Abstract
Lung cancer (LC) is associated with ageing, with the average age of affected individuals being approximately 70 years. However, despite a higher incidence and prevalence among older people, the older adult population is underrepresented in clinical trials. For LC with Epidermal Growth Factor Receptor (EGFR) mutations, there is no clear association of this mutation with age. Geriatric assessments (GAs) and a multidisciplinary approach are essential for defining the optimal treatment. In this consensus, a group of experts selected from the Oncogeriatrics Section of the Spanish Society of Medical Oncology (Sección de Oncogeriatría de la Sociedad Española de Oncología Médica—SEOM), the Spanish Lung Cancer Group (Grupo Español de Cáncer de Pulmón—GECP) and the Association for Research on Lung Cancer in Women (Asociación para la Investigación del Cáncer de Pulmón en Mujeres—ICAPEM) evaluate the scientific evidence currently available and propose a series of recommendations to optimize the management of older adult patients with advanced LC with EGFR mutations.
Similar content being viewed by others
Avoid common mistakes on your manuscript.
Introduction
Scientific advances, progress in disease treatments and improvements in health conditions led to a progressive increase in the life expectancy worldwide. According to data from “World Population Prospects 2019” released by the United Nations, by the year 2050, one in every six people in the world will be over 65 years old (17%), much higher than that for the year 2019 (9%, one in every 11 people) [1].
Ageing brings with it an increased risk of cancer, originating from the accumulation ofoxidative stress and DNA damage across the years, both by endogenous and exogenous factors. The accumulation of free radicals, exposure to smoking, environmental pollution, changes in diet, etc., all increase the risk of cancer [2]. Also, with age, senescent cells accumulate, which can alter the microenvironment and promote tumour development. In addition, in older adults, there is a progressive deficit in immune function, altering the immune response to tumour growth [3]. Currently, developed countries considered 70 years old as the cut-off age for older adult patients. However, the majority of subanalysis had used 65 years old as a cut-off age.
Lung cancer (LC) is one of the neoplasms most associated with ageing. In this pathology, the risks described above accumulate.
The median age of patients with cancer is close to 70 years, but 30% are elder at diagnosis (almost 10% of patients are older than 80 years at diagnosis) [4]. Despite the higher incidence and prevalence of cancer among older individuals, the older adult population is often underrepresented in LC clinical trials. They are usually excluded due to comorbidity criteria or even due to the bias or ageism of professionals, who are less likely to include older adult patients in clinical trials.
The development of new drugs, especially targeted therapies, has made possible to change the prognostic and therapeutic paradigm of the cancer population. These advances must be employed throughout the population, regardless of chronological age [5]. For this reason, a group of experts from the Oncogeriatrics Section of the Spanish Society of Medical Oncology (Sección de Oncogeriatría de la Sociedad Española de Oncología Médica—SEOM), the Spanish Lung Cancer Group (Grupo Español de Cáncer de Pulmón—GECP) and the Association for Research on Lung Cancer in Women (Asociación para la Investigación del Cáncer de Pulmón en Mujeres—ICAPEM) reviewed the scientific evidence available for the older adult population with advanced LC, specifically in the population subgroup with activating mutations in the epidermal growth factor receptor (EGFR).
Epidemiological characteristics of older adult patients with EGFR-mutated LC
Although some studies indicate a higher incidence of EGFR-mutated LC among older adult patients [6], current data do not support a significant relationship between presence of mutation and ageing. Indeed, a recently published meta-analysis ruled out a relationship between age and a higher probability of EGFR gene mutation [7]. However, this mutation is associated with gender and smoking. Thus, while for men the incidence of mutated EGFR remains similar with age, for women, the incidence of mutated EGFR increases after the age of 65 [8]. Among never-smoker patients, EGFR mutations tend to increase with age in both sexes. The deletion of exon 19 is more frequent in patients under 50 years, while the L858R mutation in exon 21 is more common after 61 years [9]. There is no differential clinical profile of EGFR-mutated LC in the older adult population [10].
Evidence from geriatric assessments in the older adult population with LC
Geriatric assessments of cancer patients
The management of older adult patients with cancer is challenging due to the heterogeneity associated with ageing because chronological age does not always correspond to biological age. Over the years, there is a decrease in the functional reserve, leading to an increased risk of complications in situations of stress or illness. Additionally, the frequent presence of comorbidities, polypharmacy and malnutrition in this population can affect treatment tolerance and impact disease evolution (Table 1).
Since 2005, the International Society of Geriatric Oncology (SIOG) has recommended a geriatric assessment (GA) for older adult patients with cancer [11]. This recommendation also appears in the main clinical treatment guidelines of the National Comprehensive Cancer Network® (NCCN) [12], the European Society for Medical Oncology (ESMO) [13], and the SEOM [14, 15]. An adequate GA must cover functional, cognitive, and emotional aspects, nutritional status, comorbidities, social situation, and the presence of geriatric syndromes [11, 15]. GA allows the detection of problems and identification of needs in different spheres, the development of a treatment plan, an estimation of survival, and predictions of toxicity, while taking into account the preferences of the patient [16].
GA has been shown to provide more information than functional scales, such as the Eastern Cooperative Oncology Group (ECOG) performance status (PS) or the Karnofsky index, which are frequently used in daily clinical practice [17]. Given that the population of older patients with cancer is increasing and that GA requires considerable time to perform, a series of screening tools have been developed to select patients who require a more complete and specific assessment. The most widely used tool in oncology is the G8 scale, which was developed specifically for use in older patients with cancer [18].
Once a GA is completed, patients are classified as robust, prefragile and fragile [19]. GA, in addition to allowing treatment to be adapted to the profile of each patient, allows for the identification of dose adjustments or reductions and alternative treatment options, for example, granulocyte colony-stimulating factors (G-CSF), especially for individuals indicated for chemotherapy and at a high risk of toxicity [14].
GA in patients with LC, including EGFR-mutations
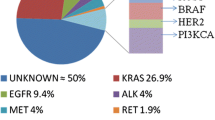
Evidence supports the use of GA to evaluate vulnerabilities in older patients with LC. Instrumental activities of daily living (IADL) identify one of the most frequently detected impairments, followed by polypharmacy, comorbidity, risk of malnutrition and depression. GA classified 37% of evaluated patients with PS 0, and 33% with PS 1, as vulnerable because of comorbidity; and 11% and 19%, respectively, as frail because of activities of daily living (ADL) and comorbidity, respectively (Fig. 1) [20].
A systematic review demonstrated the association between GA and outcome in patients treated with chemotherapy not assessed for PS [21]. Patients with a median age of 76 years had a high prevalence of geriatric impairments (29% cognitive, 70% IADL). Objective physical capacity and nutritional status had a consistent association with mortality and with chemotherapy completion.
A phase III trial randomized 494 patients ≥ 70 years, with PS 0–2 and stage IV non-small cell lung cancer (NSCLC) [22], to a standard strategy of treatment allocation based on age and PS compared with an experimental arm based on GA. All patients were EGFR and ALK wild type or unknown. In the control arm, patients received double or single chemotherapy agent according to PS and age. In the experimental arm, fit and vulnerable patients received double or single agent, respectively, and frail patients received best support care. Patients in the GA arm experienced significantly less all-grade toxicities (86% vs. 93%, respectively; p = 0.015). However, no differences in terms of overall survival (OS) were observed.
In older adult patients with LC harbouring an EGFR mutation, several observational studies support the safety and efficacy of EGFR tyrosine kinase inhibitors (TKIs) in first line, but there are concerns about a higher risk of toxicity. Frailty has been retrospectively evaluated in 114 patients ≥ 80 years treated with EGFR TKIs. GA was performed in 35% of them. Twenty-eight percent had PS 3–4, 45% needed assistance at home and 38% were taking ≥ 6 drugs per day. There was a clear benefit of EGFR TKIs in terms of survival, and toxicities were consistent with adverse events (AEs) observed in younger patients [23]. A recent systematic review recommends GA to identify malnutrition, comorbidities, polypharmacy, and an alteration of the functional status, which might impact OS and progression free survival (PFS) [24].
Polypharmacy due to comorbidities and drug interactions
The existence of drug interactions is relevant when initiating treatment with EGFR TKIs in older adult patients with LC, as this population is prone to polypharmacy due to the symptoms of cancer and the presence of comorbidities. In a retrospective study of 334 patients treated with EGFR TKIs, a prevalence of polypharmacy of 38% was observed, and potentially inappropriate medication (PIM) was detected for 32% of the participants [25]. Polypharmacy was independently correlated with OS and hospitalization during treatment.
Most EGFR TKIs are susceptible to drug interactions throughout the pharmacokinetic process. The alteration in gastric pH affects the absorption of erlotinib, gefitinib and dacomitinib. Among older adult patients with cancer, approximately 55% use proton pump inhibitors [26], which have been associated with a lower plasma concentration and OS in patients treated with erlotinib [27, 28].
EGFR TKIs are substrates of membrane transporters, such as P-gp and breast cancer resistance protein (BCRP). The inhibition or induction of these membrane transporters by different drugs can influence the absorption of EGFR TKIs. EGFR TKIs can increase exposure to BCRP substrates, such as rosuvastatin, and P-gp substrates, such as digoxin, dabigatran, aliskiren and pravastatin, which have a narrow therapeutic index [29].
Although the metabolism of some EGFR TKIs begins in the intestine, most are primarily metabolized in the liver. The enzyme most involved is cytochrome CYP3A4 [29]; its inhibition increases the pharmacokinetic parameters of erlotinib, gefitinib and osimertinib, and its induction decreases their plasma levels. Ciprofloxacin and strong CYP1A2 inhibitors can elevate erlotinib levels, which, together with gefitinib, can potentiate the effect of warfarin [30]. Although predictable drug interactions with direct anticoagulants, such as apixaban, may not be relevant [31], control of the therapeutic action is recommended because atrial fibrillation is the most frequent arrhythmia. Afatinib forms covalent adducts with proteins, and its enzymatic metabolism is minimal; therefore, it is not affected by cytochromes and should be considered in this context [29]. Finally, the risk of QTc interval lengthening observed with osimertinib is an important factor to consider in patients with cardiac risk factors and could increase when osimertinib is prescribed with other drugs, such as some antibiotics, antifungals, antidepressants and antiemetics [29].
Therefore, to avoid affecting efficacy and to reduce the risk of toxicity in older adult patients requiring EGFR TKIs, concomitant medication should be reviewed, and any PIM should be avoided. More studies are needed in this regard. Currently, the choice of EGFR TKI will depend on the alternatives that exist in each scenario and the concurrent medications essential for the treatment of each patient’s comorbidities.
Treatment options for older adult patients with EGFR-mutated LC
Table 2 summarizes the efficacy and safety of different schedules to treat older adult patients with EGFR-mutated LC.
First-generation drugs
Despite the rapid development of drugs targeting EGFR, there are few specific trials focused on their efficacy in older adult patients and most information comes from subgroup analyses in the major randomized clinical trials that supported the registration of the drugs.
Gefitinib
The first evidence of the efficacy of the targeted therapy gefitinib in LC EGFR-mutated patients were reported in 2004 [32, 33]. Results of phase III trials started in 2009 with the IPASS trial showing an increased PFS (9.5 vs. 6.3 months, hazard ratio [HR] 0.48) and a better response rate (RR) (71% vs. 47%) in patients with EGFR-mutated LC when treated with gefitinib compared with platinum-based chemotherapy [34]. Median age of included patients was 57 years and for 76 patients aged > 65 years results remained significant with HR 0.58 for PFS. A second phase III trial comparing gefitinib with carboplatin-docetaxel in 172 patients with a median age of 64 years achieved similar results (median PFS was 9.2 vs. 6.3 months, HR = 0.489) without any significant differences between patients older or younger than 65 years [35].
One phase II trial performed in 31 patients older than 75 years (with a median age of 80 years) showed a median PFS of 12.3 months with a RR of 74%. Disease control rate (DCR) was 90% with an incidence of grade 3–4 AEs of 29% [36]. Inferior results were seen in another phase II trial performed in 30 patients older than 80 years or with a PS 3–4 (median age: 72 years). PFS was only 6.5 months, OS was 17.8 months, RR was 66% and DCR was 90%. PS was improved in 68% of patients [37].
In a retrospective analysis of 62 patients older than 75 years with a median age of 80 years, results were PFS 13.2 months, OS 19 months, RR 61%, and DCR 84%. A total of 29% of patients showed grade 3–4 AEs [38].
Erlotinib
Phase III trials comparing erlotinib with platinum-based chemotherapy were: (i) the EURTAC trial with an HR of 0.37 in terms of PFS in favour of erlotinib in patients with a median age of 65 years. In 88 patients older than 65 years, HR was 0.28 [39]; (ii) the OPTIMAL trial with an HR of 0.16 in terms of PFS in patients with a median age of 58 years [40]. In the subgroup of patients older than 65 years, 38 of them (25%) had an HR of 0.17 when treated with erlotinib; and (iii) the ENSURE trial, which included only 45 patients (21%) aged more than 65 years, but it did not provide a specific subgroup for older adult patients [41].
Phase II trials with first-line erlotinib in patients older 75 years were: (i) Inoue et al. trial, 32 patients with a median age of 80 years who had a median PFS of 15.5 months, RR of 56%, DCR 91% with an incidence of grade 3–4 AEs observed in 28% of patients [42]; (ii) Miyamoto et al.trial, 80 patients (> 75 years or frail) with a median age 80 years (49–90) who achieved a median PFS of 9.3 months, an OS of 26.2 months, RR of 60%, DCR of 90%, and 18% of patients developing grade 3–4 AEs [43].
In a phase III trial that compared erlotinib with placebo in 770 unselected patients with advanced NSCLC unsuitable for chemotherapy (63% of them > 75 years), OS benefit was seen in patients who developed first-cycle rash in all subgroups including those with the worst characteristics, such as age ≥ 75 years [OS HR 0.77 (0.61–0.97, p = 0.028) and PFS HR 0.71 (0.56–0.89, p = 0.0032)] [44].
In a pharmacokinetics study of erlotinib plasma concentrations, age was associated with a lower oral clearance (CL/F), and a dose reduction or treatment discontinuation due to AEs was observed in 52% of patients > 75 years old compared with 25% of younger patients [45].
A meta-analysis, assessing the impact of different EGFR mutations and clinical characteristics on PFS in 1649 patients with advanced EGFR-mutant NSCLC included in randomized controlled trials of EGFR TKIs compared with chemotherapy in first-line treatment (203 of them treated with gefitinib and 278 with erlotinib in addition to 472 treated with afatinib), found that age (lower or greater than 65 years) did not predict a significant difference in terms of PFS, with HR 0.34 in younger versus 0.37 for overall population with interaction p-value of 0.27 [46].
Second-generation drugs
Currently, the second-generation TKIs available for the treatment of patients with EGFR-mutated LC are afatinib and dacomitinib.
Afatinib
In the Lux LUNG 3 and Lux LUNG 6 phase III studies of afatinib, 134 patients and 86 patients older than 65 years were included, and RR, PFS and OS results for these patients were similar to those observed in the general population, with a similar percentage of Grade 3 AEs, the most frequent being gastrointestinal (GI) toxicity, specifically diarrhoea, and dermal and nail toxicity [47, 48].
The toxicity observed in the phase III studies was the basis for the design of phase II studies with a population ≥ 70 years. A prospective study by Imai et al. included 40 patients with a median age of 77 years [49] who were initially administered 30 mg/day of afatinib. A RR of 73% was observed, with a median PFS of 12.9 months and percentages of patients alive in the first, second and fourth years of 87%, 61% and 52%, respectively. The most important grade 3 toxicities were diarrhoea (13%) and mucositis (8%). Two toxic deaths from pneumonitis were reported, and eight patients had to discontinue treatment.
A second study evaluated the administration of a starting dose of 20 mg/day of afatinib in patients with a mean age of 70 years. In that study, a RR of 66% was observed, with a PFS of 12.6 months, like previous studies with higher doses of afatinib. The incidence of GI toxicity (grade 3 diarrhoea) was 7.5%, which forms the basis of starting treatment with afatinib at low doses to maintain efficacy while reducing GI toxicity [50].
Dacomitinib
A phase III study comparing dacomitinib with gefitinib (ARCHER 1050) included 94 patients (41%) in the dacomitinib arm, without greater toxicity and with similar efficacy to the other treatment arm [51]. In a phase III study comparing dacomitinib with erlotinib (ARCHER 1009), 163 pretreated patients aged 65–74 years (37%) and 50 patients older than 70 years (11%) were included [52]. No differences were observed in terms of efficacy between the population older than 65 years and the overall study population.
For dacomitinib, there are no clinical trials with a population ≥ 70 years, but there are studies with real world data (RWD) in which dacomitinib has been administered to patients up to 83 years of age. In these studies, the starting dose was adjusted to 30 mg/day in patients with PS 1 and with a starting weight less than 60 kg, but no dose adjustment was made only according to patients’ age [53].
Third-generation drugs
Osimertinib
No data in patients ≥ 70 years have been published from pivotal phase III trials ADAURA, FLAURA, AURA 3 [54,55,56,57]. With a cut-off of 65 years, a significant benefit in terms of PFS was observed for osimertinib in all studies. Safety data based on age was not reported in these studies.
Several retrospective studies in a RWD have reported efficacy and safety data in older adult patients with osimertinib in untreated and pre-treated EGFR-mutated advanced NSCLC. Efficacy of osimertinib was in line with that observed in the pivotal trials, although the incidence of AEs seemed to be higher in older adult patients. HOT2002 is a first-line retrospective Japanese study in 132 patients ≥ 75 years with EGFR-TKI sensitizing mutations [58]. The median PFS was 19.4 months, with a better PFS in patients under 80 years of age. Grade ≥ 3 AEs were higher than in the FLAURA trial (42% vs. 34%). The most common AE was paronychia (44%), rash (39%), dry skin (39%) and anaemia (39%). The frequency of pneumonitis was 17% (grade ≥ 3 was 9%) with a mortality of 13%. A total of 41% required ≥ 1 dose reduction and 27% discontinued osimertinib, with pneumonitis the most common reason for discontinuation.
In pre-treated EGFR T790M mutation NSCLC patients, the ASTRIS trial reported similar outcomes in patients ≥ 75 years compared with < 75 years. Median PFS was 11.8 months (10.2–12.5) and 10.9 months (10.4–11.1) and estimated 1-year OS rate was 77% (68–79%) and 76% (74–78%), respectively [59]. Safety outcomes in the older adult population were not reported. In a phase II trial in 36 Japanese older adult patients (≥ 75 years) with T790M EGFR mutation, the median PFS was 11.9 months (95% confidence interval [CI] 7.9–17.5), and the median OS was 22.0 months (95% CI, 16.0-not reached [NR]) [60]. Most frequent AEs were fatigue (39%), anorexia (39%), diarrhoea (36%), rash (33%), paronychia (33%), haematological toxicity (40–48%) and hepatic toxicity (37–42%). There were no deaths, dose reductions nor discontinuations. Another study of Japanese patients included 17 patients ≥ 75 years, with no significant differences in terms of efficacy in these patients. Median PFS was 10.5 months (95% CI = 7.8–15.8) in the non-older adults’ group and 17.7 months (95% CI 8.4-NR, p = 0.11) in the older adults’ group, and median OS was NR (95% CI 15.5-NR) and 38.6 months (95% CI 14.3–52.8, p = 0.20), respectively. There were no differences in the frequency of AEs, except for grade ≥ 2 paronychia (2% vs. 17%, p = 0.04), and no differences in the incidence of dose reduction or discontinuation were observed [61]. GFPC 01-2016 included 43 octogenarian pre-treated patients that received osimertinib. Median PFS was 17.5 months (95% CI 12.2–19.0) and median OS was 22.8 months (95% CI 15.7–NR) [62]. Safety data was not reported.
Lazertinib
Lazertinib has been evaluated in a phase I/II trial in 78 pre-treated Asian patients with NSCLC harbouring the T790M EGFR mutation. However, efficacy and safety data based on the population age was not reported in this study [63].
Atypical mutations
Atypical EGFR mutations comprise 30% of EGFR-mutated NSCLC and this is a heterogenous group with different sensitivities to EGFR TKI [64].
EGFR exon20 insertions (EGFRex20ins) accounts for up to 12% of all EGFR mutations subtypes, representing the third most common EGFR mutation. Epidemiological characteristics of patients with EGFRex20ins mirror those with common EGFR mutations. However, some cohorts have reported that patients with EGFRex20ins NSCLC are older than patients with common EGFR mutations (67 years vs. 63 years, p = 0.01). NSCLC with EGFRex20ins have a poor prognosis [65], due to limited activity of the approved EGFR TKIs [66], with only some clinical activity with osimertinib at double dose and no data about the efficacy or toxicity in EGFRex20ins NSCLC according to age, because the sample size is too small [67]. Both the Food and Drug Administration (FDA) and the European Medicines Agency (EMA) have approved amivantamab in patients with platinum-refractory EGFRex20ins NSCLC [68], whereas mobocertinib has been approved only by the FDA in the same setting [69]. These drugs have shown clinical activity in terms of RR (28–40%), median PFS (7.3–8.3 months) and OS (~ 2 years). Although both drugs had higher RR in younger patients, the cut-off was 65 years-old and median age was 62 years (42–84) in amivantamab and 60 years (27–84) in mobocertinib trial, respectively. Safety profile data according to age has not been reported [68, 69].
Uncommon EGFR mutations (G719X, S7681, L861Q and combinations) can occur more frequently in older adult patients (67.5 years) compared with other EGFR mutations [70]. However, this is not confirmed by other authors, who reported a median age of 60 years [71]. In current guidelines, afatinib and/or osimertinib are recommended for treatment of patients with these mutations [70,71,72], also because less data is available from other EGFR-TKIs. Unfortunately, no data about efficacy and safety is reported according to age.
Combinations with antiangiogenic drugs and chemotherapy
Although initially effective, resistance to EGFR TKIs emerges within 10–12 months. There is also a proportion of patients with primary resistance [73,74,75]. Thus, to improve patient outcomes, new therapeutic strategies have been studied. Among them are EGFR TKIs combinations with both vascular endothelial growth factor (VEGF) inhibitors and chemotherapy.
In treatment-naïve patients, EGFR TKIs with platinum-doublet based chemotherapy compared with first-generation EGFR TKIs demonstrated improved OS, PFS and RR with the combination, though with grade ≥ 3 AEs [76,77,78]. The recent OPAL trial has addressed the combination of osimertinib plus platinum-pemetrexed chemotherapy in first-line. Although the results are encouraging (RR 91% and median PFS 31 months), 89.6% of patients experienced grade 3 AEs. Efficacy and toxicity regarding the age is not reported. Although efficacy results are encouraging, toxicity of combination strategy and the lack of direct comparison with osimertinib prevent their use as standard first-line therapy until the results of the phase III FLAURA2 trial (NCT04035486). Osimertinib plus bevacizumab was detrimental in second line compared to osimertinib alone [77]. The median age of the included population was < 65 years [76, 78]. There are no reports on safety data according to age. All these facts limit the applicability of these data to our population.
EGFR TKI combinations with both bevacizumab and ramucirumab have been studied. All RCT trials (except for one phase II) have shown improvement of PFS when compared with first-generation EGFR TKI as monotherapy, but they have not demonstrated an OS benefit [79,80,81]. Additionally, anti-VEGF drugs doubled high-grade toxicities. Efficacy data cut-off and median population age (65 years [57,58,59,60,61,62,63,64,65,66,67,68,69,70,71]) of the erlotinib-ramucirumab combination limit the evidence for this combination in our population [82]. In the RELAY study, the incidence of grade ≥ 3 AEs was higher in patients aged ≥ 70 than < 70 years in the ramucirumab plus erlotinib arm [83].
Diagnostic recommendations, management, and treatment.
Clinical guidelines strongly recommend performing a GA in all older adult patients with NSCLC, regardless of the genomic profile [84]. The GA should also therefore be considered in patients harbouring an EGFR mutation despite being candidates for EGFR TKIs, which have fewer toxic effects than platinum-based chemotherapy.
EGFR and other actionable genomic alterations should be tested in all patients diagnosed with non-squamous NSCLC, independently of the age at diagnosis [85]. Currently, multigene next-generation sequencing (NGS) is recommended in non-squamous NSCLC whenever possible [86]. In newly diagnosed patients with small tumour biopsies or lack of adequate tumour tissue for molecular testing, a liquid biopsy should be considered to assess EGFR status, either by single gene testing or by NGS [87]. Older adult patients with EGFR mutated MNSCLC should receive upfront targeted therapy with an EGFR TKI. In a pooled analysis of clinical trials evaluating first and second-generation EGFR TKIs, the benefit in terms of PFS was consistent in older adult patients (HR = 0.39, 95% CI 0.20–0.78) and in their younger counterparts (HR = 0.48, 95% CI 0.24–0.96) [88]. An exploratory subgroup analysis of the FLAURA study showed that frontline osimertinib yielded significant benefit in terms of PFS independently of the age at diagnosis [56]. Osimertinib has been considered the preferred treatment option in older adult patients with common EGFR mutations due to its favourable balance between efficacy and safety. Although safety data was not reported according to patients’ age in most trials, it is known that lung and cardiac toxicities associated with EGFR TKIs should be particularly monitored in this vulnerable population.
In patients with uncommon mutations such as G719X, S768I or L861Q, osimertinib and afatinib are the preferred treatment options, while in patients with an EGFRex20ins, amivantamab and mobocertinib have demonstrated treatment efficacy. However, data on efficacy and safety of those treatment strategies in the older adult population is still missing. Academic and collaborative initiatives to collect efficacy and safety data of EGFR TKIs in older adult patients with EGFR mutated NSCLC are therefore warranted and should be promoted by cooperative groups.
Conclusions
The population is ageing. The incidence of certain diseases, such as cancer and particularly LC, increases with age. We consider that 70 years should be the threshold for including individuals in the older adult population; however, the cut-off used in most studies is 65 years. This limits the interpretation of the current available evidence. Older adult population with cancer requires a multidisciplinary approach with specific tools developed for geriatric medicine.
GA is beneficial during the LC diagnosis and treatment process, but most of the scientific evidence applies to patients who are candidates for chemotherapy. Data on the value of GA for patients with actionable genomic alterations, specifically EGFR mutations, are limited.
Given the efficacy of EGFR TKI in the older adult population and its favourable toxicity profile, it is essential to carry out mutational studies for these patients with LC, regardless of age and stage of LC. Applying GA in the population with EGFR mutation continues to be a healthcare challenge, given its lower level of scientific evidence and constraints in clinical practice. Prospective data on the value of GA in this population are also needed.
Availability of data and material
Not applicable.
Code availability
Not applicable.
References
United Nations DoEaSA. World population prospects 2019: Data Booklet. ST/ESA/SER.A/424. 2019.
Berben L, Floris G, Wildiers H, Hatse S. Cancer and aging: two tightly interconnected biological processes. Cancers (Basel). 2021. https://doi.org/10.3390/cancers13061400.
Franceschi C, Campisi J. Chronic inflammation (inflammaging) and its potential contribution to age-associated diseases. J Gerontol A Biol Sci Med Sci. 2014;69(Suppl 1):S4-9. https://doi.org/10.1093/gerona/glu057.
SEER. Cancer Stat Facts: Lung and Bronchus Cancer. https://seer.cancer.gov/statfacts/html/lungb.html. 2022.
Presley CJ, Reynolds CH, Langer CJ. Caring for the older population with advanced lung cancer. Am Soc Clin Oncol Educ Book. 2017;37:587–96. https://doi.org/10.1200/edbk_179850.
Ueno T, Toyooka S, Suda K, Soh J, Yatabe Y, Miyoshi S, et al. Impact of age on epidermal growth factor receptor mutation in lung cancer. Lung Cancer. 2012;78(3):207–11. https://doi.org/10.1016/j.lungcan.2012.09.006.
Melosky B, Kambartel K, Häntschel M, Bennetts M, Nickens DJ, Brinkmann J, et al. Worldwide prevalence of epidermal growth factor receptor mutations in non-small cell lung cancer: a meta-analysis. Mol Diagn Ther. 2022;26(1):7–18. https://doi.org/10.1007/s40291-021-00563-1.
Gahr S, Stoehr R, Geissinger E, Ficker JH, Brueckl WM, Gschwendtner A, et al. EGFR mutational status in a large series of Caucasian European NSCLC patients: data from daily practice. Br J Cancer. 2013;109(7):1821–8. https://doi.org/10.1038/bjc.2013.511.
Zhang Y, He D, Fang W, Kang S, Chen G, Hong S, et al. The difference of clinical characteristics between patients with Exon 19 deletion and those with L858R mutation in nonsmall cell lung cancer. Medicine (Baltimore). 2015;94(44):e1949. https://doi.org/10.1097/md.0000000000001949.
Liu L, Xiong X. Clinicopathologic features and molecular biomarkers as predictors of epidermal growth factor receptor gene mutation in non-small cell lung cancer patients. Curr Oncol. 2021;29(1):77–93. https://doi.org/10.3390/curroncol29010007.
Decoster L, Van Puyvelde K, Mohile S, Wedding U, Basso U, Colloca G, et al. Screening tools for multidimensional health problems warranting a geriatric assessment in older cancer patients: an update on SIOG recommendations†. Ann Oncol. 2015;26(2):288–300. https://doi.org/10.1093/annonc/mdu210.
NCCN. NCCN Guidelines Older Adult Oncology, NCCN clinical practice guidelines in oncology—Older Adult Oncology. 2022. https://www.nccn.org/professionals/physician_gls/pdf/senior.pdf. Accessed Jan 15 2023.
Planchard D, Popat S, Kerr K, Novello S, Smit EF, Faivre-Finn C, et al. Metastatic non-small cell lung cancer: ESMO Clinical Practice Guidelines for diagnosis, treatment and follow-up. Ann Oncol. 2018;29(Suppl 4):iv192–237. https://doi.org/10.1093/annonc/mdy275.
Gironés Sarrió R, Antonio Rebollo M, Molina Garrido MJ, Guillén-Ponce C, Blanco R, Gonzalez Flores E, et al. General recommendations paper on the management of older patients with cancer: the SEOM geriatric oncology task force’s position statement. Clin Transl Oncol. 2018;20(10):1246–51. https://doi.org/10.1007/s12094-018-1856-x.
Molina-Garrido MJ, Guillén-Ponce C, Blanco R, Saldaña J, Feliú J, Antonio M, et al. Delphi consensus of an expert committee in oncogeriatrics regarding comprehensive geriatric assessment in seniors with cancer in Spain. J Geriatr Oncol. 2018;9(4):337–45. https://doi.org/10.1016/j.jgo.2017.11.012.
Hamaker ME, Jonker JM, de Rooij SE, Vos AG, Smorenburg CH, van Munster BC. Frailty screening methods for predicting outcome of a comprehensive geriatric assessment in elderly patients with cancer: a systematic review. Lancet Oncol. 2012;13(10):e437–44. https://doi.org/10.1016/s1470-2045(12)70259-0.
Extermann M, Hurria A. Comprehensive geriatric assessment for older patients with cancer. J Clin Oncol. 2007;25(14):1824–31. https://doi.org/10.1200/jco.2007.10.6559.
Martinez-Tapia C, Canoui-Poitrine F, Bastuji-Garin S, Soubeyran P, Mathoulin-Pelissier S, Tournigand C, et al. Optimizing the G8 screening tool for older patients with cancer: diagnostic performance and validation of a six-item version. Oncologist. 2016;21(2):188–95. https://doi.org/10.1634/theoncologist.2015-0326.
Hamaker ME, Te Molder M, Thielen N, van Munster BC, Schiphorst AH, van Huis LH. The effect of a geriatric evaluation on treatment decisions and outcome for older cancer patients—a systematic review. J Geriatr Oncol. 2018;9(5):430–40. https://doi.org/10.1016/j.jgo.2018.03.014.
Gironés R, Aparisi F, García-Sánchez J, Sánchez-Hernández A, García Piñón F, Juan-Vidal Ó. Geriatric assessment in clinical practice for patients with stage IV non-small-cell lung cancer: the Grup de Investigació I Divulgació Oncològica experience. Eur J Cancer Care (Engl). 2018;27(6):e12950. https://doi.org/10.1111/ecc.12950.
Schulkes KJ, Hamaker ME, van den Bos F, van Elden LJ. Relevance of a geriatric assessment for elderly patients with lung cancer—a systematic review. Clin Lung Cancer. 2016;17(5):341-9.e3. https://doi.org/10.1016/j.cllc.2016.05.007.
Corre R, Greillier L, Le Caër H, Audigier-Valette C, Baize N, Bérard H, et al. Use of a comprehensive geriatric assessment for the management of elderly patients with advanced non-small-cell lung cancer: the phase III randomized ESOGIA-GFPC-GECP 08–02 study. J Clin Oncol. 2016;34(13):1476–83. https://doi.org/10.1200/jco.2015.63.5839.
Corre R, Gervais R, Guisier F, Tassy L, Vinas F, Lamy R, et al. Octogenarians with EGFR-mutated non-small cell lung cancer treated by tyrosine-kinase inhibitor: a multicentric real-world study assessing tolerance and efficacy (OCTOMUT study). Oncotarget. 2018;9(9):8253–62. https://doi.org/10.18632/oncotarget.23836.
Greillier L, Gauvrit M, Paillaud E, Girard N, Montégut C, Boulahssass R, et al. Targeted therapy for older patients with non-small cell lung cancer: systematic review and guidelines from the French Society of Geriatric Oncology (SoFOG) and the French-Language Society of Pulmonology (SPLF)/French-Language Oncology Group (GOLF). Cancers (Basel). 2022. https://doi.org/10.3390/cancers14030769.
Hakozaki T, Matsuo T, Shimizu A, Ishihara Y, Hosomi Y. Polypharmacy among older advanced lung cancer patients taking EGFR tyrosine kinase inhibitors. J Geriatr Oncol. 2021;12(1):64–71. https://doi.org/10.1016/j.jgo.2020.09.011.
Sharma M, Holmes HM, Mehta HB, Chen H, Aparasu RR, Shih YT, et al. The concomitant use of tyrosine kinase inhibitors and proton pump inhibitors: prevalence, predictors, and impact on survival and discontinuation of therapy in older adults with cancer. Cancer. 2019;125(7):1155–62. https://doi.org/10.1002/cncr.31917.
Chu MP, Ghosh S, Chambers CR, Basappa N, Butts CA, Chu Q, et al. Gastric acid suppression is associated with decreased erlotinib efficacy in non-small-cell lung cancer. Clin Lung Cancer. 2015;16(1):33–9. https://doi.org/10.1016/j.cllc.2014.07.005.
Cardoso E, Guidi M, Khoudour N, Boudou-Rouquette P, Fabre E, Tlemsani C, et al. Population pharmacokinetics of erlotinib in patients with non-small cell lung cancer: its application for individualized dosing regimens in older patients. Clin Ther. 2020;42(7):1302–16. https://doi.org/10.1016/j.clinthera.2020.05.008.
Libiad Y, Boutayeb S, Chaibi A. Drug-drug interactions of tyrosine kinase inhibitors in treatment of non-small-cell lung carcinoma. Bull Cancer. 2022;109(3):358–81. https://doi.org/10.1016/j.bulcan.2021.11.019.
Hiraide M, Minowa Y, Nakano Y, Suzuki K, Shiga T, Nishio M, et al. Drug interactions between tyrosine kinase inhibitors (gefitinib and erlotinib) and warfarin: assessment of international normalized ratio elevation characteristics and in vitro CYP2C9 activity. J Oncol Pharm Pract. 2019;25(7):1599–607. https://doi.org/10.1177/1078155218801061.
López-Fernández T, Martín-García A, Roldán Rabadán I, Mitroi C, Mazón Ramos P, Díez-Villanueva P, et al. Atrial fibrillation in active cancer patients: expert position paper and recommendations. Rev Esp Cardiol (Engl Ed). 2019;72(9):749–59. https://doi.org/10.1016/j.rec.2019.03.019.
Lynch TJ, Bell DW, Sordella R, Gurubhagavatula S, Okimoto RA, Brannigan BW, et al. Activating mutations in the epidermal growth factor receptor underlying responsiveness of non-small-cell lung cancer to gefitinib. N Engl J Med. 2004;350(21):2129–39. https://doi.org/10.1056/NEJMoa040938.
Paez JG, Jänne PA, Lee JC, Tracy S, Greulich H, Gabriel S, et al. EGFR mutations in lung cancer: correlation with clinical response to gefitinib therapy. Science. 2004;304(5676):1497–500. https://doi.org/10.1126/science.1099314.
Mok TS, Wu YL, Thongprasert S, Yang CH, Chu DT, Saijo N, et al. Gefitinib or carboplatin-paclitaxel in pulmonary adenocarcinoma. N Engl J Med. 2009;361(10):947–57. https://doi.org/10.1056/NEJMoa0810699.
Mitsudomi T, Morita S, Yatabe Y, Negoro S, Okamoto I, Tsurutani J, et al. Gefitinib versus cisplatin plus docetaxel in patients with non-small-cell lung cancer harbouring mutations of the epidermal growth factor receptor (WJTOG3405): an open label, randomised phase 3 trial. Lancet Oncol. 2010;11(2):121–8. https://doi.org/10.1016/s1470-2045(09)70364-x.
Maemondo M, Minegishi Y, Inoue A, Kobayashi K, Harada M, Okinaga S, et al. First-line gefitinib in patients aged 75 or older with advanced non-small cell lung cancer harboring epidermal growth factor receptor mutations: NEJ 003 study. J Thorac Oncol. 2012;7(9):1417–22. https://doi.org/10.1097/JTO.0b013e318260de8b.
Inoue A, Kobayashi K, Usui K, Maemondo M, Okinaga S, Mikami I, et al. First-line gefitinib for patients with advanced non-small-cell lung cancer harboring epidermal growth factor receptor mutations without indication for chemotherapy. J Clin Oncol. 2009;27(9):1394–400. https://doi.org/10.1200/jco.2008.18.7658.
Kuwako T, Imai H, Masuda T, Miura Y, Seki K, Yoshino R, et al. First-line gefitinib treatment in elderly patients (aged ≥75 years) with non-small cell lung cancer harboring EGFR mutations. Cancer Chemother Pharmacol. 2015;76(4):761–9. https://doi.org/10.1007/s00280-015-2841-5.
Rosell R, Carcereny E, Gervais R, Vergnenegre A, Massuti B, Felip E, et al. Erlotinib versus standard chemotherapy as first-line treatment for European patients with advanced EGFR mutation-positive non-small-cell lung cancer (EURTAC): a multicentre, open-label, randomised phase 3 trial. Lancet Oncol. 2012;13(3):239–46. https://doi.org/10.1016/s1470-2045(11)70393-x.
Zhou C, Wu YL, Chen G, Feng J, Liu XQ, Wang C, et al. Erlotinib versus chemotherapy as first-line treatment for patients with advanced EGFR mutation-positive non-small-cell lung cancer (OPTIMAL, CTONG-0802): a multicentre, open-label, randomised, phase 3 study. Lancet Oncol. 2011;12(8):735–42. https://doi.org/10.1016/s1470-2045(11)70184-x.
Wu YL, Zhou C, Liam CK, Wu G, Liu X, Zhong Z, et al. First-line erlotinib versus gemcitabine/cisplatin in patients with advanced EGFR mutation-positive non-small-cell lung cancer: analyses from the phase III, randomized, open-label. ENSURE study Ann Oncol. 2015;26(9):1883–9. https://doi.org/10.1093/annonc/mdv270.
Inoue Y, Inui N, Asada K, Karayama M, Matsuda H, Yokomura K, et al. Phase II study of erlotinib in elderly patients with non-small cell lung cancer harboring epidermal growth factor receptor mutations. Cancer Chemother Pharmacol. 2015;76(1):155–61. https://doi.org/10.1007/s00280-015-2784-x.
Miyamoto S, Azuma K, Ishii H, Bessho A, Hosokawa S, Fukamatsu N, et al. Low-dose erlotinib treatment in elderly or frail patients with EGFR mutation-positive non-small cell lung cancer: a multicenter phase 2 trial. JAMA Oncol. 2020;6(7):e201250. https://doi.org/10.1001/jamaoncol.2020.1250.
Lee SM, Khan I, Upadhyay S, Lewanski C, Falk S, Skailes G, et al. First-line erlotinib in patients with advanced non-small-cell lung cancer unsuitable for chemotherapy (TOPICAL): a double-blind, placebo-controlled, phase 3 trial. Lancet Oncol. 2012;13(11):1161–70. https://doi.org/10.1016/s1470-2045(12)70412-6.
Evelina C, Guidi M, Khoudour N, Pascaline B-R, Fabre E, Tlemsani C, et al. Population pharmacokinetics of erlotinib in patients with non-small cell lung cancer: its application for individualized dosing regimens in older patients. Clin Ther. 2020;42(7):1302–16. https://doi.org/10.1016/j.clinthera.2020.05.008.
Lee CK, Wu YL, Ding PN, Lord SJ, Inoue A, Zhou C, et al. Impact of specific epidermal growth factor receptor (EGFR) mutations and clinical characteristics on outcomes after treatment with EGFR tyrosine kinase inhibitors versus chemotherapy in EGFR-mutant lung cancer: a meta-analysis. J Clin Oncol. 2015;33(17):1958–65. https://doi.org/10.1200/jco.2014.58.1736.
Wu YL, Sequist LV, Geater SL, Orlov S, Lee KH, Tsai CM, et al. 446P Afatinib versus chemotherapy for EGFR mutation-positive NSCLC patients aged ≥65 years: Subgroup analyses of LUX-Lung 3 and LUX-Lung 6. Ann Oncol. 2015;26:i125. https://doi.org/10.1093/annonc/mdv532.30.
Yang JC, Wu YL, Schuler M, Sebastian M, Popat S, Yamamoto N, et al. Afatinib versus cisplatin-based chemotherapy for EGFR mutation-positive lung adenocarcinoma (LUX-Lung 3 and LUX-Lung 6): analysis of overall survival data from two randomised, phase 3 trials. Lancet Oncol. 2015;16(2):141–51. https://doi.org/10.1016/s1470-2045(14)71173-8.
Imai H, Kaira K, Suzuki K, Anzai M, Tsuda T, Ishizuka T, et al. A phase II study of afatinib treatment for elderly patients with previously untreated advanced non-small-cell lung cancer harboring EGFR mutations. Lung Cancer. 2018;126:41–7. https://doi.org/10.1016/j.lungcan.2018.10.014.
Noro R, Igawa S, Bessho A, Hirose T, Shimokawa T, Nakashima M, et al. A prospective, phase II trial of monotherapy with low-dose afatinib for patients with EGFR, mutation-positive, non-small cell lung cancer: thoracic oncology research group 1632. Lung Cancer. 2021;161:49–54. https://doi.org/10.1016/j.lungcan.2021.08.007.
Wu YL, Cheng Y, Zhou X, Lee KH, Nakagawa K, Niho S, et al. Dacomitinib versus gefitinib as first-line treatment for patients with EGFR-mutation-positive non-small-cell lung cancer (ARCHER 1050): a randomised, open-label, phase 3 trial. Lancet Oncol. 2017;18(11):1454–66. https://doi.org/10.1016/s1470-2045(17)30608-3.
Ramalingam SS, Jänne PA, Mok T, O’Byrne K, Boyer MJ, Von Pawel J, et al. Dacomitinib versus erlotinib in patients with advanced-stage, previously treated non-small-cell lung cancer (ARCHER 1009): a randomised, double-blind, phase 3 trial. Lancet Oncol. 2014;15(12):1369–78. https://doi.org/10.1016/s1470-2045(14)70452-8.
Li HS, Zhang JY, Yan X, Xu HY, Hao XZ, Xing PY, et al. A real-world study of dacomitinib in later-line settings for advanced non-small cell lung cancer patients harboring EGFR mutations. Cancer Med. 2022;11(4):1026–36. https://doi.org/10.1002/cam4.4495.
Mok TS, Wu YL, Ahn MJ, Garassino MC, Kim HR, Ramalingam SS, et al. Osimertinib or platinum-pemetrexed in EGFR T790M-positive lung cancer. N Engl J Med. 2017;376(7):629–40. https://doi.org/10.1056/NEJMoa1612674.
Ramalingam SS, Vansteenkiste J, Planchard D, Cho BC, Gray JE, Ohe Y, et al. Overall survival with osimertinib in untreated, EGFR-mutated advanced NSCLC. N Engl J Med. 2020;382(1):41–50. https://doi.org/10.1056/NEJMoa1913662.
Soria JC, Ohe Y, Vansteenkiste J, Reungwetwattana T, Chewaskulyong B, Lee KH, et al. Osimertinib in untreated EGFR-mutated advanced non-small-cell lung cancer. N Engl J Med. 2018;378(2):113–25. https://doi.org/10.1056/NEJMoa1713137.
Wu YL, Tsuboi M, He J, John T, Grohe C, Majem M, et al. Osimertinib in resected EGFR-mutated non-small-cell lung cancer. N Engl J Med. 2020;383(18):1711–23. https://doi.org/10.1056/NEJMoa2027071.
Yamamoto G, Asahina H, Honjo O, Sumi T, Nakamura A, Ito K, et al. First-line osimertinib in elderly patients with epidermal growth factor receptor-mutated advanced non-small cell lung cancer: a retrospective multicenter study (HOT2002). Sci Rep. 2021;11(1):23140. https://doi.org/10.1038/s41598-021-02561-z.
Provencio M, Cheema PK, Vansteenkiste JF, Cho BC, Zhou C, Yu J, et al. ASTRIS global real world study of osimertinib in patients (pts) with EGFR T790M non-small cell lung cancer (NSCLC): subpopulation analyses. Ann Oncol. 2018;29:ix145–6. https://doi.org/10.1093/annonc/mdy446.007.
Nakao A, Hiranuma O, Uchino J, Sakaguchi C, Araya T, Hiraoka N, et al. Final results from a phase II trial of osimertinib for elderly patients with epidermal growth factor receptor t790m-positive non-small cell lung cancer that progressed during previous treatment. J Clin Med. 2020. https://doi.org/10.3390/jcm9061762.
Furuta H, Uemura T, Yoshida T, Kobara M, Yamaguchi T, Watanabe N, et al. Efficacy and safety data of osimertinib in elderly patients with NSCLC who harbor the EGFR T790M mutation after failure of initial EGFR-TKI treatment. Anticancer Res. 2018;38(9):5231–7. https://doi.org/10.21873/anticanres.12847.
Auliac JB, Saboundji K, Andre M, Madelaine J, Quere G, Masson P, et al. Real-life efficacy of osimertinib in pretreated octogenarian patients with T790M-mutated advanced non-small cell lung cancer. Target Oncol. 2019;14(3):307–14. https://doi.org/10.1007/s11523-019-00646-4.
Cho BC, Han JY, Kim SW, Lee KH, Cho EK, Lee YG, et al. A phase 1/2 study of lazertinib 240 mg in patients with advanced EGFR T790M-positive NSCLC after previous EGFR tyrosine kinase inhibitors. J Thorac Oncol. 2022;17(4):558–67. https://doi.org/10.1016/j.jtho.2021.11.025.
Robichaux JP, Le X, Vijayan RSK, Hicks JK, Heeke S, Elamin YY, et al. Structure-based classification predicts drug response in EGFR-mutant NSCLC. Nature. 2021;597(7878):732–7. https://doi.org/10.1038/s41586-021-03898-1.
Burnett H, Emich H, Carroll C, Stapleton N, Mahadevia P, Li T. Epidemiological and clinical burden of EGFR Exon 20 insertion in advanced non-small cell lung cancer: a systematic literature review. PLoS ONE. 2021;16(3):e0247620. https://doi.org/10.1371/journal.pone.0247620.
Yang JC, Schuler M, Popat S, Miura S, Heeke S, Park K, et al. Afatinib for the treatment of NSCLC harboring uncommon EGFR mutations: a database of 693 cases. J Thorac Oncol. 2020;15(5):803–15. https://doi.org/10.1016/j.jtho.2019.12.126.
Piotrowska Z, Wang Y, Sequist LV, Ramalingam SS. ECOG-ACRIN 5162: a phase II study of osimertinib 160 mg in NSCLC with EGFR exon 20 insertions. J Clin Oncol. 2020;38(15 suppl):9513. https://doi.org/10.1200/JCO.2020.38.15_suppl.9513.
Park K, Haura EB, Leighl NB, Mitchell P, Shu CA, Girard N, et al. Amivantamab in EGFR Exon 20 insertion-mutated non-small-cell lung cancer progressing on platinum chemotherapy: initial results from the CHRYSALIS phase I study. J Clin Oncol. 2021;39(30):3391–402. https://doi.org/10.1200/jco.21.00662.
Zhou C, Ramalingam SS, Kim TM, Kim SW, Yang JC, Riely GJ, et al. Treatment outcomes and safety of mobocertinib in platinum-pretreated patients with EGFR Exon 20 insertion-positive metastatic non-small cell lung cancer: a phase 1/2 open-label nonrandomized clinical trial. JAMA Oncol. 2021;7(12):e214761. https://doi.org/10.1001/jamaoncol.2021.4761.
Janning M, Süptitz J, Albers-Leischner C, Delpy P, Tufman A, Velthaus-Rusik JL, et al. Treatment outcome of atypical EGFR mutations in the German National Network Genomic Medicine Lung Cancer (nNGM). Ann Oncol. 2022. https://doi.org/10.1016/j.annonc.2022.02.225.
Cho JH, Lim SH, An HJ, Kim KH, Park KU, Kang EJ, et al. Osimertinib for patients with non-small-cell lung cancer harboring uncommon EGFR mutations: a multicenter, open-label, phase II trial (KCSG-LU15-09). J Clin Oncol. 2020;38(5):488–95. https://doi.org/10.1200/jco.19.00931.
Moran T, Taus A, Arriola E, Aguado C, Dómine M, Rueda AG, et al. Clinical activity of afatinib in patients with non-small-cell lung cancer harboring uncommon EGFR mutations: a spanish retrospective multicenter study. Clin Lung Cancer. 2020;21(5):428-36.e2. https://doi.org/10.1016/j.cllc.2020.04.011.
Lai-Kwon J, Tiu C, Pal A, Khurana S, Minchom A. Moving beyond epidermal growth factor receptor resistance in metastatic non-small cell lung cancer - a drug development perspective. Crit Rev Oncol Hematol. 2021;159:103225. https://doi.org/10.1016/j.critrevonc.2021.103225.
Blakely CM, Watkins TBK, Wu W, Gini B, Chabon JJ, McCoach CE, et al. Evolution and clinical impact of co-occurring genetic alterations in advanced-stage EGFR-mutant lung cancers. Nat Genet. 2017;49(12):1693–704. https://doi.org/10.1038/ng.3990.
Le X, Nilsson M, Goldman J, Reck M, Nakagawa K, Kato T, et al. Dual EGFR-VEGF pathway inhibition: a promising strategy for patients with EGFR-mutant NSCLC. J Thorac Oncol. 2021;16(2):205–15. https://doi.org/10.1016/j.jtho.2020.10.006.
Hosomi Y, Morita S, Sugawara S, Kato T, Fukuhara T, Gemma A, et al. Gefitinib alone versus gefitinib plus chemotherapy for non-small-cell lung cancer with mutated epidermal growth factor receptor: NEJ009 study. J Clin Oncol. 2020;38(2):115–23. https://doi.org/10.1200/jco.19.01488.
Mok TSK, Kim SW, Wu YL, Nakagawa K, Yang JJ, Ahn MJ, et al. Gefitinib plus chemotherapy versus chemotherapy in epidermal growth factor receptor mutation-positive non-small-cell lung cancer resistant to first-line gefitinib (IMPRESS): overall survival and biomarker analyses. J Clin Oncol. 2017;35(36):4027–34. https://doi.org/10.1200/jco.2017.73.9250.
Noronha V, Patil VM, Joshi A, Menon N, Chougule A, Mahajan A, et al. Gefitinib versus gefitinib plus pemetrexed and carboplatin chemotherapy in EGFR-mutated lung cancer. J Clin Oncol. 2020;38(2):124–36. https://doi.org/10.1200/jco.19.01154.
Saito H, Fukuhara T, Furuya N, Watanabe K, Sugawara S, Iwasawa S, et al. Erlotinib plus bevacizumab versus erlotinib alone in patients with EGFR-positive advanced non-squamous non-small-cell lung cancer (NEJ026): interim analysis of an open-label, randomised, multicentre, phase 3 trial. Lancet Oncol. 2019;20(5):625–35. https://doi.org/10.1016/s1470-2045(19)30035-x.
Stinchcombe TE, Jänne PA, Wang X, Bertino EM, Weiss J, Bazhenova L, et al. Effect of erlotinib plus bevacizumab vs erlotinib alone on progression-free survival in patients with advanced EGFR-mutant non-small cell lung cancer: a phase 2 randomized clinical trial. JAMA Oncol. 2019;5(10):1448–55. https://doi.org/10.1001/jamaoncol.2019.1847.
Yamamoto N, Seto T, Nishio M, Goto K, Yamamoto N, Okamoto I, et al. Erlotinib plus bevacizumab vs erlotinib monotherapy as first-line treatment for advanced EGFR mutation-positive non-squamous non-small-cell lung cancer: survival follow-up results of the randomized JO25567 study. Lung Cancer. 2021;151:20–4. https://doi.org/10.1016/j.lungcan.2020.11.020.
Nakagawa K, Garon EB, Seto T, Nishio M, Ponce Aix S, Paz-Ares L, et al. Ramucirumab plus erlotinib in patients with untreated, EGFR-mutated, advanced non-small-cell lung cancer (RELAY): a randomised, double-blind, placebo-controlled, phase 3 trial. Lancet Oncol. 2019;20(12):1655–69. https://doi.org/10.1016/s1470-2045(19)30634-5.
Nadal E, Horinouchi H, Shih JY, Nakagawa K, Reck M, Garon EB, et al. RELAY, ramucirumab plus erlotinib versus placebo plus erlotinib in patients with untreated, epidermal growth factor receptor mutation-positive, metastatic non-small-cell lung cancer: safety profile and manageability. Drug Saf. 2022;45(1):45–64. https://doi.org/10.1007/s40264-021-01127-2.
Pallis AG, Gridelli C, Wedding U, Faivre-Finn C, Veronesi G, Jaklitsch M, et al. Management of elderly patients with NSCLC; updated expert’s opinion paper: EORTC Elderly Task Force, Lung Cancer Group and International Society for Geriatric Oncology. Ann Oncol. 2014;25(7):1270–83. https://doi.org/10.1093/annonc/mdu022.
Kalemkerian GP, Narula N, Kennedy EB, Biermann WA, Donington J, Leighl NB, et al. Molecular testing guideline for the selection of patients with lung cancer for treatment with targeted tyrosine kinase inhibitors: American Society of Clinical Oncology Endorsement of the College of American Pathologists/International Association for the Study of Lung Cancer/Association for Molecular Pathology Clinical Practice Guideline Update. J Clin Oncol. 2018;36(9):911–9. https://doi.org/10.1200/jco.2017.76.7293.
Mosele F, Remon J, Mateo J, Westphalen CB, Barlesi F, Lolkema MP, et al. Recommendations for the use of next-generation sequencing (NGS) for patients with metastatic cancers: a report from the ESMO Precision Medicine Working Group. Ann Oncol. 2020;31(11):1491–505. https://doi.org/10.1016/j.annonc.2020.07.014.
Rolfo C, Mack P, Scagliotti GV, Aggarwal C, Arcila ME, Barlesi F, et al. Liquid biopsy for advanced NSCLC: a consensus statement from the international association for the study of lung cancer. J Thorac Oncol. 2021;16(10):1647–62. https://doi.org/10.1016/j.jtho.2021.06.017.
Roviello G, Zanotti L, Cappelletti MR, Gobbi A, Dester M, Paganini G, et al. Are EGFR tyrosine kinase inhibitors effective in elderly patients with EGFR-mutated non-small cell lung cancer? Clin Exp Med. 2018;18(1):15–20. https://doi.org/10.1007/s10238-017-0460-7.
Acknowledgements
The authors are grateful for the editorial assistance of Marta Bosch of HealthCo Trials (Madrid, Spain) in the drafting of this manuscript.
Funding
SEOM, GECP and ICAPEM acknowledge the financial support for this project in the form of unrestricted collaboration in the logistics from AstraZeneca.
Author information
Authors and Affiliations
Contributions
All authors contributed to the study conception and design. All authors participated in the writing of the first draft of the manuscript, commented on following draft versions and approved the final version of the manuscript.
Corresponding author
Ethics declarations
Conflict of interest
The authors declare that, when writing and revising the text, they did not know the names of the pharmaceutical companies that provided financial support for this project, so this support has not influenced the content of this article.
Ethical approval
Not applicable.
Consent to participate
Not applicable.
Consent for publication
Not applicable.
Additional information
Publisher's Note
Springer Nature remains neutral with regard to jurisdictional claims in published maps and institutional affiliations.
Rights and permissions
Open Access This article is licensed under a Creative Commons Attribution 4.0 International License, which permits use, sharing, adaptation, distribution and reproduction in any medium or format, as long as you give appropriate credit to the original author(s) and the source, provide a link to the Creative Commons licence, and indicate if changes were made. The images or other third party material in this article are included in the article's Creative Commons licence, unless indicated otherwise in a credit line to the material. If material is not included in the article's Creative Commons licence and your intended use is not permitted by statutory regulation or exceeds the permitted use, you will need to obtain permission directly from the copyright holder. To view a copy of this licence, visit http://creativecommons.org/licenses/by/4.0/.
About this article
Cite this article
Nadal, E., Oré-Arce, M., Remon, J. et al. Expert consensus to optimize the management of older adult patients with advanced EGFR-mutated non-small cell lung cancer. Clin Transl Oncol 25, 3139–3151 (2023). https://doi.org/10.1007/s12094-023-03286-3
Received:
Accepted:
Published:
Issue Date:
DOI: https://doi.org/10.1007/s12094-023-03286-3