Abstract
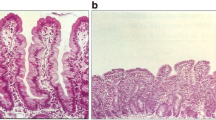
Recent diagnostic advances have demonstrated that celiac disease is relatively common although most patients have less florid symptoms than previously recognised. The mucosal lesion of this autoimmune disorder depends on both adaptive and innate immune responses. The characteristic antibodies to tissue transglutaminase-2 (tTG-2) and deamidated gliadin peptides may be produced in persons possessing the relevant HLA-DQ genotypes if intact gliadin peptides can penetrate the epithelial barrier to reach antigen presenting cells. Progression from celiac autoimmunity to overt disease may depend on innate immune mechanisms, not HLA-restricted, where IL-15 is generated within the epithelial compartment. A specific innate immune response previously thought restricted to invertebrates, the encapsulation reaction, may contribute to mucosal volume expansion through recruitment of syndecan-expressing leukocytes and stimulated matrix production. It is notable that tissue transglutaminase is critical in this reaction in insects, and that the very few insects that can predate wheat, possess specific salivary or intestinal enzymes that degrade gluten. Animal models in HLA-DQ transgenic mice suggest that the microbial flora of the intestine may play a role in host responses and modulate the evolution of the disease. This suggests that therapeutic modulation of the microbiome may contribute to management of celiac disease. In developing world countries, there is a potential difficulty in histological diagnosis because of the widespread incidence of environmental enteropathy amongst apparently healthy children. Thus, recognition of local patterns of enteropathy will be important for histopathologists, and high titre tTG-2 autoantibody titres may hold considerable diagnostic significance.


Similar content being viewed by others
References
Dowd B, Walker-Smith J. Samuel gee, Aretaeus, and the coeliac affection. BMJ. 1974;2:45–7.
van Berge-Henegouwen GP, Mulder CJ. Pioneer in the gluten free diet: Willem-Karel Dicke 1905-1962, over 50 years of gluten free diet. Gut. 1993;34:1473–5.
Paulley JW. Observations on the aetiology of idiopathic steatorrhoea. BMJ. 1954;2:1318–21.
Sakula J, Shiner M. Coeliac disease with atrophy of the small intestine mucosa. Lancet. 1957;273:876–7.
De Re V, Caggiari L, Tabuso M, Cannizzaro R. The versatile role of gliadin peptides in celiac disease. Clin Biochem. 2013;46:552–60.
Abadie V, Sollid LM, Barreiro LB, Jabri B. Integration of genetic and immunological insights into a model of celiac disease pathogenesis. Annu Rev Immunol. 2011;29:493–525.
Ludvigsson JF, Leffler DA, Bai JC, et al. The Oslo definitions for coeliac disease and related terms. Gut. 2013;62:43–52.
Veitch AM, Kelly P, Zulu IS, Segal I, Farthing MJ. Tropical enteropathy: a T-cell-mediated crypt hyperplastic enteropathy. Eur J Gastroenterol Hepatol. 2001;13:1175–81.
Campbell DI, Murch SH, Lunn PG, et al. Chronic T cell-mediated enteropathy in rural west African children: relationship with nutritional status and small bowel function. Pediatr Res. 2003;54:306–11.
van Gils T, Nijeboer P, van Wanrooij RL, Bouma G, Mulder CJ. Mechanisms and management of refractory coeliac disease. Nat Rev Gastroenterol Hepatol. 2015;12:572–9.
Maki M, Holm K, Koskimies S, Hallstrom O, Visakorpi JK. Normal small bowel biopsy followed by coeliac disease. Arch Dis Child. 1990;65:1137–41.
Steens RF, Csizmadia CG, George EK, Ninaber MK, Hira Sing RA, Mearin ML. A national prospective study on childhood celiac disease in the Netherlands 1993-2000: an increasing recognition and a changing clinical picture. J Pediatr. 2005;147:239–43.
Kang JY, Kang AH, Green A, Gwee KA, Ho KY. Systematic review: worldwide variation in the frequency of coeliac disease and changes over time. Aliment Pharmacol Ther. 2013;38:226–45.
Rätsch IM, Catassi C. Coeliac disease: a potentially treatable health problem of Saharawi refugee children. Bull World Health Organ. 2001;79:541–5.
Lionetti E, Gatti S, Pulvirenti A, Catassi C. Celiac disease from a global perspective. Best Pract Res Clin Gastroenterol. 2015;29:365–79.
Makharia GK, Verma AK, Amarchand R, et al. Prevalence of celiac disease in the northern part of India: a community based study. J Gastroenterol Hepatol. 2011;26:894–900.
Crane RJ, Jones KD, Berkley JA. Environmental enteric dysfunction: an overview. Food Nutr Bull. 2015;36:S76–87.
Keusch GT, Denno DM, Black RE, et al. Environmental enteric dysfunction: pathogenesis, diagnosis, and clinical consequences. Clin Infect Dis. 2014;59:S207–12.
Bhattacharya M, Lomash A, Sakhuja P, Dubey AP, Kapoor S. Clinical and histopathological correlation of duodenal biopsy with IgA anti-tissue transglutaminase titers in children with celiac disease. Indian J Gastroenterol. 2014;33:350–4.
Mubarak A, Spierings E, Wolters V, van Hoogstraten I, Kneepkens CM, Houwen R. Human leukocyte antigen DQ2.2 and celiac disease. J Pediatr Gastroenterol Nutr. 2013;56:428–30.
Liu E, Lee HS, Aronsson CA, et al; TEDDY Study Group. Risk of pediatric celiac disease according to HLA haplotype and country. N Engl J Med. 2014;371:42–9.
Lionetti E, Castellaneta S, Francavilla R, et al; SIGENP (Italian Society of Pediatric Gastroenterology, Hepatology, and Nutrition) Working Group on Weaning and CD Risk. Introduction of gluten, HLA status, and the risk of celiac disease in children. N Engl J Med. 2014;371:1295–303.
Ivarsson A, Myléus A, Norström F, et al. Prevalence of childhood celiac disease and changes in infant feeding. Pediatrics. 2013;131:e687–94.
Gutierrez-Achury J, Coutinho d AR, Wijmenga C. Shared genetics in coeliac disease and other immune-mediated diseases. J Intern Med. 2011;269:591–603.
Verdu EF, Galipeau HJ, Jabri B. Novel players in coeliac disease pathogenesis: role of the gut microbiota. Nat Rev Gastroenterol Hepatol. 2015;12:497–506.
Olivares M, Neef A, Castillejo G, et al. The HLA-DQ2 genotype selects for early intestinal microbiota composition in infants at high risk of developing coeliac disease. Gut. 2015;64:406–17.
Galipeau HJ, McCarville JL, Huebener S, et al. Intestinal microbiota modulates gluten-induced immunopathology in humanized mice. Am J Pathol. 2015;185:2969–82.
Husby S, Koletzko S, Korponay-Szabó IR, et al; ESPGHAN Working Group on Coeliac Disease Diagnosis; ESPGHAN Gastroenterology Committee; European Society for Pediatric Gastroenterology, Hepatology, and Nutrition. European Society for Pediatric Gastroenterology, Hepatology, and Nutrition guidelines for the diagnosis of coeliac disease. J Pediatr Gastroenterol Nutr. 2012;54:136–60.
Amarri S, Alvisi P, De Giorgio R, et al. Antibodies to deamidated gliadin peptides: an accurate predictor of coeliac disease in infancy. J Clin Immunol. 2013;33:1027–30.
Lammi A, Arikoski P, Simell S, et al. Antibodies to deamidated gliadin peptide in diagnosis of celiac disease in children. J Pediatr Gastroenterol Nutr. 2015;60:626–31.
Giersiepen K, Lelgemann M, Stuhldreher N, et al; ESPGHAN Working Group on Coeliac Disease Diagnosis. Accuracy of diagnostic antibody tests for coeliac disease in children: summary of an evidence report. J Pediatr Gastroenterol Nutr. 2012;54:229–41.
Taavela J, Koskinen O, Huhtala H, et al. Validation of morphometric analyses of small-intestinal biopsy readouts in celiac disease. PLoS One. 2013;8:e76163.
Murch S, Jenkins H, Auth M, et al. Joint BSPGHAN and Coeliac UK guidelines for the diagnosis and management of coeliac disease in children. Arch Dis Child. 2013;98:806–11.
Downey L, Houten R, Murch S, Longson D; Guideline Development Group. Recognition, assessment, and management of coeliac disease: summary of updated NICE guidance. BMJ. 2015;351:h4513.
Kiefte-de Jong JC, Jaddoe VW, Uitterlinden AG, et al. Levels of antibodies against tissue transglutaminase during pregnancy are associated with reduced fetal weight and birth weight. Gastroenterology. 2013;144:726–35.
Anjum N, Baker PN, Robinson NJ, Aplin JD. Maternal celiac disease autoantibodies bind directly to syncytiotrophoblast and inhibit placental tissue transglutaminase activity. Reprod Biol Endocrinol. 2009;7:16.
Di Simone N, Silano M, Castellani R, et al. Anti-tissue transglutaminase antibodies from celiac patients are responsible for trophoblast damage via apoptosis in vitro. Am J Gastroenterol. 2010;105:2254–61.
Sapone A, Lammers KM, Mazzarella G, et al. Differential mucosal IL-17 expression in two gliadin-induced disorders: gluten sensitivity and the autoimmune enteropathy celiac disease. Int Arch Allergy Immunol. 2010;152:75–80.
Salvestrini C, Lucas M, Lionetti P, et al. Matrix expansion and syncytial aggregation of syndecan-1+ cells underpin villous atrophy in coeliac disease. PLoS One. 2014;9:e106005.
Fernández S, Molina IJ, Romero P, et al. Characterization of gliadin-specific Th17 cells from the mucosa of celiac disease patients. Am J Gastroenterol. 2011;106:528–38.
Harris KM, Fasano A, Mann DL. Monocytes differentiated with IL-15 support Th17 and Th1 responses to wheat gliadin: implications for celiac disease. Clin Immunol. 2010;135:430–9.
Maiuri L, Ciacci C, Ricciardelli I, et al. Association between innate response to gliadin and activation of pathogenic T cells in coeliac disease. Lancet. 2003;362:30–7.
Nanayakkara M, Lania G, Maglio M, et al. An undigested gliadin peptide activates innate immunity and proliferative signaling in enterocytes: the role in celiac disease. Am J Clin Nutr. 2013;98:1123–35.
Jelínková L, Tucková L, Cinová J, Flegelová Z, Tlaskalová-Hogenová H. Gliadin stimulates human monocytes to production of IL-8 and TNF-alpha through a mechanism involving NF-κB. FEBS Lett. 2004;571:81–5.
Rakhimova M, Esslinger B, Schulze-Krebs A, Hahn EG, Schuppan D, Dieterich W. In vitro differentiation of human monocytes into dendritic cells by peptic-tryptic digest of gliadin is independent of genetic predisposition and the presence of celiac disease. J Clin Immunol. 2009;29:29–37.
Bernardo D, Garrote JA, Fernández-Salazar L, Riestra S, Arranz E. Is gliadin really safe for non-coeliac individuals? Production of interleukin 15 in biopsy culture from non-coeliac individuals challenged with gliadin peptides. Gut. 2007;56:889–90.
Palová-Jelínková L, Dáňová K, Drašarová H, et al. Pepsin digest of wheat gliadin fraction increases production of IL-1β via TLR4/MyD88/TRIF/MAPK/NF-κB signaling pathway and an NLRP3 inflammasome activation. PLoS One. 2013;8:e62426.
Williams MJ. Drosophila hemopoiesis and cellular immunity. J Immunol. 2007;178:4711–6.
Wang Z, Wilhelmsson C, Hyrsl P, et al. Pathogen entrapment by transglutaminase – a conserved early innate immune mechanism. PLoS Pathog. 2010;6:e1000763.
Cho MY, Lee HS, Lee KM, Homma K, Natori S, Lee BL. Molecular cloning and functional properties of two early-stage encapsulation-relating proteins from the coleopteran insect, Tenebrio molitor larvae. Eur J Biochem. 1999;262:737–44.
Konarev AV, Beaudoin F, Marsh J, et al. Characterization of a glutenin-specific serine proteinase of Sunn bug Eurygaster integricepts put. J Agric Food Chem. 2011;59:2462–70.
Every D, Sutton KH, Shewry PR, Tatham AS, Coolbear T. Specificity of action of an insect proteinase purified from wheat grain infested by the New Zealand wheat bug, Nysius huttoni. J Cereal Sci. 2005;42:185–91.
Batt RM, Carter MW, McLean L. Morphological and biochemical studies of a naturally occurring enteropathy in the Irish setter dog: a comparison with coeliac disease in man. Res Vet Sci. 1984;37:339–46.
Author information
Authors and Affiliations
Corresponding author
Ethics declarations
Conflict of Interest
None.
Source of Funding
None.
Rights and permissions
About this article
Cite this article
Murch, S. Recent Advances in Celiac Disease. Indian J Pediatr 83, 1428–1435 (2016). https://doi.org/10.1007/s12098-016-2161-8
Received:
Accepted:
Published:
Issue Date:
DOI: https://doi.org/10.1007/s12098-016-2161-8