Abstract
Purpose
Considering the increased cancer patient survivorship, the focus is now on addressing the impacts of treatment on quality of life. In young people, altered reproductive function is a major issue and its effects in young males are largely neglected by novel research. To improve clinician awareness, we systematically reviewed side effects of chemotherapy for Hodgkin lymphoma (HL) in young males.
Methods
The review was prospectively registered (PROSPERO N. CRD42019122868). Three databases (Medline via PUBMED, SCOPUS, and Cochrane Library) were searched for studies featuring males aged 13-51-years who underwent chemotherapy for HL using ABVD (Adriamycin® (doxorubicin), bleomycin, vinblastine, and dacarbazine) or BEACOPP (bleomycin, etoposide, doxorubicin, cyclophosphamide, vincristine, procarbazine, and prednisolone) regimens. These chemotherapy regimens were compared against each other using sperm characteristics, FSH, and inhibin B levels to measure fertility levels.
Results
Data were extracted from five studies featuring 1344 patients. 6 months post-ABVD saw marked deterioration in sperm count, further reduced by more cycles (P = 0.05). Patients treated with BEACOPP rather than ABVD were more prone to oligospermia. Receiving fewer cycles of both regimens increased the likelihood of sperm production recovering. Patients treated with 6-8 cycles of BEACOPP did not recover spermiogenesis.
Conclusions
ABVD and BEACOPP regimens significantly reduce fertility function to varying effects depending on treatment duration. ABVD temporarily causes significant reductions in male fertility, whereas BEACOPP’s effects are more permanent. Therefore, clinicians should discuss fertility preservation with male patients receiving infertility-inducing gonadotoxic therapy. Further high-quality studies are required to more adequality describe the risk to fertility by chemotherapy.
Similar content being viewed by others
Avoid common mistakes on your manuscript.
Introduction
Anticancer treatment has become increasingly effective, with strategies possessing high survival rates of around 90% [1, 2]. However, as survivorship improves, the focus has shifted to the impact of treatment on patients’ quality of life with infertility status being one prominent example [1,2,3,4]. This is especially relevant in young people where haematological cancers are the most diagnosed malignancies. Reduction in fertility is experienced in 80% of lymphoma patients further emphasized by 20–25% of females encountering difficulties in achieving successful pregnancy [1, 5,6,7].
These side effects arise largely due to the use of alkylating agent-based chemotherapies, which indiscriminately target the hypothalamic–pituitary–adrenal axis and the gonads. In males, this results in azoospermia, sexual dysfunction, infertility, and associated psychological issues [2, 5, 8,9,10,11,12].
Whilst extensive research has been performed on females in this field, few robust studies exist for males. In response to a recent Cochrane review calling for discussion of treatment-related infertility in males with Hodgkin lymphoma (HL) [13] our study aims to (1) systematically review the literature on effects of anticancer therapy on the fertility of males with HL, (2) identify potential strategies to preserve reproductive function.
Methods
This systematic review was designed according to the PRISMA Checklist 2009 and prospectively registered via the PROSPERO database, registration number: CRD42019122868 [14].
Study eligibility criteria
Randomised-control trials, non-randomised studies of interventions, and other observational studies which included males diagnosed with Hodgkin’s lymphoma between the ages 13 and 51 who received anticancer treatment were included in this review. This age range was estimated to be when males are most fertile, between puberty onset and elderly decline in fertility [15,16,17]. Only studies using ABVD (Adriamycin® (doxorubicin), bleomycin, vinblastine, dacarbazine) or BEACOPP (bleomycin, etoposide, doxorubicin, cyclophosphamide, vincristine, procarbazine, prednisolone) regimens were included as these regimens are the most common and effective treatments for HL [18, 19]. Studies of mixed patients which did not distinguish demographics, interventions, or without pre-treatment and post-treatment data were excluded. Additional exclusion criteria were studies published before January 2000, not written in English, conference abstracts, reviews, editorials, case reports or series.
Information sources and search
Three databases were searched; MEDLINE via PubMed, Scopus and Cochrane Library up to 27 May 2020, filtering for human studies, written in English and published after 01/01/2000. A combination of search terms and keywords was utilised with variations in spelling also considered. Key words used were “MALE”, “HODGKIN LYMPHOMA” “LYMPHOMA”, “FERTILITY”, “INFERTILITY”, “TREATMENT”, in combinations using Boolean operators (Appendix A). ClinicalTrials.gov and the ISRCTN registry were searched for ongoing clinical trials with authors contacted for unpublished results.
Study selection
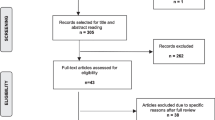
Selection of studies was carried out independently by two reviewers (MSAA and CS). Following deduplication, titles and abstracts were screened and potentially relevant articles selected for full-text retrieval. Reasons were stated for excluding articles after full-text review. Discrepancies between authors were reviewed by a third author (OB) until 100% agreement was achieved.
Data collection and data items
Data extraction was performed independently by MSAA and CS, again with OB reviewing any inconsistencies. Study characteristics extracted included, author, year, population description, number of participants, study aim, design, treatments received, and author conclusions.
Primary outcomes extracted were measures assessing the chemotherapy-induced changes to fertility. This was measured using sperm count, spermatogenesis, sperm motility and changes to gonadal function reflected by concentrations of sex hormones (follicle stimulating hormone (FSH), luteinizing hormone (LH), Inhibin B, and testosterone). Secondary outcomes for this review were methods for fertility preservation using identical measures to our primary outcome to assess their effectiveness.
Risk of bias assessment
All selected studies were critically appraised for risk of bias by two authors (MSAA and CS). As no RCTs were identified the ‘Risk Of Bias In Non-randomized Studies of Interventions’ (ROBINS-I) tool was utilised [20]. Studies which scored an overall rating of “CRITICAL” were not taken forward for data extraction or discussion.
Results
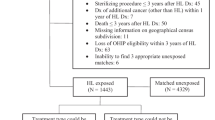
Study selection and risk of bias
Initial searches yielded 636 articles, with 354 remaining post deduplication (Fig. 1). After title and abstract screening 15 articles were reviewed in full of which 7 were selected for critical appraisal using the ROBINs-I test (Appendix B). All studies scored ‘moderate’ for risk of bias in measurement outcomes due to a lack of blinding between patient groups and assessors. Two studies scored ‘critical’ for overall risk study bias and were excluded [21, 22] leaving 5 with a ‘low’ score and therefore suitable for final inclusion and data analysis (Table 1) [4, 23,24,25,26].
Study characteristics
Together, the 5 studies discussed 1344 males with HL and comprised of 1 retrospective cohort [26] and four prospective cohort studies [4, 23,24,25] (Table 2). All studies discussed chemotherapy for HL with four featuring ABVD [4, 23, 25, 26], two featuring BEACOPP [4, 24], and three featuring escBEACOPP [4, 24, 26]. Three studies measured semen characteristics and FSH levels [23,24,25], two studies measured only semen characteristics [25, 26] and one study used Inhibin B/FSH ratios [4].
Changes to sperm count
Pre-treatment sperm count was higher in early stage disease when compared to late stage but was still in normal ranges [23, 26]. Subsequent changes to these pre-treatment values were verified by interval or regression analysis to be strictly due to treatment used and not age or disease stage (P = 0·05) [4, 23, 26]. However, one study observed no difference in pre-treatment sperm quality between HL or control group patients [25].
At 6 months post-ABVD, 38% of patients had oligospermia, with a further 40% having azoospermia [25]. 6–8 cycles of ABVD lowered sperm count more than 2–4 cycles (P = 0·05) [26]. ABVD combined with radiotherapy, either inguinal sparing or inguinal involved field caused patients to become oligospermic or azoospermic, respectively at 6 months [26]. A minority of patients who had received inguinal radiotherapy recovered spermiogenesis but sperm quality was severely impaired [26]. Inguinal-sparing radiotherapy maintained oligospermia in patients at 12 months post-treatment (P = 0·01) [26]. By 12–18 months, 50% of patients treated with ABVD had recovered normal sperm characteristics [4] which rose to 57% at 24 months with Paoli et al. observing normospermia by 24 months [25, 26].
Paoli et al. [26] reported three patients who underwent 2–4 cycles of BEACOPP recovered sperm function by 4 years post-treatment, whereas 13 patients who received 6–8 cycles BEACOPP did not. Behringer et al. [4] also observed that patients who had 6–8 cycles of BEACOPP did not recover spermiogenesis.
There were no statistical differences in fertility rates between males treated with BEACOPP or escBEACOPP regimen (P > 0·999) with 89% becoming azoospermic and 11% dyspermic [24]. Only 4% of dyspermic patients recovered spermatogenesis with timing varying from 1.5–6.7 years post-therapy [24].
Patients treated with BEACOPP were more likely to have oligospermia than those treated with ABVD [4]. As such, patients with early stage HL were significantly more likely to have children born via natural methods due to the more gonadotoxic treatment used for advanced stage disease [4].
Changes to sperm morphology
At 6 months, patients treated with both ABVD and inguinal-sparing radiotherapy had significantly decreased sperm motility (P = 0.001) and significant changes to sperm morphology (P = 0.01) when compared to pre-treatment values [26]. O’Flaherty et al. [25] also recorded a decrease in the proportion of sperm demonstrating normal physiology at 6 months in patients treated solely with ABVD.
Changes to sex hormones
Pre-treatment values of serum testosterone and FSH gave no indication of post-therapy azoospermia (P > 0.05) [23]. Pre-treatment Inhibin B/FSH ratios were closer to fertile levels in early stage rather than late stage disease [4]. FSH was raised at 6 and 12 months post-ABVD treatment compared to healthy controls (P = 0.008) before returning to normal [4, 23, 25]. Treatment using BEACOPP (6–8 cycles) resulted in lower Inhibin B/FSH ratios corresponding to levels of impaired fertility (P < 0.001) [4]. LH and testosterone did not significantly change before and after treatment with ABVD (P = 0.203, P = 0.844, respectively) [23].
Fertility preservation
None of the studies addressed fertility preservation methods for patients with HL so data on successful pregnancies was not extracted. However, it was reported that natural conception of offspring post-treatment was more likely in patients with early stage disease than advanced (P = 0.04) [4].
Discussion
Fertility risk is important to young adult male patients, yet clinicians are uncomfortable with discussing this issue as they are ill-informed to side effects of anticancer treatment [2, 8, 27, 28]. Consequently, patients are unable to make informed treatment decisions surrounding their fertility and potential reproductive function post-treatment. The ensuing inability to conceive can result in anxiety and depression for patients [28]. Experts recommend that patients wishing to preserve fertility be referred to specialists [11] or be informed of preservation methods before commencing treatment [4]. However, it has been reported that more than 50% of oncologists do not refer their young adult patients for fertility preservation, going against the American Society of Clinical Oncology (ASCO) guidelines [27]. Raising awareness of side effects of anticancer treatment to male fertility may promote referral to underutilised fertility preservation services [8, 11]. This review highlights the high impact of ABVD and BEACOPP chemotherapy on fertility in males with Hodgkin lymphoma, and thereby the need for utilisation of these services.
ABVD is used in patients with early and advanced stage HL [18, 29]. In patients who took ABVD, normal reproductive function returned between 12 months and 2 years post-treatment as reflected by rises in sperm count and serum FSH levels. Furthermore, increased number of ABVD cycles from 2–4 to 6–8 is associated with marked reductions to sperm count, delaying and reducing recovery of reproductive function and more unlikely to regain normospermia. This demonstrates that longer exposure to gonadotoxic material has an incremental impact on fertility. Patients who received ABVD alongside inguinal sparing radiotherapy recovered normospermia by 2 years post-remission. On the other hand, patients who received ABVD but with inguinal radiotherapy took up 5 years to recover spermiogenesis while sperm motility and morphology remained impaired. As lymphoma management may use variations of adjuvant radiotherapy e.g. inguinal or inguinal sparring [5], the associated risks to quality of life should be discussed with the patient.
The BEACOPP regimen is used for the treatment of advanced stage HL [18]. However, despite having a better progression-free survival rate than ABVD, the presence of enhanced alkylating agents makes it more gonadotoxic than ABVD increasing the risk of oligospermia and resultant lower quality of life [2, 4, 5, 10, 30]. Similarly, to the increased cycles of ABVD, 6–8 cycles of BEACOPP resulted in no recovery of reproductive function, whereas it did return 3–4 years post-treatment when 2–4 cycles were used. Ultimately, BEACOPP results in great damage to spermiogenesis, with most patients never recovering function.
As serum FSH levels mirrored changes to sperm count, serum FSH may have potential as a convenient early marker of post-treatment fertility. Changes to other sex hormones were not reflective of altered gonadal function.
The secondary outcome was to evaluate effective methods of fertility preservation. No methods were identified yet it remains an important factor for discussion. Recommendations for fertility preservation by the American Society of Clinical Oncology (ASCO) and the European Society of Medical Oncology (ESMO) include sperm cryopreservation which can be used for intrauterine insemination [11, 28]. Other artificial reproduction technologies include gonadal stem cell transplants and testicular tissue preservation, but as they are untested, sperm cryopreservation remains the best option for sperm-producing males [3, 31,32,33]. However, only a few studies identify the effectiveness of this method in producing children, but this may be due to patients being of a young age, having no plans for offspring, or lost to follow-up [3].
One study not included in the review found microsurgical testicular sperm extraction (TESE) beneficial in retrieving sperm from young males with leukaemia and Hodgkin lymphoma who did not cryopreserve their sperm prior to treatment identifying its clinical potential [34]. Guidance from the American Society for Reproductive Medicine (ASRM) advocates TESE usage in oligo- or azoospermic males [3, 33, 35]. However, evidence not included in the guidance suggests waiting 18–24 months post-therapy to allow for the testes to be cleared of damaged germ cells before seeking artificial reproductive methods [31, 36]. Despite lacking a high-quality evidence for TESE in post-treatment fertility preservation, we have used the guidance from these leading clinical societies and the methods used for other cancers, to suggest fertility management strategies for Hodgkin lymphoma patients if sperm cryopreservation fails (Fig. 2).
This review has served to identify the impacts of treatments of common haematological malignancy treatment for young males where gaps in the literature exist. The review’s primary strength was the robust methodology including only relevant content, with a low risk of bias as identified by the ROBINS-I score. The large populations and homogenous results allowed for study comparison and development of common conclusion. However, as with any review, there are limitations. First, the review was limited by the relatively small number of articles included. Moreover, whilst articles included had similar aims in observing sperm characteristics, there was heterogeneity in exact measures recorded. Studies which measured the same outcomes observed different exact treatments or released raw data from incomparable categories, thereby preventing any meaningful meta-analysis from being conducted. Furthermore, due to human error there is always the risk of relevant studies being missed during the literature search; however, we aimed to minimise this by our comprehensive methodology using independent reviewers. Finally, there is a limitation within the overall level of evidence included as no randomised studies were suitable for inclusion.
To address the limitations of the review and of the literature, high-quality randomised controlled trials are certainly required to further define the fertility implications of cancer treatment in Hodgkin lymphoma. Treatment regimens must be precisely documented with outcomes measuring pre-treatment fertility markers such as sperm count, sperm motility, and FSH levels. Subsequent samples should be taken at 0, 6, 12, 18, and 24 months post-treatment for comparison with significant endpoints such as pregnancy rates also accommodated for.
Conclusion
The literature review demonstrates that ABVD and BEACOPP treatments are gonadotoxic in males with Hodgkin lymphoma. Strong evidence suggests that ABVD is the less gonadotoxic option of the two regimens and prolonged treatment cycles lead to greater gonadal insult culminating in permanent infertility. Therefore, clinicians ought to adequately discuss fertility risk and management options with patients prior to commencing these treatments and potentially other alkylating agent-based regimens. Future clinical practice may involve modifications to established regimens as it has been suggested that this may reduce therapy side effects [37]. One example of a modification is BEACOPP being changed to BEACOP-Dac where dacarbazine replaces procarbazine. This novel de-escalation therapy aims to be less sterilising by giving fewer courses of chemotherapy to patients who achieve complete response to the original regimen, thereby reducing the side effects to fertility. However, this is yet to be evaluated. At present, only limited evidence exists for fertility preservation options pre- and post- treatment. However, we have extrapolated methods from study designs to recommend a research pathway for future studies to effectively focus on clinically important outcomes including side-effects of treatments and effective methods for fertility preservation (Fig. 3). In the absence of these studies, the conclusions of this review regarding HL treatment may be used as a basis for future fertility preservation in young males treated for other forms of cancer.
References
Miller KD, et al. Cancer treatment and survivorship statistics, 2016. CA Cancer J Clin. 2016;66(4):271–89.
Harel S, Fermé C, Poirot C. Management of fertility in patients treated for Hodgkin's lymphoma. Haematologica. 2011;96(11):1692–9.
Fu L, et al. Sperm cryopreservation for male cancer patients: more than 10 years of experience, in Beijing China. Med Sci Monit. 2019;25:3256–61.
Behringer K, et al. Gonadal function and fertility in survivors after Hodgkin lymphoma treatment within the German Hodgkin Study Group HD13 to HD15 trials. J Clin Oncol. 2013;31(2):231–9.
Colpi GM, et al. Testicular function following chemo-radiotherapy. Eur J Obstet Gynecol Reprod Biol. 2004;113(SUPPL.):S2–S6.
Patterson P, et al. Emerging issues among adolescent and young adult cancer survivors. Semin Oncol Nurs. 2015;31(1):53–9.
Kamimura K, et al. Cancers among adolescents and young adults at one institution in Japan. Oncol Lett. 2018;16(6):7212–22.
Docherty SL, et al. The adolescent and young adult with cancer: a developmental life course perspective. Semin Oncol Nurs. 2015;31(3):186–96.
Jacobs LA, Pucci DA. Adult survivors of childhood cancer: the medical and psychosocial late effects of cancer treatment and the impact on sexual and reproductive health. J Sexual Med. 2013;10(SUPPL.):120–6.
Traila A, et al. Fertility preservation in Hodgkin's lymphoma patients that undergo targeted molecular therapies: an important step forward from the chemotherapy era. Cancer Manag Res. 2018;10:1517–26.
Lambertini M, et al. Cancer and fertility preservation: international recommendations from an expert meeting. BMC Med. 2016;14:1–1.
Armitage JO, et al. Non-hodgkin lymphoma. Lancet. 2017;390(10091):298–310.
Skoetz N, et al. Comparison of first-line chemotherapy including escalated BEACOPP versus chemotherapy including ABVD for people with early unfavourable or advanced stage Hodgkin lymphoma. Cochrane Database Syst Rev. 2017;5:CD007941.
Moher D, Liberati A, Tetzlaff J, Altman DG. Preferred reporting items for systematic reviews and meta-analyses: the PRISMA statement. PLoS Med. 2009;6(7):e1000097.
Handelsman DJ. Sex differences in athletic performance emerge coinciding with the onset of male puberty. Clin Endocrinol (Oxf). 2017;87(1):68–72.
Khera M. Male hormones and men's quality of life. Curr Opin Urol. 2016;26(2):152–7.
eaVuichoud C, Loughlin KR. Benign prostatic hyperplasia: epidemiology, economics and evaluation. Can J Urol. 2015;22(Suppl 1):1–6.
Dann EJ, et al. Modification of initial therapy in early and advanced Hodgkin lymphoma, based on interim PET/CT is beneficial: a prospective multicentre trial of 355 patients. Br J Haematol. 2017;178(5):709–18.
Bröckelmann PJ, et al. Patient and physician preferences for first-line treatment of classical Hodgkin lymphoma in Germany, France and the United Kingdom. Br J Haematol. 2019;184(2):202–14.
Sterne JAC, HM, Reeves BC, Savović J, Berkman ND, Viswanathan M, Henry D, Altman DG, Ansari MT, Boutron I, Carpenter JR, Chan AW, Churchill R, Deeks JJ, Hróbjartsson A, Kirkham J, Jüni P, Loke YK, Pigott TD, Ramsay CR, Regidor D, Rothstein HR, Sandhu L, Santaguida PL, Schünemann HJ, Shea B, Shrier I, Tugwell P, Turner L, Valentine JC, Waddington H, Waters E, Wells GA, Whiting PF. ROBINS.
Boltezar L, Pintaric K, Jezersek Novakovic B. Fertility in young patients following treatment for Hodgkin's lymphoma: a single center survey. J Assist Reprod Genet. 2016;33(3):325–33.
Van der Kaaij MAE, et al. Gonadal function in males after chemotherapy for early-stage Hodgkin's lymphoma treated in four subsequent trials by the European Organisation for Research and Treatment of Cancer: EORTC Lymphoma Group and the Groupe d'Étude des Lymphomes de l'Adulte. J Clin Oncol. 2007;25(19):2825–32.
Tal R, et al. Follow-up of sperm concentration and motility in patients with lymphoma. Hum Reprod. 2000;15(9):1985–8.
Sieniawski M, et al. Fertility in male patients with advanced Hodgkin lymphoma treated with BEACOPP: a report of the German Hodgkin Study Group (GHSG). Blood. 2008;111(1):71–6.
O'Flaherty C, et al. Impact of chemotherapeutics and advanced testicular cancer or Hodgkin lymphoma on sperm deoxyribonucleic acid integrity. Fertil Steril. 2010;94(4):1374–9.
Paoli D, et al. Spermatogenesis in Hodgkin's lymphoma patients: A retrospective study of semen quality before and after different chemotherapy regimens. Hum Reprod. 2016;31(2):263–72.
Salsman JM, et al. Documentation of fertility preservation discussions for young adults with cancer: examining compliance with treatment guidelines. J Natl Compr Canc Netw. 2016;14(3):301–9.
Benedict C, Shuk E, Ford JS. Fertility issues in adolescent and young adult cancer survivors. J Adolesc Young Adult Oncol. 2016;5(1):48–57.
Kahn JM, et al. Adolescent and young adult lymphoma: collaborative efforts toward optimizing care and improving outcomes. Blood Adv. 2017;1(22):1945–58.
Barnett M, et al. Psychosocial outcomes and interventions among cancer survivors diagnosed during adolescence and young adulthood (AYA): a systematic review. J Cancer Survivorship Res Pract. 2016;10(5):814–31.
Valli-Pulaski H, et al. Testicular tissue cryopreservation: 8 years of experience from a coordinated network of academic centers. Hum Reprod. 2019;34(6):966–77.
Vermeulen M, et al. Role of stem cells in fertility preservation: current insights. Stem Cells Cloning. 2019;12:27–48.
Sineath RC, Mehta A. Preservation of fertility in testis cancer management. Urol Clin North Am. 2019;46(3):341–51.
Shin T, et al. Microdissection testicular sperm extraction in Japanese patients with persistent azoospermia after chemotherapy. Int J Clin Oncol. 2016;21(6):1167–71.
Halpern JA, Hill R, Brannigan RE. Guideline based approach to male fertility preservation. Urol Oncol. 2019;38:31–5.
Martinez F. Update on fertility preservation from the Barcelona International Society for Fertility Preservation-ESHRE-ASRM 2015 expert meeting: indications, results and future perspectives. Fertil Steril. 2017;108(3):407–415.e11.
Mauz-Korholz C, et al. Procarbazine-free OEPA-COPDAC chemotherapy in boys and standard OPPA-COPP in girls have comparable effectiveness in pediatric Hodgkin's lymphoma: the GPOH-HD-2002 study. J Clin Oncol. 2010;28(23):3680–6.
Acknowledgements
Oliver Brunckhorst acknowledges research support from the MRC Centre for Transplantation at King’s College London and the King’s Medical Research Trust (KMRT). Kamran Ahmed acknowledges receiving research support from The Urology Foundation, the Royal College of Surgeons of England, the Pelican Group, KMRT and the MRC Centre for Transplantation at King’s College London.
Author information
Authors and Affiliations
Contributions
MSAA was responsible for developing the methodology, article retrieval, data extraction, writing and revising the manuscript. OB assisted in developing methodology, settling article inclusion disputes and review of the manuscript. CS was responsible for carrying out article retrieval and data extraction. WD was responsible for manuscript review. MG was responsible for manuscript review. MK was responsible for manuscript review. KA supervised the project providing initial concepts and final approval of the manuscript.
Corresponding author
Ethics declarations
Conflict of interests
Not applicable.
Research involving human participants and/or animals
The article does not contain any human or animal studies by any of the authors.
Informed consent
For this type of study, consent is not required.
Additional information
Publisher's Note
Springer Nature remains neutral with regard to jurisdictional claims in published maps and institutional affiliations.
Electronic supplementary material
Below is the link to the electronic supplementary material.
Rights and permissions
Open Access This article is licensed under a Creative Commons Attribution 4.0 International License, which permits use, sharing, adaptation, distribution and reproduction in any medium or format, as long as you give appropriate credit to the original author(s) and the source, provide a link to the Creative Commons licence, and indicate if changes were made. The images or other third party material in this article are included in the article's Creative Commons licence, unless indicated otherwise in a credit line to the material. If material is not included in the article's Creative Commons licence and your intended use is not permitted by statutory regulation or exceeds the permitted use, you will need to obtain permission directly from the copyright holder. To view a copy of this licence, visit http://creativecommons.org/licenses/by/4.0/.
About this article
Cite this article
Amin, M.S.A., Brunckhorst, O., Scott, C. et al. ABVD and BEACOPP regimens’ effects on fertility in young males with Hodgkin lymphoma. Clin Transl Oncol 23, 1067–1077 (2021). https://doi.org/10.1007/s12094-020-02483-8
Received:
Accepted:
Published:
Issue Date:
DOI: https://doi.org/10.1007/s12094-020-02483-8