Abstract
Gastrointestinal impairment induced sleep, behavioral and psychiatric disorders were reported in patients of autism spectrum disorders (ASDs). These may be life-long neuro-developmental disorders. Standardized diagnostic criteria for ASDs include: restricted and repetitive behavior, ongoing deficiencies in social interaction and communication. Pro-antioxidant and anti-inflammatory effects of dietry polyphenols/poly-phenol-rich derivatives as bioactive compounds enhanced permeability of blood brain barrier, consequently leads to delay in the onset of ASDs symptoms and can be effectively used in the management of ASDs. During the research on ASDs numerous therapeutic modalities, such as chemical and plant-based therapies, have been investigated. Due to their possible neuro-psychopharmacological benefits, plant-based treatments have attracted interest. These natural source therapies have demonstrated potential in reducing ASDs-related symptoms. Plant-based psycho-pharmaceuticals have been thoroughly investigated, and the investigations have confirmed their therapeutic effects. The therapeutic qualities of plants not only address the complex neurological aspects of ASDs but also provide a comprehensive approach to treatment. These substances may restore neurochemical equilibrium by focusing on particular biochemical pathways associated with the illness. Advancements in pharmacology and neurochemistry have enabled targeted interventions through chemical approaches. The treatment of ASDs approached through a combination of plant-based solutions and chemical methods can be better than one alone. By targeting the restorative properties of both natural compounds and synthesized chemicals, researchers aim to address the diverse range of symptoms and underlying neurobiological abnormalities associated with ASDs. Further clinical studies are required to validate the potential of bioactive molecules scientifically.
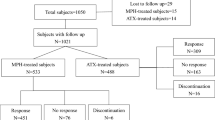
Graphical Abstract








Similar content being viewed by others
References
Serra D, Almeida LM, Dinis TCP (2019) Polyphenols as food bioactive compounds in the context of Autism spectrum disorders: a critical mini-review. Neurosci Biobehav Rev 102:290–298. https://doi.org/10.1016/j.neubiorev.2019.05.010
Kanner L (1995) Follow-up study of eleven autistic children originally reported in: 1943–1971"LaPsychiatrie de L’enfant 38:421–461
Ferguson BJ, Dovgan K, Takahashi N, Beversdorf DQ (2019) The relationship among gastrointestinal symptoms, problem behaviors, and internalizing symptoms in children and adolescents with autism spectrum disorder. Front Psychiatry 10:194. https://doi.org/10.3389/fpsyt.2019.00194
Maenner MJ, Arneson CL, Levy SE, Kirby RS, Nicholas JS, Durkin MS (2012) Brief report: association between behavioral features and gastrointestinal problems among children with autism spectrum disorder. J Autism Dev Disord 42:1520–1525. https://doi.org/10.1007/s10803-011-1379-6
Widiger TA, Costa PT Jr (2013) Personality disorders and the five-factor model of personality: rationale for the third edition. Am Psychol Assoc. https://doi.org/10.1037/13939-000
Elsabbagh M, Divan G, Koh YJ, Kim YS, Kauchali S, Marcín C, Montiel-Nava C, Patel V, Paula CS, Wang C, Yasamy MT (2012) Global prevalence of autism and other pervasive developmental disorders. Autism Res 5:160–179. https://doi.org/10.1002/aur.239
Baxter AJ, Brugha TS, Erskine HE, Scheurer RW, Vos T, Scott JG (2015) The epidemiology and global burden of autism spectrum disorders. Psychol Med 45:601–613. https://doi.org/10.1017/S003329171400172X
Kogan MD, Vladutiu CJ, Schieve LA, Ghandour RM, Blumberg SJ, Zablotsky B, Perrin JM, Shattuck P, Kuhlthau KA, Harwood RL, Lu MC (2018) The prevalence of parent-reported autism spectrum disorder among US children. Pediatr 142:6. https://doi.org/10.1542/peds.2017-4161
Fombonne E (2009) Epidemiology of pervasive developmental disorders. Pediatr Res 65:591–598. https://doi.org/10.1203/PDR.0b013e31819e7203
Rabie AH, Saleh AI (2023) A new diagnostic autism spectrum disorder (DASD) strategy using ensemble diagnosis methodology based on blood tests. Health Inf Sci Syst 11:36. https://doi.org/10.1007/s13755-023-00234-x
Hadoush H, Alafeef M, Abdulhay E (2019) Automated identification for autism severity level: EEG analysis using empirical mode decomposition and second order difference plot. Behav Brain Res 362:240–248. https://doi.org/10.1016/j.bbr.2019.01.018
First MB, Yousif LH, Clarke DE, Wang PS, Gogtay N, Appelbaum PS (2022) DSM-5-TR: overview of what’s new and what’s changed. WPA 21:2018–2219. https://doi.org/10.1002/wps.20989
Vorstman JAS, Parr JR, Moreno-De-Luca D, Anney RJL, Nurnberger JI Jr, Hallmayer JF (2017) Autism genetics: opportunities and challenges for clinical translation. Nat Rev Genet 18:362–376. https://doi.org/10.1038/nrg.2017.4
Modabbernia A, Velthorst E, Reichenberg A (2017) Environmental risk factors for autism: an evidence-based review of systematic reviews and meta-analyses. Mol Autism 8:1–16. https://doi.org/10.1186/s13229-017-0121-4
Pugsley K, Scherer SW, Bellgrove MA, Hawi Z (2022) Environmental exposures associated with elevated risk for autism spectrum disorder may augment the burden of deleterious de novo mutations among probands. Mol Psychiatry 27:710–730. https://doi.org/10.1038/s41380-021-01142-w
Allen L, Leon-Attia O, Shaham M, Shefer S, Gabis LV (2020) Autism risk linked to prematurity is more accentuated in girls. PLoS ONE 15:e0236994. https://doi.org/10.1371/journal.pone.0236994
Lin P-Y, Chen Y-L, Hsiao RC, Chen H-L, Yen C-F (2023) Risks of attention-deficit/hyperactivity disorder, autism spectrum disorder, and intellectual disability in children delivered by caesarean section: a population-based cohort study. Asian J Psychiatry 80:103334
Shen MD, Piven J (2017) Infant brain and behaviour development in autism. Dialog Clin Neurosci 19:325–333. https://doi.org/10.31887/DCNS.2017
Ratnesh RK, Mehata MS (2018) Tunable single and double emission semiconductor nanocrystal quantum dots: a multianalyte sensor. Method Appl Fluoresc 6:035006. https://doi.org/10.1088/2050-6120/aaba8a
Gardener H, Spiegelman D, Buka SL (2011) Perinatal and neonatal risk factors for autism: a comprehensive meta-analysis. Pediatr 128:344–355. https://doi.org/10.1542/peds.2010-1036
Wang C, Geng H, Liu W, Zhang G (2017) Prenatal, perinatal, and postnatal factors associated with autism: a meta-analysis. Med (Baltimore) 96:e6696. https://doi.org/10.1097/MD.0000000000006696
Pender B, Brendel W, Richard F, Summers; Dejong S 2022 Diagnostic and statistical manual of mental disorders fifth edition text revision American psychiatric association publishing, Washington, DC
Gentile S (2014) Risks of neurobehavioral teratogenicity associated with prenatal exposure to valproate monotherapy: a systematic review with regulatory repercussions. CNS Spectr 19:305–315. https://doi.org/10.1017/S1092852913000990
Kobayashi T et al (2016) autism spectrum disorder and prenatal exposure to selective serotonin reuptake inhibitors: a systematic review and metaanalysis. Reprod Toxicol 65:170–178. https://doi.org/10.1016/j.reprotox.2016.07.016
Rosen BN et al (2015) Maternal smoking and autism spectrum disorder: a metaanalysis. J Autism Dev Disord 45:1689–1698. https://doi.org/10.1007/s10803-014-2327-z
Garg A, Ratnesh RK., Chauhan RK., Mittal N, Shankar H (2022) Current advancement and progress in BioFET: a review, international conference on signal and information processing (IConSIP) IEEE: 1–7 https://doi.org/10.1109/ICoNSIP49665.2022.10007517
Bölte S, Girdler S, Marschik PB (2019) The contribution of environmental exposure to the etiology of autism spectrum disorder. Cell Mol Life Sci 76:1275–1297. https://doi.org/10.1007/s00018-018-2988-4
Gallardo-Carrasco MC, Jiménez-Barbero JA, Bravo-Pastor MDM, Martin-Castillo D, Sánchez-Muñoz M (2022) Serum vitamin D, folate and fatty acid levels in children with autism spectrum disorders: a systematic review and meta-analysis. J Autism Dev Disord 52:4708–4721. https://doi.org/10.1007/s10803-021-05335-8
Taleb A, Lin W, Xu X, Zhang G, Qi-G Z, Naveed M, Meng F, Fukunaga K, Han F (2021) Emerging mechanisms of valproic acid-induced neurotoxic events in autism and its implications for pharmacological treatment. Biomed pharmacother 137:111322. https://doi.org/10.1016/j.biopha.2021.111322
Kuo HY, Liu FC (2022) Pathophysiological studies of monoaminergic neurotransmission systems in valproic acid-induced model of autism spectrum disorder. Biomedicines 10:560. https://doi.org/10.3390/biomedicines10030560
Sabers A, Bertelsen FC, Scheel-Krüger J, Nyengaard JR, Møller A (2014) Long-term valproic acid exposure increases the number of neocortical neurons in the developing rat brain. a possible new animal model of autism. Neurosci lett 580:12–16. https://doi.org/10.1016/j.neulet.2014.07.036
Wang Z, Hong Y, Zou L, Zhong R, Zhu B, Shen N, Chen W, Lou J, Ke J, Zhang T, Wang W (2014) Reelin gene variants and risk of autism spectrum disorders: an integrated meta-analysis. AJMGB 165:192–200. https://doi.org/10.1002/ajmg.b.32222
Bartholomeusz HH, Courchesne E, Karns CM (2002) Relationship between head circumference and brain volume in healthy normal toddlers, children, and adults. Neuropediatrics 33:239–241. https://doi.org/10.1055/s-2002-36735
Xu X, Miller EC, Pozzo-Miller L (2014) Dendritic spine dysgenesis in Rett syndrome. Front neuroanat 8:97. https://doi.org/10.3389/fnana.2014.00097
Kelleher RJ, Bear MF (2014) The autistic neuron: troubled translation? Cell (2008) 135:401–406. https://doi.org/10.1016/j.cell.2008.10.017
Gonzales ML, LaSalle JM (2010) The role of MeCP2 in brain development and neurodevelopmental disorders. Curr psychiatry rep 12:127–134. https://doi.org/10.1007/s11920-010-0097-7
Laumonnier F, Nguyen LS, Jolly L, Raynaud M, Gecz J (2014) UPF3B gene and nonsense-mediated mRNA decay in autism spectrum disorders. In: Patel VB, Preedy VR, Martin CR (eds) Comprehensive Guide to Autism. Springer, New York, pp 1663–1678. https://doi.org/10.1007/978-1-4614-4788-7_101
Bierne H, Hamon M, Cossart P (2012) Epigenetics and bacterial infections. Cold Spring Harb perspect med 2:a010272. https://doi.org/10.1101/cshperspect.a010272
Kawicka A, Regulska-Ilow B (2013) How nutritional status, diet and dietary supplements can affect autism? A review. Rocz 64:1
Hyman SL, Stewart PA, Schmidt B, Cain U, Lemcke N, Foley JT, Peck R, Clemons T, Reynolds A, Johnson C, Handen B (2012) Nutrient intake from food in children with autism. Pediatrics 130:S145–S153. https://doi.org/10.1542/peds.2012-0900L
Garg A, Ratnesh RK (2022) Solar cell trends, and the future: a review J Pharma Negat Result 13 :2051–2060. https://doi.org/10.47750/pnr.2022.13.S06.268
Tildesley NT, Kennedy DO, Perry EK, Ballard CG, Wesnes KA, Scholey AB (2005) Positive modulation of mood and cognitive performance following administration of acute doses of Salvia lavandulaefolia essential oil to healthy young volunteers. Physiol behav 83:699–709. https://doi.org/10.1016/j.physbeh.2004.09.010
Casano AM, Peri F (2015) Microglia: multitasking specialists of the brain. Dev Cell 32:469–477. https://doi.org/10.1016/j.devcel.2015.01.018
Streit WJ, Mrak RE, Griffin WS (2004) Microglia and neuroinflammation: a pathological perspective. J neuroinflam 1:1–4. https://doi.org/10.1186/1742-2094-1-14
Kim JW, Hong JY, Bae SM (2018) Microglia and autism spectrum disorder: overview of current evidence and novel immunomodulatory treatment options. Clin Psychopharmacol Neurosci 16:246. https://doi.org/10.9758/cpn.2018.16.3.246
Kumar R, Ratnesh RK, Singh J, Kumar A, Chandra R (2024) IoT-driven experimental framework for advancing electrical impedance tomography. J Solid-State Sci Technol 13:027002. https://doi.org/10.1149/2162-8777/ad2331
Bertolino B, Crupi R, Impellizzeri D, Bruschetta G, Cordaro M, Siracusa R, Esposito E, Cuzzocrea S (2017) Beneficial effects of co-ultramicronized palmitoylethanolamide/luteolin in a mouse model of autism and in a case report of autism. CNS Neurosci Ther 23:87–98. https://doi.org/10.1111/cns.12648
Tsilioni I, Taliou A, Francis K, Theoharides TC (2015) Children with autism spectrum disorders, who improved with a luteolin-containing dietary formulation, show reduced serum levels of TNF and IL-6. Transl Psychiatry 5:e647. https://doi.org/10.1038/tp.2015.142
Rossignol DA, Frye RE (2014) Evidence linking oxidative stress, mitochondrial dysfunction, and inflammation in the brain of individuals with autism. Front Physiol 5:150. https://doi.org/10.3389/fphys.2014.00150
Schimidt HL, Garcia A, Martins A, Mello-Carpes PB, Carpes FP (2017) Green tea supplementation produces better neuroprotective effects than red and black tea in Alzheimer-like rat model. Food Res Int 100:442–448. https://doi.org/10.1016/j.foodres.2017.07.026
Cabrera C, Artacho R, Giménez R (2006) Beneficial effects of green tea—a review. J Am Coll Nutr 25:79–99. https://doi.org/10.1080/07315724.2006.10719518
Vaidyanathan JB, Walle T (2001) Transport and metabolism of the tea flavonoid (–)-epicatechin by the human intestinal cell line Caco-2. Pharm Res 18:1420–1425. https://doi.org/10.1023/a:1012200805593
Pathak S, Kishore N, Upadhyay G, Ratnesh RK, Mishra R (2021) A compact size planar microstrip-fed patch antenna with hexagonal dgs slot for wlan application. recent trends in electronics and communication, LNEE. Springer. 777:263-271. https://doi.org/10.1007/978-981-16-2761-3_25
Urdaneta KE, Castillo MA, Montiel N, Semprún-Hernández N, Antonucci N, Siniscalco D (2018) Autism spectrum disorders: potential neuro-psychopharmacotherapeutic plant-based drugs. Assay Drug Dev Technol 16:433–444. https://doi.org/10.1089/adt.2018.848
McNamara FN, Randall A, Gunthorpe MJ (2005) Effects of piperine, the pungent component of black pepper, at the human vanilloid receptor (TRPV1). Br J Pharmacol 144:781. https://doi.org/10.1038/sj.bjp.0706040
Ornoy A, Weinstein-Fudim L, Ergaz Z (2019) Prevention or amelioration of autism-like symptoms in animal models: will it bring us closer to treating human ASD? Int J Mol Sci 20:1074. https://doi.org/10.3390/ijms20051074
Wattanathorn J, Chonpathompikunlert P, Muchimapura S, Priprem A, Tankamnerdthai O (2008) The potential functional food for mood and cognitive disorders. Food Chem Toxicol 46:3106–3110. https://doi.org/10.1016/j.fct.2008.06.014
Al-Askar M, Bhat RS, Selim M, Al-Ayadhi L, El-Ansary, (2017) A Postnatal treatment using curcumin supplements to amend the damage in VPA-induced rodent models of autism. BMC Complement Altern 17:1–1. https://doi.org/10.1186/s12906-017-1763-7
Jackson SJ, Murphy LL, Venema RC, Singletary KW, Young AJ (2013) Curcumin binds tubulin, induces mitotic catastrophe, and impedes normal endothelial cell proliferation. Food Chem Toxicol 60:431–438. https://doi.org/10.1016/j.fct.2013.08.008
Feroe AG, Uppal N, Gutiérrez-Sacristán A, Mousavi S, Greenspun P, Surati R, Kohane IS, Avillach P (2021) Medication use in the management of comorbidities among individuals with autism spectrum disorder from a large nationwide insurance database. JAMA Pediatr 175:957–965. https://doi.org/10.1001/jamapediatrics.2021.1329
Aishworiya R, Valica T, Hagerman R, Restrepo B (2022) An update on psychopharmacological treatment of autism spectrum disorder. Neurotherapeutics 19:248–262. https://doi.org/10.1007/s13311-022-01183-1
Pertwee RG (2015) Endocannabinoids and their pharmacological actions. Springer Int Publ. https://doi.org/10.1007/978-3-319-20825-1-1
Pertwee RG, Howlett AC, Abood ME, Alexander SP, Di Marzo V, Elphick MR, Greasley PJ, Hansen HS, Kunos G, Mackie K, Mechoulam R (2010) International union of basic and clinical pharmacology. LXXIX. Cannabinoid receptors and their ligands: beyond CB1 and CB2 Pharmacol Rev 62:588–631 https://doi.org/10.1124/pr.110.003004
Siniscalco D, Sapone A, Giordano C, Cirillo A, de Magistris L, Rossi F, Fasano A, Bradstreet JJ, Maione S, Antonucci N (2013) Cannabinoid receptor type 2, but not type 1, is up-regulated in peripheral blood mononuclear cells of children affected by autistic disorders. J Autism Dev Disord 43:2686–2695. https://doi.org/10.3390/ijms18071425
Habib SS, Al-Regaiey K, Bashir S, Iqbal M (2017) Role of endocannabinoids on neuroinflammation in autism spectrum disorder prevention J clin diagn res: JCDR 11:CE01 https://doi.org/10.7860/JCDR/2017/23862.9969
Fu M, Sun ZH, Zuo HC (2010) Neuroprotective effect of piperine on primarily cultured hippocampal neurons. Biol Pharm Bull 33:598–603. https://doi.org/10.1248/bpb.33.598
Vang O, Ahmad N, Baile CA, Baur JA, Brown K, Csiszar A, Das DK, Delmas D, Gottfried C, Lin HY, Ma QY (2011) What is new for an old molecule? Systematic review and recommendations on the use of resveratrol. PLoS ONE 6:e19881. https://doi.org/10.18632/aging.100445
Sha H, Ma Q, Jha RK, Xu F, Wang L, Wang Z, Zhao Y, Fan F (2008) Resveratrol ameliorates hepatic injury via the mitochondrial pathway in rats with severe acute pancreatitis. Eur J Pharmacol 601:136–142. https://doi.org/10.1016/j.ejphar.2008.10.017
Herbert MR (2010) Contributions of the environment and environmentally vulnerable physiology to autism spectrum disorders. Curr Opin Neurol 23:103–110. https://doi.org/10.1097/WCO.0b013e328336a01f
Kumari K, Tewari N, Mehta MS, Pandey N, Tiwari K, Ratnesh RK, Joshi HC, Pant S (2019) Steady state and time-resolved fluorescence study of 7, 8-Benzoquinoline: reinvestigation of excited state protonation. Journal of Molecular Structure 1180:855-860. https://doi.org/10.1016/j.molstruc.2018.12.013
Kothiyal SR, Ratnesh RK, Kumar A (2023) Field effect transistor (FET)-sensor for biological applications international conference on device intelligence. Computing and Communication Technologies, (DICCT) IEEE 433–438 https://doi.org/10.1109/DICCT56244.2023.10110155
Bakheet SA, Alzahrani MZ, Ansari MA, Nadeem A, Zoheir KM, Attia SM, Al-Ayadhi LY, Ahmad SF (2017) Resveratrol ameliorates dysregulation of Th1, Th2, Th17, and T regulatory cell-related transcription factor signaling in a BTBR T+ tf/J mouse model of autism. Mol Neurobiol 54:5201–5212. https://doi.org/10.1007/s12035-016-0066-1
Bhandari R, Kuhad A (2017) Resveratrol suppresses neuroinflammation in the experimental paradigm of autism spectrum disorders. Neurochem Int 103:8–23. https://doi.org/10.1016/j.neuint.2016.12.012
Brigida AL, Schultz S, Cascone M, Antonucci N, Siniscalco D (2017) Endocannabinod signal dysregulation in autism spectrum disorders: a correlation link between inflammatory state and neuro-immune alterations. Int J Mol Sci 18:1425. https://doi.org/10.3390/ijms18071425
Ude C, Schubert-Zsilavecz M, Wurglics M (2013) Ginkgo biloba extracts: a review of the pharmacokinetics of the active ingredients. Clin Pharmacokinet 52:727–749. https://doi.org/10.1007/s40262-013-0074-5
Fang W, Deng Y, Li Y, Shang E, Fang F, Lv P, Bai L, Qi Y, Yan F, Mao L (2010) Blood brain barrier permeability and therapeutic time window of Ginkgolide B in ischemia–reperfusion injury. Eur J Pharm Sci 39:8–14. https://doi.org/10.1016/j.ejps.2009.10.002
Malishev R, Shaham-Niv S, Nandi S, Kolusheva S, Gazit E, Jelinek R (2017) Bacoside-A, an Indian traditional-medicine substance, inhibits β-amyloid cytotoxicity, fibrillation, and membrane interactions. ACS Chem Neurosci 8:884–891. https://doi.org/10.1021/acschemneuro.6b00438
Russo A, Borrelli F (2005) Bacopa monniera, a reputed nootropic plant: an overview. Phytomedicine 12:305–317. https://doi.org/10.1016/j.phymed.2003.12.008
Gohil KJ, Patel JA (2010) A review on Bacopa monniera: current research and future prospects Int J Green Pharm 4 https://doi.org/10.22377/ijgp.v4i1.111
Uabundit N, Wattanathorn J, Mucimapura S, Ingkaninan K (2010) Cognitive enhancement and neuroprotective effects of Bacopa monnieri in Alzheimer’s disease model. J Ethnopharmacol 127:26–31. https://doi.org/10.1016/j.jep.2009.09.056
Shinomol GK, Bharath MS, Muralidhara, (2012) Neuromodulatory propensity of Bacopa monnieri leaf extract against 3-nitropropionic acid-induced oxidative stress: in vitro and in vivo evidences. Neurotox Res 22:102–114. https://doi.org/10.1007/s12640-011-9303-6
Holcomb LA, Dhanasekaran M, Hitt AR, Young KA, Riggs M, Manyam BV (2006) Bacopa monniera extract reduces amyloid levels in PSAPP mice. JAD 9:243–251. https://doi.org/10.3233/jad-2006-9303
Bhattacharya SK, Bhattacharya A, Kumar A, Ghosal S (2000) Antioxidant activity of Bacopa monniera in rat frontal cortex, striatum and hippocampus. Phytother Res 14:174–179. https://doi.org/10.1002/(SICI)1099-1573(200005)14:33.0.CO;2-O
Al-Ayadhi LY, Elamin NE 2013 Camel milk as a potential therapy as an antioxidant in autism spectrum disorder (ASD) eCAM https://doi.org/10.1155/2013/602834
Kappeler S, Farah Z, Puhan Z (1998) Sequence analysis of camelus dromedarius milk caseins. J Dairy Res 65:209–222. https://doi.org/10.1017/s0022029997002847
Chauhan A, Chauhan V (2006) Oxidative stress in autism. Pathophysiology 13:171–181. https://doi.org/10.1016/j.pathophys.2006.05.007
Theoharides TC, Asadi S, Panagiotidou SA (2012) Case series of a luteolin formulation (NeuroProtek®) in children with autism spectrum disorders. Int J Immunopathol Pharmacol 25:317–323. https://doi.org/10.1177/039463201202500201
Pragnya B, Kameshwari JS, Veeresh B (2014) Ameliorating effect of piperine on behavioral abnormalities and oxidative markers in sodium valproate induced autism in BALB/C mice. Behav Brain Res 270:86–94. https://doi.org/10.1016/j.bbr.2014.04.045
Sandhya T, Sowjanya J, Veeresh B (2012) Bacopa monniera (L.) Wettst ameliorates behavioral alterations and oxidative markers in sodium valproate induced autism in rats. Neurochem Res 37:1121–1131. https://doi.org/10.1007/s11064-012-0717-1
Chandana SR, Behen ME, Juhász C, Muzik O, Rothermel RD, Mangner TJ, Chakraborty PK, Chugani HT, Chugani DC (2005) Significance of abnormalities in developmental trajectory and asymmetry of cortical serotonin synthesis in autism. Int J Dev Neurosci 23:171–182. https://doi.org/10.1016/j.ijdevneu.2004.08.002
Jansson LC, Louhivuori L, Wigren HK, Nordström T, Louhivuori V, Castrén ML, Åkerman KE (2012) Brain-derived neurotrophic factor increases the motility of a particular n-methyl-d-aspartate/GABA-responsive subset of neural progenitor cells. Neuroscience 224:223–234. https://doi.org/10.1016/j.neuroscience.2012.08.038
Posey DJ, Aman MG, McCracken JT, Scahill L, Tierney E, Arnold LE, Vitiello B, Chuang SZ, Davies M, Ramadan Y, Witwer AN (2007) Positive effects of methylphenidate on inattention and hyperactivity in pervasive developmental disorders: an analysis of secondary measures. Biol Psychiatry 61:538–544. https://doi.org/10.1038/tpj.2013.23
Cortese S, Adamo N, Del Giovane C, Mohr-Jensen C, Hayes AJ, Carucci S, Atkinson LZ, Tessari L, Banaschewski T, Coghill D, Hollis C (2018) Comparative efficacy and tolerability of medications for attention-deficit hyperactivity disorder in children, adolescents, and adults: a systematic review and network meta-analysis. Lancet Psychiatry 5:727–738. https://doi.org/10.1016/S2215-0366(18)30269-4
Carmassi C, Palagini L, Caruso D, Masci I, Nobili L, Vita A, Dell’Osso L (2019) Systematic review of sleep disturbances and circadian sleep desynchronization in autism spectrum disorder: toward an integrative model of a self-reinforcing loop. Front Psychiatry 10:366. https://doi.org/10.3389/fpsyt.2019.00366
Rubenstein JL, Merzenich MM (2003) Model of autism: increased ratio of excitation/inhibition in key neural systems. Genes Brain and Behav 2:255–267. https://doi.org/10.1034/j.1601-183x.2003.00037.x
Hardan AY, Fung LK, Libove RA, Obukhanych TV, Nair S, Herzenberg LA, Frazier TW, Tirouvanziam R (2012) A randomized controlled pilot trial of oral N-acetylcysteine in children with autism. Biol psychiatr 71:956–961. https://doi.org/10.1016/j.biopsych.2012.01.014
Santos E, Clark C, Biag HMB, Tang SJ, Kim K, Ponzini MD, Schneider A, Giulivi C, Montanaro FAM, Gipe JT-E et al (2023) Open-label sulforaphane trial in FMR1 premutation carriers with fragile-X-associated tremor and ataxia syndrome (FXTAS). Cells 12:2773. https://doi.org/10.3390/cells12242773
Glaze DG, Neul JL, Kaufmann WE, Berry-Kravis E, Condon S, Stoms G, Oosterholt S, Della Pasqua O, Glass L, Jones NE, Percy AK (2019) Double-blind, randomized, placebo-controlled study of trofinetide in pediatric Rett syndrome. Neurology 92:e1912–e1925. https://doi.org/10.1212/WNL.0000000000007316
Fatemi SH, Folsom TD (2011) The role of fragile X mental retardation protein in major mental disorders. Neuropharmacology 60:1221–1226. https://doi.org/10.1016/j.neuropharm.2010.11.011
Hara Y, Ago Y, Taruta A, Hasebe S, Kawase H, Tanabe W, Tsukada S, Nakazawa T, Hashimoto H, Matsuda T, Takuma K (2017) Risperidone and aripiprazole alleviate prenatal valproic acid-induced abnormalities in behaviors and dendritic spine density in mice. Psychopharmacology 234:3217–3228. https://doi.org/10.1007/s00213-017-4703-9
Kim SJ, Shonka S, French WP, Strickland J, Miller L, Stein MA (2017) Dose-response effects of long-acting liquid methylphenidate in children with attention deficit/hyperactivity disorder (ADHD) and autism spectrum disorder (ASD): a pilot study. J Autism Dev Disord 47:2307–2313. https://doi.org/10.1007/s10803-017-3125-1
Nash K, Carter KJ (2016) Treatment options for the management of pervasive developmental disorders. Int J Psychiatry Med 51:201–210. https://doi.org/10.1177/0091217416636600
Floriano PN, Christodoulides N, Miller CS, Ebersole JL, Spertus J, Rose BG, Kinane DF, Novak MJ, Steinhubl SA, S, et al (2009) Use of saliva-based nano-biochip tests for acute myocardial infarction at the point of care: a feasibility study. Clin Chem 55:1530–1538. https://doi.org/10.1373/clinchem.2008.117713
Xie Z, Yin X, Gong B, Nie W, Wu B, Zhang X, Huang J, Zhang P, Zhou Z, Li Z (2015) Salivary microRNAs show potential as a noninvasive biomarker for detecting resectable pancreatic cancer. Cancer Prev Res 8:165. https://doi.org/10.1158/1940-6207.CAPR-14-0192
A Garg RK Ratnesh (2022)Design and simulation of GaAs/InP and Si/SiC hetrojunction solar cells ICCCES-2022. Lacture notes in electrical engineering (LNEE)Springer https://doi.org/10.1007/978-981-19-7753-4-66
Feng S, Huang S, Lin D, Chen G, Xu Y, Li Y, Huang Z, Pan J, Chen R, Zeng H (2015) Surface-enhanced Raman spectroscopy of saliva proteins for the noninvasive differentiation of benign and malignant breast tumors. Int J Nanomed 10:537–547. https://doi.org/10.2147/IJN.S71811
Lee Y-C (2021) Diagnostic value of salivary miRNA in head and neck squamous cell cancer: systematic review and meta-analysis. Int J Mol Sci 22:7026. https://doi.org/10.3390/ijms22137026
Setti G, Pezzi ME, Viani MV, Pertinhez TA, Cassi D, Magnoni C, Bellini P, Musolino A, Vescovi P, Meleti M (2020) Salivary microrna for diagnosis of cancer and systemic diseases: a systematic review. Int J Mol Sci 21:1–22. https://doi.org/10.3390/ijms21030907
Condrat CE, Thompson DC, Barbu MG, Bugnar OL, BA, Cretoiu D, Suciu N, Cretoiu S.M., Voinea SC, (2020) miRNAs as biomarkers in disease latest findings regarding their role in diagnosis and prognosis. Cells 9:276. https://doi.org/10.3390/cells9020276
Brister D, Werner BA, Gideon G, McCarty PJ, Lane A, Burrows BT, McLees S, Adelson PD, Arango JI, Marsh W, Flores A (2022) Central nervous system metabolism in autism, epilepsy and developmental delays: a cerebrospinal fluid analysis. Metabolites 12:371. https://doi.org/10.3390/metabo12050371
Mesleh AG, Abdulla SA, El-Agnaf O (2021) Paving the way toward personalized medicine: current advances and challenges in multi-OMICS approach in autism spectrum disorder for biomarkers discovery and patient stratification. J Pers Med 11:41. https://doi.org/10.3390/jpm11010041
Adams JB, Sorenson JC, Pollard EL, Kirby JK, Audhya T (2021) Evidence-based recommendations for an optimal prenatal supplement for women in the US, part two: Minerals. Nutrients 13:1849. https://doi.org/10.3390/nu13061849
Cabibihan J-J, Javed H, Aldosari M, Frazier TW, Elbashir H (2017) Sensing technologies for autism spectrum disorder screening and intervention. Sensor 17:2–25. https://doi.org/10.3390/s17010046
Pasinszki T, Krebsz M, Tung TT, Losic D (2017) Carbon nanomaterial based biosensors for non-invasive detection of cancer and disease biomarkers for clinical diagnosis. Sensor 17:1919. https://doi.org/10.3390/s17081919
Ngowi EE, Wang Y-Z, Qian L, Helmy ASH, Anyomi B, Li T, Zheng M, Jiang E-S, Duan S-F, Wei J-S, Wu D-D, Ji X-Y (2021) The application of nanotechnology for the diagnosis and treatment of brain diseases and disorders. Front Bioeng Biotechnol 9:629832. https://doi.org/10.3389/fbioe.2021.629832
Alafeef M, Moitra P, Pan D (2020) Nano-enabled sensing approaches for pathologic bacterial detection. Biosens Bioelectron 165:112276
Ivanov YD, Malsagova KA, Goldaeva KV, Pleshakova TO, Shumov ID, Galiullin RA, Kapustina SI, Iourov IY, Vorsanova SG, Ryabtsev SV et al (2022) Silicon-on-insulator-based nanosensor for the revelation of microRNA markers of autism. Genes 13:199. https://doi.org/10.3390/genes13020199
Nájera-Maldonado JM, Salazar R, Alvarez-Fitz P, Acevedo-Quiroz M, Flores-Alfaro E, Hernández-Sotelo D, Espinoza-Rojo M, Ramírez M (2024) Phenolic compounds of therapeutic interest in neuroprotection. J Xenobiot 14:227–246. https://doi.org/10.3390/jox14010014
Acknowledgements
The Authors would like to thank the department of Pharmaceutical Technology and Electronics and Communication Engineering, Meerut Institute of Engineering and Technology, Mr. Puneet Agarwal (Vice-chairman), Prof. Brijesh Singh (Director), and Prof. Garima Garg and Prof. Neha Mittal HOD’s of Pharmaceutical Technology and Electronics and Communication Engineering respectively, for providing useful infrastructure and support to carry out this research work. Author J. S. acknowledges BHU for providing a seed grant under Ministry of Education (MoE), Govt. of India, Institute of Eminence (IoE), under Dev. Scheme No. 6031.
Author information
Authors and Affiliations
Corresponding author
Ethics declarations
Conflict of interest
The authors declare that they have no conflict of interest.
Additional information
Publisher's Note
Springer Nature remains neutral with regard to jurisdictional claims in published maps and institutional affiliations.
Rights and permissions
Springer Nature or its licensor (e.g. a society or other partner) holds exclusive rights to this article under a publishing agreement with the author(s) or other rightsholder(s); author self-archiving of the accepted manuscript version of this article is solely governed by the terms of such publishing agreement and applicable law.
About this article
Cite this article
Ashwlayan, V.D., Ratnesh, R.K., Sharma, D. et al. A Comprehensive Review on Plant-Based Medications and Chemical Approaches for Autism Spectrum Disorders (ASDs) Psychopharmacotherapy. Indian J Microbiol (2024). https://doi.org/10.1007/s12088-024-01265-y
Received:
Accepted:
Published:
DOI: https://doi.org/10.1007/s12088-024-01265-y