospital admission, admission to ICU and/or severe Covid-19 symptoms and mortality. Most of the 82 studies included reported an increased risk for adverse outcomes for the MEM population.
Clinical Outcomes
Differences in hospitalisation rates were considered by 16 studies, those on ICU admission and severe outcomes by 26 studies and differences in mortality risks by 65 studies. Among these, 24 studies investigated more than one outcome. Overall, most studies focused on the differences in the mortality risk.
Even if the research highlighted a clear enhanced risk of adverse outcome and mortality due to Covid-19, the consistency among the studies differs, depending on the outcome taken into consideration.
Regarding hospital admission, almost all the papers reported an increased risk of hospitalisation for MEMs, except one (Kakkar, 2020). However, this study lacked adjusted measures and had a ‘low-quality’ rating according to our quality evaluation.
Among the studies considering ICU admission rates and other severe outcomes, 21 out of 26 studies showed an increased risk of ICU admission and 43 studies out of 65 reported an increased risk of mortality for MEM people. Therefore, a consistent enhanced risk of adverse outcomes for MEMs resulted throughout all the variables considered.
The main factors implied in the genesis of health inequalities identified throughout the retrieved literature are defined as the social determinants of health (SDH). It is well recognised by the scientific community that SDH is deeply involved in shaping the health condition of the individual and the communities and social deprivation has been associated with increased risk of SARS-CoV-2 infection and Covid-19 (Morante-García, 2022; Patel JA, 2020). Indeed, MEM people are usually over-represented among key workers, in low income and/or in public-facing jobs, in precarious contracts or self-employed and they live in larger, intergenerational crowded housing (Lassale, 2020). They are also more likely to present lower levels of language proficiency, which constitute a barrier in accessing health information and leads, therefore, to a lower health literacy (Hayward, 2021; WHO, 2022a, 2022b). Moreover, if not legally resident, migrants may be frightened to access official healthcare services due to fear of legal consequences or repatriation (WHO, 2020).
These factors contribute to increasing the risk of infection of SARS-CoV-2 among this population (Jaljaa, 2022) but might also be involved in the worse clinical presentation and the faster progression of Covid-19 disease (Bambra 2020; Fiorini, 2020) among this group. Barriers such as language, administrative, legal, cultural and social and the fear of a restriction of working activities due to isolation/quarantine may have been obstacles to the early access to healthcare services, thus, leading to a delayed diagnosis (Baumer, 2020; Fabiani, 2021). As reported in studies from the UK, it is also possible that, in areas with MEMs population, an asymmetrical access to healthcare or the quality of care itself could heighten the risk of infection, hospitalisation and mortality (Gopal-Rao, 2021). In addition, a disadvantaged socio-economic status, also supported by structural racism, is likewise related to the higher comorbidity rates observed among MEM population, increasing the susceptibility to poor outcomes consequent to Covid-19 infection (Lo, 2020).
However, even if the hospital and ICU admission is higher for the target population, some studies do not register a subsequent increase in mortality rates (Bannaga, 2020; Gopal-Rao, 2021; Papageorgiu, 2020). These findings were attributed to the small sample size (Bannaga, 2020), and the low overall mortality rates reported by the study (Gopal-Rao, 2021), that could not help in highlighting the possible differences. Some authors justified the fact by clarifying that elderly European patients with severe disease were not being considered for ICU at the beginning of the pandemic, or that, since an increase in comorbidities in the non-European group admitted to ICU should probably have led to worse outcomes and a higher mortality, which was not observed; other determinants, such as genetic factors, may also be playing a role in the outcome for these patients (Norman, 2021). Some other authors left the finding without a proper explanation (Dennis, 2021; Farrell, 2021; Galloway, 2020). On the other hand, Patel addressed physiological factors—such as increased comorbidity burden and/or delayed hospital presentation, as precluding factors for MEM group from critical care. Social and cultural factors such as family and support networks may affect healthcare accessibility which may also impact outcomes (Patel A, 2020).
Some authors identify the different biological susceptibilities of distinct ethnic minorities as a key factor in the interpretation of the higher rates of negative consequences of Covid-19 (Davies, 2020; Norman, 2021). However, regardless of the biological susceptibility factors, the variables that influence the degree of control that individuals exert on their own lives can affect their ability to cope with the biological factors. These variables are identified in the socio-economic conditions which characterise health status. Each factor that disrupts the balance in the coping ability influences the frailty of the individual, worsening health conditions and outcomes (Costa, 2020). The interaction between social components and pre-existing medical conditions which causes a worsening in clinical outcomes, as occurred during the current pandemic, relates to the notion of syndemic (Horton, 2020). Interestingly, especially with regard to the mortality risk, wide differences between ethnic groups were highlighted. The reasons behind these findings could be various and heterogeneous, and further qualitative and quantitative studies are needed to better interpret the phenomenon.
Another factor playing a significant role is the different groupage operated by the researchers, where populations with differences in social, biological conditions and migration histories are included in the same broad category, as ‘Asian’, ‘Black’ and a generic ‘other ethnic minorities’.
Just four studies (Baronio, 2021; Davies, 2020; Felsenstein, 2020; Swann, 2020) focused on the paediatric population. For this reason, it is premature to draw any conclusion and we await a larger body of scientific evidence.
Even though the research was performed in the same days as the one investigating the difference in the risk of SARS-CoV-2 infection (Jaljaa, 2022), the total number of articles retrieved was more than three times higher. The reason could be a higher interest in clinical outcomes related to Covid-19 compared to risk of infection or could also be explained by the fact that hospitals were hit by a massive wave of hospitalisation of Covid-19 patients and the healthcare professionals were focused on reducing the mortality rate. Likewise, the scientific production was directed to this issue (De Felice & Polimeni, 2020; Nowakowska, 2020). Indeed, the articles included in the review considered a timeframe between January and October 2020, which corresponds to the first wave of Covid-19 contagions in the European region, when the immunisation through vaccination was not yet available.
However, even though the European Region of WHO includes 53 countries, the research gathered publications from just eight of them and 81.7% of the studies were conducted in the UK. In this country, the National Healthcare Service (NHS) has information and databases which are more structured and accessible compared to other countries, and do not face comparable difficulties of retrieving ethnicity data for public health purposes.
The current policy in force in some of these nations hinders the collection of data on the ethnicity of the individuals (Balestra & Fleischer, 2018). Even if the clear aim of this policy is to protect those groups of people historically victims of prejudices, it also prevents the researchers from obtaining the required information to properly study their conditions and needs. These data turn out to be essential to formulate adequate social and political responses to the issues raised also by the current pandemic.
Nevertheless, the results of this review highlighted the necessity to take into account the socio-economic barriers that MEMs face, in achieving and preserving their health status. These factors have to be considered by policymakers in developing public health prevention plans.
Strengths and Limitations
This systematic review is one of the few conducted on the topic (Agyemang, 2021; Hayward, 2021). It is the only one focused specifically on the European Region of the WHO and on both migrants and ethnic minorities. Moreover, the time span taken into consideration was longer, up to the first months of 2021, whereas Agyemang et al. included articles published up to September 2020 and Hayward et al. up to November 2020. The results of the three reviews are consistent in terms of the increased risk of severe consequences of Covid-19 among migrants (Hayward 2021) and ethnic minorities (Agyemang 2021).
Furthermore, this is the second part of a three-query research which aims at providing a thorough picture of the impact of the Covid-19 pandemic on MEM population from the aspects of risk of infection, risk of adverse clinical outcomes and the achievement of healthcare services and vaccination. The research group working on this study is composed of different professional figures operating in various fields related to migration and public health, thus bringing the value of a holistic point of view to the subject.
We also recognise some limitations. Most of the studies identified White ethnicity as the population of comparison, although the definition of ‘White ethnicity’ is broad and does not allow one to distinguish the possible migration background within this group.
On the other hand, the definition of migrant and ethnic minority is loose, meaning that the quantity and quality of the composition of the MEM population can be very different from one place to another. This, therefore, challenges the interpretation of the higher risk of negative outcomes due to Covid-19 in this population.
Nevertheless, we believe that this enhanced risk of Covid-19 severe outcomes and mortality in migrant and ethnic minorities compared to the general population in the European WHO region can be attributed to the unequal distribution of the social determinants of health, since MEM population belongs more often to the most socio-economic disadvantaged section of the population.
Conclusion
The findings of this systematic review highlight the disproportionate impact of Covid-19 on MEM population in terms of clinical consequences.
It raises, therefore, the urgent need for healthcare policies to take into consideration the higher vulnerability of these people to SARS-CoV-2 infection and worse Covid-19 clinical outcomes and to aim at tackling the socio-economic gradient, acknowledged cause of health inequalities.
Hence, we recommend conducting similar studies to be conducted in countries where the number of publications on this issue is still very scarce or inexistent.
Notes
The EU15 comprised the following 15 countries: Austria, Belgium, Denmark, Finland, France, Germany, Greece, Ireland, Italy, Luxembourg, Netherlands, Portugal, Spain, Sweden and the UK. Glossary of statistical terms, OECD.
Abbreviations
- MEMs:
-
migrants and ethnic minorities
- SARS-CoV-2:
-
severe acute respiratory syndrome coronavirus-2
- WHO:
-
World Health Organisation
- PRISMA:
-
Preferred Reporting Items for Systematic Reviews and Meta-Analyses
- IOM:
-
International Organisation for Migration
- RR:
-
relative risk
- OR:
-
odds ratio
- UK:
-
United Kingdom
- BAME:
-
Black, Asian and minority ethnic
- BMI:
-
body mass index
- HR:
-
hazard ratio
- NHS:
-
National Health Service
- PCR:
-
polymerase chain reaction
- HCWs:
-
healthcare workers
- PPE:
-
personal protective equipment
References
Abubakar, I., Aldridge, R. W., Devakumar, D., Orcutt, M., Burns, R., Barreto, M. L., Dhavan, P., Fouad, F. M., Groce, N., Guo, Y., Hargreaves, S., Knipper, M., Miranda, J. J., Madise, N., Kumar, B., Mosca, D., McGovern, T., Rubenstein, L., Sammonds, P., Sawyer, S. M., Sheikh, K., Tollman, S., Spiegel, P., Zimmerman, C., & UCL-Lancet Commission on Migration an Health. (2018). The UCL–Lancet Commission on Migration and Health: The health of a world on the move. The Lancet, 392(10164), 2606–2654. https://doi.org/10.1016/S0140-6736(18)32114-7
Alaa, A., Qian, Z., Rashbass, J., Benger, J., & van der Schaar, M. (2020). Retrospective cohort study of admission timing and mortality following COVID-19 infection in England. BMJ Open, 10(11), e042712. https://doi.org/10.1136/bmjopen-2020-042712
Aldridge, R. W., Lewer, D., Katikireddi, S. V., Mathur, R., Pathak, N., Burns, R., Fragaszy, E. B., Johnson, A. M., Devakumar, D., Abubakar, I., & Hayward, A. (2020). Black, Asian and minority ethnic groups in England are at increased risk of death from COVID-19: Indirect standardisation of NHS mortality data. Wellcome Open Res., 5, 88. https://doi.org/10.12688/wellcomeopenres.15922.2
Agyemang, C., Richters, A., Jolani, S., Hendriks, S., Zalpuri, S., Yu, E., Pijls, B., Prins, M., Stronks, K., & Zeegers, M. P. (2021). Ethnic minority status as social determinant for COVID-19 infection, hospitalisation, severity, ICU admission and deaths in the early phase of the pandemic: A meta-analysis. BMJ Glob. Health, 6(11), e007433. https://doi.org/10.1136/bmjgh-2021-007433
Apea, V. J., Wan, Y. I., Dhairyawan, R., Puthucheary, Z. A., Pearse, R. M., Orkin, C. M., & Prowle, J. R. (2021). Ethnicity and outcomes in patients hospitalised with COVID-19 infection in East London: An observational cohort study. BMJ Open, 11(1), e042140. https://doi.org/10.1136/bmjopen-2020-042140
Atkins, J. L., Masoli, J. A. H., Delgado, J., Pilling, L. C., Kuo, C. L., Kuchel, G. A., & Melzer, D. (2020). Preexisting comorbidities predicting COVID-19 and mortality in the UK Biobank community cohort. J. Gerontol. A Biol. Sci. Med. Sci., 75(11), 2224–2230. https://doi.org/10.1093/gerona/glaa183
Aw, D., Woodrow, L., Ogliari, G., & Harwood, R. (2020). Association of frailty with mortality in older inpatients with Covid-19: A cohort study. Age Ageing, 49(6), 915–922. https://doi.org/10.1093/ageing/afaa184
Ayoubkhani, D., Nafilyan, V., White, C., Goldblatt, P., Gaughan, C., Blackwell, L., Rogers, N., Banerjee, A., Khunti, K., Glickman, M., Humberstone, B., & Diamond, I. (2021). Ethnic-minority groups in England and Wales-factors associated with the size and timing of elevated COVID-19 mortality: A retrospective cohort study linking census and death records. Int. J. Epidemiol., 49(6), 1951–1962. https://doi.org/10.1093/ije/dyaa208
Balestra, C., & Fleischer, L. (2018). Diversity statistics in the OECD: How do OECD countries collect data on ethnic, racial and indigenous identity? In OECD Statistics Working Papers, No. 2018/09. OECD Publishing. https://doi.org/10.1787/89bae654-en
Bambra, C., Riordan, R., Ford, J., & Matthews, F. (2020). The COVID-19 pandemic and health inequalities. J. Epidemiol. Community Health, 74(11), 964–968. https://doi.org/10.1136/jech-2020-214401
Bannaga, A. S., Tabuso, M., Farrugia, A., Chandrapalan, S., Somal, K., Lim, V. K., Mohamed, S., Nia, G. J., Mannath, J., Wong, J. L., Noufaily, A., Disney, B. R., & Arasaradnam, R. P. (2020). C-reactive protein and albumin association with mortality of hospitalised SARS-CoV-2 patients: A tertiary hospital experience. Clin. Med. (Lond.), 20(5), 463–467. https://doi.org/10.7861/clinmed.2020-0424
Baronio, R., Savaré, L., Ruggiero, J., Crotti, B., Mazza, A., Marseglia, G. L., Dodi, I., Cavalli, C., & Schumacher, R. F. (2021). Impact of ethnicity on COVID-19 related hospitalizations in children during the first pandemic wave in Northern Italy. Front. Pediatr., 9, 625398. https://doi.org/10.3389/fped.2021.625398
Barron, E., Bakhai, C., Kar, P., Weaver, A., Bradley, D., Ismail, H., Knighton, P., Holman, N., Khunti, K., Sattar, N., Wareham, N. J., Young, B., & Valabhji, J. (2020). Associations of type 1 and type 2 diabetes with COVID-19-related mortality in England: A whole-population study. Lancet Diabetes Endocrinol., 8(10), 813–822. https://doi.org/10.1016/S2213-8587(20)30272-2
Batty, G. D., Deary, I. J., & Gale, C. R. (2021). Pre-pandemic cognitive function and COVID-19 mortality: Prospective cohort study. Eur. J. Epidemiol., 36(5), 559–564. https://doi.org/10.1007/s10654-021-00743-7
Batty, G. D., Gaye, B., Gale, C. R., Hamer, M., & Lassale, C. (2021). Explaining ethnic disparities in COVID-19 mortality: Population-based, prospective cohort study. medRxiv, 10. https://doi.org/10.1101/2021.02.07.21251079
Baumer, T., Phillips, E., Dhadda, A., & Szakmany, T. (2020). Epidemiology of the first wave of COVID-19 ICU admissions in South Wales-The interplay between ethnicity and deprivation. Front Med (Lausanne), 7, 569714. https://doi.org/10.3389/fmed.2020.569714
Bozorgmehr, K., Biddle, L., Rohleder, S., Puthoopparambil, S. J., & Jahn, R. (2019). What is the evidence on availability and integration of refugee and migrant health data in health information systems in the WHO European Region? Themed issues on migration and health, X. WHO Regional Office for Europe.
Bray, I., Gibson, A., & White, J. (2020). Coronavirus disease 2019 mortality: A multivariate ecological analysis in relation to ethnicity, population density, obesity, deprivation and pollution. Public Health, 185, 261–263. https://doi.org/10.1016/j.puhe.2020.06.056
Canevelli, M., Palmieri, L., Raparelli, V., Punzo, O., Donfrancesco, O., Lo Noce, C., Vanacore, N., Brusaferro, S., Onder, G., et al. (2020). COVID-19 mortality among migrants living in Italy. Annali dell’Istituto superiore di sanita, 56(3), 373–377. https://doi.org/10.4415/ANN_20_03_16
Cheng, D., Calderwood, C., Skyllberg, E., & Ainley, A. (2021). Clinical characteristics and outcomes of adult patients admitted with COVID-19 in East London: A retrospective cohort analysis. BMJ Open Respir. Res., 8(1). https://doi.org/10.1136/BMJRESP-2020-000813
Clift, A. K., Coupland, C. A. C., Keogh, R. H., Diaz-Ordaz, K., Williamson, E., Harrison, E. M., Hayward, A., Hemingway, H., Horby, P., Mehta, N., Benger, J., Khunti, K., Spiegelhalter, D., Sheikh, A., Valabhji, J., Lyons, R. A., Robson, J., Semple, M. G., Kee, F., et al. (2020). Living risk prediction algorithm (QCOVID) for risk of hospital admission and mortality from coronavirus 19 in adults: National derivation and validation cohort study. BMJ, 371, m3731. https://doi.org/10.1136/bmj.m3731
Clough, H. E., McIntyre, K. M., Patterson, G. E., Harris, J. P., & Rushton, J. (2021). Use of routine death and illness surveillance data to provide insight for UK pandemic planning: Lessons from COVID-19. BMJ Open, 11(2), e044707. https://doi.org/10.1136/bmjopen-2020-044707
Corcillo A, Cohen S, Game D, Karalliedde J. H. (2021). Prevalence of Afro-Caribbean ethnicity and hypoglycaemia in patients with diabetes and end stage renal disease hospitalized with COVID-19. Nephrology (Carlton), 26(3):252-254. doi: https://doi.org/10.1111/nep.13809.
Corvacho, M., & França, G. (2021). The hidden damage of the COVID-19: The impact of the pandemic on migrants and ethnic minorities. Public Health Pract (Oxf), 2, 100184. https://doi.org/10.1016/j.puhip.2021.100184
Costa, G. (2020). Vulnerability and frailty in public health, in health policies, and in study methods. Epidemiol. Prev., 44(5–6), 14–17. https://doi.org/10.19191/EP20.5-6.S1.P014.069
Critical Appraisal | Read Clinical Papers With Confidence. (2022). https://www.criticalappraisal.com/?gclid=CjwKCAjwuYWSBhByEiwAKd_n_uOq7FRXcyHexVDRPjVwCAc4tvNTHm2XZZbwefzBhjkOHmSTWEfoxhoCrl8QAvD_BwE
Daras, K., Alexiou, A., Rose, T. C., Buchan, I., Taylor-Robinson, D., & Barr, B. (2021). How does vulnerability to COVID-19 vary between communities in England? Developing a small area vulnerability index (SAVI). J. Epidemiol. Community Health, 75(8), 729–734. https://doi.org/10.1136/jech-2020-215227
Davies, P., Evans, C., Kanthimathinathan, H. K., Lillie, J., Brierley, J., Waters, G., Johnson, M., Griffiths, B., du Pré, P., Mohammad, Z., Deep, A., Playfor, S., Singh, D., Inwald, D., Jardine, M., Ross, O., Shetty, N., Worrall, M., Sinha, R., et al. (2020). Intensive care admissions of children with paediatric inflammatory multisystem syndrome temporally associated with SARS-CoV-2 (PIMS-TS) in the UK: A multicentre observational study. Lancet Child Adolesc Health, 4(9), 669–677. https://doi.org/10.1016/S2352-4642(20)30215-7
Davies, N. G., Jarvis, C. I., CMMID COVID-19 Working Group, Edmunds, W. J., Jewell, N. P., Diaz-Ordaz, K., & Keogh, R. H. (2021). Increased mortality in community-tested cases of SARS-CoV-2 lineage B.1.1.7. Nature, 593(7858), 270–274. https://doi.org/10.1038/s41586-021-03426-1
De Felice, F., & Polimeni, A. (2020). Coronavirus disease (COVID-19): A machine learning bibliometric analysis. In Vivo, 34(3 suppl), 1613–1617. https://doi.org/10.21873/INVIVO.11951
de Lusignan, S., Joy, M., Oke, J., McGagh, D., Nicholson, B., Sheppard, J., Akinyemi, O., Amirthalingam, G., Brown, K., Byford, R., Dabrera, G., Krajenbrink, E., Liyanage, H., LopezBernal, J., Okusi, C., Ramsay, M., Sherlock, J., Sinnathamby, M., Tsang, R. S. M., et al. (2020). Disparities in the excess risk of mortality in the first wave of COVID-19: Cross sectional study of the English sentinel network. J. Infect., 81(5), 785–792. https://doi.org/10.1016/j.jinf.2020.08.037
Dennis, J. M., Mateen, B. A., Sonabend, R., Thomas, N. J., Patel, K. A., Hattersley, A. T., Denaxas, S., AP, M. G., & Vollmer, S. J. (2021). Type 2 diabetes and COVID-19-related mortality in the critical care setting: A national cohort study in England, March-July 2020. Diabetes Care, 44(1), 50–57. https://doi.org/10.2337/dc20-1444
Dennis, J. M., McGovern, A. P., Vollmer, S. J., & Mateen, B. A. (2021). Improving survival of critical care patients with coronavirus disease 2019 in England: A national cohort study, March to June 2020. Crit. Care Med., 49(2), 209–214. https://doi.org/10.1097/CCM.0000000000004747
Di Girolamo, C., Bartolini, L., Caranci, N., & Moro, M. L. (2020). Socioeconomic inequalities in overall and COVID-19 mortality during the first outbreak peak in Emilia-Romagna Region (Northern Italy). Epidemiol. Prev., 44(5-6 Suppl 2), 288–296. https://doi.org/10.19191/EP20.5-6.S2.129
Dite, G. S., Murphy, N. M., & Allman, R. (2021). An integrated clinical and genetic model for predicting risk of severe COVID-19: A population-based case-control study. PLoS One, 16(2), e0247205. https://doi.org/10.1371/journal.pone.0247205
Drefahl, S., Wallace, M., Mussino, E., Aradhya, S., Kolk, M., Brandén, M., Malmberg, B., & Andersson, G. (2020). A population-based cohort study of socio-demographic risk factors for COVID-19 deaths in Sweden. Nat. Commun., 11(1), 5097. https://doi.org/10.1038/s41467-020-18926-3
ECDC. (2022). COVID-19. https://www.ecdc.europa.eu/en/covid-19 .
Elliott, J., Bodinier, B., Whitaker, M., Delpierre, C., Vermeulen, R., Tzoulaki, I., Elliott, P., & Chadeau-Hyam, M. (2021). COVID-19 mortality in the UK Biobank cohort: revisiting and evaluating risk factors. Eur. J. Epidemiol., 36(3), 299–309. https://doi.org/10.1007/s10654-021-00722-y
Etienne, N., Karmochkine, M., Slama, L., Pavie, J., Batisse, D., Usubillaga, R., Letembet, V. A., Brazille, P., Canouï, E., Slama, D., Joumaa, H., Canoui-Poitrine, F., Segaux, L., Weiss, L., Viard, J. P., Salmon, D., & COVID-19 ID Team. (2020). HIV infection and COVID-19: Risk factors for severe disease. AIDS, 34(12), 1771–1774. https://doi.org/10.1097/QAD.0000000000002651
Fabiani, M., Mateo-Urdiales, A., Andrianou, X., Bella, A., Del Manso, M., Bellino, S., Rota, M. C., Boros, S., Vescio, M. F., D'Ancona, F. P., Siddu, A., Punzo, O., Filia, A., Brusaferro, S., Rezza, G., Dente, M. G., Declich, S., Pezzotti, P., & Riccardo, F. (2021). COVID-19 Working Group. Epidemiological characteristics of COVID-19 cases in non-Italian nationals notified to the Italian surveillance system. Eur. J. Pub. Health, 31(1), 37–44. https://doi.org/10.1093/eurpub/ckaa249
Farrell, R. J., O'Regan, R., O'Neill, E., Bowens, G., Maclellan, A., Gileece, A., Bradley, M., Smyth, C., Kelly, O., Hall, B., Cormican, L., Faul, J., Wanic, K., McDermott, J., Sreenan, S., Tun, T. K., Duffy, T., Bhatti, A. I., Donohoe, O., et al. (2021). Sociodemographic variables as predictors of adverse outcome in SARS-CoV-2 infection: An Irish hospital experience. Ir. J. Med. Sci., 190(3), 893–903. https://doi.org/10.1007/s11845-020-02407-z
Felsenstein, S., Willis, E., Lythgoe, H., McCann, L., Cleary, A., Mahmood, K., Porter, D., Jones, J., McDonagh, J., Chieng, A., Varnier, G., Hughes, S., Boullier, M., Ryan, F., Awogbemi, O., Soda, G., Duong, P., Pain, C., Riley, P., & Hedrich, C. M. (2020). Presentation, treatment response and short-term outcomes in paediatric multisystem inflammatory syndrome temporally associated with SARS-CoV-2 (PIMS-TS). J. Clin. Med., 9(10), 3293. https://doi.org/10.3390/jcm9103293
Ferrando-Vivas, P., Doidge, J., Thomas, K., Gould, D. W., Mouncey, P., Shankar-Hari, M., Young, J. D., Rowan, K. M., Harrison, D. A., & ICNARC COVID-19 Team. (2021). Prognostic factors for 30-day mortality in critically ill patients with coronavirus disease 2019: An observational cohort study. Crit. Care Med., 49(1), 102–111. https://doi.org/10.1097/CCM.0000000000004740
Fiorini, G., Rigamonti, A. E., Galanopoulos, C., Adamoli, M., Ciriaco, E., Franchi, M., Genovese, E., Corrao, G., & Cella, S. G. (2020). Undocumented migrants during the COVID-19 pandemic: Socio-economic determinants, clinical features and pharmacological treatment. J. Public Health Res., 9(4), 1852. https://doi.org/10.4081/jphr.2020.1852
Galloway, J. B., Norton, S., Barker, R. D., Brookes, A., Carey, I., Clarke, B. D., Jina, R., Reid, C., Russell, M. D., Sneep, R., Sugarman, L., Williams, S., Yates, M., Teo, J., Shah, A. M., & Cantle, F. (2020). A clinical risk score to identify patients with COVID-19 at high risk of critical care admission or death: An observational cohort study. J. Infect., 81(2), 282–288. https://doi.org/10.1016/j.jinf.2020.05.064
Giorgi Rossi, P., Marino, M., Formisano, D., Venturelli, F., Vicentini, M., Grilli, R., & Reggio Emilia COVID-19 Working Group. (2020). Characteristics and outcomes of a cohort of COVID-19 patients in the Province of Reggio Emilia, Italy. PLoS One, 15(8), e0238281. https://doi.org/10.1371/journal.pone.0238281
Gopal Rao, G., Allen, A., Papineni, P., Wang, L., Anderson, C., McGregor, A., Whittington, A., John, L., Harris, M., Hiles, S., Nicholas, T., Adams, K., Akbar, A., Blomquist, P., Decraene, V., Patel, B., Manuel, R., Chow, Y., Kuper, M., & London North West Healthcare Trust COVID-19 Research Group. (2021). Cross-sectional observational study of epidemiology of COVID-19 and clinical outcomes of hospitalised patients in North West London during March and April 2020. BMJ Open, 11(2), e044384. https://doi.org/10.1136/bmjopen-2020-044384
Greenaway, C., Hargreaves, S., Barkati, S., Coyle, C. M., Gobbi, F., Veizis, A., & Douglas, P. (2020). COVID-19: Exposing and addressing health disparities among ethnic minorities and migrants. J. Travel Med., 27(7), taaa113. https://doi.org/10.1093/jtm/taaa113
Guijarro, C., Pérez-Fernández, E., González-Piñeiro, B., Meléndez, V., Goyanes, M. J., Renilla, M. E., Casas, M. L., Sastre, I., Velasco, M., & e investigadores COVID Alcorcón; Investigadores COVID Alcorcón (colaboradores). (2021). Riesgo de COVID-19 en españoles y migrantes de distintas zonas del mundo residentes en España en la primera oleada de la enfermedad [Differential risk for COVID-19 in the first wave of the disease among Spaniards and migrants from different areas of the world living in Spain]. Rev Clin Esp (Barc), 221(5), 264–273. https://doi.org/10.1016/j.rce.2020.10.006
Harris, R. (2020). Exploring the neighbourhood-level correlates of Covid-19 deaths in London using a difference across spatial boundaries method. Health Place, 66, 102446. https://doi.org/10.1016/j.healthplace.2020.102446
Harrison, E. M., et al. (2020). Ethnicity and outcomes from COVID-19: The ISARIC CCP-UK prospective observational cohort study of hospitalised patients. SSRN Electron. J. https://doi.org/10.2139/SSRN.3618215
Hayward, S. E., Deal, A., Cheng, C., Crawshaw, A., Orcutt, M., Vandrevala, T. F., Norredam, M., Carballo, M., Ciftci, Y., Requena-Méndez, A., Greenaway, C., Carter, J., Knights, F., Mehrotra, A., Seedat, F., Bozorgmehr, K., Veizis, A., Campos-Matos, I., Wurie, F., et al. (2021). Clinical outcomes and risk factors for COVID-19 among migrant populations in high-income countries: A systematic review. J Migr Health, 3, 100041. https://doi.org/10.1016/j.jmh.2021.100041
Hippisley-Cox, J., Young, D., Coupland, C., Channon, K. M., Tan, P. S., Harrison, D. A., Rowan, K., Aveyard, P., Pavord, I. D., & Watkinson, P. J. (2020). Risk of severe COVID-19 disease with ACE inhibitors and angiotensin receptor blockers: cohort study including 8.3 million people. Heart, 106(19), 1503–1511. https://doi.org/10.1136/heartjnl-2020-317393
Holman, N., Knighton, P., Kar, P., O'Keefe, J., Curley, M., Weaver, A., Barron, E., Bakhai, C., Khunti, K., Wareham, N. J., Sattar, N., Young, B., & Valabhji, J. (2020). Risk factors for COVID-19-related mortality in people with type 1 and type 2 diabetes in England: A population-based cohort study. Lancet Diabetes Endocrinol., 8(10), 823–833. https://doi.org/10.1016/S2213-8587(20)30271-0
Horton, R. (2020). Offline: COVID-19 is not a pandemic. Lancet, 396(10255), 874. https://doi.org/10.1016/S0140-6736(20)32000-6
Indseth, T., Grøsland, M., Arnesen, T., Skyrud, K., Kløvstad, H., Lamprini, V., Telle, K., & Kjøllesdal, M. (2021). COVID-19 among immigrants in Norway, notified infections, related hospitalizations and associated mortality: A register-based study. Scand. J. Public Health, 49(1), 48–56.
IOM. (2019). Glossary on migration 2019. https://publications.iom.int/system/files/pdf/iml_34_glossary.pdf
Jaljaa, A., Caminada, S., Tosti, M. E., D'Angelo, F., Angelozzi, A., Isonne, C., Marchetti, G., Mazzalai, E., Giannini, D., Turatto, F., De Marchi, C., Gatta, A., Declich, S., Pizzarelli, S., Geraci, S., Baglio, G., & Marceca, M. (2022). Risk of SARS-CoV-2 infection in migrants and ethnic minorities compared with the general population in the European WHO region during the first year of the pandemic: A systematic review. BMC Public Health, 22(1), 143. https://doi.org/10.1186/s12889-021-12466-1
Joy, M., Hobbs, F. R., Bernal, J. L., Sherlock, J., Amirthalingam, G., McGagh, D., Akinyemi, O., Byford, R., Dabrera, G., Dorward, J., Ellis, J., Ferreira, F., Jones, N., Oke, J., Okusi, C., Nicholson, B. D., Ramsay, M., Sheppard, J. P., Sinnathamby, M., et al. (2020). Excess mortality in the first COVID pandemic peak: Cross-sectional analyses of the impact of age, sex, ethnicity, household size, and long-term conditions in people of known SARS-CoV-2 status in England. Br. J. Gen. Pract., 70(701), e890–e898. https://doi.org/10.3399/bjgp20X713393
Kakkar, D. N., Dunphy, D. J., & Raza, D. M. (2020). Ethnicity profiles of COVID-19 admissions and outcomes. J. Infect., 81(2), e110–e111. https://doi.org/10.1016/j.jinf.2020.05.059
Ken-Dror, G., Wade, C., Sharma, S., Law, J., Russo, C., Sharma, A., Joy, E., John, J., Robin, J., John, S., Mahana, K., Fluck, D., Bentley, P., & Sharma, P. (2020). COVID-19 outcomes in UK centre within highest health and wealth band: A prospective cohort study. BMJ Open, 10(11), e042090. https://doi.org/10.1136/bmjopen-2020-042090
Kolhe, N. V., Fluck, R. J., Selby, N. M., & Taal, M. W. (2020). Acute kidney injury associated with COVID-19: A retrospective cohort study. PLoS Med., 17(10), e1003406. https://doi.org/10.1371/journal.pmed.1003406
Kuo, C. L., Pilling, L. C., Atkins, J. L., Masoli, J. A. H., Delgado, J., Tignanelli, C., Kuchel, G. A., Melzer, D., Beckman, K. B., & Levine, M. E. (2021). Biological aging predicts vulnerability to COVID-19 severity in UK Biobank participants. J. Gerontol. A Biol. Sci. Med. Sci., 76(8), e133–e141. https://doi.org/10.1093/gerona/glab060
Lassale C, Gaye B, Hamer M, Gale CR, Batty GD. (2020). Ethnic disparities in hospitalization for COVID-19: A community-based cohort study in the UK. medRxiv [Preprint]. 2020.05.19.20106344. doi: 10.1101/2020.05.19.20106344. Update in: Brain Behav Immun. 2020 Aug; 88:44-49. PMID: 32511503; PMCID: PMC7273271.
Lau, L. L., Hung, N., & Wilson, K. (2020). COVID-19 response strategies: Considering inequalities between and within countries. Int. J. Equity Health, 19(1), 137. https://doi.org/10.1186/s12939-020-01254-9
Liberati, A., Altman, D. G., Tetzlaff, J., Mulrow, C., Gøtzsche, P. C., Ioannidis, J. P., Clarke, M., Devereaux, P. J., Kleijnen, J., & Moher, D. (2009). The PRISMA statement for reporting systematic reviews and meta-analyses of studies that evaluate healthcare interventions: Explanation and elaboration. BMJ, 339, b2700. https://doi.org/10.1136/bmj.b2700
Livingston, G., Rostamipour, H., Gallagher, P., Kalafatis, C., Shastri, A., Huzzey, L., Liu, K., Sommerlad, A., & Marston, L. (2020). Prevalence, management, and outcomes of SARS-CoV-2 infections in older people and those with dementia in mental health wards in London, UK: A retrospective observational study. Lancet Psychiatry, 7(12), 1054–1063. https://doi.org/10.1016/S2215-0366(20)30434-X
Lo, C. H., Nguyen, H. L., Drew, D. A., Graham, M. S., Warner, E. T., Joshi, A. D., Astley, C. M., Guo, C., Ma, W., Mehta, R. S., Kwon, S., Song, M., Davies, R., Capdevila, J., Lee, K. A., Lochlainn, M. N., Varsavsky, T., Sudre, C. H., Wolf, J., et al. (2020). Racial and ethnic determinants of Covid-19 risk. medRxiv. https://doi.org/10.1101/2020.06.18.20134742
Lok, J., & Gess, M. (2020). Liver dysfunction in COVID-19: A useful prognostic marker of severe disease? Frontline Gastroenterol., 12(4), 293–298. https://doi.org/10.1136/flgastro-2020-101689
Mahil, S. K., Dand, N., Mason, K. J., ZZN, Y., Tsakok, T., Meynell, F., Coker, B., McAteer, H., Moorhead, L., Mackenzie, T., Rossi, M. T., Rivera, R., Mahe, E., Carugno, A., Magnano, M., Rech, G., Balogh, E. A., Feldman, S. R., De La Cruz, C., et al. (2021). Factors associated with adverse COVID-19 outcomes in patients with psoriasis-insights from a global registry-based study. J. Allergy Clin. Immunol., 147(1), 60–71. https://doi.org/10.1016/j.jaci.2020.10.007
Marceca, M. (2017). Migration and health from a public health perspective. In I. Muenstermann (Ed.), People's Movements in the 21st Century - Risks, Challenges and Benefits. IntechOpen.
Marmot, M., & Allen, J. (2020). COVID-19: Exposing and amplifying inequalities. J. Epidemiol. Community Health, 74, 681–682.
Melchior, M., Desgrées du Loû, A., Gosselin, A., Datta, G. D., Carabali, M., Merckx, J., & Kaufman, J. S. (2021). Migrant status, ethnicity and COVID-19: More accurate European data are greatly needed. Clin. Microbiol. Infect., 27(2), 160–162. https://doi.org/10.1016/j.cmi.2020.10.014
Miles, A., Webb, T. E., Mcloughlin, B. C., Mannan, I., Rather, A., Knopp, P., & Davis, D. (2020). Outcomes from COVID-19 across the range of frailty: Excess mortality in fitter older people. Eur Geriatr Med., 11(5), 851–855. https://doi.org/10.1007/s41999-020-00354-7
Moody, W. E., Mahmoud-Elsayed, H. M., Senior, J., Gul, U., Khan-Kheil, A. M., Horne, S., Banerjee, A., Bradlow, W. M., Huggett, R., Hothi, S. S., Shahid, M., & Steeds, R. P. (2021). Impact of right ventricular dysfunction on mortality in patients hospitalized with COVID-19, According to Race. CJC Open, 3(1), 91–100. https://doi.org/10.1016/j.cjco.2020.09.016
Morante-García, W., Zapata-Boluda, R. M., García-González, J., Campuzano-Cuadrado, P., Calvillo, C., & Alarcón-Rodríguez, R. (2022). Influence of social determinants of health on COVID-19 infection in socially vulnerable groups. Int. J. Environ. Res. Public Health, 19(3), 1294. https://doi.org/10.3390/ijerph19031294
Navaratnam, A. V., Gray, W. K., Day, J., Wendon, J., & Briggs, T. W. R. (2021). Patient factors and temporal trends associated with COVID-19 in-hospital mortality in England: An observational study using administrative data. Lancet Respir. Med., 9(4), 397–406. https://doi.org/10.1016/S2213-2600(20)30579-8
Nazroo, J., & Becares, L. (2020). Evidence for ethnic inequalities in mortality related to COVID-19 infections: Findings from an ecological analysis of England. BMJ Open, 10(12), e041750. https://doi.org/10.1136/bmjopen-2020-041750
Nikoloudis, D., Kountouras, D., & Hiona, A. (2020). The frequency of combined IFITM3 haplotype involving the reference alleles of both rs12252 and rs34481144 is in line with COVID-19 standardized mortality ratio of ethnic groups in England. PeerJ., 8, e10402. https://doi.org/10.7717/peerj.10402
Norman, F. F., Crespillo-Andújar, C., Pérez-Molina, J. A., Comeche, B., Chamorro, S., Monge-Maillo, B., Moreno-Guillén, S., López-Vélez, R., & COVID-19 ID Team. (2021). COVID-19 and geographical area of origin. Clin. Microbiol. Infect., 27(4), 632.e1–632.e5. https://doi.org/10.1016/j.cmi.2020.11.011
Nowakowska, J., Sobocińska, J., Lewicki, M., Lemańska, Ż., & Rzymski, P. (2020). When science goes viral: The research response during three months of the COVID-19 outbreak. Biomed. Pharmacother., 129, 110451. https://doi.org/10.1016/j.biopha.2020.110451
Papageorgiou, N., Providencia, R., Saberwal, B., Sohrabi, C., Tyrlis, A., Atieh, A. E., Lim, W. Y., Creta, A., Khanji, M., Rusinova, R., Chooneea, B., Khiani, R., Wijesuriya, N., Chow, A., Butt, H., Browne, S., Joshi, N., Kay, J., & Ahsan, S. (2020). Ethnicity and COVID-19 cardiovascular complications: A multi-center UK cohort. Am J Cardiovasc Dis., 10(4), 455–462.
Patel, A., Abdulaal, A., Ariyanayagam, D., Killington, K., Denny, S. J., Mughal, N., Hughes, S., Goel, N., Davies, G. W., Moore, L. S. P., & Charani, E. (2020). Investigating the association between ethnicity and health outcomes in SARS-CoV-2 in a London secondary care population. PLoS One, 15(10), e0240960. https://doi.org/10.1371/journal.pone.0240960
Patel, A. P., Paranjpe, M. D., Kathiresan, N. P., et al. (2020). Race, socioeconomic deprivation, and hospitalization for COVID-19 in English participants of a national biobank. Int. J. Equity Health, 19, 114. https://doi.org/10.1186/s12939-020-01227-y
Patel, J. A., Nielsen, F. B. H., Badiani, A. A., Assi, S., Unadkat, V. A., Patel, B., Ravindrane, R., & Wardle, H. (2020). Poverty, inequality and COVID-19: The forgotten vulnerable. Public Health, 183, 110–111. https://doi.org/10.1016/j.puhe.2020.05.006
Perez-Guzman, P. N., Daunt, A., Mukherjee, S., Crook, P., Forlano, R., Kont, M. D., Løchen, A., Vollmer, M., Middleton, P., Judge, R., Harlow, C., Soubieres, A., Cooke, G., White, P. J., Hallett, T. B., Aylin, P., Ferguson, N., Hauck, K., Thursz, M. R., & Nayagam, S. (2021). Clinical characteristics and predictors of outcomes of hospitalized patients with coronavirus disease 2019 in a multiethnic London National Health Service Trust: A retrospective cohort study. Clin. Infect. Dis., 73(11), e4047. https://doi.org/10.1093/cid/ciaa1091
Perkin, M. R., Heap, S., Crerar-Gilbert, A., Albuquerque, W., Haywood, S., Avila, Z., Hartopp, R., Ball, J., Hutt, K., & Kennea, N. (2020). Deaths in people from Black, Asian and minority ethnic communities from both COVID-19 and non-COVID causes in the first weeks of the pandemic in London: A hospital case note review. BMJ Open, 10(10), e040638. https://doi.org/10.1136/bmjopen-2020-040638
Phiri, P., Delanerolle, G., Al-Sudani, A., & Rathod, S. (2021). COVID-19 and Black, Asian, and minority ethnic communities: A complex relationship without just cause. JMIR Public Health Surveill., 7(2), e22581. https://doi.org/10.2196/22581
Platt, L., & Warwick, R. (2020). COVID-19 and ethnic inequalities in England and Wales. Fisc. Stud. https://doi.org/10.1111/1475-5890.12228
Richards-Belle, A., Orzechowska, I., Gould, D. W., Thomas, K., Doidge, J. C., Mouncey, P. R., Christian, M. D., Shankar-Hari, M., Harrison, D. A., Rowan, K. M., & ICNARC COVID-19 Team. (2020). COVID-19 in critical care: Epidemiology of the first epidemic wave across England, Wales and Northern Ireland. Intensive Care Med., 46(11), 2035–2047. https://doi.org/10.1007/s00134-020-06267-0
Rose, T. C., Mason, K., Pennington, A., McHale, P., Buchan, I., Taylor-Robinson, D. C., & Barr, B. (2020). Inequalities in COVID19 mortality related to ethnicity and socioeconomic deprivation. medRxiv, 20079491. https://doi.org/10.1101/2020.04.25.20079491
Rostila, M., Cederström, A., Wallace, M., Brandén, M., Malmberg, B., & Andersson, G. (2021). Disparities in coronavirus disease 2019 mortality by country of birth in Stockholm, Sweden: A total-population-based cohort study. Am. J. Epidemiol., 190(8), 1510–1518. https://doi.org/10.1093/aje/kwab057
Russell, B., Moss, C., Papa, S., Irshad, S., Ross, P., Spicer, J., Kordasti, S., Crawley, D., Wylie, H., Cahill, F., Haire, A., Zaki, K., Rahman, F., Sita-Lumsden, A., Josephs, D., Enting, D., Lei, M., Ghosh, S., Harrison, C., et al. (2020). Factors affecting COVID-19 outcomes in cancer patients: A first report from guy's cancer center in London. Front. Oncol., 10, 1279. https://doi.org/10.3389/fonc.2020.01279
Saban, M., Myers, V., & Wilf-Miron, R. (2020). Coping with the COVID-19 pandemic – The role of leadership in the Arab ethnic minority in Israel. Int. J. Equity Health, 19, 154. https://doi.org/10.1186/s12939-020-01257-6
Santorelli, G., Sheldon, T., West, J., Cartwright, C., & Wright, J. (2020). COVID-19 in-patient hospital mortality by ethnicity. Wellcome Open Res, 5, 86. https://doi.org/10.12688/wellcomeopenres.15913.1
Sapey, E., Gallier, S., Mainey, C., Nightingale, P., McNulty, D., Crothers, H., Evison, F., Reeves, K., Pagano, D., Denniston, A. K., Nirantharakumar, K., Diggle, P., & Ball, S. (2020). All clinicians and students at University Hospitals Birmingham NHS Foundation Trust. Ethnicity and risk of death in patients hospitalised for COVID-19 infection in the UK: An observational cohort study in an urban catchment area. BMJ Open. Respir. Res., 7(1), e000644. https://doi.org/10.1136/bmjresp-2020-000644
Sattar, N., Ho, F. K., Gill, J. M., Ghouri, N., Gray, S. R., Celis-Morales, C. A., Katikireddi, S. V., Berry, C., Pell, J. P., McMurray, J. J., & Welsh, P. (2020). BMI and future risk for COVID-19 infection and death across sex, age and ethnicity: Preliminary findings from UK biobank. Diabetes Metab. Syndr., 14(5), 1149–1151. https://doi.org/10.1016/j.dsx.2020.06.060
Savino, M., Casula, A., Santhakumaran, S., Pitcher, D., Wong, E., Magadi, W., Evans, K. M., Benoy-Deeney, F., Griffin, J., Plumb, L., Steenkamp, R., Nitsch, D., & Medcalf, J. (2020). Sociodemographic features and mortality of individuals on haemodialysis treatment who test positive for SARS-CoV-2: A UK Renal Registry data analysis. PLoS One, 15(10), e0241263. https://doi.org/10.1371/journal.pone.0241263
Shaaban, A. N., Peleteiro, B., & Martins, M. R. O. (2020). The writing's on the wall: On health inequalities, migrants, and coronavirus. Front. Public Health, 8, 505. https://doi.org/10.3389/fpubh.2020.00505
Singh, B. M., Bateman, J., Viswanath, A., Klaire, V., Mahmud, S., Nevill, A., & Dunmore, S. J. (2021). Risk of COVID-19 hospital admission and COVID-19 mortality during the first COVID-19 wave with a special emphasis on ethnic minorities: An observational study of a single, deprived, multiethnic UK health economy. BMJ Open, 11(2), e046556. https://doi.org/10.1136/bmjopen-2020-046556
Staines, H. M., Kirwan, D. E., Clark, D. J., Adams, E. R., Augustin, Y., Byrne, R. L., Cocozza, M., Cubas-Atienzar, A. I., Cuevas, L. E., Cusinato, M., Davies, B. M. O., Davis, M., Davis, P., Duvoix, A., Eckersley, N. M., Forton, D., Fraser, A. J., Garrod, G., Hadcocks, L., et al. (2021). IgG seroconversion and pathophysiology in severe acute respiratory syndrome coronavirus 2 infection. Emerg. Infect. Dis., 27(1), 85–91. https://doi.org/10.3201/eid2701.203074
Stevens, A. J., Ray, A. M., Thirunavukarasu, A., Johnson, E., Jones, L., Miller, A., & Elston, J. W. T. (2021). The experiences of socially vulnerable groups in England during the COVID-19 pandemic: A rapid health needs assessment. Public Health Pract (Oxf)., 2, 100192. https://doi.org/10.1016/j.puhip.2021.100192
Svensson, P., Hofmann, R., Häbel, H., Jernberg, T., & Nordberg, P. (2021). Association between cardiometabolic disease and severe COVID-19: A nationwide case-control study of patients requiring invasive mechanical ventilation. BMJ Open, 11(2), e044486. https://doi.org/10.1136/bmjopen-2020-044486
Swann, O. V., Holden, K. A., Turtle, L., Pollock, L., Fairfield, C. J., Drake, T. M., Seth, S., Egan, C., Hardwick, H. E., Halpin, S., Girvan, M., Donohue, C., Pritchard, M., Patel, L. B., Ladhani, S., Sigfrid, L., Sinha, I. P., Olliaro, P. L., Nguyen-Van-Tam, J. S., et al. (2020). ISARIC4C Investigators. Clinical characteristics of children and young people admitted to hospital with covid-19 in United Kingdom: Prospective multicentre observational cohort study. BMJ., 370, m3249. https://doi.org/10.1136/bmj.m3249
Sze, S., Pan, D., Nevill, C. R., Gray, L. J., Martin, C. A., Nazareth, J., Minhas, J. S., Divall, P., Khunti, K., Abrams, K. R., Nellums, L. B., & Pareek, M. (2020). Ethnicity and clinical outcomes in COVID-19: A systematic review and meta-analysis. EclinicalMedicine, 29, 100630. https://doi.org/10.1016/j.eclinm.2020.100630
Thompson, J. V., Meghani, N. J., Powell, B. M., Newell, I., Craven, R., Skilton, G., Bagg, L. J., Yaqoob, I., Dixon, M. J., Evans, E. J., Kambele, B., Rehman, A., & Ng Man Kwong, G. (2020). Patient characteristics and predictors of mortality in 470 adults admitted to a district general hospital in England with Covid-19. Epidemiol. Infect., 148, e285. https://doi.org/10.1017/S0950268820002873
Thomson, R. J., Hunter, J., Dutton, J., Schneider, J., Khosravi, M., Casement, A., Dhadwal, K., & Martin, D. (2020). Clinical characteristics and outcomes of critically ill patients with COVID-19 admitted to an intensive care unit in London: A prospective observational cohort study. PLoS One, 15(12), e0243710. https://doi.org/10.1371/journal.pone.0243710
UNHCR (2010) Convention and protocol relating to the status of refugees. https://www.unhcr.org/protection/basic/3b66c2aa10/convention-protocol-relating-status-refugees.html
Verma, A. M., Goddard, A. F., O'Donoghue, D., Newbery, N., Phillips, C., & Trudgill, N. (2021). The UK physician workforce: One-third at increased risk of death from COVID-19. Clin. Med. (Lond.), 21(2), e161–e165. https://doi.org/10.7861/clinmed.2020-0756
Williamson, E. J., Walker, A. J., Bhaskaran, K., Bacon, S., Bates, C., Morton, C. E., Curtis, H. J., Mehrkar, A., Evans, D., Inglesby, P., Cockburn, J., McDonald, H. I., MacKenna, B., Tomlinson, L., Douglas, I. J., Rentsch, C. T., Mathur, R., Wong, A. Y. S., Grieve, R., et al. (2020). Factors associated with COVID-19-related death using OpenSAFELY. Nature, 584(7821), 430–436. https://doi.org/10.1038/s41586-020-2521-4
Woodward, A., Howard, N., & Wolffers, I. (2014). Health and access to care for undocumented migrants living in the European Union: A scoping review. Health Policy Plan., 29(7), 818–830. https://doi.org/10.1093/heapol/czt061
World Health Organization. Regional Office for Europe. (2018). Report on the health of refugees and migrants in the WHO European Region: No public health without refugee and migrant health. World Health Organization. Regional Office for Europe https://apps.who.int/iris/handle/10665/311347
World Health Organization. (2010). How health systems can address health inequities linked to migration and ethnicity. https://www.euro.who.int/__data/assets/pdf_file/0005/127526/e94497.pdf
World Health Organization. (2020). ApartTogether survey: Preliminary overview of refugees and migrants self-reported impact of COVID-19. World Health Organization https://apps.who.int/iris/handle/10665/337931. License: CC BY-NC-SA 3.0 IGO
World Health Organization. (2022a). Coronavirus (COVID-19) dashboard | WHO coronavirus (COVID-19) dashboard with vaccination data. https://covid19.who.int/.
World Health Organization. (2022b). Coronavirus disease (COVID-19): Vaccines. https://www.who.int/news-room/questions-and-answers/item/coronavirus-disease-(covid-19)-vaccines?gclid=CjwKCAjwrqqSBhBbEiwAlQeqGuZD05Hq9dPjWHS3thaBqKaofmbXFvjFx64_aUxLlEDtcceHHeblxRoCAncQAvD_BwE&topicsurvey=v8kj13)
Zakeri, R., Bendayan, R., Ashworth, M., Bean, D. M., Dodhia, H., Durbaba, S., O'Gallagher, K., Palmer, C., Curcin, V., Aitken, E., Bernal, W., Barker, R. D., Norton, S., Gulliford, M., Teo, J. T. H., Galloway, J., Dobson, R. J. B., & Shah, A. M. (2020). A case-control and cohort study to determine the relationship between ethnic background and severe COVID-19. EclinicalMedicine, 28, 100574. https://doi.org/10.1016/j.eclinm.2020.100574
Acknowledgements
Marise Sabato performed the linguistic revision. Vincenza Lorusso supported the research team by giving a clinical perspective to the manuscript.
Availability of Data and Materials
Data sharing is not applicable to this article as no datasets were generated or analysed during the current study.
Funding
Open access funding provided by Università degli Studi di Roma La Sapienza within the CRUI-CARE Agreement.
Author information
Authors and Affiliations
Contributions
All authors contributed to the study conceptualization and design. MET, FDA and SP performed the literature search. MET led the methodology and coordinated the data analysis. AA, AG, AJ, CDM, DG, EM, FT, GM and SC screened the records and performed the data analysis. DG, EM, FT and MM drafted the manuscript. MET, FDA, MM and SD contributed to interpretation of the results. All authors contributed to the critical revision of the manuscript. All authors approved the final manuscript. MM is the guarantor for the study. The corresponding author attests that all listed authors meet authorship criteria and that no others meeting the criteria have been omitted.
Corresponding author
Ethics declarations
Ethics Approval
This is an observational study; therefore, no ethical approval is required.
Competing Interests
The authors declare no competing interests.
Additional information
Publisher’s Note
Springer Nature remains neutral with regard to jurisdictional claims in published maps and institutional affiliations.
Supplementary information
Supplementary material
The online version contains supplementary material available at sAppendix 1 and 2.
Rights and permissions
Open Access This article is licensed under a Creative Commons Attribution 4.0 International License, which permits use, sharing, adaptation, distribution and reproduction in any medium or format, as long as you give appropriate credit to the original author(s) and the source, provide a link to the Creative Commons licence, and indicate if changes were made. The images or other third party material in this article are included in the article's Creative Commons licence, unless indicated otherwise in a credit line to the material. If material is not included in the article's Creative Commons licence and your intended use is not permitted by statutory regulation or exceeds the permitted use, you will need to obtain permission directly from the copyright holder. To view a copy of this licence, visit http://creativecommons.org/licenses/by/4.0/.
About this article
Cite this article
Mazzalai, E., Giannini, D., Tosti, M.E. et al. Risk of Covid-19 Severe Outcomes and Mortality in Migrants and Ethnic Minorities Compared to the General Population in the European WHO Region: a Systematic Review. Int. Migration & Integration 24, 1305–1335 (2023). https://doi.org/10.1007/s12134-023-01007-x
Accepted:
Published:
Issue Date:
DOI: https://doi.org/10.1007/s12134-023-01007-x