Abstract
In a sample of men who have sex with men (MSM) (N = 3436) in Spain who bear intrinsic HIV risk, we investigated how internalised homonegativity (IH) is associated with the number of non-steady male partners with condomless intercourse (as a proxy of sexual risk behaviour). Using structural equation modelling (SEM), we examined the relationship between IH and sexual risk behaviour, and mediating effects of HIV/PrEP knowledge and substance use during sex on this relationship. We found no direct association between IH and sexual risk behaviour, nor did IH influence substance use during sex. In line with our hypothesis, association between IH and sexual risk behaviour was significant when mediated by HIV/PrEP knowledge. We found that as IH increased, sexual risk behaviour decreased, because higher IH was associated with lower HIV/PrEP knowledge while higher HIV/PrEP knowledge was associated with increased non-condom use with non-steady partners. Substance use during sex was significantly associated with sexual risk behaviour. Our results emphasize the continuing importance of prevention strategies focused on behavioural changes and community level interventions, especially targeting substance use.
Similar content being viewed by others
Avoid common mistakes on your manuscript.
Introduction
Forty years into the epidemic, sex between men remains the predominant mode of HIV transmission in the countries of the European Economic Area, accounting for 38.7% of all new HIV diagnoses in 2019 (European Centre for Disease Prevention and Control & World Health Organization, 2020). In Spain, 3381 new HIV diagnoses were reported in 2017, with more than half (54.3%) of these in men who have sex with men (MSM) (Centro Nacional de Epidemiología, 2018). A recent bio-behavioural study conducted in 13 European cities showed that Barcelona (Spain) has one of the highest rates of HIV among MSM (Mirandola et al., 2018). In addition to the spread of HIV, increasing numbers of sexually transmitted infections (STIs) have been reported in Spain after 2005 (Centro Nacional de Epidemiología, 2020).
Sexual transmission risk among MSM is mediated by multiple social and structural factors that influence individuals’ sexual practices (Baral et al., 2013). These factors not only influence risk behaviours, but also directly limit options for accessing prevention services for HIV and other STIs and jeopardise prevention efforts (Andrinopoulos et al., 2015; Velter et al., 2015). Meyer (2003) developed the minority stress model, which refers to the “excess stress to which individuals from stigmatized social categories are exposed as a result of their social, often a minority, position”, and which may partly explain behaviours that increase HIV transmission risk, such as substance use and condomless sex (Meyer, 2003). Internalised Homonegativity (IH), defined as negative feelings about one's homosexuality (Herek, 2004), is the product of social and political stigma and bias instead of a response which stems from within individuals. IH is one of the minority stressors that has been expanded upon in Meyer’s (2003) minority stress model, and has a documented damaging effect on the mental health and well-being of sexual minorities (Newcomb & Mustanski, 2010a). However, inconsistent research results point to uncertainties about the extent to which IH influences engagement in sexual risk behaviours (Newcomb & Mustanski, 2010a; Puckett et al., 2017). In Catalonia, an autonomous community of Spain, previous research among gay, bisexual and other MSM found that IH was an independent predictor of sexual risk behaviours (SRB). This has also been shown for European (Berg et al., 2015) and non-European countries (Ross et al., 2013). However, other studies have not found significant associations between IH and SRB (Dudley et al., 2004; Kashubeck-West & Szymanski, 2008a). These inconsistencies on the literature may reflect, in part, the existence of potential mediating variables that affect the relation between IH and sexual risk behaviours (Kashubeck-West & Szymanski, 2008a; Newcomb & Mustanski, 2010b).
Similar inconsistent research results exist regarding the relation between IH and drug use. Some researchers found that IH was associated with higher levels of drug use, whereas others found either no significant relation with drug use or negative associations (Puckett et al., 2017; Ross et al., 2001). The effect of sexualized drug use on SRB has also been studied extensively. Previous studies in Spain found evidence that a higher prevalence of drug use consumption was associated with a higher prevalence of condomless anal sex or sex with multiple partners (Fernández-Dávila & Zaragoza Lorca, 2009; Folch et al., 2006, 2010; González-Baeza et al., 2018).
Men with high level of IH are less likely to be involved in the gay community and likewise more isolated from getting informed about HIV prevention and risk reduction programs. Among 569 gay and bisexual men Huebner et al. (Huebner et al., 2002) found that IH was negatively associated with the number of HIV-related services that these men were aware of. Further, of the 443 MSM who had heard about at least one service, IH was not a significant predictor for participation in these services, when controlled for education levels. Therefore, high IH was a barrier for men to be aware of these services in the first place. On the other hand, the results of the 2010 wave of EMIS among more than 144,000 MSM across 38 countries in Europe provide evidence that IH was positively associated with less knowledge about HIV and HIV testing (Berg et al., 2013). Likewise, in a sample of substance using HIV-negative and unknown status gay and bisexual men in New York City, it was found that community connection was protective against sexual risk and drug use, especially among younger men (Lelutiu-Weinberger et al., 2013). Previous research also documented that IH can hinder gay men’s connection to the gay community (Goldbach et al., 2015; Moody et al., 2018), which can, in part, explain a possible link between IH and SRB, through a lack of gay community acculturation and where the targeted information is available for gay and bisexual men (Williamson, 2000).
An improved understanding of the impact of critical factors that mediate the relation between IH and SRB would be important in general, and in Spain specifically, in order to tailor community services to those MSM with higher levels of IH and in turn at higher risk of HIV infection. Therefore, using structural equation modelling (SEM), our study aimed to disentangle the possible influence of drug use and knowledge regarding HIV and PrEP on the relation between IH and SRB in a national sample of MSM living in Spain and recruited online. We had three hypotheses. First, we tested the ‘IH will be positively associated with sexual risk behaviour (SRB)’ hypothesis. As abovementioned, we argue that inconsistencies in previous research regarding the relationship between IH and SRB may reflect particular roles of mediator variables, such as frequency of sex under the influence of substances and HIV/PrEP knowledge. Thus, we tested our second and third hypotheses; HIV/PrEP knowledge will strongly mediate the relationship between IH and SRB’ and ‘sex under the influence of substances will strongly mediate the relationship between IH and SRB.’
Methods
Sample and Data
We used data from the 2017 wave of the European MSM Internet Survey (EMIS-2017). The detailed methods have been reported elsewhere (Weatherburn et al., 2020). In summary, EMIS-2017 was a 33-language, internet-based, self-completion survey for men living in Europe who have sex with men and/or are sexually attracted to other men. No financial incentives were given to participants; no personal identifying information (including IP addresses) were collected. More background information is available at www.emis2017.eu. The sub-sample of MSM living in Spain consisted of 10,652 respondents, including men living in the autonomous provinces of Canarias, Ceuta, Melilla (geographically outside Europe) as well as men living in the Principality of Andorra (but not in the British Overseas Territory of Gibraltar), with 92.1% using the Spanish (Castilian) version of the survey (no other co-official languages of Spain, such as Catalan/Valencian, Galician, or Basque were offered). Recruitment occurred through trans-national dating apps (Grindr accounted for 48% of recruits living in Spain, PlanetRomeo for 19%, SCRUFF, GROWLr, RECON, Gaydar, Hornet, and Manhunt/Jack’d, collectively for 11%), through national partners via websites (16%) and social media (1%) (Ministerio de Sanidad, 2020).
The Short Internalised Homonegativity Scale (SIHS) was randomly distributed to half of respondents (N = 5310) of which 4632 answered all SIHS items. This random distribution has been done to avoid losing participants because of asking too many questions. MSM who did not provide answers to all seven items were excluded. We also excluded 583 HIV-diagnosed MSM who reported having undetectable viral load, and 78 PrEP users, because condomless anal intercourse among men with undetectable viral load or using PrEP does not bear any intrinsic HIV risk. The analytic sample thus consists of 3436 MSM living in Spain.
Measures
Internalised homonegativity—To assess IH, we used the 7-item SIHS (Berg et al., 2013; Tran et al., 2018). This term was defined by Ross and colleagues (Berg et al., 2013), and the construct of IH commonly refers to internalization of homophobic attitudes within lesbian, gay, and bisexual individuals (Newcomb & Mustanski, 2011), thus an attachment of external homonegativity (often incorrectly referred to as ‘homophobia’) to the sense of self (Malyon, 1982; Stein & Cohen, 1986). EMIS-2017 participants answered 7 items on a 7-point disagree-agree (with does-not-apply) scale. These items were “social situations with gay men make me feel uncomfortable”; “homosexuality is morally acceptable to me”; “even if I could change my sexual orientation, I wouldn't”; “I feel comfortable in gay bars”; “I feel comfortable being seen in public with an obviously gay person”; “I feel comfortable being a homosexual man”; “even if I could change my sexual orientation, I wouldn't”. The validity and reliability of SIHS were also confirmed across 38 European countries, with multigroup validation for 7-item scale fit indices showing good fit to data from 38 country groups (CFI = 0.982, TLI = 0.983, and RMSEA = 0.032) (see, Tran et al. (2018) for further statistics).
Sexual Risk Behaviour (SRB)—SRB of the respondents was assessed with a single question: “how many non-steady male partners have you had intercourse without a condom with in the last 12 months?” Here, participants were informed that non-steady partners mean “men you have had sex with once only, and men you have sex with more than once but who you don’t think of as a steady partner (including one-night stands, anonymous and casual partners, regular sex buddies)”. The possible answer options for this question in the survey ranged from 0 to 15; with numbers 0 to 10 equivalent to their values, and numbers 11 to 15 indicating 11–20, 21–30, 31–40, 41–50, and more than 50 partners respondents had condomless intercourse with. We recoded this variable into seven categories: 0; 1; 2–5; 6–10; 11–20; 20–50; and more than 50. We would like to highlight that our definition of the risk behaviour is related to HIV risk and does not relate directly to other STIs.
HIV/PrEP Knowledge – To construct the HIV/PrEP knowledge latent variable, two measures were used: HIV knowledge and PrEP knowledge. HIV knowledge was constructed from seven items, assessed with a 5-point knowledge response set, with possible answers including “I do not believe this”, “I wasn’t sure about this”, and “I knew this already”. These items were “AIDS is caused by a virus called HIV”; “if someone becomes infected with HIV it may take several weeks before it can be detected in a test”; “you cannot be confident about whether someone has HIV or not from their appearance”; “there is a medical test that can show whether or not you have HIV”; “There is currently no cure for HIV infection”; “HIV infection can be controlled with medicines so that its impact on health is much less”; “a person with HIV who is on effective treatment (called ‘undetectable viral load’) cannot pass their virus to someone else during sex.” PrEP knowledge included three items assessed with the same response set: “Pre-Exposure Prophylaxis (PrEP) involves someone who does not have HIV taking pills before as well as after sex to prevent them getting HIV”; “PrEP can be taken as a single daily pill if someone does not know in advance when they will have sex”; “If someone knows in advance when they will have sex, PrEP needs to be taken as a double dose approximately 24 h before sex and then at both 24 and 48 h after the double dose.” Each of these 10 items were recoded into a dummy variable, with value 1 indicating “I knew this already,” and value 0 indicating all the other answers. Then, we created an additive scale with these 10 items, ranging from 0 to 10. With each factual knowledge (I knew this already) of each question, respondents scored one point in the additive scale.
Substance Use—We used six observed variables for the substance use latent variable, based on how long ago respondents used substances in any context. The six substances (see Table 1) were assessed with an 8-point recency scale, ranging from (1) “never” to (8) “in the past 24 h” (after inverting the original scale).
Sex Under the Influence of Substances (SUIS) – For this variable, the respondents were asked, “in the last 12 months, how much of the sex you’ve had with men has been under the influence of alcohol or any other drug?” The possible answers for this question ranged from (1) “none of it” to (7) “all of it”.
Statistical Analysis
We use RStudio and the ‘lavaan’ package (Rosseel, 2012) to analyse the hypothesized structural equation model. Prior to the analysis, the data was checked for multicollinearity, missing data, departures from normality and distributions. Multicollinearity was not present. Missing data were handled with pairwise deletion.
First, we examined descriptive statistics and correlation among variables used. Second, we estimated the confirmatory factor analysis (CFA) model. Finally, we estimated the hypothesized SEM presented in Fig. 1. Since we will be testing mediation effects, we follow the study of Shrout and Bolger, (2002) and use bias-corrected bootstrap method for estimating our model. This estimation method allows interval estimated without relying on a distribution assumption. Bias-corrected bootstrap estimation adjusts for possible bias and problematic skewness, if any, in the bootstrap samples’ distribution (Beaujean, 2014). Therefore, we estimated our SEM using a bootstrapped MLM estimator. The SEM had 16 observed variables, and 136 known parameters ((16*17) * ½ = 136). The total number of unknowns were 36 and constitutive of; 4 covariances, 16 factor loadings, 16 error variances. Thus, our model was over-identified with 100 (136–36) degrees of freedom, and over-identification is a necessary factor in structural model’s fit to data (Weston & Gore, 2006).
Hypothesized Structural Equation Model. Circles represent latent variables. Rectangles represent observed (manifest) variables. e* represent errors of observed variables to be estimated. Dashed paths represent the direct relationship (Hypothesis 1) to be mediated between Internalised Homonegativity and sexual risk behaviour. IHS1…7: Seven internalised homonegativity scale items. Drug-1…Drug-5: Ecstasy (pill), ecstasy (powder), speed, GHB/GHL (gamma-Hydroxybutyric acid/Butyrolactone), and cocaine use recency scales (in this order). Refer to Table 1 for detailed summary of the variables
Proceeding to the structural model, we examine its fit to the data. Evaluation of the structural model’s fit to the data is not a simple procedure (Raykov et al., 1991), and there are no universally accepted fit indices (Raykov et al., 1991; Saris et al., 2009; Thoemmes et al., 2018; Weston & Gore, 2006). To assess our model’s fit to our data, we examine both global and local fit indices. We do not pay attention to the significance of the χ2 statistic, as in large samples (N > 500) the χ2 is affected by sample size (Martens, 2005; Raykov et al., 1991; Weston & Gore, 2006). Furthermore, χ2 test statistics and global fit indices are asymmetrically sensitive to different misspecifications (Saris et al., 2009), thus we also look at the local fit indices; expected parameters change (EPC) and modification index (MI) test (Saris et al., 1987). These tests are done with examining the power of the EPC’s and significance of MI’s; whereas the combination of high-power EPC’s and nonsignificant MI’s indicate no misspecification, and the combination of low-power EPC’s and significant MI’s indicate the misspecification of the parameter(s).
For our SEM, we provide both unstandardized and standardized estimates of coefficients and errors. Unstandardized estimates do not depend on equal variances from our specific sample, therefore they serve as more generalizable estimates of the relationships (Grace & Bollen, 2005) and interpret the unstandardized coefficients of the estimates and errors of the hypothesized measurement model.
Results
In this section we provide results from our descriptive statistics, correlations matrix, CFA, and SEM. From Table 1, we see that possible scores for this scale ranged from 0 to 6, with higher scores indicating greater IH, and MSM in our sample had a mean score of 1.34 (SD = 1.22). For SRB, out of 3,694 MSM 59.7% (N = 2,205) reported no no-steady partners that they had condomless sex with, while 0.5% (N = 17) reported more than 50 partners in the last twelve months. In the HIV/PrEP additive scale, out of 3,838 MSM in Spain in our sample 432 respondents has acquired a score of 10, and 3 has acquired a score of 0; the mean score was 7.15. Almost half of respondents (46.2%, N = 1,717) reported no SUIS in the last twelve months, while a small portion reported almost all of it and all of it (4.74%, N = 176).
In Table 2 correlational analysis among main study variables is presented in order to examine the relationship between variables. Due to the nature of the variables used, some of them are highly correlated. For this reason, we use a p-value of 0.001 in order to reduce the possible Type I Error threat, following the study of Kashubeck-West and Szymanski (2008). From Table 2 we note that we did not find a relationship between IH and SRB, nor with each of the items of IH (except for the first item, IH1). On the other hand, we found that HIV/PrEP knowledge (r = 0.11) and SUIS (r = 0.18) were positively related to SRB, meaning that when these variables increased, SRB also increased. Similarly, more recent use of each substance was positively related to SRB, expect for alcohol. We will further test these relationships with using CFA and SEM.
Confirmatory Factor Analysis
As the first step in SEM, we test the model’s fit to the data using a CFA. For both CFA and SEM, there are copious measures to test model fit to the data (Meuleners et al., 2003). As commonly used global fit indices and based on Raykov et al. (1991), Hu and Bentler (1999) and Martens (2005), we used the following; (a) the Comparative Fit Index (CFI); (b) the Tucker-Lewis Index (TLI); (c) the root mean square error of approximation (RMSEA), and (d) Standardized root mean squared residual (SRMR). The majority of studies suggest that values higher than 0.95 for CFI and TLI indicate good fit (Hu & Bentler, 1999; Weston & Gore, 2006); while others suggest that CFI and TLI > 0.90 indicate a good fit to data (Moonie et al., 2009), as these fit indicates are susceptible to factors such as estimators and complexity (Xia & Yang, 2019). We use the cut-off value set by Hu and Bentler (1999). Further, Hu and Bentler (1999) suggested that values of RMSEA and SRMR < 0.06 are acceptable, and these values are widely accepted (Weston & Gore, 2006).
The results of the CFA proved that the model is a good fit to the data; CFI = 0.95, TLI = 0.95, RMSEA = 0.044 (90% confidence interval [CI] for the RMSEA lower bound = 0.041 and upper bound = 0.047), and SRMR = 0.03. A summary of these (and also for SEM, see below) fit indices can be found in Table 3.
Structural Equation Modelling
The SEM output for these global fit indices suggested that the measurement model (Fig. 1) was a good fit to the data; CFI = 0.96, TLI = 0.95, RMSEA = 0.044 (90% confidence interval [CI] for the RMSEA lower bound = 0.041 and upper bound = 0.047), and SRMR = 0.03. All of the parameter estimates were significant. Further, expected parameters change (EPC) and modification index (MI) test’s fit indices recommendations and cut-off values can be found in Table 3. All EPC’s and MI’s of the measurement model’s parameters are not mis-specified and each value meets the criteria suggested by Saris et al., (1987, 2009).
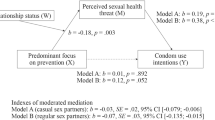
The unstandardized estimation results of SEM are presented in Fig. 2 and Table 4. In Fig. 2, we present the estimated SEM results, with upper numbers presenting the unstandardized path coefficients, numbers in brackets presenting standardized coefficients, and numbers in parenthesis presenting robust standard errors. In Table 4, we present the estimated results for the defined parameters (i.e. mediation effects) from the structural model.
Estimated SEM Results. Significance levels *p < 0.1, **p < 0.05, ***p < 0.01. Arrow width represents the strength of the relationships. Upper numbers are the unstandardized path coefficients; numbers in brackets are standardized coefficients; and numbers in parenthesis are robust standard errors. Dashed paths represent the direct relationship to be mediated between Internalised Homonegativity and sexual risk behaviour. Coefficients of observed variables and their standard errors are not shown
The direct path from IH to SRB (dashed line, Fig. 2) was statistically insignificant. Similarly, the defined parameter for the direct effect of IH to SRB (Table 4) was also insignificant. We did not find evidence for our first hypothesis, IH will be positively associated with SRB, at least not within a single country, in the specified SEM model.
As can be seen in Fig. 2, IH was negatively associated with HIV/PrEP knowledge, each unit increase in the IH latent variable was significantly associated with 0.39 decrease in the HIV/PrEP knowledge units. On the other hand, HIV/PrEP knowledge increases SRB, each unit increase in the HIV/PrEP knowledge was significantly associated with 0.04 increase in the SRB units. The indirect relationship between IH and SRB through HIV/PrEP knowledge was statistically significant (Table 4). An increase of 0.38 units in the IH latent variable was associated with 0.01 decrease SRB units, when mediated by the HIV/PrEP knowledge. Therefore, we found that as IH increased, the number of condomless intercourse with non-steady partners reported (SRB) decreased; because higher IH decreases HIV/PrEP knowledge while higher HIV knowledge predicted increased SRB. Thus, we found evidence for our second hypothesis, that HIV/PrEP knowledge will fully mediate the relationship between IH and sexual risk behaviour.
With respect to the relationship among IH, SUIS and SRB, we see that the relationship between IH and SUIS is insignificant, while the association between SUIS latent variable and SRB was positive and significant. Expectedly, Fig. 2 shows that a unit increase in SUIS was significantly associated with a 0.35 increase in the SRB units. The indirect path between IH and SRB mediated by SUIS was statistically insignificant (Table 4). Therefore, we did not find evidence for our third hypothesis that, sex under the influence of substances will fully mediate the relationship between IH and sexual risk behaviour.
In Fig. 2, we found that as IH decreased the recency of substance use. On the other hand, recency of substance use predicted SUIS significantly and positively. As can be seen in Table 4 (row 3), the indirect path from IH to SUIS when mediated by substance use recency, however, was statistically significant. As IH increased, SUIS decreased; because higher IH predicted less recent use of substances and more recent use of substances predicted higher numbers of sex under the influence of substances (SUIS). When looking at the variances, as expected, the role of alcohol in explaining the variances in SRB in comparison to rest of the substances is relatively small (0.032). The analysis has shown that particular substances in the SEM had greater influence than the rest, with ‘ecstasy’, regardless of its form, explaining the biggest share of the variances in the model (pill = 0.728; crystal = 0.701).
In another model (not shown here, available upon request), we added total number of partners (regardless of condom use or intercourse) in the last 12 months for controlling the HIV/PrEP knowledge latent variable. We found that the total number of partners is associated with increased HIV/PrEP knowledge significantly, and the rest of the results reported above stayed same or changed slightly. However, this model’s fit indices were very different than the accepted criteria (CFI = 0.89, TLI = 0.87, RMSEA = 0.073, SRMR = 0.064). Therefore, we did not include this variable in our SEM model. Implications of this variable on our current results will be discussed.
Discussion
In this study, we investigated the relation between two variables, IH and SRB, and the possible mediating effects of HIV/PrEP knowledge and SUIS in a sample of non-PrEP using MSM living in Spain, who are HIV-negative or have been diagnosed with HIV but have detectable or unknown viral load. Contrary to our hypothesis that IH will be positively associated with SRB, we did not find any direct effect of IH on SRB. Some studies found that higher levels of IH leads to SRB (Folch et al., 2009; Newcomb & Mustanski, 2010a; Puckett et al., 2017), while some studies did not find evidence for this direct relationship (Dawson et al., 2019; Newcomb & Mustanski, 2010a; Puckett et al., 2017), including ours. Therefore, our study further contributes to the literature which suggest that there might be potential mediating variables that affect the relation between IH and SRB (Kashubeck-West & Szymanski, 2008a; Newcomb & Mustanski, 2010b). On one hand, in line with this and our expectations, results of our SEM analysis showed that HIV/PrEP knowledge mediated the relationship between IH and SRB. On the other hand, the results indicated that while SUIS was significantly associated with SRB, it did not mediate the relationship between IH and SRB.
We found that the more knowledgeable men are about how HIV is transmitted and PrEP works, the higher the numbers of condomless sexual intercourse with non-steady partners reported. One explanation for this surprising result might be that these men, in particular, take their sexual health seriously and are confident in knowing when to use condom and in their condom negotiation skills with non-steady partners. For example, Klein (2013) found that condom use self-efficacy, which refers to an individual’s self-confidence in their ability to use condoms, was significantly and positively associated with HIV knowledge. Therefore, these men may be more comfortable initiating conversation about how long ago they have been tested, whether their non-steady partner is using PrEP, or negotiate safeness that go into sex (i.e. knowing that no HIV transmissions from the HIV-positive partner to the HIV-negative partner would occur if their viral load is undetectable (“U = U; Undetectable = Untransmittable”)). Our additional analysis (not shown in the paper, available upon request) has shown that the total number of partners may, in return, influence HIV/PrEP knowledge. Similarly, men who have a higher number of partners might have a better connection to the gay community and an increased chance of acquiring more knowledge about protecting themselves. Empirical theories about the link between behaviour and knowledge suggest that self-perceived vulnerability to HIV is probably the main factor underlying SRB, more so than knowledge (McKusik et al., 1985). That is, when people perceive that they are less vulnerable to HIV, they would be more likely to engage in potential sexual risk behaviour, independent of their knowledge about HIV. Moreover, HIV knowledge showed to be necessary, but not sufficient, to motivate individuals to avoid HIV-related risks (Pando et al., 2013). Therefore, HIV prevention programs should consider focusing on communicating what actually makes one less vulnerable to HIV, which is the knowledge that goes into the ability to negotiate safe sex.
We found that as IH increased, the number of condomless intercourse with non-steady partners reported (SRB) decreased; because higher IH decreases HIV/PrEP knowledge while higher HIV knowledge predicted increased SRB. A high level of IH may serve as a barrier to participation in HIV testing and other health-promoting behaviours, and less contact with prevention and educational interventions. From previous studies we know that men with higher IH showed a reduced perception of their self-efficacy for condom use, even after intervention (Huebner et al., 2002). This finding may be indicative of certain men with high IH who are not confident and knowledgeable enough to communicate safer sex practices with non-steady partners. Alternatively, it is possible that the men with higher IH in our sample are less likely to be involved in sexual intercourse with non-steady partners in the first place. However, our conclusions are in consistency with the notion that IH is most likely harmful; higher levels of IH may lead to reduced number of non-steady partners, but it also reduces relevant knowledge to protect oneself (Ross et al., 2013), or is associated with condom use frequency in general, and is not directly associated with the number of non-steady partners. As discussed, with the development of PrEP the meaning of ‘risky’ sex may also change for MSM; with the number of partners not relating to risk if one knows how to protect oneself. Therefore, future research and prevention programs should consider different indicators for ‘risky sex’ in an aim to target those who not only have condomless sex with random partners, but those who do not know how to protect themselves.
MSM in our sample who were more prone to use alcohol or any other drug during sexual intercourse reported higher frequency of anal sex with non-steady partners without using condom. Provided they are, or their partner is seropositive (in the case of not knowing one’s own or partner’s HIV status), use of substances during sex can be of immediate relevance for risk of HIV exposure, for each individual. Further, higher IH was not associated with increased SUIS, nor was SUIS a variable through which IH influenced sexual risk behaviour. Connection to the gay community may promote unhealthy behaviours through submersion into a subculture that promotes drug use and provides easier access to drugs (Halkitis et al., 2005). High levels of IH may serve as a barrier to engagement with the gay community, thereby also serving as a barrier from community level factors that lead to greater substance use (Moody et al., 2018). These results emphasize the continuing importance of community level interventions that address substance use in the gay community.
Our results show that SUIS predicted the higher numbers of condomless intercourse with non-steady partners reported, without IH influencing SUIS. We found that substance use recency mediated the relationship between IH and SUIS. As IH increased, SUIS decreased; because higher IH predicted less recent use of substances and more recent use of substances predicted higher numbers of SUIS. When looking at the variances, as expected, the role of alcohol in explaining the variances in SRB in comparison to rest of the substances is relatively small (0.032). The analysis has shown that particular substances in the SEM had greater influence than the rest, with ecstasy explaining the largest share of the variances in the model (pill = 0.728; crystal = 0.701)—which is in line with how the question was asked (i.e. the question was asked as the most recent use of substances, and not the recent use of substances in amounts that would affect one’s thinking or decision-making).
Strength and Limitations
Our study has several methodological strengths, including being the largest dataset of MSM living in Spain and use of SEM. We also note its limitations. We use recency time formats (when did you last…) for substance use variables, which further reduces the chance of recall bias—unlike frequency formats, which is not natural for most people. Similarly, there is no recall bias in knowledge, or the proportion of sex under the influence of substances. Accurately reporting partner numbers is generally a problem; but that does not affect our conclusions. Another strength of this survey lies in its anonymous character, through which the risk of social desirability bias is reduced (as opposed to the interview setting). While we used a large, diverse sample of MSM, the data come from a non-probability sample, potentially limiting generalizability, especially to those who are older, have lower education, fewer LGBT community attachments, or are more likely to conceal their sexual orientation (Prah et al., 2016). Yet, our analyses assume that the distribution of variables in the EMIS-2017 sample matches the distribution of these variables in the population. Further, non-probability sampling can also lead to higher estimates of sexual risk, drug use, or knowledge among MSM. These concerns are somewhat attenuated given that the present study was not focused on establishing population estimates or risk behaviours, HIV/PrEP knowledge, or IH, but instead sought to examine associations among variables, for which non-probability sampling is more appropriate (Meyer & Wilson, 2009). Further, probability-based studies typically include relatively small numbers of sexual minorities in one country only, and thus would not have provided an adequate sample size across numerous countries with which to evaluate our research aims.
Conclusion
The impacts of IH on the sexual risk behaviours of gay, bisexual and other MSM have been extensively studied, and we extend knowledge of the nature of the relation by attempting to disentangle the potential influence of HIV-related knowledge and substance use. Our SEM results suggest that IH is not directly implicated in the path to SRB and that HIV/PrEP knowledge, but not SUIS, mediate the relationship between IH and SRB. Future prevention strategies should also target specific counselling for MSM with low IH, and who are relatively knowledgeable about HIV risks and how PrEP works, in order to ensure that they are included within the prevention messages. Similarly, future interventions should consider addressing particular problems at the community level, such as substance use in general, sex under the influence of substances, and social homophobia which is exercised structurally against individuals.
Availability of Data and Material
Data is property of the LSHTM and can be accessed upon reasonable request to coordinator@emis-project.eu.
Code Availability
Not applicable.
References
Andrinopoulos, K., Hembling, J., Guardado, M. E., de Maria Hernández, F., Nieto, A. I., & Melendez, G. (2015). Evidence of the negative effect of sexual minority stigma on HIV testing among msm and transgender women in San Salvador El Salvador. AIDS and Behavior, 19(1), 60–71. https://doi.org/10.1007/s10461-014-0813-0
Baral, S., Logie, C. H., Grosso, A., Wirtz, A. L., & Beyrer, C. (2013). Modified social ecological model: A tool to guide the assessment of the risks and risk contexts of HIV epidemics. BMC Public Health. https://doi.org/10.1186/1471-2458-13-482
Beaujean, A. A. (2014). Appendix: Bootstrapping Latent Variable Models, in Latent Variable Modeling using R: A Step-by-Step Guide. Routledge. https://cpb-us-w2.wpmucdn.com/blogs.baylor.edu/dist/0/4392/files/2013/12/AppendixBootstrapping-1gyf69b.pdf
Berg, R. C., Ross, M. W., Weatherburn, P., & Schmidt, A. J. (2013). Structural and environmental factors are associated with internalised homonegativity in men who have sex with men: Findings from the European MSM internet survey (EMIS) in 38 countries. Social Science & Medicine, 78, 61–69. https://doi.org/10.1016/j.socscimed.2012.11.033
Berg, R. C., Weatherburn, P., Ross, M. W., & Schmidt, A. J. (2015). The relationship of internalized homonegativity to sexual health and well-being among men in 38 European countries who have sex with men. Journal of Gay & Lesbian Mental Health, 19(3), 285–302. https://doi.org/10.1080/19359705.2015.1024375
Centro Nacional de Epidemiología. (2018). Plan Nacional sobre el Sida, 2017 (Vigilancia Epidemiológica Del VIH y Sida En España. Sistema de Información Sobre Nuevos Diagnósticos de VIH y Registro Nacional de Casos de Sida). https://www.mscbs.gob.es/ciudadanos/enfLesiones/enfTransmisibles/sida/vigilancia/doc/InformeVIH_SIDA_2018_21112018.pdf
Centro Nacional de Epidemiología. (2020). Vigilancia Epidemiológica del VIH y SIDA en España 2019. Instituto de Salud Carlos III/Plan Nacional sobre el Sida, Dirección General de Salud Pública, Calidad e Innovación. https://www.mscbs.gob.es/ciudadanos/enfLesiones/enfTransmisibles/sida/vigilancia/Informe_VIH_SIDA_20201130.pdf
Dawson, E. L., Mendoza, M. C. B., Gaul, Z., Jeffries, W. L., IV., Sutton, M. Y., & Wilson, P. A. (2019). Resilience, condom use self-efficacy, internalized homophobia, and condomless anal sex among black men who have sex with men New York City. PLoS ONE, 14(4), e0215455. https://doi.org/10.1371/journal.pone.0215455
Dudley, M. G., Rostosky, S. S., Korfhage, B. A., & Zimmerman, R. S. (2004). Correlates of high-risk sexual behavior among young men who have sex with men. AIDS Education and Prevention, 16(4), 328–340. https://doi.org/10.1521/aeap.16.4.328.40397
European Centre for Disease Prevention and Control & World Health Organization. (2020). HIV/AIDS surveillance in Europe 2020: 2019 data. Publications Office. https://data.europa.eu/doi/https://doi.org/10.2900/073965
Fernández-Dávila, P., & Zaragoza Lorca, K. (2009). Internet y riesgo sexual en hombres que tienen sexo con hombres. Gaceta Sanitaria, 23(5), 380–387. https://doi.org/10.1016/j.gaceta.2008.11.004
Folch, C., Esteve, A., Zaragoza, K., Munoz, R., & Casabona, J. (2010). Correlates of intensive alcohol and drug use in men who have sex with men in Catalonia, Spain. The European Journal of Public Health, 20(2), 139–145. https://doi.org/10.1093/eurpub/ckp091
Folch, C., Marks, G., Esteve, A., Zaragoza, K., Muñoz, R., & Casabona, J. (2006). Factors associated with unprotected sexual intercourse with steady male, casual male, and female partners among men who have sex with men in Barcelona Spain. AIDS Education and Prevention, 18(3), 227–242. https://doi.org/10.1521/aeap.2006.18.3.227
Folch, C., Muñoz, R., Zaragoza, K., & Casabona, J. (2009). Sexual risk behaviour and its determinants among men who have sex with men in Catalonia Spain. Eurosurveillance. https://doi.org/10.2807/ese.14.47.19415-en
Goldbach, J. T., Schrager, S. M., Dunlap, S. L., & Holloway, I. W. (2015). The application of minority stress theory to Marijuana use among sexual minority adolescents. Substance Use & Misuse, 50(3), 366–375. https://doi.org/10.3109/10826084.2014.980958
González-Baeza, A., Dolengevich-Segal, H., Pérez-Valero, I., Cabello, A., Téllez, M. J., Sanz, J., Pérez-Latorre, L., Bernardino, J. I., Troya, J., De La Fuente, S., Bisbal, O., Santos, I., Arponen, S., Hontañon, V., Casado, J. L., Ryan, P., & The U-SEX GESIDA 9416 Study. (2018). Sexualized drug use (Chemsex) is associated with high-risk sexual behaviors and sexually transmitted infections in HIV-positive men who have sex with men: Data from the U-SEX GESIDA 9416 Study. AIDS Patient Care and STDs, 32(3), 112–118. https://doi.org/10.1089/apc.2017.0263
Grace, J. B., & Bollen, K. A. (2005). Interpreting the results from multiple regression and structural equation models. Bulletin of the Ecological Society of America, 86(4), 283–295. https://doi.org/10.1890/0012-9623(2005)86[283:ITRFMR]2.0.CO;2
Halkitis, P. N., Fischgrund, B. N., & Parsons, J. T. (2005). Explanations for methamphetamine use among gay and bisexual men in New York City. Substance Use & Misuse, 40(9–10), 1331–1345. https://doi.org/10.1081/JA-200066900
Herek, G. M. (2004). Beyond “Homophobia”: Thinking about sexual prejudice and stigma in the twenty-first century. Sexuality Research and Social Policy, 1(2), 6–24. https://doi.org/10.1525/srsp.2004.1.2.6
Hu, L., & Bentler, P. M. (1999). Cutoff criteria for fit indexes in covariance structure analysis: Conventional criteria versus new alternatives. Structural Equation Modeling: A Multidisciplinary Journal, 6(1), 1–55. https://doi.org/10.1080/10705519909540118
Huebner, D. M., Davis, M. C., Nemeroff, C. J., & Aiken, L. S. (2002). The impact of internalized homophobia on HIV preventive interventions. American Journal of Community Psychology, 30(3), 327–348. https://doi.org/10.1023/A:1015325303002
Kashubeck-West, S., & Szymanski, D. M. (2008). Risky sexual behavior in gay and bisexual men: Internalized heterosexism, sensation seeking, and substance use. The Counseling Psychologist, 36(4), 595–614. https://doi.org/10.1177/0011000007309633
Klein, H. (2013). Condom use self-efficacy and HIV risk practices among men who use the internet to find male partners for unprotected sex. American Journal of Men’s Health, 8(3), 190–204. https://doi.org/10.1177/1557988313492172
Lelutiu-Weinberger, C., Pachankis, J. E., Golub, S. A., Walker, J. J., Bamonte, A. J., & Parsons, J. T. (2013). Age cohort differences in the effects of gay-related stigma, anxiety and identification with the gay community on sexual risk and substance use. AIDS and Behavior, 17(1), 340–349. https://doi.org/10.1007/s10461-011-0070-4
Malyon, A. K. (1982). Psychotherapeutic implications of internalized homophobia in gay men. Journal of Homosexuality, 7(2–3), 59–69. https://doi.org/10.1300/J082v07n02_08
Martens, M. P. (2005). The use of structural equation modeling in counseling psychology research. The Counseling Psychologist, 33(3), 269–298. https://doi.org/10.1177/0011000004272260
McKusik, L., Wiley, J., Coates, T. J., Stall, R., Glen, S., Morin, S., Charles, K., Horstman, W., & Conant, M. A. (1985). Reported changes in the sexual behavior of men at risk for AIDS, San Francisco, 1982–84 the AIDS behavioral research project. Public Health Reports, 100(6), 622–629.
Meuleners, L. B., Lee, A. H., Binns, C. W., & Lower, A. (2003). Quality of life for adolescents: Assessing measurement properties using structural equation modelling. Quality of Life Research, 12, 283–290.
Meyer, I. H. (2003). Prejudice, social stress, and mental health in lesbian, gay, and bisexual populations: Conceptual issues and research evidence. Psychological Bulletin, 129(5), 674–697.
Meyer, I. H., & Wilson, P. A. (2009). Sampling lesbian, gay, and bisexual populations. Journal of Counseling Psychology, 56(1), 23–31. https://doi.org/10.1037/a0014587
Mirandola, M., Gios, L., Sherriff, N., Marcus, U., Toskin, I., Rosinska, M., Schink, S., Kühlmann-Berenzon, S., Suligoi, B., Folch, C., Nöstlinger, C., Dias, S., Stanekova, D., Klavs, I., Caplinskas, S., Rafila, A., Marin, C., Alexiev, I., Zohrabyan, L., & on behalf of the SIALON II Network. (2018). Quantifying unmet prevention needs among MSM in Europe through a multi-site bio-behavioural survey. Eurosurveillance. https://doi.org/10.2807/1560-7917.ES.2018.23.49.1800097
Moody, R. L., Starks, T. J., Grov, C., & Parsons, J. T. (2018). Internalized homophobia and drug use in a national cohort of gay and bisexual men: Examining depression, sexual anxiety, and gay community attachment as mediating factors. Archives of Sexual Behavior, 47(4), 1133–1144. https://doi.org/10.1007/s10508-017-1009-2
Moonie, S., Huang, X., & Sterling, D. A. (2009). Quality of life estimation with structural equation modeling in school aged children with asthma. Global Health Governance, 3, 1–16.
Newcomb, M. E., & Mustanski, B. (2010a). Internalized homophobia and internalizing mental health problems: A meta-analytic review. Clinical Psychology Review, 30(8), 1019–1029. https://doi.org/10.1016/j.cpr.2010.07.003
Newcomb, M. E., & Mustanski, B. (2010b). The importance of measuring internalized homophobia/homonegativity: Reply to Ross, Rosser, and Smolenski (2010a). Archives of Sexual Behavior, 39(6), 1209–1211. https://doi.org/10.1007/s10508-010-9655-7
Newcomb, M. E., & Mustanski, B. (2011). Moderators of the relationship between internalized homophobia and risky sexual behavior in men who have sex with men: A meta-analysis. Archives of Sexual Behavior, 40(1), 189–199. https://doi.org/10.1007/s10508-009-9573-8
Pando, M. A., Balan, I., Marone, R., Dolezal, C., Barreda, V., Carballo Dieguez, A., & Avila, M. M. (2013). HIV Knowledge and beliefs among men who have sex with men (MSM) in Buenos Aires Argentina. AIDS and Behavior, 17(4), 1305–1312. https://doi.org/10.1007/s10461-012-0404-x
Prah, P., Hickson, F., Bonell, C., McDaid, L. M., Johnson, A. M., Wayal, S., Clifton, S., Sonnenberg, P., Nardone, A., Erens, B., Copas, A. J., Riddell, J., Weatherburn, P., & Mercer, C. H. (2016). Men who have sex with men in Great Britain: Comparing methods and estimates from probability and convenience sample surveys. Sexually Transmitted Infections, 92(6), 455–463. https://doi.org/10.1136/sextrans-2015-052389
Puckett, J. A., Newcomb, M. E., Garofalo, R., & Mustanski, B. (2017). Examining the conditions under which internalized homophobia is associated with substance use and condomless sex in young MSM: The moderating role of impulsivity. Annals of Behavioral Medicine, 51(4), 567–577. https://doi.org/10.1007/s12160-017-9878-0
Raykov, T., Tomer, A., & Nesselroade, J. R. (1991). Reporting structural equation modeling results in psychology and aging: Some proposed guidelines. Psychology and Aging, 6(4), 499–503. https://doi.org/10.1037//0882-7974.6.4.499
Ross, M. W., Kajubi, P., Mandel, J. S., McFarland, W., & Raymond, H. F. (2013). Internalized homonegativity/homophobia is associated with HIV-risk behaviours among Ugandan gay and bisexual men. International Journal of STD & AIDS, 24(5), 409–413. https://doi.org/10.1177/0956462412472793
Ross, M. W., Rosser, B. R. S., Bauer, G. R., Bockting, W. O., Robinson, E., Rugg, D. L., & Coleman, E. (2001). Drug use, unsafe sexual behavior, and internalized homonegativity in men who have sex with men. AIDS and Behavior, 7, 1–97.
Rosseel, Y. (2012). lavaan: An R package for structural equation modeling. Journal of Statistical Software, 48(2), 1–36.
Ministerio de Sanidad. (2020). Encuesta europea on-line para hombres que tienen sexo con hombres (EMIS-2017): Resultados en España.
Saris, W. E., Satorra, A., & Sorbom, D. (1987). The detection and correction of specification errors in structural equation models. Sociological Methodology, 17, 105–129. https://doi.org/10.2307/271030
Saris, W. E., Satorra, A., & van der Veld, W. M. (2009). Testing structural equation models or detection of misspecifications? Structural Equation Modeling: A Multidisciplinary Journal, 16(4), 561–582. https://doi.org/10.1080/10705510903203433
Shrout, P. E., & Bolger, N. (2002). Mediation in experimental and nonexperimental studies: New procedures and recommendations. Psychological Methods, 7(4), 422–445. https://doi.org/10.1037/1082-989X.7.4.422
Stein, T. S., & Cohen, C. J. (Eds.). (1986). Contemporary perspectives on psychotherapy with lesbians and gay men. US: Springer. https://doi.org/10.1007/978-1-4757-9832-6
Thoemmes, F., Rosseel, Y., & Textor, J. (2018). Local fit evaluation of structural equation models using graphical criteria. Psychological Methods, 23(1), 27–41. https://doi.org/10.1037/met0000147
Tran, H., Ross, M. W., Diamond, P. M., Berg, R. C., Weatherburn, P., & Schmidt, A. J. (2018). Structural validation and multiple group assessment of the short internalized homonegativity scale in homosexual and bisexual men in 38 European countries: Results from the European MSM internet survey. The Journal of Sex Research, 55(4–5), 617–629. https://doi.org/10.1080/00224499.2017.1380158
Velter, A., Saboni, L., Sommen, C., Bernillon, P., Bajos, N., & Semaille, C. (2015). Sexual and prevention practices in men who have sex with men in the era of combination HIV prevention: Results from the presse gays et lesbiennes survey, France, 2011. Eurosurveillance. https://doi.org/10.2807/1560-7917.ES2015.20.14.21090
Weatherburn, P., Hickson, F., Reid, D. S., Marcus, U., & Schmidt, A. J. (2020). European men-who-have-sex-with-men Internet survey (EMIS-2017): Design and methods. Sexuality Research and Social Policy, 17(4), 543–557. https://doi.org/10.1007/s13178-019-00413-0
Weston, R., & Gore, P. A. (2006). A brief guide to structural equation modeling. The Counseling Psychologist, 34(5), 719–751. https://doi.org/10.1177/0011000006286345
Williamson, I. R. (2000). Internalized homophobia and health issues affecting lesbians and gay men. Health Education Research, 15(1), 97–107. https://doi.org/10.1093/her/15.1.97
Xia, Y., & Yang, Y. (2019). RMSEA, CFI, and TLI in structural equation modeling with ordered categorical data: The story they tell depends on the estimation methods. Behavior Research Methods, 51(1), 409–428. https://doi.org/10.3758/s13428-018-1055-2
Acknowledgements
EMIS-2017 was coordinated by Sigma Research at the London School of Hygiene and Tropical Medicine (LSHTM) in association with the Robert Koch Institute (RKI) in Berlin. EMIS core team @ Sigma Research (LSHTM): Dr Axel J. Schmidt, Dr Ford Hickson; David Reid, and Peter Weatherburn; in association with Dr Ulrich Marcus and Dr Susanne B. Schink @ RKI. We thank all participants and all our partners for being part of something huge. We would like to thank Asunción Díaz (Instituto de Salud Carlos III, CNE, Ministerio de Ciencia e Innovación), Maria C. Vázquez (SPNS, Ministerio de Sanidad), Sebastian Meyer (Asociación Stop Sida) for reviewing and commenting on the final version of the manuscript. In particular, we would like to thank the following companies and organisations: PlanetRomeo, Stop Sida (Spain) European AIDS Treatment Group (EATG), European Centre for Disease Prevention and Control (ECDC), European Monitoring Centre for Drugs & Drug Addiction (EMCDDA), European Commission (DG SANTE). Finally, we would like to thank Maria Jose Gonzalez Lopez, who continuously provided feedback for the development of this article.
Funding
Open Access funding provided thanks to the CRUE-CSIC agreement with Springer Nature. EMIS-2017 was carried out as part of ESTICOM, under the service contract 2015 71 01 with The Consumers, Health, Agriculture and Food Executive Agency (Chafea), acting under powers delegated by the Commission of the European Union. The contract arises from the Call for tender No Chafea/2015/Health/38.
Author information
Authors and Affiliations
Contributions
Methodology, formal analysis and investigation: İS. Conceptualization and design: İS, AJS, CF, NL, and RB. Resources and data: AJS. Writing—original draft preparation: İS. Writing—introduction: CF, NL. Writing—sample and data: AJS. Writing—discussion: İS, AJS, CF, NL, RB, NT. Writing—conclusion: RB. Supervision of development: AJS. Supervision of statistical analysis: NT.
Corresponding author
Ethics declarations
Conflict of interest
The authors declare that they have no conflict of interest.
Ethical Approval
The Observational Research Ethics Committee at the London School of Hygiene and Tropical Medicine approved the original study (Reference 14421/RR/8805).
Consent to Participate
All participants included in this analysis indicated online, prior to providing their answers, that they understand the nature and purpose of the study and consented to take part.
Consent for Publication
Not applicable.
Additional information
Publisher's Note
Springer Nature remains neutral with regard to jurisdictional claims in published maps and institutional affiliations.
Rights and permissions
Open Access This article is licensed under a Creative Commons Attribution 4.0 International License, which permits use, sharing, adaptation, distribution and reproduction in any medium or format, as long as you give appropriate credit to the original author(s) and the source, provide a link to the Creative Commons licence, and indicate if changes were made. The images or other third party material in this article are included in the article's Creative Commons licence, unless indicated otherwise in a credit line to the material. If material is not included in the article's Creative Commons licence and your intended use is not permitted by statutory regulation or exceeds the permitted use, you will need to obtain permission directly from the copyright holder. To view a copy of this licence, visit http://creativecommons.org/licenses/by/4.0/.
About this article
Cite this article
Sönmez, İ., Folch, C., Lorente, N. et al. Influence of Internalised Homonegativity on Sexual Risk Behaviour of Men Who Have Sex with Men in Spain. Sexuality & Culture 26, 932–950 (2022). https://doi.org/10.1007/s12119-021-09925-7
Accepted:
Published:
Issue Date:
DOI: https://doi.org/10.1007/s12119-021-09925-7