Abstract
Neonates truly constitute the foundation of a nation and no sensible government can afford to neglect their needs and rights. In the last 50 y, technology has revolutionized neonatology and we have moved from an exceedingly passive or “hands-off” philosophy to an extremely aggressive or mechanistic approach. Deaths during first 28 d of life account for over 60 % of all infant deaths and 40 % of all deaths of under-5 children. If we have to further reduce infant mortality rate in our country we must focus our strategies to improve health and survival of newborn babies. There should be equitable distribution of resources for the care of mothers and babies in the community and establishment of high-tech newborn care facilities. In 21st century, we must delink and sever our dependence on traditional birth attendants or dais and develop necessary infrastructure and facilities to ensure that every pregnant woman is provided with essential antenatal care and all deliveries take place at health care facilities and they are conducted by trained health care professionals. In the best pediatric tradition, there is a need for greater focus on preventive rather than curative health care strategies because a large number of neonatal deaths occur due to potentially preventable disorders like birth asphyxia, hypothermia, hypoglycemia and infections. The art and science of neonatology should be integrated and we should follow a “middle path” and strike a balance between art and technology in the care of newborns.
Similar content being viewed by others
Avoid common mistakes on your manuscript.
Introduction
“The seeds of neonatal morbidity and childhood disability are sown in the perinatal period.”
– Meharban Singh
Neonates truly constitute the foundation of human life. Just as children are not mini-adults, neonates are not mini-children. They have unique health issues and problems due to structural and functional immaturity of various body organs depending upon their gestational age and birth weight. Newborn period is the most vulnerable phase of life and deaths during first 28 d of life account for over 60 % of all infant deaths and 40 % of all deaths of under-5 children. Apart from high neonatal mortality rate of 32 per 1,000 live births in India, many avoidable handicaps during childhood such as cerebral palsy mental subnormality, learning disabilities and recurrent seizures have their origin in the perinatal period [1]. Disabilities cause tremendous stress and strain to the family and society especially when we lack resources, facilities and social support system to tackle them. Based on the “developmental origins of adult diseases” or “thrifty gene” hypothesis, there is evidence to suggest that infants with intrauterine growth restriction are at an increased risk to develop certain adult-onset diseases like hypertension, coronary artery disease, type 2 diabetes mellitus and hyperlipidemia [2]. The aim and goal of newborn care is not only to reduce neonatal mortality but more importantly to ensure their intact survival. It is futile to save babies if they become a liability rather than an asset to the society. The enhancement of neonatal and infant survival is truly the key to the success of family welfare program and stabilization of population dynamics.
Evolution of Neonatology
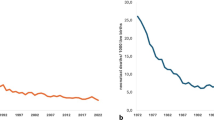
The concept and practice of neonatology evolved about 70 y ago and since then we have made outstanding advances in the care of newborn babies. It is amazing that a newborn baby with a birth weight of 1.0 kg had a mortality risk of 95 % in 1950 and now has a 95 % probability of survival. There have been four distinct phases in the development of neonatology. Neonatology has evolved from a state of passive or “hands-off years” (1920–1950) followed by aggressive or “heroic years” (1950–1970) and reached a phase of “experienced years” (1970–2000) by promotion of evidence-based newborn care practices [3]. Due to integration of science and art of newborn care, the practice of neonatology has now reached the “years of wisdom” (middle path concept) and focus has shifted from mere survival to “intact” survival.
Major advances in neonatology include effective resuscitation at birth, prevention of hypothermia and bacterial infections, rational use of antibiotics and promotion of optimal nutrition with human milk and parenteral nutrition. Availability of micro sampling of blood has ensured frequent monitoring and prompt correction of abnormalities in blood gases, acid–base parameters, electrolytes, glucose, bilirubin and other biochemical indices. It is possible to monitor vital signs and arterial oxygen saturation with the help of non-invasive technology. The outcome and survival of preterm babies has improved by use of antenatal corticosteroids, administration of synthetic or exogenous surfactant and respiratory support (CPAP and assisted ventilation). Pharmacological closure of ductus arteriosus, support of blood pressure, cot-side echocardiography and amplitude integrated EEG (aEEG), use of inhaled nitric oxide (iNO), interventional cardiology, newer modalities of assisted ventilation (PTV, SIMV and high frequency ventilation), and extracorporeal membrane oxygenation (ECMO) have revolutionized the cardiopulmonary management of critically sick neonates. Phototherapy has reduced the need for exchange blood transfusions and risk of bilirubin encephalopathy. A number of therapeutic misadventures (iatrogenic disorders) or disasters of our good intents like retinopathy of prematurity (ROP), kernicterus (sulfisoxazole prophylaxis, synthetic vitamin K, novobiocin), methemoglobinemia (diaper markings), hexachlarophene toxicity, “gray-baby” syndrome (chloramphenicol), pyloric stenosis (prokinetics like erythromycin), intraventricular hemorrhage (aggressive handling, bolus administration of sodium bicarbonate), cerebral palsy (corticosteroids), pulmonary air leaks and bronchopulmonary dysplasia (BPD) due to aggressive assisted ventilation can be prevented or recognized early and managed effectively [4]. It is important that we must exercise restraint and caution while introducing newer therapeutic interventions while keeping in mind their safety and cost-effectiveness.
Global Neonatal Health
Globally 3.07 million newborns die during first 28 d of life [5]. In addition, nearly 2.65 million still births occur every year [6] i.e., 11 lives are lost every minute. Most neonatal deaths occur during first week of life (75 %) and almost 25 % during first 24 h. The risk of mortality during neonatal period is 30-fold higher compared to the mortality during the post-neonatal period. About 96 % of neonatal deaths occur in developing countries. India has the dubious distinction of having highest number of annual neonatal births and deaths among all countries in the world. Every year about 27 million babies (20 % of global births) are born in India and about 1.0 million die during newborn period accounting for 30 % of global deaths. Neonatal deaths account for two-third of all infant deaths and 41 % deaths of under-5 children. The millennium development goal 4 (reducing under-5 mortality by two-third) cannot be achieved unless we ensure substantial reduction in neonatal mortality.
According to data published in Lancet 2010, WHO 2000 estimates, the main direct causes of neonatal deaths include bacterial infections (29 %), preterm births (29 %), birth asphyxia (23 %) and congenital malformations (8 %). The primary causes of global neonatal deaths are shown in Fig. 1 [7]. The common correlates of adverse neonatal outcome include poor health status of women, illiteracy, lack of empowerment, early marriages and frequent pregnancies. In developing countries, lack of resources, poor infrastructure, lack of antenatal care, deliveries by unskilled birth attendants or relatives and poor accessibility and credibility of the facility-based health care services are the leading causes of dismal situation of newborn health [8].
Maternal Health and Newborn Survival
“The health and well-being of fetus is dependent upon the health and nutrition of the mother (not the father!) because she is both the seed as well as the soil where in the baby is nurtured for 9 mo.”
– Meharban Singh
Mothers are the creators and sustainers of progeny. The health and well being of children is intimately linked with the health, nutrition, education and status of their mothers. Healthy and well informed mothers are likely to produce healthy and normal weight babies while undernourished and high-risk mothers are likely to produce high-risk and preterm or low birth weight babies. Healthy mothers are in a much better position to look after the health and well-being of their children. Mother is the best primary health worker because of her strong motivation, concern and commitment. She must be provided with information, knowledge and skills on mother-craft to handle her baby with ease and confidence [9].
Over one-third of women in India are undernourished with a body weight of less than 40 kg or height of less than 145 cm. They are prone to develop a variety of infections, genital colonization, bacterial vaginosis with high prevalence of pelvic inflammatory disease (PID) and unsatisfactory reproductive health. Almost one-half of women in India are illiterate; they lack personal and financial independence and empowerment. The situation is further complicated by early marriages, teenage and frequent pregnancies. No wonder every fourth baby is a low birth weight (LBW) baby in our country.
Focus on Girl Children
“The prevailing sense of despair and despondency at the birth of a female child should be replaced by the awareness and hope that she is the creator and sustainer of progeny.”
– Meharban Singh
There is a need to provide equal status and opportunities to girl children so that they grow to become healthy, literate, empowered and economically independent women to look after their own health and well-being of their children. The concept of gender equality means that boys and girls should have equal access to food, health care, education and opportunities in life. Adolescent boys and girls should be provided with family life education and mother-craft skills in various CBSE and NCERT schools. A “life-cycle” approach should be followed to provide optimal nutrition and health care during infancy, childhood, adolescence, pregnancy and lactation. Women should have dignity, status and say in society in order to improve the health indices of children as has been achieved in Kerala, Goa and some North-Eastern states of India.
The girls should undergo pre-marital health check-up to ensure that they are healthy and well nourished before they enter their reproductive life. Child marriages and teenage pregnancies must be curbed. The ideal age of women for reproduction is between 25 and 35 y. The marriages among first degree relatives and carrier couples should be avoided to reduce the risk of genetic disorders. Complete physical examination should be done to identify and treat any systemic disorder. Ensure adequacy of hemoglobin and nutritional status by intake of healthy diet and supplements of iron, folic acid, calcium and vitamin D during adolescence. It is important that nutritional deficits are corrected during adolescence and not delayed till early pregnancy. Girls must be effectively immunized against rubella and tetanus before they are married. Women must avoid smoking, chewing tobacco and substance abuse due to risk of adverse effects on their offsprings.
Myths and Misconceptions Regarding Newborn Care
There are a number of myths and misconceptions which can discourage health care professionals in initiating effective interventions to improve newborn survival [10].
-
1.
Newborn mortality can be reduced only by developed countries with high gross domestic product (GDP).
Several countries with a low GDP like Sri Lanka, Indonesia, Vietnam, Cuba, Honduras, Nicargua etc. have reduced neonatal mortality rates (NMR).
-
2.
High-tech interventions are needed to improve newborn survival
Many countries have reduced NMR to about 15 per 1,000 live births with community-based interventions without the use of complex technology. There are minimum technology needs to provide essential care to newborns in the community (Table 1).
Table 1 The technology needs for care of newborns in the community -
3.
Newborn care is expensive and not cost-effective
Several low-cost interventions are effective to reduce neonatal mortality like health care of girl children, nutritional supplements to adolescent girls, administration of tetanus toxoid to pregnant women, exclusive breast feeding, kangaroo mother care for LBW babies, prevention and early use of antibiotics for treatment of bacterial infections.
-
4.
Newborn health is not a priority in a developing country because high neonatal mortality is a blessing in disguise to control population dynamics.
Newborn survival is indeed the greatest assurance and incentive to parents to adopt family planning measures and achieve population goals.
-
5.
The ongoing child survival and safe motherhood (CSSM) and reproductive and child health (RCH) programs are sufficient to reduce deaths of newborns.
Till recently, CSSM and RCH programs in India focused on reduction of post-neonatal deaths by promotion of breast feeding, immunizations, oral rehydration solution (ORS) for treatment of diarrhea and early administration of antibiotics for treatment of acute respiratory tract infections. The need for specific neonatal interventions is now being addressed in India by launching essential newborn care in the community (Bang’s model) with the help of accredited social health activists (ASHAs) and introduction of integrated management of neonatal and childhood illnesses (IMNCI) programs so that common newborn diseases are tackled through simple algorithms [11]. We should create a network of good quality level II newborn care units throughout the country which are more cost-effective and less technology or labor-intensive and can bring down the neonatal mortality rate to less than 20 per 1,000 live births.
Essential Newborn Care
There should be equitable distribution of resources for care of mothers and babies in the community and establishment of high-tech newborn care facilities by creation of a network of special care and intensive care neonatal units in a phased manner. The components of essential newborn care services include good quality antenatal care (at least 4 ANC contacts), safe delivery and optimal care at birth, prevention and early treatment of hypothermia and bacterial infections, and promotion of exclusive breast feeding. The delivery should be conducted by a skilled health worker in a nearby health care facility or hospital. The moderate sized low birth weight babies (birth weight >1,800 g and/or gestation >34 wk) account for 90 % of LBW babies and they should be provided essential newborn care at home or primary health care facility. Kangaroo mother care has been shown to reduce the risk of nosocomial infections and hypothermia with improved survival of LBW babies. It is credited to enhance mother-infant bonding, improve weight gain velocity and shorten the duration of hospital stay [12]. . There is a need for greater focus on the preventive rather than curative strategies because a large number of neonatal deaths occur due to potentially preventable disorders like birth asphyxia, hypothermia, hypoglycemia and septicemia. Essential newborn care should be provided to all deliveries taking place at home, subcenter or primary health center as a national priority in order to further reduce infant mortality rate.
The Art of Neonatology
The technology has revolutionized the practice of neonatology and we have moved from an exceedingly “passive” or gentle “hands-off” approach to an over enthusiastic technology-oriented “aggressive” or “robotic” approach. It is a sad reality that nobody knows the ultimate or absolute truth. Science only provides a tentative or partial truth or truth for the time being. Neonatology is dynamic and we are likely to find new facts and new data in due course of time. Therefore, we should not be dogmatic and we must work with humility, common sense and compassion. We should exercise restraint with a check and balance on the pace of change to ensure that knowledge is transformed into wisdom and it should be effectively harnessed keeping in mind the existent social constraints and realities. We should not merely try to satisfy our ego by using aggressive measures to save “previable premies” but our aim should be to ensure “intact” survival so that every neonate grows to become an asset to the nation rather than a liability to the society.
The art and science of neonatal care should be integrated to provide holistic care to preterm babies. Babies should not be handled as “objects” and should be provided with humanized developmentally supportive care [13, 14]. The nurses should be trained to provide individualized developmentally supportive care to preterm babies by adopting a “flexible” approach. They should feel connected and tuned with babies under their care. All the health care professionals in the neonatal intensive care unit (NICU) should be gentle, considerate and compassionate in providing care to preterm babies. The nature is supreme the way it look after all the needs of the baby in the womb. The baby is gently rocked in the warm amniotic fluid and is well protected from infections and effectively shielded against light and sound. The baby is comfortably “nested” in a flexed posture with hands in the midline in front of the face. The uterine blood flow provides a soothing music skin to a waterfall while maternal heart beats provide him constant soothing tick-tacks like a cuckoo clock. The physiological needs of oxygenation, nutrition and excretion are admirably met by the utero-placental unit. We should try to create a baby-friendly womb-like ambience and ecology in the NICU to simulate in-utero environment (Table 2). Despite several attempts, scientists have failed to fabricate an incubator with all the qualities and characteristics of the womb.
Clinical Assessment
The health problems of newborn babies are unique and distinctive compared to diseases of infants and children. Neonates are prone to develop health problems due to transition from dependent fetal life to independent neonatal physiology. A large number of disorders occur due to structural and functional immaturity of various body organs, developmental defects and a variety of iatrogenic disorders due to aggressive use of technology in the NICU. Most problems of healthy term neonates are minor, physiological or developmental and without any clinical significance. But when a newborn baby is genuinely sick, he is likely to be very sick and cannot be managed on an ambulatory basis. The newborn baby has a limited capacity to express specific clinical manifestations of a disease process. Neonates are likely to manifest with an identical non-specific stereotyped responses to a variety of diseases. Therefore, the diagnosis of a neonatal disorder is based more on the nature of predisposing and associated conditions and antecedent events rather than the clinical manifestations of the underlying disease process.
The assessment of a preterm baby in the NICU can be simplified into a simple non-invasive protocol of just see, touch the baby and ask the nurse. There is no need for any detailed systemic examination which may be traumatic to the baby and has a poor yield. The characteristics of a healthy stable preterm baby are listed in Table 3.
Harness the Caring Cues from Nature
Nature has profound biological wisdom. We cannot go wrong when we do what nature does. When a mammal delivers the baby, the parturient mother gnaws the umbilical cord only when pulsations have stopped. We should not be in a hurry to ligate the “life-line” because delayed clamping of the cord is associated with smoother extrauterine transition, reduced risk of anemia due to materno-fetal transfusion and necrotizing enterocolitis [15]. It is recommended that the obstetrician should follow a relaxed approach in clamping the cord, neither immediate nor deliberate delay should be adopted. In high-risk situations like cord around the neck, fetal hypoxia and Rh-isoimmunization, it is desirable to ensure early clamping of the cord. No one cleans or sucks the oral cavity of young ones of animals. There is no need to do oro-pharyngeal suction in a crying infant and baby’s nose and mouth can be wiped with a gauze piece. We have all wondered why practically every baby is jaundiced during first week of life. Bilirubin is a potent antioxidant and it seems it provides protection to the neonates against oxygen free radicals which is a recognized pathogenetic mechanism in the causation of a variety of neonatal disorders. The nature has so designed that when a baby is born, a readymade drink flows out as a divine nectar. Breast milk of different animals is not only species specific, it is indeed baby specific. The milk of a mother is most suitable to serve the nutritional and biological needs of her baby. The milk of mothers delivering prematurely provides a higher concentration of fat, protein, sodium and secretory IgA which are required for rapid growth of preterm babies. Breast milk of a healthy mother is a complete nutritional drink for her healthy baby except that it has relatively low levels of vitamin K and vitamin D which are provided as supplements. Animals keep their young ones warm by close skin-to-skin contact and we should emulate by providing kangaroo mother care [16]. We must create womb-like ambience in the incubator to harness all the virtues of the womb which nature is able to provide with great precision.
Provide Evidence-Based Newborn Care
Evidence-based neonatal care or Cochrane data base is probably closest to truth but it must be integrated with personal experience or expertise, and common sense to transform these recommendations into cost-effective best newborn care practices in order to harness best dividends. The National Neonatology Forum of India has done a commendable job to bring out a publication on evidence-based newborn care practices. There are a large number of interventions which must be avoided in the care of preterm babies due to their potential hazards leading to increased morbidity due to iatrogenic disorders (Table 4). Asepsis protocols and hand washing are far more important than prophylactic administration of antibiotics or intravenous immunoglobulins which are potentially dangerous.
Ethical Issues and Concerns
“No other gift is greater than the gift of life. The patient may doubt his relatives, his sons and even his parents, but he has full faith in his physician. He gives himself up in the doctor’s hand and has no misgivings about him. Therefore, it is the physician’s duty to look after him as his own .....”
– Charaka
There is an age old trust and respect towards physicians in Indian culture. To maintain this trust and faith, which is essential to augment the process of healing, it is incumbent on physicians to be ethical, honest and uptodate in their knowledge and skills. Ethical decisions are based on the five principles of beneficence, non-maleficence, parental autonomy, correct medical facts and social justice. Hippocrates epitomized the principle of non-maleficence by advocating primum non nocere (do no harm). The ethical decisions should be taken jointly after undertaking discussions with the concerned consultants and nurses, and by taking parents into confidence. A large number of issues are taken into consideration while handling ethical dilemmas [17]. Is there any reasonable chance of survival of the infant with available technology? Would the quality of life be worth living if the neonate survives with aggressive management? Can the family afford expensive treatment? Should we be concerned with the best interests of the infant alone or global interests of the family, society and state? Should a “brain dead” pregnant woman be maintained on the life support system for the sake of her unborn baby? In view of our limited resources, should a poor risk extremely low birth weight baby be hooked off the ventilator to provide assisted ventilation to a more salvageable bigger baby? Should a non-salvageable infant with a lethal congenital malformation provided with assisted life support? Moreover, there are several cultural considerations, the fertility of the couple, gender of the infant, the concept of destiny or will of God, the doctor-knows-best-attitude, socio-economic status, education of parents, social support and national priorities. It is unfortunate but true that in a developing country, financial and social realities may outweigh and override ethical considerations.
There are a large number of ethical issues and dilemmas in the care of newborn babies. According to the provisions of the Medical Termination of Pregnancy (MTP) Act, pregnancy of less than 20 wk can be aborted on medical or family welfare grounds. However, when duration of pregnancy is more than 20 wk, the physician has the right to ‘terminate’ it in order to save the life of mother, but abortion is not permitted on fetal grounds. However, it is morally justified though illegal to abort a malformed fetus after 20 wk if two conditions are fulfilled, (i) fetus is afflicted with a lethal congenital malformation and (ii) prenatal diagnosis of the fetal condition can be made with a high degree of reliability. In an infant who is inevitably destined to die, or likely to survive with a profound risk of severe neuromotor disability, “selective non-treatment” is ethically and morally acceptable. The same reasons that justify withholding of treatment are also valid for withdrawal of life support [18]. These conditions include extremely preterm baby, grade 4 intraventricular hemorrhage, lethal CNS malformations, severe birth asphyxia with lack of spontaneous breathing efforts for more than 30 min or HIE Sarnat stage 4, brain death, and persistent vegetative state. Every NICU should clearly define its policies for selective non-treatment, denial of life-support interventions and withdrawal of life-support to ensure uniformity of approach and as a legal safeguard. Other ethical issues and dilemmas pertain to assisted reproductive techniques, surrogacy, genetic engineering, organ transplantation, perinatal human immunodeficiency virus (HIV) infection, and end-of-life decisions etc. In developed countries where medical care is supported by social security system or health insurance companies, parents demand intensive care with all the conceivable life support measures even when treating health team feels that it is futile to treat. On the other hand, in developing countries, many a times treatable conditions and salvageable babies are denied life sustaining therapies either due to non availability of technology or because of non-affordability by the parents. We should evolve a rational process and sound mechanism to make correct ethical decisions. Bioethics Committees and Grievance Redress Cells should be constituted in all hospitals who should serve as a watch dog to monitor and maintain the sanctity of all ethical decisions.
Future Developments and Perspectives
A large number of newer interventions are in the pipeline to further revolutionize the practice of neonatology. A number of multicentric randomized controlled trials (RCTs) have been launched to identify evidence-based, reliable, and safe newborn care practices. Skin surface electrodes are being developed for non-invasive monitoring of blood gases, glucose, bilirubin, electrolytes, pH etc. There is a need to develop ultra micro techniques for assessment of complete biochemical parameters with the help of a drop of blood. Newer diagnostic techniques with the help of polymerase chain reaction (PCR) are being developed for the diagnosis of a variety of infective and genetic disorders. Neonatal screening for inborn errors of metabolism is likely to become universal. Efforts are being made to develop specific monoclonal antibodies for prevention and treatment of life-threatening infective disorders. Vaccines are being developed for prevention of Group B streptococci (GBS), cytomegalovirus (CMV) and human immunodeficiency virus (HIV) infections. Tailor-made drugs are being formulated with the help of pharmacogenetics and attempts are made to deliver the drugs to the site of disease with the help of liposomes. There is increasing use of homologous blood obtained from placenta and possibility of developing a synthetic blood substitute. The possibility of storing cord blood has become a reality for future use as “totipotent” stem cells for repair of any organ and treatment of malignant or genetic disorders in the donor, siblings or parents. Genetic engineering is being exploited to replace a “bad” gene with a “good” gene by tagging it to the carrier viruses. Assisted reproductive technologies (ARTs) are being harnessed to produce genetically normal babies, flawless designer babies and gender selection raising several moral and ethical issues. There is a need to develop strategies to prevent premature birth of babies who are structurally normal. Prolongation of gestation and improvement of fetal nutrition are important interventions to improve birth weight which is the single most important correlate of improved survival and outcome of a neonate. However, the ultimate dream of a neonatologist, which has defied all attempts till date, is to create a prototype of a utero-placental unit to provide all virtues of the womb to nurture babies who are born prematurely.
Epilogue
Neonatology is the first subspecialty of pediatrics which has been developed and actively pursued in India. It has gradually come off age and is currently at the threshold of its “adolescent growth spurt”. It has given an identity and status to the pediatricians by virtue of use of high profile technology in the NICU. However, the art and science of neonatology must be integrated and we should follow a “middle path” in the care of newborn babies. We should avoid both extremely “passive” as well as blatantly aggressive or “robotic” approach. In the best pediatric tradition, our approach in perinatal medicine should be oriented towards prevention, early diagnosis and prompt management of common neonatal disorders. Technology should not be allowed to further dehumanize neonatology. The narrow focus on high-tech medical rescues in NICUs should give way to compassionate acts of social interventions for global benefits for all rather than narrow gains for a few. We must treat babies not only with our heads but also with our hearts. It is important to remember that brain is business like but heart is holistic and it has the same root as harmony, healing and health. All efforts should be made to enhance the survival of preterm and sick babies but our goal should be to improve the quality of life among those who survive. It is desirable that every newborn unit must have an integrated follow-up program to assess the quality of life of their NICU graduates and provide them with early stimulation.
References
Singh M. Introduction to the care of newborns. In: Singh M, ed. A Manual of Essential Pediatrics. 2nd ed. Noida: Thieme Medical and Scientific Publishers, Pvt. Ltd; 2013. pp. 129–37.
De Boo HA, Harding JE. The developmental origin of adult disease (Barker) hypothesis. Aust N Z J Obstet Gynaecol. 2006;46:4–14.
Philip AGS. The evolution of neonatology. Pediatr Res. 2005;58:799–815.
Robertson AF. Reflections on errors in neonatology: I. The “Hands-Off” years, 1920 to 1950. J Perinatol. 2003;23:48–55.
Liu L, Johnson HL, Cousens S, Perin J, Scott S, Lawn JE, et al; Child Health Epidemiology Reference Group of WHO and UNICEF. Global, regional, and national causes of child mortality: An updated systematic analysis for 2010 with time trends since 2000. Lancet. 2012;379:2151–61.
Lawn JE, Blencowe H, Pattinson R, Cousens S, Kumar R, Ibiebele I, et al; Lancet's Stillbirths Series Stecring Committee. Stillbirths: Where? When? Why? How to make the data count? Lancet. 2011;377:1448–63.
Lawn JE, Kerber K, Enweronu-Laryea C, Cousens S. 3.6 million neonatal deaths—what is progressing and what is not? Semin Perinatol. 2010;34:371–86.
Singh M. Perinatal services in India: current status and future perspectives. Natl Med J India. 2003;16:S1–4.
Singh M. Medical Quotations by Eminent Physicians and Philosophers. 3rd ed. New Delhi: Sagar Publications; 2013.
Singh M. Myths and misconceptions regarding newborn care. In: Singh M, ed. Care of the Newborn. 7th ed. New Delhi: Sagar Publications; 2010. pp. 2–3.
Bang AT, Bang RA, Baitule SB, Reddy MH, Deshmukh MD. Effect of home-based neonatal care and management of sepsis on neonatal mortality: field trial in rural India. Lancet. 1999;354:1955–61.
Conde-Agudelo A, Belizan JM, Diaz-Rossello J. Kangaroo mother care to reduce morbidity and mortality in low birth weight infants. Cochrane Database Syst Rev. 2011;3: CD002771.
Singh M, Deorari AK. Humanized care of preterm babies. Indian Pediatr. 2003;40:13–20.
Fleisher BE, Vandenberg K, Constantinou J, Heller C, Benitz WE, Johnson A, et al. Individualized developmental care for very low birth weight premature infants. Clin Pediatr (Phila). 1995;34:523–9.
Rabe H, Diaz-Rossello JL, Duley L, Dowswell T. Effect of timing of umbilical cord clamping and other strategies to influence placental transfusion at preterm birth on maternal and infant outcomes. Cochrane Database Syst Rev. 2012;8: CD003248.
Simkiss DE. Kangaroo mother care (Editorial). J Trop Pediatr. 1999;45:192–4.
Singh M. Ethical issues and dilemmas in the care of newborn babies in the developing world. Semin Neonatol. 1999;4:151–7.
American Academy of Pediatrics Committee on the Fetus and Newborn, Bell EF. Noninitiation or withdrawal of intensive care for high-risk newborns. Pediatrics. 2007;119:401–3.
Contribution
Dr. Meharban Singh will act as guarantor for this paper.
Conflict of Interest
None.
Role of Funding Source
None.
Author information
Authors and Affiliations
Corresponding author
Rights and permissions
About this article
Cite this article
Singh, M. The Art, Science and Philosophy of Newborn Care. Indian J Pediatr 81, 552–559 (2014). https://doi.org/10.1007/s12098-014-1359-x
Received:
Accepted:
Published:
Issue Date:
DOI: https://doi.org/10.1007/s12098-014-1359-x