Abstract
Objective
To investigate the impact of discontinuation of mechanical bowel preparation in advanced ovarian cancer surgery within the context of the ERAS program.
Methods
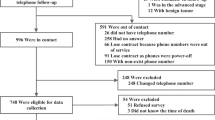
We retrospectively reviewed the medical records of patients with advanced ovarian cancer who underwent cytoreductive surgery with simultaneous colon and/or rectal resection from January 2012 to November 2020. Patients were divided into two groups based on whether preoperative mechanical bowel preparation (MBP) was given (pre-ERAS) or not (post-ERAS). Patient characteristics, including duration of antibiotic treatment, surgical complexity, and incidence of surgical and nonsurgical complications, were compared.
Results
During the study period, 114 patients who underwent colon and/or rectal resection were examined, of whom 39 received MBP and 75 did not receive MBP (NMBP). On comparison between the two groups, no significant differences were noted in the assessed patient characteristics, including mean age, FIGO stage, ASA class, BMI, or residual tumor. One patient (2.6%) in the MBP group, and 4 patients (5.3%) in the NMBP group experienced an anastomotic leakage (p = 0.11). No significant differences were found with respect to surgical site infection. (p = 0.5).
Conclusion
MBP was not associated with any specific benefit for advanced ovarian cancer surgery. Gynecologic oncologists who use MBP should consider discontinuing this practice.

Similar content being viewed by others
References
Siegel RL, Miller KD, Jemal A. Cancer statistics, 2020. CA Cancer J Clin. 2020;70:7–30.
Du Bois A, Reuss A, Pujade-Lauraine E, Harter P, Ray-Coquard I, Pfisterer J, et al. Role of surgical outcome as prognostic factor in advanced epithelial ovarian cancer: a combined exploratory analysis of 3 prospectivelyrandomized phase 3 multicenter trials: by the Arbeitsgemeinschaft Gynaekologische Onkologie Studiengruppe Ovarialkarzinom (AGO-OVAR) and the Groupe d’Investigateurs Nationaux Pour les Etudes des Cancers de l’Ovaire (GINECO). Cancer. 2009;115:1234–44.
Chang S-J, Hodeib M, Chang J, Bristow RE. Survival impact of complete cytoreduction to no gross residual disease for advanced-stageovarian cancer: a meta-analysis. Gynecol Oncol. 2013;130:493–8.
Tseng JH, Cowan RA, Zhou Q, Iasonos A, Byrnee M, Polcino T, et al. Continuous improvement in primary Debulking surgery for advanced ovarian cancer: do increased complete gross resection rates independently lead to increased progression-free and overall survival? Gynecol Oncol. 2018;151(1):24–31.
Gustafsson UO, Scott MJ, Hubner M, Nygren J, Demartines N, Francis N, et al. Guidelines for perioperative care in elective colorectal surgery: enhanced recovery after surgery (ERAS®) society recommendations: 2018. World J Surg. 2019;43(3):659–95.
Nelson G, Bakkum-Gamez J, Kalogera E, Glaser Alon Altman G, Meyer AL, et al. Guidelines for perioperative care in gynecologic/oncology: enhanced recovery after surgery (ERAS) society recommendation 2019 update. Int J Gynecol Cancer. 2019;29(4):651–68.
Bhandoria GP, Bhandarkar P, Ahuja V, Maheshwari A, Sekhon RK, Gultekin M, et al. Enhanced recovery after surgery (ERAS) in gynecologic oncology: an international survey of peri-operative practice. Int J Gynecol Cancer. 2020;30(10):1471–8.
Sanchez-Iglesias JL, Carbonell-Socias M, Assumpcio Perez-Benavente MA, Clua SM, Manrique-Muñoz S, Gorriz MG, et al. PROFAST: a randomised trial implementing enhanced recovery after surgery for highcomplexity advanced ovarian cancer surgery. Eur J Cancer. 2020;136:149–58.
Dindo D, Demartines N, Clavien P-A. Classification of surgical complications: a new proposal with evaluation in a cohort of 6336 patients and results of a survey. Ann Surg. 2004;240(2):205–13.
Horan TC, Gaynes RP, Martone WJ, Jarvis WR, Emori TG, et al. CDC definitions of nosocomial surgical site infections, 1992: a modification of CDC definitions of surgical wound infections. Infect Control Hosp Epidemiol. 1992;13:606–8.
Tamussino KF, Lim PC, Webb MJ, Lee RA, Lesnick TG. Gastrointestinal surgery in patients with ovarian cancer. Gynecol Oncol. 2001;80(1):79–84. https://doi.org/10.1006/gyno.2000.6037.
Stefanović A, Jeremić K, Kadija S, Milincić N, Mircić A, Petković S, et al. Intestinal surgery in treatment of advanced ovarian cancer–review of our experience. Eur J Gynaecol Oncol. 2011;32(4):419–22.
Paladini D, Fontanelli R, Raspagliesi F, Ntousias V. Intestinal operations during surgical procedures for epithelial ovarian cancer. Int J Gynecol Cancer. 1994;4:320–3.
Smith ST, Seski JC, Copeland LJ, Gershenson DM, Edwards CL, Herson J. Surgical management of irradiation-induced small bowel damage. Obstet Gynecol. 1985;65:563–7.
Lippitt MH, Fairbairn MG, Matsuno R, Stone RL, Tanner EJ 3rd, Wick EC, et al. Outcomes associated with a five-point surgical site infection prevention bundle in women undergoing surgery for ovarian cancer. Obstet Gynecol. 2017;130(4):756–64.
Lindemann K, Kok PS, Stockler M, Sykes P, Brand A. Enhanced recovery after surgery for suspected ovarian malignancy: a survey of perioperative practice among gynecologic oncologists in Australia and New Zealand to inform a clinical trial. Int J Gynecol Cancer. 2017;27(5):1046–50.
Cao F, Li J, Li F. Mechanical bowel preparation for elective colorectal surgery: updated systematic review and meta-analysis. Int J Colorectal Dis. 2012;27:803–10.
Dahabreh IJ, Steele DW, Shah N, et al. Oral mechanical bowel preparation for colorectal surgery: systematic review and metaanalysis. Dis Colon Rectum. 2015;58:698–707.
Pineda CE, Shelton AA, Hernandez-Boussard T, et al. Mechanical bowel preparation in intestinal surgery: a meta-analysis and review of the literature. J Gastrointest Surg. 2008;12:2037–44.
Slim K, Vicaut E, Launay-Savary M-V, et al. Updated systematic review and meta-analysis of randomized clinical trials on the role of mechanical bowel preparation before colorectal surgery. Ann Surg. 2009;249:203–9.
Rollins KE, Javanmard-Emamghissi H, Lobo DN. Impact of mechanical bowel preparation in elective colorectal surgery: a meta-analysis. World J Gastroenterol. 2018;24(4):519–36.
Koskenvuo L, Lehtonen T, Koskensalo S, Rasilainen S, Klintrup K, Ehrlich A, et al. Mechanical and oral antibiotic bowel preparation versus no bowel preparation for elective colectomy (MOBILE):a multicentre, randomised, parallel, single-blinded trial. Lancet. 2019;394:840–8.
Espin Basany E, Solís-Peña A, Pellino G, Kreisler E, Fraccalvieri D, Muinelo-Lorenzo M, et al. Preoperative oral antibiotics and surgical-site infections incolon surgery ORALEV): a multicentre, single-blind, pragmatic, randomised controlled trial. Lancet Gastroenterol Hepatol. 2020;5(8):729–38.
Golder AM, Steele CW, Conn D, MacKay JG, McMillan DC, Horgan PG, et al. Effect of preoperative oral antibiotics in combination with mechanical bowel preparation on inflammatory response andshort-term outcomes following left-sided colonic andrectal resections. BJS Open. 2019;3:830–9.
Liu WT, Hsiao CW, Jao SW, Yu MH, Wu GJ, Liu JY, et al. Is preoperative bowel preparation necessary for gynecological oncology surgery? Taiwan J Obstet Gynecol. 2016;55:198–201.
European Society of Coloproctology (ESCP) collaborating group. Association of mechanical bowel preparation with oral antibiotics and anastomotic leak following left sided colorectal resection: an international, multi-centre, prospective audit. Colorectal Dis. 2018;20(Suppl 6):15–32.
Iniesta MD, Lasala J, Mena G, Rodriguez-Restrepo A, Salvo G, et al. Impact of compliance with an enhanced recovery after surgery pathway on patient outcomes in open gynecologic surgery. Int J Gynecol Cancer. 2019;29(9):1417–24.
Sánchez-Iglesias JL, Gómez-Hidalgo NR, Pérez- Benavente A, Carbonell-Socias M, Manrique-Muñoz S, Pamies Serrano M, et al. Importance of enhanced recovery after surgery (ERAS) protocol compliance on length of stay in ovarian cancer surgery. Annals of Surg Oncol. 2021;28:8979–86.
Ciccone MM, Aquilino A, Cortese F, Scicchitano P, Sassara M, et al. Feasibility and effectiveness of a disease and care management model in the primary health care system for patients with heart failure and diabetes (Project Leonardo). Vasc Health Risk Manag. 2010;6:297–305.
Acknowledgements
We would like to thank Drs. Cristina Centeno Mediavilla, Silvia Cabrera Díaz and Melissa Bradbury (Gynecologic Oncology Department, Vall d´Hebron Hospital, Barcelona) for valuable collaboration and support within the working group.
Funding
No sources of funding were used.
Author information
Authors and Affiliations
Contributions
Conception and design of study: JLSI, NRGH, VBC, AGM. Data collection: JLSI. Data analysis and interpretation: JLSI, NRGH, VBC. Statistical analysis: VBC. Manuscript preparation: NRGH, JLSI, VBC, APB, GN, AGM, JMR. *Jose Luis Sánchez-Iglesias (JLSI), Asunción Pérez-Benavente (APB), Antonio Gil-Moreno (AGM), Natalia R. Gómez-Hidalgo (NRGH), Vicente Bebia Conesa (VBC), Jose Manuel Ramirez (JMR), Gregg Nelson (GN).
Corresponding author
Ethics declarations
Conflict of interest
The Authors declare no financial conflicts of interest. Dr. Nelson reports speaker/advisory fees from Abbott, GSK, 3M and is the Secretary of the ERAS Society. Dr. Ramirez reports speaker/advisory fees from Vegenat, Vifor, Takeda, MSD, Menarini, BD and is the former president of the Spanish ERAS Society (GERM).
Compliance with ethics requirements
This study was carried out in the Unit of Gynecology Oncology at the Vall d’Hebron Hospital Campus in Barcelona, Spain.
Informed consent
The medical records of all patients who underwent cytoreductive surgery for advanced ovarian cancer with simultaneous colon or rectal resection from January 2012 to November 2020 were included.
Additional information
Publisher's Note
Springer Nature remains neutral with regard to jurisdictional claims in published maps and institutional affiliations.
Rights and permissions
Springer Nature or its licensor holds exclusive rights to this article under a publishing agreement with the author(s) or other rightsholder(s); author self-archiving of the accepted manuscript version of this article is solely governed by the terms of such publishing agreement and applicable law.
About this article
Cite this article
Sánchez-Iglesias, J.L., Gómez-Hidalgo, N.R., Bebia, V. et al. Discontinuation of mechanical bowel preparation in advanced ovarian cancer surgery: an enhanced recovery after surgery (ERAS) initiative. Clin Transl Oncol 25, 236–242 (2023). https://doi.org/10.1007/s12094-022-02934-4
Received:
Accepted:
Published:
Issue Date:
DOI: https://doi.org/10.1007/s12094-022-02934-4