Abstract
Purpose
The optimal drug regimen and sequence are still unknown for patients with metastatic colorectal cancer (mCRC) who are candidates for third-line (3L) or subsequent treatment. The aim of this study is to know the opinion of experts on the most appropriate treatment options for mCRC in 3L and to clarify certain clinical decisions in Spain.
Methods
Using a modified Delphi method, a group of experts discussed the treatment in 3L of patients with mCRC and developed a questionnaire with 21 items divided into 5 sections.
Results
After 2 rounds, the 67 panelists consulted agreed on 17 items (81%). They considered that the main objective of 3L is to equally increase survival and improve patients’ quality of life (QoL), but preferably the QoL. It was agreed that patients with mCRC in 3L prefer to receive active versus symptomatic treatment. Panelists considered trifluridine/tipiracil (FTD/TPI) to be the best oral treatment available to them in 3L. In patients with MSI-H or dMMR and BRAF V600E, the panelists mostly prefer targeted treatments. Panelists agreed the use of a therapeutic sequence that not only increases outcomes but also allows patients to be treated later. Finally, it was agreed that FTD/TPI has a mechanism of action that allows it to be used in patients refractory to previous treatment with 5-fluorouracil.
Conclusion
The experts agreed with most of the proposed items on 3L treatment of mCRC, prioritizing therapeutic options that increase survival and preserve QoL, while facilitating the possibility that patients can continue to be treated later.
Similar content being viewed by others
Avoid common mistakes on your manuscript.
Introduction
Colorectal cancer (CRC) is a public health problem. It is the third most common cancer in men and the second in women and represents the second leading cause of death by cancer worldwide [1]. In Spain, CRC represents the second most common tumor in both genders [2]. It is believed that in the next 30 years, the mortality rate for colon cancer will be reduced, but there will be an increase for rectal cancer [3].
Standard first- and second-line treatments are based on combinations of fluoropyrimidine plus oxaliplatin or irinotecan, associated with an anti-angiogenic monoclonal antibody or anti-epidermal growth factor receptor (EGFR), which is chosen based on the RAS mutational status, although the optimal sequence is still unknown [4, 5]. Although the prognosis for metastatic CRC (mCRC) is poor, these treatments have led to an increase in the survival of patients, reaching a median of 25 to 30 months [4, 5]. Nevertheless, there is a growing number of patients with mCRC being candidates for a third line (3L) or beyond, although the optimal drug regimen and sequence are still unknown in this setting.
Only the presence of RAS-activating mutations (KRAS/NRAS), present in 30% to 45% of mCRC, has proven to be a negative predictive biomarker of response to anti-EGFR [6]. Although no other validated predictive biomarkers have been described, there are other biomarkers of special interest, such as BRAF mutation (present in 8% to 10% of mCRC), human epidermal growth factor receptor 2 (HER2) amplification, high microsatellite instability (MSI-H), and ALK/ROS1/NTRK fusion/rearrangements (occur in 0.2–2.4% of mCRC) [7,8,9,10,11].
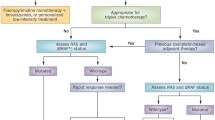
Taking in mind these biomarkers, several alternatives have been proposed in the 3L for patients who have not responded or are refractory to the previous lines: (1) sequential administration of the two oral drugs approved in this indication, trifluridine/tipiracil and regorafenib, which have shown a statistically significant benefit in progression-free survival (PFS) and overall survival (OS) with a different toxicity profile both in clinical trials and in real-life studies [12, 13]; (2) administration of an anti-EGFR, such as cetuximab or panitumumab, in treatment-naive patients with RAS wild type, which is increasingly rare because these drugs are usually indicated in first or second line [14]; (3) reuse drugs already administered that were discontinued owing to toxicity or progression (oxaliplatin, irinotecan, fluoropyrimidine, anti-angiogenics, and anti-EGFR [if RAS wild type]). In this case, high-quality evidence is limited, but this strategy is often used in routine clinical practice in the absence of alternative therapies, especially in patients with good performance status [15, 16]; (4) specific treatments for selected populations, such as dual inhibition of HER2 in HER2-positive CRC (i.e., tucatinib plus trastuzumab), immunotherapy in MSI-H, and intrahepatic therapies in limited disease or primarily located in the liver, although the main recommendation is to include patients in clinical trials [17].
Although there are different therapeutic options for the 3L treatment of mCRC, the optimal sequence of these therapies and the management of these patients in 3L are unknown. For this reason, the aim of this work is to develop a consensus to know the opinion of a panel of Spanish experts on the management of patients with mCRC in the 3L and to clarify certain points regarding clinical decisions in this setting.
Methods
Study design
The study used a modified Delphi method, a structured communication technique that allows a group of experts to gather opinions on a given complex or controversial topic for which there is insufficient evidence, or their knowledge is incomplete or uncertain [18, 19]. In addition, it allows the opinions of a group of experts to be explored and unified without the difficulties and inconveniences inherent to consensus methods based on face-to-face discussions, such as displacements or the biases of influence or non-confidential interaction.
The study was performed in three distinct phases from July 2021 to July 2022: (a) meeting of the scientific committee to raise the problem to be addressed and draft a statement list (July 2021); (b) two successive rounds of online surveys to obtain the opinion of a panel of experts about the items of the statement list (February–July 2022); and (c) analysis and discussion of the results to draw conclusion (July 2022).
Participants
Three groups participated in the study: a scientific committee, a technical team, and a panel of experts. The scientific committee consisted of five oncologists involved in the treatment of patients with mCRC and provide care in public and private hospitals in Spain, whose role was to review the literature and draft a questionnaire with items regarding the treatment of mCRC in the 3L. The technical team, which directed and supervised the entire process, was responsible for the instrumental implementation of the method (search of the literature, distribution of the questionnaire to the panelists, analysis of the responses, and statistical interpretation of the consensus). Finally, the scientific committee chose the panel of experts, selected according to the type of center in which they work, their clinical experience, their experience in the management of patients with mCRC, their experience in the use of treatments for the disease, and according to the geographic region to which they belong, trying to achieve the maximum representation of all of Spain.
Delphi questionnaire
Based on the discussions of the scientific committee, and according to the evidence found on the topic, the scientific committee developed a Delphi questionnaire consisting of 21 items grouped in 5 sections that included the most relevant controversies on the treatment of mCRC in the 3L: (1) 3L objectives (three items); (2) treatment options in 3L (seven items); (3) subgroup of patients (five items); (4) therapeutic sequences (four items); and (5) conditions of use of trifluridine/tipiracil (three items).
For the evaluation of the questionnaire, a single nine-point Likert-type ordinal scale was proposed, according to the model developed by the UCLA-RAND Corporation for the comparative evaluation and prioritization between different health-care options (minimum 1, complete disagreement; and maximum 9, complete agreement) [19]. This scale was structured in three groups according to the level of agreement–disagreement of the statement: from 1 to 3, interpreted as rejection or disagreement; from 4 to 6, interpreted as no agreement or disagreement; and from 7 to 9, interpreted as expression of agreement or support.
Phases of Delphi consensus
Following the Delphi methodology procedure [20], the questionnaire was sent to the panel of experts to respond by showing their degree of agreement with the items. In the first round, the panelists responded to the questionnaire online and were offered the possibility of adding their opinion as an open text. The technical team evaluated and presented the results of the first round using bar graphs to facilitate comments and clarifications from each participant. In the second round, the panelists contrasted their personal opinion with that of the other participants and, if necessary, reconsidered their initial opinion on those items where consensus was not reached. The results of this second round were tabulated and presented descriptively. In a final meeting, the scientific committee discussed and interpreted the results.
Analysis and interpretation of results
The median and interquartile range of the scores obtained for each item were used to analyze the data for both rounds. There was consensus when two-thirds or more of the respondents (≥ 66.7%) scored within the three-point range (1–3 or 7–9) that contained the median. The type of consensus reached on each item was determined by the score median. There was agreement if the median was ≥ 7 and there was disagreement if the median was ≤ 3. No consensus was considered when one-third or more of the panelists (≥ 33.3%) scored in the range of 1–3 and another third or more in the range of 7–9. When the median score fell between the range of 4 and 6, the items were considered uncertain to a representative majority of the group.
The size of the expert panel was determined as follows: with a minimum sample size of 50 experts, a 14% marginal error is obtained, for a confidence level of 95% and a heterogeneity of 50% in the sub-analyses by specialty. A total of 67 experts in the treatment of patients with mCRC were finally selected.
Results
The 67 experts consulted completed the 2 rounds of the Delphi consensus. Of the 21 items proposed in the first round, consensus was reached on 16 (76%), all of them in agreement. The five non-consensus items were sent to the panelists to be assessed in a second round. Of these, consensus was reached only in one item (in agreement) and four did not reach consensus. After the 2 rounds, with a total of 21 items, 17 reached consensus in agreement (81%) and 4 did not reach consensus (19%) (Fig. 1). Table 1 shows in detail the degree of agreement reached with each item after the two rounds.
Third-line objectives
Of the three items proposed, only one remained without consensus. Panelists agreed in the first round that the objective of 3L is to equally increase survival and improve the quality of life of patients (75% of agreement). In the second round, panelists agreed that although the objective of 3L is to equally increase survival and improve patients’ quality of life, patients’ quality of life is prioritized over survival (70%). The panelists differed on prioritizing survival over quality of life, and then the item did not reach consensus.
Treatment options in third line
Of the seven items proposed, five reached consensus in agreement in the first round. The item with the highest degree of consensus stated that “patients with mCRC in third-line mostly prefer to receive active treatment rather than only symptomatic treatment” (97% of agreement). Other item with a high degree of agreement said that “clinical trials are one of the options for patients with mCRC in third-line if they meet the inclusion criteria” (94%). In addition, panelists agreed that “among the oral treatments available in third-line, trifluridine/tipiracil is the drug that best combines, overall in most patients, an increase in survival, a manageable safety profile, and maintenance of functional status” (90%).
The two items that remained without consensus stated that “regorafenib is effective and safe in most patients with mCRC in third-line”, and that “maintenance of the anti-angiogenic agent in third-line could benefit chemotherapy”.
Subgroup of patients
The four items proposed were agreed with a high degree of consensus in the first round. One of them said that, “if available, administration of cetuximab in second- or third-line together with encorafenib may be an option in patients with mCRC and BRAF V600E mutation” (97% agreement). Another of the agreed items stated that “based on clinical experience in RAS/BRAF wild-type mCRC, retreatment (rechallenge) with anti-EGFR is an option to be assessed for patients who have PFS ≥ 4–6 months to anti-EGFR in first-line, an anti-EGFR-free treatment interval of at least 4 months, and remain wild-type after liquid biopsy” (88%).
Therapeutic sequences
The four proposed items reached consensus in the agreement in the first round. The item with the highest degree of agreement stated that “when establishing a therapeutic sequence beyond second-line, an option must be used that increases survival with good tolerance and ideally allows the patient to continue to be treated thereafter” (94% agreement). Other items said that “trifluridine/tipiracil used in third-line preserves the functional status in a high percentage of patients and therefore allows patients to be treated with other alternative therapies if necessary” (91%).
Conditions of use of trifluridine/tipiracil
Of the three items proposed, only one item did not reach consensus. This item stated that, “in addition to dose reduction and other modifications of trifluridine–tipiracil therapy according to the degrees of neutropenia described in the data sheet, I use G-CSF sometimes in case of neutropenia”. The item with the highest degree of agreement (reached in the first round) stated that “the mechanism of action of trifluridine/tipiracil, which is different from that of conventional fluoropyrimidines, provides evidence for its use in patients refractory to previous lines of 5-fluorouracil or who cannot receive it” (90% agreement).
Discussion
Although the optimal pharmacologic regimen and sequence for patients with mCRC who are candidates for 3L or subsequent treatment are still unknown, the experts consulted showed a high degree of agreement with the proposed items (81%). However, there was no clearly defined position on 19% of the items, indicating there was no consensus. This shows that in certain specific cases of mCRC management in the 3L, the opinions and criteria of the experts on the same issues differ considerably.
Most of the panelists considered that the main objective of third-line is to equally increase survival and improve patients’ quality of life, but preferably the quality of life. Currently, all lines of treatment are required to increase overall survival, but prioritizing patient’s quality of life. Panelists argued that it would be equally valid to increase survival even at the cost of an “acceptable” deterioration in quality of life.
Regarding treatment options in the 3L, the option most agreed by the panelists was that patients preferred active treatment over symptomatic treatment. Although they considered trifluridine/tipiracil to be the best oral treatment available to patients with mCRC in 3L, there was no consensus on regorafenib. The panelists argued that although there is a group of patients who could benefit from regorafenib, this drug has adverse events that often require dose adjustments [21]. In relation to the maintenance of anti-angiogenics in 3L to improve chemotherapy, despite being feasible due to their mechanism of action, the panelists considered that more clinical evidence is still needed [15]. Even some commented that it is not necessary to continue using the anti-angiogenic drug when there are alternatives such as regorafenib. At the time of this Delphi consensus, the SUNLIGHT study had not been published and was, therefore, not part of the questionnaire. The results of this study support that trifluridine/tipiracil plus bevacizumab may represent a new standard of care for the treatment of patients with refractory mCRC who have progressed after two lines of therapy [22]. Even more, the ESMO living guidelines for mCRC include this therapeutic combination for the 3L and beyond [23]. However, even if the study and ESMO recommendations had been published prior to our Delphi consensus, this combination still does not have a reimbursement price in Spain and cannot be used, so health-care professionals would continue to administer the 3L with the available options, options that would remain valid for those who are not candidates for trifluridine/tipiracil plus bevacizumab combination therapy.
In a specific group of patients, panelists mostly prefer targeted treatments, such as cetuximab together with encorafenib in patients with BRAF V600E, and immunotherapy in patients with MSI-H or dMMR. Clinical evidence with these therapeutic strategies seems to be valid to the experts [14, 24,25,26,27]. Even so, they also consider that trifluridine/tipiracil offers better outcomes in patients with ECOG PS 0–1, one or two metastatic sites, time from first metastasis ≥ 18 months, and those without liver metastases. In addition, they considered the option of rechallenge with anti-EGFR in patients with RAS/BRAF wild-type mCRC, PFS ≥ 4–6 months to this therapy in first line, with an anti-EGFR-free interval of at least 4 months, and remain wild type after liquid biopsy [28].
Panelists agreed the use of a therapeutic sequence that not only increases outcomes but also allows patients to be treated later. However, it is interesting to note one of the most widely agreed items, the use of as many lines as possible to improve patient survival [29].
It has been described that the mechanism of action of trifluridine/tipiracil is different from that of the other fluoropyrimidine. This allows this drug to be used in those patients refractory to previous treatment with 5-fluorouracil or in whom this treatment cannot be administered [30, 31]. Panelists agreed with this information. Despite the scarce evidence (LONGBOARD trial, Clinicaltrials.gov ID: NCT04166604), opinions on the use of G-CSF after trifluridine/tipiracil administration are noteworthy. Some panelists commented that although there is no study to support it, the use of G-CSF is common due to the experience acquired with other chemotherapies, to avoid delays and to obtain the maximum benefit from the molecule. Other panelists explained that neutropenia caused by trifluridine/tipiracil is not severe and can be managed with delay in treatment by maintaining the dose without the need to use G-CSF.
Despite the benefits of this methodology, this work has some limitations. The selection of panelists was neither systematic nor randomized; recruitment was based on their clinical expertise in mCRC management. Panelists were recruited from different Spanish regions, although not all regions were represented. Finally, the results may have been influenced by ambiguity in the phrasing of some of the statements. In addition, panelists received honoraria from the sponsor. The fact that the survey was online had the advantage of anonymity, but it could lead to erroneous interpretations of the statements by the panelists, which could influence the result.
Conclusion
This Delphi consensus is of particular relevance and highlights expert opinions on the treatment of patients with mCRC in 3L. The experts agreed with most of the proposed items on 3L treatment of mCRC, prioritizing therapeutic options that increase survival and preserve quality of life, while facilitating the possibility that patients can continue to be treated later. The lack of consensus observed in some items suggests the need to improve knowledge about them.
Data availability statement
Not applicable.
References
Sung H, Ferlay J, Siegel RL, Laversanne M, Soerjomataram I, Jemal A, et al. Global Cancer Statistics 2020: GLOBOCAN estimates of incidence and mortality worldwide for 36 cancers in 185 countries. CA Cancer J Clin. 2021;71:209–49.
Galceran J, Ameijide A, Carulla M, Mateos A, Quiros JR, Rojas D, et al. Cancer incidence in Spain, 2015. Clin Transl Oncol. 2017;19:799–825.
Araghi M, Soerjomataram I, Jenkins M, Brierley J, Morris E, Bray F, et al. Global trends in colorectal cancer mortality: projections to the year 2035. Int J Cancer. 2019;144:2992–3000.
Cremolini C, Loupakis F, Antoniotti C, Lupi C, Sensi E, Lonardi S, et al. FOLFOXIRI plus bevacizumab versus FOLFIRI plus bevacizumab as first-line treatment of patients with metastatic colorectal cancer: updated overall survival and molecular subgroup analyses of the open-label, phase 3 TRIBE study. Lancet Oncol. 2015;16:1306–15.
Venook AP, Niedzwiecki D, Lenz HJ, Innocenti F, Fruth B, Meyerhardt JA, et al. Effect of first-line chemotherapy combined with cetuximab or bevacizumab on overall survival in patients with KRAS wild-type advanced or metastatic colorectal cancer: a randomized clinical trial. JAMA. 2017;317:2392–401.
Sorich MJ, Wiese MD, Rowland A, Kichenadasse G, McKinnon RA, Karapetis CS. Extended RAS mutations and anti-EGFR monoclonal antibody survival benefit in metastatic colorectal cancer: a meta-analysis of randomized, controlled trials. Ann Oncol. 2015;26:13–21.
Pietrantonio F, Petrelli F, Coinu A, Di Bartolomeo M, Borgonovo K, Maggi C, et al. Predictive role of BRAF mutations in patients with advanced colorectal cancer receiving cetuximab and panitumumab: a meta-analysis. Eur J Cancer. 2015;51:587–94.
Sartore-Bianchi A, Trusolino L, Martino C, Bencardino K, Lonardi S, Bergamo F, et al. Dual-targeted therapy with trastuzumab and lapatinib in treatment-refractory, KRAS codon 12/13 wild-type, HER2-positive metastatic colorectal cancer (HERACLES): a proof-of-concept, multicentre, open-label, phase 2 trial. Lancet Oncol. 2016;17:738–46.
Overman MJ, Lonardi S, Wong KYM, Lenz HJ, Gelsomino F, Aglietta M, et al. Durable clinical benefit with nivolumab plus ipilimumab in DNA mismatch repair-deficient/microsatellite instability-high metastatic colorectal cancer. J Clin Oncol. 2018;36:773–9.
Le DT, Durham JN, Smith KN, Wang H, Bartlett BR, Aulakh LK, et al. Mismatch repair deficiency predicts response of solid tumors to PD-1 blockade. Science. 2017;357:409–13.
Pietrantonio F, Di Nicolantonio F, Schrock AB, Lee J, Tejpar S, Sartore-Bianchi A, et al. ALK, ROS1, and NTRK rearrangements in metastatic colorectal cancer. J Natl Cancer Inst. 2017. https://doi.org/10.1093/jnci/djx089.
Grothey A, Van Cutsem E, Sobrero A, Siena S, Falcone A, Ychou M, et al. Regorafenib monotherapy for previously treated metastatic colorectal cancer (CORRECT): an international, multicentre, randomised, placebo-controlled, phase 3 trial. Lancet. 2013;381:303–12.
Mayer RJ, Van Cutsem E, Falcone A, Yoshino T, Garcia-Carbonero R, Mizunuma N, et al. Randomized trial of TAS-102 for refractory metastatic colorectal cancer. N Engl J Med. 2015;372:1909–19.
Price TJ, Peeters M, Kim TW, Li J, Cascinu S, Ruff P, et al. Panitumumab versus cetuximab in patients with chemotherapy-refractory wild-type KRAS exon 2 metastatic colorectal cancer (ASPECCT): a randomised, multicentre, open-label, non-inferiority phase 3 study. Lancet Oncol. 2014;15:569–79.
Vogel A, Hofheinz RD, Kubicka S, Arnold D. Treatment decisions in metastatic colorectal cancer - Beyond first and second line combination therapies. Cancer Treat Rev. 2017;59:54–60.
Arnold D, Prager GW, Quintela A, Stein A, Moreno Vera S, Mounedji N, et al. Beyond second-line therapy in patients with metastatic colorectal cancer: a systematic review. Ann Oncol. 2018;29:835–56.
Strickler JH, Cercek A, Siena S, Andre T, Ng K, Van Cutsem E, et al. Tucatinib plus trastuzumab for chemotherapy-refractory, HER2-positive, RAS wild-type unresectable or metastatic colorectal cancer (MOUNTAINEER): a multicentre, open-label, phase 2 study. Lancet Oncol. 2023;24:496–508.
Jones J, Hunter D. Consensus methods for medical and health services research. BMJ. 1995;311:376–80.
Fitch K, Bernstein SJ, Aguilar MD, Burnand B, LaCalle JR, Lázaro P et al. The RAND/UCLA Appropriateness Method User’s Manual. http://www.rand.org/pubs/monograph_reports/MR1269.html. Accessed 27 November 2023.
Hasson F, Keeney S, McKenna H. Research guidelines for the Delphi survey technique. J Adv Nurs. 2000;32:1008–15.
Abrahao ABK, Ko YJ, Berry S, Chan KKW. A comparison of regorafenib and TAS-102 for metastatic colorectal cancer: a systematic review and network meta-analysis. Clin Colorectal Cancer. 2018;17:113–20.
Prager GW, Taieb J, Fakih M, Ciardiello F, Van Cutsem E, Elez E, et al. Trifluridine-tipiracil and bevacizumab in refractory metastatic colorectal cancer. N Engl J Med. 2023;388:1657–67.
ESMO Metastatic Colorectal Cancer Living Guideline. Advanced and Metastatic Disease Without Potential Conversion. Third and Further Lines. https://www.esmo.org/living-guidelines/esmo-metastatic-colorectal-cancer-living-guideline/advanced-and-metastatic-disease-without-potential-conversion/advanced-and-metastatic-disease-without-potential-conversion/third-and-further-lines. Accessed 27 November 2023.
Jonker DJ, O’Callaghan CJ, Karapetis CS, Zalcberg JR, Tu D, Au HJ, et al. Cetuximab for the treatment of colorectal cancer. N Engl J Med. 2007;357:2040–8.
Cunningham D, Humblet Y, Siena S, Khayat D, Bleiberg H, Santoro A, et al. Cetuximab monotherapy and cetuximab plus irinotecan in irinotecan-refractory metastatic colorectal cancer. N Engl J Med. 2004;351:337–45.
Saltz LB, Meropol NJ, Loehrer PJ Sr, Needle MN, Kopit J, Mayer RJ. Phase II trial of cetuximab in patients with refractory colorectal cancer that expresses the epidermal growth factor receptor. J Clin Oncol. 2004;22:1201–8.
Karapetis CS, Khambata-Ford S, Jonker DJ, O’Callaghan CJ, Tu D, Tebbutt NC, et al. K-ras mutations and benefit from cetuximab in advanced colorectal cancer. N Engl J Med. 2008;359:1757–65.
Tabernero J, Argiles G, Sobrero AF, Borg C, Ohtsu A, Mayer RJ, et al. Effect of trifluridine/tipiracil in patients treated in RECOURSE by prognostic factors at baseline: an exploratory analysis. ESMO Open. 2020;5: e000752.
Van Cutsem E, Cervantes A, Adam R, Sobrero A, Van Krieken JH, Aderka D, et al. ESMO consensus guidelines for the management of patients with metastatic colorectal cancer. Ann Oncol. 2016;27:1386–422.
Lenz HJ, Stintzing S, Loupakis F. TAS-102, a novel antitumor agent: a review of the mechanism of action. Cancer Treat Rev. 2015;41:777–83.
Temmink OH, Emura T, de Bruin M, Fukushima M, Peters GJ. Therapeutic potential of the dual-targeted TAS-102 formulation in the treatment of gastrointestinal malignancies. Cancer Sci. 2007;98:779–89.
Acknowledgements
The authors would like to thank Fernando Sánchez Barbero PhD on behalf of Springer Healthcare for his help in the preparation of this manuscript. This assistance was funded by Servier. The authors would also like to thank the panelists who disinterestedly participated in the two rounds of the Delphi (Appendix).
Funding
Open Access funding provided thanks to the CRUE-CSIC agreement with Springer Nature. Servier funded this project without participating in any way.
Author information
Authors and Affiliations
Contributions
All authors contributed equally to the study conception and design. All of them participated in the discussion, drafting, revision, and final approval of the manuscript.
Corresponding author
Ethics declarations
Competing interests
PG-A received honoraria/consultation fees for speaker and consultancy/advisory roles from Amgen, Bayer, Bristol, Merck Serono, MSD, Lilly, Roche, Sanofi, Servier, and Pierre Fabre. RV received honoraria from/acted in an advisory role for Roche, Sanofi, MSD, Merck, Amgen, Novartis, Pierre Fabre, Lilly, and Servier; funding for educational/research programs from Roche, Lilly, and MSD; as well as payment of travel/accommodation expenses from Roche, Merck, Sanofi, Pierre Fabre, Servier, and MSD. EA received honoraria for an advisory role from Amgen, Bayer, Bristol Myers Squibb, Merck, Roche, Sanofi, and Servier; and received research funding from Roche. EE received honoraria from Amgen, Bayer, Hoffman La-Roche, Merck Serono, MSD, Novartis, Organon, Pierre Fabre, Pfizer, Sanofi, Seagen, Servier, and Takeda. FR was a consultant/advisor for Roche, Merck-Serono, Amgen, MSD, BMS, Lilly, Celgene, Sanofi-Aventis, Servier, Astra-Zeneca, Bayer, and Astellas; received research funding from Roche, Merck-Serono, Amgen, MSD, Lilly, Celgene, Sanofi-Aventis, Servier, Bayer; participated as a speaker for Roche, Merck-Serono, Amgen, MSD, BMS, Lilly, Celgene, Sanofi-Aventis, Servier, Bayer; and received grant support from Amgen.
Ethical approval
The manuscript does not contain clinical studies or patient data. No patients have participated.
Informed consent
Informed consent were not necessary.
Additional information
Publisher's Note
Springer Nature remains neutral with regard to jurisdictional claims in published maps and institutional affiliations.
Appendix
Rights and permissions
Open Access This article is licensed under a Creative Commons Attribution 4.0 International License, which permits use, sharing, adaptation, distribution and reproduction in any medium or format, as long as you give appropriate credit to the original author(s) and the source, provide a link to the Creative Commons licence, and indicate if changes were made. The images or other third party material in this article are included in the article's Creative Commons licence, unless indicated otherwise in a credit line to the material. If material is not included in the article's Creative Commons licence and your intended use is not permitted by statutory regulation or exceeds the permitted use, you will need to obtain permission directly from the copyright holder. To view a copy of this licence, visit http://creativecommons.org/licenses/by/4.0/.
About this article
Cite this article
García-Alfonso, P., Vera, R., Aranda, E. et al. Delphi consensus for the third-line treatment of metastatic colorectal cancer. Clin Transl Oncol 26, 1429–1437 (2024). https://doi.org/10.1007/s12094-023-03369-1
Received:
Accepted:
Published:
Issue Date:
DOI: https://doi.org/10.1007/s12094-023-03369-1