Abstract
Background
Emerging evidence suggests that stemness in cancer cells is a cause of drug resistance or metastasis and is an important therapeutic target. PR [positive regulatory domain I-binding factor 1 (PRDI-BF1) and retinoblastoma protein-interacting zinc finger gene (RIZ1)] domain containing 14 (PRDM14), that regulates pluripotency in primordial germ cell, has reported the overexpression and function of stemness in various malignancies, suggesting it as the possible therapeutic target. However, to our knowledge, there have been no reports on the expression and function of PRDM14 in colorectal cancer (CRC). Therefore, we investigated the expression and the role of PRDM14 in CRC.
Methods
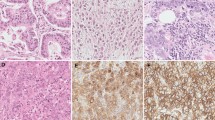
We performed immunohistochemistry evaluations and assessed PRDM14 expression on 414 primary CRC specimens. Colon cancer cell lines were subjected to functional and stemness assays in vitro and in vivo.
Results
We found that PRDM14 positive staining exhibited heterogeneity in the CRC primary tumor, especially at the tumor invasion front. The aberrant expression of PRDM14 at the invasion front was associated with lymph node metastasis and disease stage in patients with CRC. Furthermore, the multivariate analysis revealed high PRDM14 expression as an independent prognostic factor in the patients with Stage III CRC. Overexpression of PRDM14 enhanced the invasive, drug-resistant and stem-like properties in colon cancer cells in vitro and tumorigenicity in vivo.
Conclusion
Our findings suggest that PRDM14 is involved in progression and chemoresistance of CRC, and is a potential prognostic biomarker and therapeutic target in the CRC patients.



Similar content being viewed by others
Data availability
The datasets generated and analyzed during the current study are available from the corresponding author on reasonable request.
Abbreviations
- ALDH:
-
Aldehyde dehydrogenase
- CI:
-
Confidence interval
- CRC:
-
Colorectal cancer
- ESC:
-
Embryonic stem cell
- FFPE:
-
Formalin-fixed, paraffin-embedded
- HR:
-
Hazard ratio
- IHC:
-
Immunohistochemistry
- PGC:
-
Primordial germ cell
- PRDM14:
-
Positive regulatory domain I-binding factor 1 and retinoblastoma protein-interacting zinc finger gene 1 domain containing 14
- qRT-PCR:
-
Quantitative reverse transcription PCR
- SD:
-
Standard deviation
- TIF:
-
Tumor invasion front
References
Fitzmaurice C, Allen C, Barber RM, Barregard L, Bhutta ZA, Brenner H, et al. Global, regional, and national cancer incidence, mortality, years of life lost, years lived with disability, and disability-adjusted life-years for 32 cancer groups, 1990 to 2015: a systematic analysis for the global burden of disease study. JAMA Oncol. 2017;3(4):524–48. https://doi.org/10.1001/jamaoncol.2016.5688.
Siegel RL, Miller KD, Jemal A. Cancer statistics, 2018. CA. 2018;68(1):7–30. https://doi.org/10.3322/caac.21442.
Ferlay J, Colombet M, Soerjomataram I, Mathers C, Parkin DM, Pineros M, et al. Estimating the global cancer incidence and mortality in 2018: GLOBOCAN sources and methods. Int J Cancer. 2019;144(8):1941–53. https://doi.org/10.1002/ijc.31937.
Meacham CE, Morrison SJ. Tumour heterogeneity and cancer cell plasticity. Nature. 2013;501(7467):328–37. https://doi.org/10.1038/nature12624.
Visvader JE, Lindeman GJ. Cancer stem cells: current status and evolving complexities. Cell Stem Cell. 2012;10(6):717–28. https://doi.org/10.1016/j.stem.2012.05.007.
Maccalli C, De Maria R. Cancer stem cells: perspectives for therapeutic targeting. CII. 2015;64(1):91–7. https://doi.org/10.1007/s00262-014-1592-1.
Nakaki F, Saitou M. PRDM14: a unique regulator for pluripotency and epigenetic reprogramming. Trends Biochem Sci. 2014;39(6):289–98. https://doi.org/10.1016/j.tibs.2014.04.003.
Chia NY, Chan YS, Feng B, Lu X, Orlov YL, Moreau D, et al. A genome-wide RNAi screen reveals determinants of human embryonic stem cell identity. Nature. 2010;468(7321):316–20. https://doi.org/10.1038/nature09531.
Tsuneyoshi N, Sumi T, Onda H, Nojima H, Nakatsuji N, Suemori H. PRDM14 suppresses expression of differentiation marker genes in human embryonic stem cells. Biochem Biophys Res Commun. 2008;367(4):899–905. https://doi.org/10.1016/j.bbrc.2007.12.189.
Yamaji M, Seki Y, Kurimoto K, Yabuta Y, Yuasa M, Shigeta M, et al. Critical function of Prdm14 for the establishment of the germ cell lineage in mice. Nat Genet. 2008;40(8):1016–22. https://doi.org/10.1038/ng.186.
Moriya C, Taniguchi H, Miyata K, Nishiyama N, Kataoka K, Imai K. Inhibition of PRDM14 expression in pancreatic cancer suppresses cancer stem-like properties and liver metastasis in mice. Carcinogenesis. 2017;38(6):638–48. https://doi.org/10.1093/carcin/bgx040.
Nishikawa N, Toyota M, Suzuki H, Honma T, Fujikane T, Ohmura T, et al. Gene amplification and overexpression of PRDM14 in breast cancers. Can Res. 2007;67(20):9649–57. https://doi.org/10.1158/0008-5472.CAN-06-4111.
Terashima K, Yu A, Chow W-YT, Hsu W-cJ, Chen P, Wong S, et al. Genome-wide analysis of DNA copy number alterations and loss of heterozygosity in intracranial germ cell tumors. Pediatr Blood Cancer. 2014;61(4):593–600. https://doi.org/10.1002/pbc.24833.
Weiser KC, Liu B, Hansen GM, Skapura D, Hentges KE, Yarlagadda S, et al. Retroviral insertions in the VISION database identify molecular pathways in mouse lymphoid leukemia and lymphoma. Mamm Genome. 2007;18(10):709–22. https://doi.org/10.1007/s00335-007-9060-2.
Zhang T, Meng L, Dong W, Shen H, Zhang S, Liu Q, et al. High expression of PRDM14 correlates with cell differentiation and is a novel prognostic marker in resected non-small cell lung cancer. Med Oncol. 2013;30(3):605. https://doi.org/10.1007/s12032-013-0605-9.
Bi HX, Shi HB, Zhang T, Cui G. PRDM14 promotes the migration of human non-small cell lung cancer through extracellular matrix degradation in vitro. Chin Med J. 2015;128(3):373–7. https://doi.org/10.4103/0366-6999.150109.
Carofino BL, Ayanga B, Justice MJ. A mouse model for inducible overexpression of Prdm14 results in rapid-onset and highly penetrant T-cell acute lymphoblastic leukemia (T-ALL). Dis Mod Mech. 2013;6(6):1494–506. https://doi.org/10.1242/dmm.012575.
Dettman EJ, Simko SJ, Ayanga B, Carofino BL, Margolin JF, Morse HC 3rd, et al. Prdm14 initiates lymphoblastic leukemia after expanding a population of cells resembling common lymphoid progenitors. Oncogene. 2011;30(25):2859–73. https://doi.org/10.1038/onc.2011.12.
Taniguchi H, Hoshino D, Moriya C, Zembutsu H, Nishiyama N, Yamamoto H, et al. Silencing PRDM14 expression by an innovative RNAi therapy inhibits stemness, tumorigenicity, and metastasis of breast cancer. Oncotarget. 2017;8(29):46856–74. https://doi.org/10.18632/oncotarget.16776.
Nosho K, Kure S, Irahara N, Shima K, Baba Y, Spiegelman D, et al. A prospective cohort study shows unique epigenetic, genetic, and prognostic features of synchronous colorectal cancers. Gastroenterology. 2009;137(5):1609–20. https://doi.org/10.1053/j.gastro.2009.08.002(e1–3).
Iwagami S, Baba Y, Watanabe M, Shigaki H, Miyake K, Ishimoto T, et al. LINE-1 hypomethylation is associated with a poor prognosis among patients with curatively resected esophageal squamous cell carcinoma. Ann Surg. 2013;257(3):449–55. https://doi.org/10.1097/SLA.0b013e31826d8602.
Ashktorab H, Shakoori A, Zarnogi S, Sun X, Varma S, Lee E, et al. Reduced representation bisulfite sequencing determination of distinctive DNA hypermethylated genes in the progression to colon cancer in African Americans. Gastroenterol Res Pract. 2016;2016:1–8. https://doi.org/10.1155/2016/2102674.
Haraguchi N, Ohara N, Koseki J, Takahashi H, Nishimura J, Hata T, et al. High expression of ADAMTS5 is a potent marker for lymphatic invasion and lymph node metastasis in colorectal cancer. Mol Clin Oncol. 2017;6(1):130–4. https://doi.org/10.3892/mco.2016.1088.
Huang L, Wang X, Wen C, Yang X, Song M, Chen J, et al. Hsa-miR-19a is associated with lymph metastasis and mediates the TNF-alpha induced epithelial-to-mesenchymal transition in colorectal cancer. Sci Rep. 2015;5:13350. https://doi.org/10.1038/srep13350.
Zheng Y, Song D, Xiao K, Yang C, Ding Y, Deng W, et al. LncRNA GAS5 contributes to lymphatic metastasis in colorectal cancer. Oncotarget. 2016;7(50):83727–34. https://doi.org/10.18632/oncotarget.13384.
Baltaci E, Karaman E, Dalay N, Buyru N. Analysis of gene copy number changes in head and neck cancer. Clin Otolaryngol. 2018;43(4):1004–9. https://doi.org/10.1111/coa.12686.
Baykara O, Bakir B, Buyru N, Kaynak K, Dalay N. Amplification of chromosome 8 genes in lung cancer. J Cancer. 2015;6(3):270–5. https://doi.org/10.7150/jca.10638.
Moelans CB, de Weger RA, Monsuur HN, Vijzelaar R, van Diest PJ. Molecular profiling of invasive breast cancer by multiplex ligation-dependent probe amplification-based copy number analysis of tumor suppressor and oncogenes. Mod Pathol. 2010;23(7):1029–39. https://doi.org/10.1038/modpathol.2010.84.
Cancer Genome Atlas N. Comprehensive molecular characterization of human colon and rectal cancer. Nature. 2012;487(7407):330–7. https://doi.org/10.1038/nature11252.
Nandy SB, Orozco A, Lopez-Valdez R, Roberts R, Subramani R, Arumugam A, et al. Glucose insult elicits hyperactivation of cancer stem cells through miR-424-cdc42-prdm14 signalling axis. Br J Cancer. 2017;117(11):1665–75. https://doi.org/10.1038/bjc.2017.335.
Brabletz T, Jung A, Reu S, Porzner M, Hlubek F, Kunz-Schughart LA, et al. Variable beta-catenin expression in colorectal cancers indicates tumor progression driven by the tumor environment. Proc Natl Acad Sci USA. 2001;98(18):10356–61. https://doi.org/10.1073/pnas.171610498.
Brabletz T, Jung A, Hermann K, Gunther K, Hohenberger W, Kirchner T. Nuclear overexpression of the oncoprotein beta-catenin in colorectal cancer is localized predominantly at the invasion front. Pathol Res Pract. 1998;194(10):701–4.
Hlubek F, Brabletz T, Budczies J, Pfeiffer S, Jung A, Kirchner T. Heterogeneous expression of Wnt/beta-catenin target genes within colorectal cancer. Int J Cancer. 2007;121(9):1941–8. https://doi.org/10.1002/ijc.22916.
Kahlert C, Lahes S, Radhakrishnan P, Dutta S, Mogler C, Herpel E, et al. Overexpression of ZEB2 at the invasion front of colorectal cancer is an independent prognostic marker and regulates tumor invasion in vitro. Clin Cancer Res. 2011;17(24):7654–63. https://doi.org/10.1158/1078-0432.CCR-10-2816.
Le NH, Franken P, Fodde R. Tumour-stroma interactions in colorectal cancer: converging on beta-catenin activation and cancer stemness. Br J Cancer. 2008;98(12):1886–933. https://doi.org/10.1038/sj.bjc.6604401.
Nemolato S, Restivo A, Cabras T, Coni P, Zorcolo L, Orru G, et al. Thymosin beta 4 in colorectal cancer is localized predominantly at the invasion front in tumor cells undergoing epithelial mesenchymal transition. Cancer Biol Ther. 2012;13(4):191–7. https://doi.org/10.4161/cbt.13.4.18691.
Ougolkov AV, Yamashita K, Mai M, Minamoto T. Oncogenic β-catenin and MMP-7 (matrilysin) cosegregate in late-stage clinical colon cancer. Gastroenterology. 2002;122(1):60–71. https://doi.org/10.1053/gast.2002.30306.
Vignjevic D, Schoumacher M, Gavert N, Janssen KP, Jih G, Lae M, et al. Fascin, a novel target of beta-catenin-TCF signaling, is expressed at the invasive front of human colon cancer. Can Res. 2007;67(14):6844–53. https://doi.org/10.1158/0008-5472.CAN-07-0929.
Guinney J, Dienstmann R, Wang X, de Reynies A, Schlicker A, Soneson C, et al. The consensus molecular subtypes of colorectal cancer. Nat Med. 2015;21(11):1350–6. https://doi.org/10.1038/nm.3967.
Acknowledgements
We thank the pathology departments of Sapporo Medical University Hospital and Keiyukai Sapporo Hospital for providing the tissue specimens. Writing assistance: the authors would like to thank Enago (https://www.enago.jp) for English language review.
Funding
This work was supported by the Japan Society for the Promotion of Science (JSPS) Grant-in-Aid for Scientific Research (Grant number 26860515 to H. I.), Takeda Science Foundation (to H. I.), Daiwa Securities Health Foundation (to H. I.), JSPS Grant-in-Aid for Scientific Research (Grant number 16K07145 to K. N.), and Japan Agency for Medical Research and Development (Grant number 16Ack0106108h0003 to H. T.). The funding bodies had no involvement in the design of the study, collection, analysis, and interpretation of data and in writing the manuscript.
Author information
Authors and Affiliations
Contributions
Study concept and design: HI, HT. Data acquisition: HI, KI1, HK, KM, KO, IT. Data analysis and interpretation: HI, HT, KN. Drafting of the manuscript: HI, KI1, HK, KM. Critical revision of the manuscript for important intellectual content: HT, KN, KO, IT, KI2, HN. Statistical analysis: HI. Final approval of manuscript: all authors.
Corresponding author
Ethics declarations
Conflict of interest
The authors declare that they have no conflict of interest.
Ethics approval
This study was approved by the institutional review board of Sapporo Medical University Clinical trial center (reference number: 23-16), and was in accordance with the World Medical Association’s Declaration of Helsinki (1964, and its later amendments). All the animal studies were performed under the supervision of the Committee for Animal Research Center of Sapporo Medical University and in accordance with protocols approved by the Institutional Animal Care and Use Committee (reference number: 18-071).
Informed consent
Informed consent was obtained from all individual participants included in the study.
Additional information
Publisher's Note
Springer Nature remains neutral with regard to jurisdictional claims in published maps and institutional affiliations.
Electronic supplementary material
Below is the link to the electronic supplementary material.
Rights and permissions
About this article
Cite this article
Igarashi, H., Taniguchi, H., Nosho, K. et al. PRDM14 promotes malignant phenotype and correlates with poor prognosis in colorectal cancer. Clin Transl Oncol 22, 1126–1137 (2020). https://doi.org/10.1007/s12094-019-02239-z
Received:
Accepted:
Published:
Issue Date:
DOI: https://doi.org/10.1007/s12094-019-02239-z