Abstract
Bacterial pathogens have always been a part of the ecosystem in which we thrive. Some pathogens have caused deadly outbreaks in the past and have been exploited as an agent of threat. Natural hotspots for these biological pathogens are widely distributed throughout the world and hence they remain clinically important. Technological advancement and change in general lifestyle has driven the evolution of these pathogens into more virulent and resistant variants. There has been a growing concern over the development of multidrug-resistant bacterial strains that could be used as bioweapons. This rapid change in pathogens also propels the field of science to develop and innovate new strategies and methodologies which are superior and safer to the existing ones. Some bacterial agents like—Bacillus anthracis, Yersinia pestis, Francisella tularensis and toxins produced by strains of Clostridium botulinum, have been segregated as Category A substances as they pose imminent threat to public health with a history of life threatening and catastrophic disease. This review highlights some encouraging developments and value additions in the current plan of action for protection against these select biothreat bacterial pathogens.
Similar content being viewed by others
Avoid common mistakes on your manuscript.
Introduction
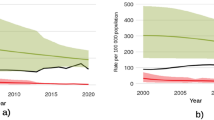
The mitigation against bacterial agents has been largely dependent upon one’s personal hygiene, available drugs (antibiotics) and vaccines (Fig. 1). Since ancient times, there have been evidences of practises which involved inoculating oneself with infectious materials to gain lifetime immunity against the disease [1]. Edward Jenner’s milestone achievement with the smallpox immunization validated this ancient concept and laid down the foundation for a more solidified research towards vaccine development [2]. Since then, a plethora of techniques, from live attenuated strains to antigenic subunits to nucleic acids, have been investigated upon to develop vaccines which are immunogenic and generating protective immune response upon administration. Vaccines have served a pivotal role in controlling diseases like polio, which is on the brink of eradication [3].
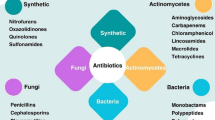
Antibiotics have also been an essential prophylactic strategy since its inception. Antibiotics have a broad spectrum impact on microorganisms and inhibit their growth by targeting specific pathways in their propagation cycle. However, effectiveness of the several antibiotics decreases with time. Pathogens have been continuously evolving to evade these molecules and thus the conventional antibiotics are bound to become ineffective at some point [4]. Microbial resistance is classified in three categories, multi-drug resistant (MDR), extensively drug-resistant (XDR) and pan drug-resistant (PDR) by Clinical Laboratory Standards Institute (CLSI), European Committee on Antimicrobial Susceptibility Testing (EUCAST), European Centre for Disease Prevention and Control (ECDC), Centres for Disease Control and Prevention (CDC) and Food and Drug Administration (FDA). MDR was defined as acquired non-susceptibility to at least one antibiotic in three or more antimicrobial classes, in XDR bacteria remain susceptible to only one or two categories and PDR defined as non-susceptibility to all antimicrobials in all antimicrobial classes [5]. It is because of these fortified pathogens, that a quest for searching new and potent broad spectrum antibiotics becomes very essential.
In addition to drugs and vaccines, monoclonal antibodies (mAbs) or to be more precise humanized-monoclonal antibodies have been recently highlighted by researchers as a valuable alternative for therapeutics [6]. The mAbs have been rigorously pursued in anti-cancer and anti-viral fields, though its applicability in bacterial infections remains unexplored. There are multiple advantageous properties which have strengthened the candidature of mAb in therapeutics; (1) mAbs are not cleared out by the host immune system as their half-life is typically 21 days, (2) mAbs used against a particular antigen do not have any collateral damaging effect on the normal tissue and symbiotic bacterial flora of the body, and (3) mAbs have multiple modes of action like direct neutralization, opsonisation by phagocytes and complement deposition [7,8,9].
The above mentioned protective strategies are highly effective but their full potential can never be tapped into unless the host immune system is evoked. The diverse immune cell repository of the host system contributes to an all-round protection against any bacteria from various locations of the body. Many discoveries have been made which have facilitated these requirements and added to the arsenal of defence against Category A bacterial agent namely: Bacillus anthracis, Yersinia pestis and Francisella tularensis and Clostridium botulinum. This review has discussed some of the recent achievements of the scientific fraternity in relation to these bacterial pathogens, which could be transformed into universally accepted therapies. Three major aspects of treatment and protection against bacteria have been discussed in the review, with an aim to provide a concise compilation of recent data relevant to microbial therapeutics against Category A bacterial biothreat agents.
Bacillus anthracis
The Gram-positive spore forming bacterium B. anthracis, is the causative organism of Anthrax, a zoonotic disease affecting humans and animals. Although mostly limited to herbivores, the disease soon finds its way up the food scale, spreading its reach to carnivores and omnivores which feed on the carcass of the infected animals (Fig. 2). Due to its endemic nature and sporadic reoccurrence once in a while, B. anthracis remains an agent of concern and a biological threat. Inhalational anthrax being the deadliest with mortality 80% or higher. The virulence of B. anthracis depends on virulent genes encoded by plasmids pXO1 and pXO2 [10]. Many antibiotics and vaccine candidate have come up since the prevalence of the disease, however, new strategies and safer alternatives are always emerging with advancements in science.
Inhalational challenge of Anthrax through spores poses as a major threat and an available prophylactic and preventive therapy is the use of Obiltoxaximab, which is a monoclonal antibody. Yamamoto et al. [11] and Hou et al. [12] through their studies had shown Obiltoxaximab to be efficacious in extending survival rates and inhibiting bacterial propagation in experimental animals. A monoclonal antibody EA 752-862 was generated which was raised in mice against r-EA1C, the C terminal domain of extractible antigen (EA1) a protein present in vegetative cells and spores of B. anthracis [13]. The mAbEA 752-862 was evaluated for its bactericidal properties using scanning electron microscopy (SEM) imaging and nucleic acid leakage assay which showed bacterial lysis in antibody treated cultures of B. anthracis. Also, the generated monoclonal antibody provided 100% protection against vegetative cells and 90% protection against spore challenge. Presently, Biothrax® (anthrax vaccine adsorbed or AVA) is the only Food and Drug Administration (FDA) approved vaccine that requires five doses in 12 months with annual booster as pre-exposure prophylaxis in person at high-risk of exposure. The same has been advised with antibiotics as post-exposure prophylaxis for persons with suspected or confirmed exposure. Attenuated deletion mutant strain vaccine of B. anthracis Sterne for the genes htrA, cya and lef provided immunity against respiratory spore challenge in animal models [14]. Implementation of advanced vaccine delivery platforms have also added to the arsenal for protection against Anthrax. Weir et al. [15] used a novel patented DPX™ no-release delivery platform (DPX), to deliver a recombinant protective antigen (rPA) vaccine in rabbits and non-human primates (NHPs). DPX formulation is composed of a lipid-mixture nanoparticle admixed with antigen and adjuvant, which was lyophilized and then solubilised in mineral oil to form a suspension. This delivery system generated an immune response at the site of vaccination. The authors investigated the protective response of the antigen rPA with the DPX system and compared it with Alum-rPA formulation and the FDA-licensed Biothrax. Single dose of DPX-rPA provided protective immunity while AVA required two immunizations. DPX-rPA was reported to provide 100% protection against B. anthracis challenge in NHPs. Similarly, a study has also been conducted using polyanhydride nanoparticles as delivery system and cyclic di-GMP (CDG) as adjuvant to generate antibody response against protective antigen. It was observed that a single dose of the formulation generated rapid protective immunity [16]. Many such next-gen vaccines are in development, AV7909 being one of them, had a probable role in post exposure prophylaxis (PEP). AV7909 is an advancement to the existing AVA that has the AVA drug substance and Toll like receptor 9 (TLR9) agonist, named as CPG 7909 as an immunostimulatory adjuvant. The AV7909 had been found to be a promising candidate induces early generation of toxin neutralising antibodies and can replace the existing Biothrax AVA vaccine regimen [17]. The safety assessment of another vaccine candidate Px563L, consisting mutant recombinant protective antigen (mrPA) and a liposome embedded monophosphoryl lipid A adjuvant was also conducted [18]. This mutant version of mrPA lacked two proteolytically sensitive sites and was incapable of toxin formation with lethal and edema factors. Phase 1 clinical trials with Px563L displayed good tolerance along with protective antibody response.
Timely administration of antibiotic regimens also proves to be effective in anthrax challenges. TP-271, a novel fluorocycline was found to be helpful in post exposure prophylactic studies in inhalational challenge models of anthrax [19]. Animals that survived post antibiotic administration had developed protective antibodies. Antibiotics targeted to effected tissues rather than through traditional systemic approach can help reduce the side effects of the drug while providing better treatment. Stratilo et al. [20] found the liposomal formulations of ciprofloxacin, Lipoquin and Apulmiq which are used as inhaled antibiotics to be highly protective in inhalational anthrax murine models. Teixobactin, a novel antibiotic which was discovered to be produced by a beta-proteobacetria is a depsipeptide that has antagonistic activity against Gram positive bacteria. Lawrence et al. [21] tested Teixobactin potency against B. anthracis in rabbit inhalational anthrax model and this treatment led to 100% survival. Table 1 provides an account of all the recent advancements in therapeutic strategies against B. anthracis.
Yersinia pestis
Yersinia pestis, is a deadly and infectious disease causing bacteria that has obtained an endemic nature in countries like USA and Madagascar. Yersinia pestis has three virulence determining plasmids namely, pPCP1, pMT1 and pCD1, each harbouring genes that are important during the pathogenic cycle of the bacteria once it has entered the host [22]. There are three known clinical manifestations upon infection with Yersinia: bubonic, septicemic and pneumonic plague (Fig. 3). The bubonic plague accounts for 70–90% of the human Y. pestis infections [23]. Fleas and rodents are the main propagators of this Gram negative, non-spore forming, non-motile bacterium. Due to this organism’s past involvement as a biothreat agent in wars, continuous progress is being made in developing new and improved mitigation strategies.
The efforts in developing possible low risk therapeutics against plague has helped researchers narrow down to certain proteins like the Fraction 1 capsular antigen (F1) which have provided mAbs that infer protection to certain extent. Liu et al. [24] had put forward their mouse hybridoma based mAb candidate F2H5. Referencing previous studies involving the F1 antigen based mAb generation; they hypothesized that the F1 protein must be containing at least one epitopic region that can provide complete protection against Y. pestis. F2H5 provided complete protection against Y. pestis challenge in mouse models and they also used computational modelling to decipher putative epitopes with which F2H5 might be interacting. Chen et al. [25] have also used the F1 antigen and synthesized an F1 antigen loaded liposome for immunization in BalB/c mice. The group has utilized microneedle based administration technique, which is a device consisting of micron sized needles arranged on a small patch. The observations in this study proved the advantageous nature of microneedles over traditional vaccine administration techniques being safer, effective and quicker. F1-liposome particles delivered using microneedles produced protecting anti-F1 IgG antibodies and cytokine response post immunization.
A novel vaccine delivery methodology has also been formulated where an attenuated strain of Y. pseudotuberculosisis used in which three genes YopK, YopJ and Asd were deleted. This mutant Yersinia strain was used to deliver a fusion protein containing a truncated YopE protein along with LcrV (a protein which is part of the type 3 secretion system (T3SS)). A single dose of this vaccine generated protective immunity against bubonic and pneumonic plague characterised by Yersinia specific CD4 and CD8 T cell production, imparting up to 90% survival rates in mice models [26]. Gupta et al. had also utilised the LcrV protein as one of the component of their bivalent fusion protein, the other protein being HSP70 Domain II of M. tuberculosis. HSP70 proteins are known immune-modulators and thus facilitate the antigenic response against the vaccine molecule. The LcrV-HSP70 fusion protein vaccine provided 100% protection against separate challenges from Y. pestis, Y. pseudotuberculosis and Y. enterocolitica bacteria in BalB/c mice [27]. Bowen et al. [28] have attempted to repurpose an existing vaccine candidate rF1-V adjuvanted with alhydrogel with an additional component SA-4-1BBL (agonist for the CD137 co-stimulatory pathway). The applicability and protective immunity of this modified vaccine was evaluated using different combinations of prime-boost doses. A priming with the original rF1-V + Alhydrogel dose and boost with the repurposed rF1-SA-4-1BBL provided protection against pneumonic plague in male mice models indicating a gender specific immunomodulation mechanism. Wang et al. [29] had generated a mutant strain of Y. pestis which produces a 1-dephosporylated hexa-acylated lipid A also named monophosphoryl lipid A (MPLA). Yersinia pestis strains produce teraacylated lipid A in mammals and this molecule is capable of evading the Toll-like Receptor 4 system. As the mutant strain is producing hexa-acylated lipid A, the strain was further substituted with a lipid A 1-phophatase gene (IpxE) from F. tularensis which led to the removal of 1-phophate from hexa-acylated lipid A as a result yielding MPLA. This mutant displayed an increased biogenesis of outer membrane vesicles (OMVs), which are lipid particles known to retain antigenic properties of the pathogen surface along with other immunogenic secretory molecules. The group further modified this strain to overexpress the Y. pestis LcrV antigen in order to increase its secretion in the OMVs, purified and used as vaccine in mice model. This OMV based vaccine was well tolerated and generated potent immune response.
Inhalational antibiotic therapies are attractive post exposure mode of drug administration since it attacks the major tissues or organs that are infected. Hamblin et al. [30] had found liposomal formulations of Ciprofloxacin to be highly efficient in protection against lethal doses of Y. pestis inhalational challenge in murine models. Gur et al. [31] had shown an inhalational therapy with Gentamicin accelerated Y. pestis elimination from lungs of mouse thus protecting against any severe secondary manifestations of the disease. A brief description of the key findings from the above mentioned studies is given in Table 2.
Francisella tularensis
Francisella tularensis is a Gram negative coccobacillus and is the causative organism of Tularemia, a rare zoonotic disease which occurs throughout Europe, North America, the Middle and East Asia and alternates through aquatic and terrestrial cycles of propagation (Fig. 4). Francisella tularensis comprises of 4 virulent subspecies namely: tularensis (type A), holoarctica (type B), novicida and mediasiatica. Subspecies tularensis is the most virulent variant of all [32]. Lack of treatment might consume an average of 30–60% life amongst infected individuals. Due to its low infectious dose, ease of dissemination through aerosolisation and high mortality, F. tularensis comes under Category A biothreat agents. Aminoglycosides are the first line of antimicrobials that are prescribed in treatment upon possible infection along with occasional usage of ciprofloxacin in case of severe infections. A broad spectrum of adaptation capabilities along with varied infection routes and life cycles makes F. tularensis to remain a candidate for further investigation.
In a quest to develop a safer and better vaccine than the available Live Vaccine Strain (LVS) of F. tularensis, a deletion mutant for the capB gene of the LVS strain was developed [33]. To further enhance the immunogenicity of the vaccine, a recombinant LVS capB strain was developed which was overexpressing Francisella Pathogenicity Island (FPI) along with a fusion protein having immune-dominant epitopes of FPI. The developed fusion protein vaccine showed similar if not in some cases lower efficacy and immunogenicity upon comparison with LVS vaccine. The new vaccine however, eliminates the toxicity and lethality of LVS vaccine. Attenuated deletion mutant vaccines are therefore quite reliant and several studies have come forward proving its applicability. Pathogenicity Determinant Protein C gene deletion mutants imparted high cellular and humoral immune response in Cynomolgus macaques [34]. Similarly, Francisella phagosomal transporter (fpt) mutants of fptA and fptF genes provide defence against lethal doses of Francisella and displayed reduced pathology in mouse model [35]. Conlan et al. [36] screened putative genes responsible for virulence in Francisella and narrowed down their findings to a clpB gene mutant that outperformed LVS vaccine in intradermal and aerosol challenges with virulent F. tularensis strains in mice.
Gaur et al. [37] and McCormick et al. [38] in separate studies attempted to evaluate the candidature of several Francisella proteins like FopA, GroEL, DnaK, OmpA, SucB and Tul4 to be used as cocktail vaccines in place LVS vaccine. An optimised antigen combination using immunogenic epitopes provided protection and also eliminated reported adverse impacts of using the live strain vaccine.
Vaccine or antigen delivery strategies can also marginally improve the cellular or humoral immunity response that is induced in the body. Whelan et al. had utilised the Glucan particle (GP) technology for delivering their in-silico screened candidate antigens to immunize mice against F. tularensis [39]. Dendritic cells phagocytose the GP through the dectin-1 receptor and the antigen are then processed and presented to induce cell mediated immunity. The Glucan particles also acted as an adjuvant in the immunization process, generating a strong immune response. The authors in this study used purified protein and Lipo-polysaccharide (LPS) from Francisella and loaded it onto the GP particle to obtain a conjugate antigen-adjuvant system for targeted and more efficient vaccine. This combined system was able to induce immune response and also a first report on a protein supplemented LPS vaccine for F. tularensis. This strategy to conjugate bacterial antigens to other known immunogens to enhance efficacy has been a well-established approach. Marshall et al. [40] used Protein Glycan Coupling technology (PGCT) for recombinant conjugation of O-antigen glycans of F. tularensis to an immunogenic Exo A protein of Pseudomonas aeruginosa, while Stefanetti et al. [41] have explored milder extraction strategies for LPS O antigen and had emphasized upon the role of epitope length i.e., high and very high molecular weight antigens in increased protection as compared to small molecular size antigens.
Although prescribed antibiotic treatment for F. tularensis is available, a possibility of emergence of a drug resistant variant although can be rare but is certainly not non-existent. Novel synthetic drugs like TP-271, a flurorcycline was potent in protecting Cynomolgus macaques under aerosol exposure of F. tularensis. TP-271 treated animals survived to the end of the study [42]. Finafloxacin, a novel fluoroquinolone demonstrated protection capability with a single dose even 96 h post challenge in mice against Francisella strain ShuS4 [43]. Altogether, advances in prophylaxis and treatment against Francisella has come long way since the LVS vaccine as compiled in Table 3 and modern scientific tools and findings will soon offer a systemic approach towards a globally acceptable prophylaxis.
Clostridium botulinum
The strains of C. botulinum produce the seven immunologically distinct neurotoxic proteins which cause the most prevalent forms of human botulism. The four naturally occurring syndromes are foodborne botulism, wound botulism, infant botulism and adult intestinal toxaemia. Upon exposure to the toxin, observable symptoms begin to appear during an acute phase (Fig. 5). Due to its high toxicity levels (with an estimated LD50 of 1–3 ng/kg in humans), ease of production on large scales and a historical record of weaponization, botulinum neurotoxins (BoNTs) come under Category A threat agent [44] classified by all national and international organizations (CDC, BTWC, FDA etc.). Antitoxins are currently the only proposed and FDA approved mode of prevention against severe exposure of BoNTs. However, there have been a few advancements and findings related to potent therapeutics which can be taken orally or through inhalation.
Antitoxins are a post exposure prophylaxis based strategy for decreasing severity in the body’s response to neurotoxin exposure. Antitoxins clear out the toxins in the circulation by inhibiting the binding of the toxins to the receptors of neurons. BAT (Botulinum Anti-Toxin Heptavalent Equine (A, B, C, D, E, F, G) manufactured by Emergent Biosolutions is a hyper-immunized plasma product which is equine based and has shown promising results in a study conducted by Kodihalli and co-workers towards its efficacy against BoNT serotype A in Rhesus macaques. BAT prevented the manifestation of signs of neurotoxicity (muscular weakness, respiratory distress) caused by botulinum toxins and also enhanced survival compared to placebo studies [45]. Equine based antitoxins, however potent they might be, are limited in usage only upon exposure to BoNTs and also remain in circulation for a brief period of time with a half-life of less than 1 day. Monoclonal antibody (mAb) based therapies offer an alternative to antitoxins and overcome the manufacturing and upscaling limitations. Since, BoNTs can be aerosolised, investigating the competence of developed mitigation strategies under inhalational challenge is also important. Tomic et al. [46] demonstrated the efficacy of two such mAb cocktails under inhalational challenge of BoNT in guinea pigs. NTM-1631 and NTM-1632 were the two candidate mAbs containing equimolar concentrations of 3 human IgG monoclonal antibodies targeting BoNTs serotype A and serotype B respectively. Both the mAb cocktails post 48 h of administration protected the Guinea pigs completely against lethal aerosol doses of BoNTs A/B. Serum levels of Neutralizing antibodies generated 6 h post administration were near to protective levels. Taking the NTM-1632 cocktail a step further, Guptill et al. [47] demonstrated its suitability of administration through human trials, assessed its safety, immunogenicity, tolerability and pharmacokinetics along with safety monitoring through physical examination of vital signs and other essential clinical studies. There were no serious observable infusion or hypersensitivity reactions and the antibodies were detected up to 121 days in 0.165-mg/kg and 0.330-mg/kg groups, both providing an upper hand compared to equine antitoxins.
Along with the conventional mAbs, Camelid single domain antibodies also known as VHHs (Variable domains of Heavy Chains) or nanobodies have been extensively worked upon recently after their discovery in the Camelid family which include alpacas. These Heavy chain antibodies lack a light chain in IgG and a constant domain (CH1) in the heavy chain, hence there is a single special variable domain which serves as the antigen binding site and is referred to as VHH. Lack of a few domains pertains to its rapid distribution and efficient recognition of difficult to access epitope regions but a shorter half-life limits their functionality to a few days. VHHs fused with human IgG Fc-fragments overcome the half-life limitations as is shown by Godakova et al. They had used the Camelid VHH-Fc fusion bodies and evaluated its efficacy against BoNT serotype A [48]. The fused bodies had improved activity and retention time in serum but the protective capacity was noted to be around only 1 h after toxin challenge in mice model indicating its usage to be only restricted as an immediate therapy or prophylaxis.
Conventional forms of delivering therapeutics for prevention against any disease causing organism might offer a temporary solution but never targets the disease pathway at its core. Taking over the pathogenesis machinery to instead deliver a cure would probably provide a more accurate targeting and neutralizing activity. The general pathway of intoxication by BoNT follows binding of its Heavy Chain (HC) to presynaptic membrane receptors and then subsequent internalization of the toxin by endocytic vesicles after which the Light Chain (LC) reaches the neuronal cytoplasm. The inherent LC metalloprotease activity cleaves SNARE proteins which ultimately blocks the overall neuronal machinery and transmission leading to the clinical symptoms of Botulism. McNutt et al. [49] had described the mutated version of BoNT serotype C1 which lacked the LC metalloprotease activity but retained the cellular trafficking and neuronal targeting. They hypothesized that the atoxic variant named C1ad could be harnessed to transport therapeutic molecules into neuronal cytoplasm which would, in theory, neutralize an incoming active BoNT toxin. To test their hypothesis, they fused a single domain antibody which was capable of functional blocking of LC activity of serotype A1 (named sdAb; B8). The resulting fusion molecule (B8C1ad) could traffic to neurons and inhibit LC/A1 catalytic activity. Administration of B8C1ad post display of symptoms gave an antidote like rescue activity in mice, guinea pigs and non-human primates.
With the advent of modern molecular and genetic engineering techniques, continuous efforts are being made to develop multivalent target specific antitoxins and vaccines. Webb et al. [50] have outlined a comparative study of their developed recombinant vaccines with catalytically inactive BoNTs holo proteins (ciBoNTs HPs). The recombinant ciBoNTs HPs elicit greater potency and the neutralizing antibodies that were produced gave better protection against both homologous and heterologous toxin challenges as compared to subunit vaccines. The presence of translocation domain, binding domain and enzymatic domain provides a better representation of the native structures of BoNTs, hence ciBoNTs HPs exhibit a large repertoire of neutralizing epitopes compared to subunit vaccines.
Synthetic drugs and molecules, categorised as small molecule inhibitors have been under continuous scrutiny in order to narrow down to a molecule that is effective against BoNTs intoxication. Compounds like 8-hydroxyquinoline have been explored for their potential against many BoNT subtypes. Chauhan et al. [51] in their study have shown their two 8-hydroxyquinoline candidate compounds: NSC1011 and NSC1014 to have remarkable extension in survival in mice models against BoNT/F challenge. Receptor binding inhibitor molecules like aurintricarboxylic acid (ATA) provided protection against BoNT A/E challenge [52]. These novel molecules and approaches hold promise towards a concluding therapeutic for BoNT spectrum pathogenesis (Table 4). Synthetic molecules not only cut down on huge production costs but also have less severe immune responses compared to antitoxins or vaccines with advantage of neutralizing capability in neuronal cells.
Conclusion
The data obtained through in-vivo clinical studies in the past decade has taken a huge leap ahead, exploring and validating several candidate therapeutic molecules having potential for up-scaling and common usage. Yet, the data seems to have scratched only the tip of the iceberg with room for more rigorous and result oriented research. A perfect prophylaxis or treatment could probably be obtained from a balanced amalgamation of the studies discussed in this review. But the difficulty lies with the prediction of the treatment’s outcome in the long run, as the results obtained in animal models can never be directly correlated to human studies. Clinical trials with respect to Category-A bacterial agent would always raise ethical concerns. However, natural sporadic reoccurrences of these pathogens in nature always alleviates the natural threat response of evaluating and exploring new avenues in science to enhance efficacy and safety of available mitigation pathways.
Availability of Data and Materials
Not applicable.
References
Troisi M, Andreano E, Sala C, Kabanova A, Rappuoli R (2020) Vaccines as remedy for antimicrobial resistance and emerging infections. Curr Opin Immunol 65:102–106. https://doi.org/10.1016/j.coi.2020.09.003
Riedel S (2005) Edward Jenner and the history of smallpox and vaccination. In: Baylor University Medical Center proceedings 2005, vol 18, No 1. Taylor & Francis, pp 21–25. https://doi.org/10.1080/08998280.2005.11928028
Greene SA, Ahmed J, Datta SD, Burns CC, Quddus A, Vertefeuille JF, Wassilak SG (2019) Progress toward polio eradication—worldwide, January 2017–March 2019. Morb Mortal Wkly Rep 68:458
Koulenti D, Xu E, Yin Sum Mok I, Song A, Karageorgopoulos DE, Armaganidis A, Lipman J, Tsiodras S (2019) Novel antibiotics for multidrug-resistant gram-positive microorganisms. Microorganisms 7:270. https://doi.org/10.3390/microorganisms7080270
Magiorakos AP, Srinivasan A, Carey RB, Carmeli Y, Falagas ME, Giske CG, Harbarth S, Hindler JF, Kahlmeter G, Olsson-Liljequist B, Paterson DL (2012) Multidrug-resistant, extensively drug-resistant and pandrug-resistant bacteria: an international expert proposal for interim standard definitions for acquired resistance. Clin Microbiol Infect 18:268–281. https://doi.org/10.1111/j.1469-0691.2011.03570.x
Zurawski DV, McLendon MK (2020) Monoclonal antibodies as an antibacterial approach against bacterial pathogens. Antibiotics 9:155. https://doi.org/10.3390/antibiotics9040155
Hey A (2015) History and practice: antibodies in infectious diseases. Microbiol Spectr 3:3. https://doi.org/10.1128/microbiolspec.AID-0026-2014
Heesterbeek DA, Angelier ML, Harrison RA, Rooijakkers SH (2018) Complement and bacterial infections: from molecular mechanisms to therapeutic applications. J Innate Immun 10:455–464. https://doi.org/10.1159/000491439
Storek KM, Auerbach MR, Shi H, Garcia NK, Sun D, Nickerson NN, Vij R, Lin Z, Chiang N, Schneider K, Wecksler AT (2018) Monoclonal antibody targeting the β-barrel assembly machine of Escherichia coli is bactericidal. Proc Natl Acad Sci 115:3692. https://doi.org/10.1073/pnas.1800043115
Levy H, Glinert I, Sittner A, Ben-Shmuel A, Bar-David E, Kobiler D, Weiss S (2019) Challenges associated with Bacillus anthracis as a bio-threat agent. In: Singh SK, Kuhn JH (eds) Defense against biological attacks. Springer, Cham, pp 115–137. https://doi.org/10.1007/978-3-030-03071-1_5
Yamamoto BJ, Shadiack AM, Carpenter S, Sanford D, Henning LN, Gonzales N, O’Connor E, Casey LS, Serbina NV (2016) Obiltoxaximab prevents disseminated Bacillus anthracis infection and improves survival during pre-and postexposure prophylaxis in animal models of inhalational anthrax. Antimicrob Agents Chemother 60:5796–5805. https://doi.org/10.1128/AAC.01102-16
Hou AW, Morrill AM (2017) Obiltoxaximab: adding to the treatment arsenal for Bacillus anthracis infection. Ann Pharmacother 51:908–913. https://doi.org/10.1177/1060028017713029
Majumder S, Das S, Kingston J, Shivakiran MS, Batra HV, Somani VK, Bhatnagar R (2020) Functional characterization and evaluation of protective efficacy of EA752-862 monoclonal antibody against B. anthracis vegetative cell and spores. Med Microbiol Immunol 209:125–37. https://doi.org/10.1016/j.vaccine.2021.05.077
Chitlaru T, Rotem S, Elia U, Bar-Haim E, Ehrlich S, Cohen O, Shafferman A (2017) A novel live attenuated anthrax spore vaccine based on an acapsular Bacillus anthracis Sterne strain with mutations in the htrA, lef and cya genes. Vaccine 35:6030–6040. https://doi.org/10.1016/j.vaccine.2017.03.033
Weir GM, MacDonald LD, Rajagopalan R, Sivko GS, Valderas MW, Rayner J, Berger BJ, Sammatur L, Stanford MM (2019) Single dose of DPX-rPA, an enhanced-delivery anthrax vaccine formulation, protects against a lethal Bacillus anthracis spore inhalation challenge. npj Vaccines 4:1–9. https://doi.org/10.1038/s41541-019-0102-z
Kelly SM, Larsen KR, Darling R, Petersen AC, Bellaire BH, Wannemuehler MJ, Narasimhan B (2021) Single-dose combination nanovaccine induces both rapid and durable humoral immunity and toxin neutralizing antibody responses against Bacillus anthracis. Vaccine 39:3862–3870. https://doi.org/10.1016/j.vaccine.2021.05.077
Shearer JD, Henning L, Sanford DC, Li N, Skiadopoulos MH, Reece JJ, Ionin B, Savransky V (2021) Efficacy of the AV7909 anthrax vaccine candidate in guinea pigs and nonhuman primates following two immunizations two weeks apart. Vaccine 39:1–5. https://doi.org/10.1016/j.vaccine.2020.10.095
Schneider JC, Chen HC, Bautista E, Retallack D (2021) Safety and immunogenicity of Px563L, a recombinant anthrax vaccine candidate, in a two-dose regimen for post-exposure prophylaxis in healthy adults. Vaccine 39:6333–6339. https://doi.org/10.1016/j.vaccine.2021.08.075
Grossman TH, Anderson MS, Drabek L, Gooldy M, Heine HS, Henning LN, Lin W, Newman JV, Nevarez R, Siefkas-Patterson K, Radcliff AK (2017) The fluorocycline TP-271 is efficacious in models of aerosolized Bacillus anthracis infection in BALB/c mice and cynomolgus macaques. Antimicrob Agents Chemother 61:e01103-17. https://doi.org/10.1128/AAC.01103-17
Stratilo CW, Jager S, Crichton M, Blanchard JD (2020) Evaluation of liposomal ciprofloxacin formulations in a murine model of anthrax. PLoS ONE 15:e0228162. https://doi.org/10.1371/journal.pone.0228162
Lawrence WS, Peel JE, Sivasubramani SK, Baze WB, Whorton EB, Beasley DW, Comer JE, Hughes DE, Ling LL, Peterson JW (2020) Teixobactin provides protection against inhalation anthrax in the rabbit model. Pathogens 9:773. https://doi.org/10.3390/pathogens9090773
Rajerison M, Kratz T (2019) Yersinia pestis. In: Singh SK, Kuhn JH (eds) Defense against biological attacks. Springer, Cham, pp 251–269. https://doi.org/10.1007/978-3-030-03071-1_11
Sebbane F, Lemaître N (2021) Antibiotic therapy of plague: a review. Biomolecules 11:724. https://doi.org/10.3390/biom11050724
Liu W, Ren J, Zhang J, Song X, Liu S, Chi X, Chen Y, Wen Z, Li J, Chen W (2017) Identification and characterization of a neutralizing monoclonal antibody that provides complete protection against Yersinia pestis. PLoS ONE 12:e0177012. https://doi.org/10.1371/journal.pone.0177012
Chen YC, Chen SJ, Cheng HF, Yeh MK (2020) Development of Yersinia pestis F1 antigen-loaded liposome vaccine against plague using microneedles as a delivery system. J Drug Deliv Sci Technol 55:101443. https://doi.org/10.1016/j.jddst.2019.101443
Singh AK, Curtiss R III, Sun W (2019) A recombinant attenuated Yersinia pseudotuberculosis vaccine delivering a Y. pestis YopENt138-LcrV fusion elicits broad protection against plague and yersiniosis in mice. Infect Immun 87:e00296-19. https://doi.org/10.1128/IAI.00296-19
Gupta A, Narayan B, Kumar S, Verma SK (2020) Vaccine potential of a recombinant bivalent fusion protein LcrV-HSP70 against plague and yersiniosis. Front Immunol 11:988. https://doi.org/10.3389/fimmu.2020.00988
Bowen W, Batra L, Pulsifer AR, Yolcu ES, Lawrenz MB, Shirwan H (2019) Robust Th1 cellular and humoral responses generated by the Yersinia pestis rF1-V subunit vaccine formulated to contain an agonist of the CD137 pathway do not translate into increased protection against pneumonic plague. Vaccine 37:5708–5716. https://doi.org/10.1016/j.vaccine.2019.07.103
Wang X, Singh AK, Zhang X, Sun W (2020) Induction of protective antiplague immune responses by self-adjuvanting bionanoparticles derived from engineered Yersinia pestis. Infect Immun 88:e00081-20. https://doi.org/10.1128/IAI.00081-20
Hamblin KA, Armstrong SJ, Barnes KB, Davies C, Laws TR, Blanchard JD, Harding SV, Atkins HS (2017) Inhaled liposomal ciprofloxacin protects against a lethal infection in a murine model of pneumonic plague. Front Microbiol 8:91. https://doi.org/10.3389/fmicb.2017.00091
Gur D, Glinert I, Aftalion M, Vagima Y, Levy Y, Rotem S, Zauberman A, Tidhar A, Tal A, Maoz S, Ber R (2018) Inhalational gentamicin treatment is effective against pneumonic plague in a mouse model. Front Microbiol 9:741. https://doi.org/10.3389/fmicb.2018.00741
Barel M, Charbit A (2019) Francisella tularensis: causative agent of tularemia and biothreat agent. In: Singh SK, Kuhn JH (eds) Defense against biological attacks. Springer, Cham, pp 239–250. https://doi.org/10.1007/978-3-030-03071-1_10
Jia Q, Bowen R, Lee BY, Dillon BJ, Masleša-Galić S, Horwitz MA (2016) Francisella tularensis live vaccine strain deficient in capB and overexpressing the fusion protein of IglA, IglB, and IglC from the bfr promoter induces improved protection against F. tularensis respiratory challenge. Vaccine 34:4969–4978. https://doi.org/10.1016/j.vaccine.2016.08.041
Tian D, Uda A, Ami Y, Hotta A, Park ES, Nagata N, Iwata-Yoshikawa N, Yamada A, Hirayama K, Miura K, Koyama Y (2019) Protective effects of the Francisella tularensis ΔpdpC mutant against its virulent parental strain SCHU P9 in cynomolgus macaques. Sci Rep 9:1–5. https://doi.org/10.1038/s41598-019-45412-8
Hobbs BE, Matson CA, Theofilou VI, Webb TJ, Younis RH, Barry EM (2021) Deletion mutants of Francisella phagosomal transporters FptA and FptF are highly attenuated for virulence and are protective against lethal intranasal Francisella LVS challenge in a murine model of respiratory tularemia. Pathogens 10:799. https://doi.org/10.3390/pathogens10070799
Conlan JW, Sjöstedt A, Gelhaus HC, Fleming P, McRae K, Cobb RR, De Pascalis R, Elkins KL (2021) Modern development and production of a new live attenuated bacterial vaccine, SCHU S4 ΔclpB, to prevent tularemia. Pathogens 10:795. https://doi.org/10.3390/pathogens10070795
Gaur R, Kamboj DV (2019) A humoral immune response study of concoction of recombinant FopA, DnaK and GroEL in mouse model as vaccine candidate against Francisella tularensis. Indian J Biotechnol 18:16–21
McCormick AA, Shakeel A, Yi C, Kaur H, Mansour AM, Bakshi CS (2018) Intranasal administration of a two-dose adjuvanted multi-antigen TMV-subunit conjugate vaccine fully protects mice against Francisella tularensis LVS challenge. PLoS ONE 13:e0194614. https://doi.org/10.1371/journal.pone.0194614
Whelan AO, Flick-Smith HC, Homan J, Shen ZT, Carpenter Z, Khoshkenar P, Abraham A, Walker NJ, Levitz SM, Ostroff GR, Oyston PC (2018) Protection induced by a Francisella tularensis subunit vaccine delivered by glucan particles. PLoS ONE 13:e0200213. https://doi.org/10.1371/journal.pone.0200213
Marshall LE, Nelson M, Davies CH, Whelan AO, Jenner DC, Moule MG, Denman C, Cuccui J, Atkins TP, Wren BW, Prior JL (2018) An O-antigen glycoconjugate vaccine produced using protein glycan coupling technology is protective in an inhalational rat model of tularemia. J Immunol Res. https://doi.org/10.1155/2018/8087916
Stefanetti G, Okan N, Fink A, Gardner E, Kasper DL (2019) Glycoconjugate vaccine using a genetically modified O antigen induces protective antibodies to Francisella tularensis. Proc Natl Acad Sci 116:7062–7070. https://doi.org/10.1073/pnas.1900144116
Grossman TH, Anderson MS, Christ D, Gooldy M, Henning LN, Heine HS, Kindt MV, Lin W, Siefkas-Patterson K, Radcliff AK, Tam VH (2017) The fluorocycline TP-271 is efficacious in models of aerosolized Francisella tularensis SCHU S4 infection in BALB/c mice and cynomolgus macaques. Antimicrob Agents Chemother 61:e00448-17. https://doi.org/10.1128/AAC.00448-17
Barnes KB, Richards MI, Laws TR, Núñez A, Thwaite JE, Bentley C, Harding SV (2021) Finafloxacin is an effective treatment for inhalational tularemia and plague in mouse models of infection. Antimicrob Agents Chemother 65:e02294-20. https://doi.org/10.1128/AAC.02294-20
Cope RB (2020) Botulinum toxin. In: Gupta RC (ed) Handbook of toxicology of chemical warfare agents. Academic Press, London, pp 427–454. https://doi.org/10.1016/B978-0-12-819090-6.00029-5
Kodihalli S, Emanuel A, Takla T, Hua Y, Hobbs C, LeClaire R, O’Donnell DC (2017) Therapeutic efficacy of equine botulism antitoxin in Rhesus macaques. PLoS ONE 12:e0186892. https://doi.org/10.1371/journal.pone.0186892
Tomic MT, Espinoza Y, Martinez Z, Pham K, Cobb RR, Snow DM, Earnhart CG, Pals T, Syar ES, Niemuth N, Kobs DJ (2019) Monoclonal antibody combinations prevent serotype A and serotype B inhalational botulism in a guinea pig model. Toxins 11:208. https://doi.org/10.3390/toxins11040208
Guptill JT, Raja SM, Juel VC, Walter EB, Cohen-Wolkowiez M, Hill H, Sendra E, Hauser B, Jackson P, Swamy GK (2021) Safety, tolerability, and pharmacokinetics of NTM-1632, a novel mixture of three monoclonal antibodies against botulinum toxin B. Antimicrob Agents Chemother 65:e02329-20. https://doi.org/10.1128/AAC.02329-20
Godakova SA, Noskov AN, Vinogradova ID, Ugriumova GA, Solovyev AI, Esmagambetov IB, Tukhvatulin AI, Logunov DY, Naroditsky BS, Shcheblyakov DV, Gintsburg AL (2019) Camelid VHHs fused to human Fc fragments provide long term protection against botulinum neurotoxin A in mice. Toxins 11:464. https://doi.org/10.3390/toxins11080464
McNutt PM, Vazquez-Cintron EJ, Tenezaca L, Ondeck CA, Kelly KE, Mangkhalakhili M, Machamer JB, Angeles CA, Glotfelty EJ, Cika J, Benjumea CH (2021) Neuronal delivery of antibodies has therapeutic effects in animal models of botulism. Sci Transl Med 13:eabd7789. https://doi.org/10.1126/scitranslmed.abd7789
Webb R, Wright PM, Brown JL, Skerry JC, Guernieri RL, Smith TJ, Stawicki C, Smith LA (2020) Potency and stability of a trivalent, catalytically inactive vaccine against botulinum neurotoxin serotypes C, E and F (triCEF). Toxicon 176:67–76. https://doi.org/10.1016/j.toxicon.2020.02.001
Chauhan R, Chauhan V, Sonkar P, Vimal M, Dhaked RK (2019) Targeted 8-hydroxyquinoline fragment based small molecule drug discovery against neglected botulinum neurotoxin type F. Bioorg Chem 92:103297. https://doi.org/10.1016/j.bioorg.2019.103297
Ben David A, Barnea A, Diamant E, Dor E, Schwartz A, Torgeman A, Zichel R (2021) Small molecule receptor binding inhibitors with in vivo efficacy against botulinum neurotoxin serotypes A and E. Int J Mol Sci 22:8577. https://doi.org/10.3390/ijms22168577
Acknowledgements
Authors are thankful to Director DRDE, Gwalior. The manuscript is assigned laboratory Accession No. IREC-01-25/08/2022. No external funding solicited for this manuscript.
Funding
Not applicable/No external funding received.
Author information
Authors and Affiliations
Contributions
AP and SR have written the manuscript and the article has been reviewed by RKD.
Corresponding author
Ethics declarations
Conflict of interest
The authors declare no conflicts of interest with respect to authorship for publication of this review article.
Ethical Approval
Not applicable.
Consent to Participate
Not applicable.
Consent for Publication
All authors have consented and have no objection for publication of the article.
Additional information
Publisher's Note
Springer Nature remains neutral with regard to jurisdictional claims in published maps and institutional affiliations.
Rights and permissions
Springer Nature or its licensor (e.g. a society or other partner) holds exclusive rights to this article under a publishing agreement with the author(s) or other rightsholder(s); author self-archiving of the accepted manuscript version of this article is solely governed by the terms of such publishing agreement and applicable law.
About this article
Cite this article
Patnaik, A., Rai, S.K. & Dhaked, R.K. Recent Advancements and Novel Approaches Contributing to the Present Arsenal of Prophylaxis and Treatment Strategies Against Category A Bacterial Biothreat Agents. Indian J Microbiol 63, 161–172 (2023). https://doi.org/10.1007/s12088-023-01075-8
Received:
Accepted:
Published:
Issue Date:
DOI: https://doi.org/10.1007/s12088-023-01075-8