Abstract
Objective
Acute Invasive Fungal Rhinosinusitis is a rare condition which recently has gained attention due to its increased occurrence in the post COVID-19 patients past the second wave. The current study retrospectively evaluates the occurrence of Acute Invasive Fungal Rhinosinusitis (Mucormycosis) in post COVID-19 (Corona Virus Disease-19) patients.
Methods
A descriptive study included patients diagnosed with Acute Invasive Fungal Rhinosinusitis (Mucormycosis) after recent COVID-19 infection. 110 patients were evaluated retrospectively with histopathological confirmation of Mucormycosis. Surgical treatment was restricted to patients who tested Real Time Polymerase Chain Reaction (RT PCR) negative for COVID-19 except for three patients who were tested positive. Antifungal agents were given to patients following surgery.
Results
A total of 110 patients with a mean age of 48.42 years were included. The most common risk factor was diabetes mellitus (88.2%). Sino-nasal, orbital, palatal and intracranial involvement were 57.9%, 48.5%, 12.7% and 5.6% respectively. Histopathological confirmation revealed mucormycosis. The most common reported symptoms were periorbital oedema (20.5%), headache (20.3%), gingival swelling (18.5%) facial pain (18.4%) and facial swelling (18.2%). All the patients were treated with surgical debridement and antifungal medications. The overall survival rate was 95.32%.
Conclusion
Acute Invasive Fungal Rhinosinusitis is a life-threatening opportunistic infection. Patients with moderate to severe COVID-19 infection are more susceptible to it. Uncontrolled diabetes mellitus and intake of corticosteroids increase the risk of developing Acute Invasive Fungal Rhinosinusitis. Early diagnosis and timely management can improve survival rates of the patients.
Similar content being viewed by others
Avoid common mistakes on your manuscript.
Introduction
Coronavirus disease 2019 (COVID-19), the highly contagious disease caused by severe acute respiratory syndrome coronavirus 2 (SARS-CoV-2) is the leading cause of emergency global pandemic [1]. COVID-19 patients found to have immunosuppression due to decrease in CD4+(Cluster of differentiation) T cells and CD8 + T cells. This immune suppression resulted in a diverse bacterial and fungal infections in association with comorbidities like diabetes mellitus [2].
Acute Invasive Fungal Rhino sinusitis (AIFRS) is a rare disease with high morbidity and mortality. Acute Invasive Fungal sinusitis is an aggressive and fatal infection of the paranasal sinuses and neighbouring vital organs. The spread and pathogenesis of the disease is by angioinvasion. The causative pathogens are a diverse group of fungal organisms that are widely distributed within the environment. Normally functioning as saprophytes that inhabit decomposing organic matter, these organisms become pathogenic under the right circumstances. Many fungal species can cause invasive infections, but the Zygomycetes (Rhizopus, Mucor, Rhizomucor) and species of Aspergillus are the most common etiologic agents in the sino-nasal cavity [3].
The presentation of AIFRS can be quite variable therefore clinical suspicion for AIFRS should be raised in the immunocompromised patient (COVID-19 infection in our study) presenting with new onset and rapidly progressive sinusitis or facial discomfort. Nasal endoscopy demonstrates areas of mucosal ischemia, frank necrosis or crusting. Radiographic imaging shows nonspecific findings of sinus opacification. Histopathological confirmation of the diagnosis requires the presence of invasive fungal elements within the submucosal tissues of the nasal cavity or paranasal sinuses. Early and accurate diagnosis is essential as the prognosis is governed by the surgical debridement and rapid initiation of antifungal therapy [3].
Materials and methods
Study setting
A retrospective descriptive study was being conducted in a tertiary ENT care centre, the nodal centre for mucormycosis.
Study population
Hundred and ten patients diagnosed with mucormycosis associated with recent COVID-19 infection from May 2021 to June 2021. The diagnosis of mucormycosis was made based on acute onset, rapid progression and histopathological confirmation.
Inclusion criteria
Patients who were tested Real Time Polymerase Chain Reaction (RT PCR) negative after recent COVID-19 infection and histopathological report suggestive of Acute Invasive Fungal Rhinosinusitis- Mucormycosis of all ages and sex were included in the study.
Exclusion criteria
Patients who were tested RT PCR positive and negative histopathological report for mucormycosis were excluded from the study.
Investigations
Computed tomography scans for chest, nose, paranasal sinuses and Magnetic resonance imaging for orbit, brain was obtained for all the patients included in the study.
Nasal endoscopy was done and the samples were taken for Potassium hydroxide (KOH) mount and fungal culture. Patients were biopsied for histopathological confirmation of mucormycosis.
Interventions
Surgical procedure was planned according to the patient’s findings. Endoscopic, open and combined approaches were utilized with debridement to clear the disease. Post operatively antifungal medications consisted of Amphotericin (intravenous) followed by Posaconazole (peroral).
Results
110 patients were diagnosed with Post COVID-19 Mucormycosis. The mean age was 48.42 (range 26–85). The sex distribution was 71.0% males and 29.0% females. The most common associated risk factor was diabetes mellitus 88.2% with de-novo 24.5% and known diabetes 63.7%.
The sino-nasal, orbital, palatal and intracranial involvement were 57.9%, 48.6%, 12.7% and 5.6% respectively. The summary of presenting symptoms and signs is presented in Table 1:
Palatal involvement included 5.8% for right side and 6.8% for left side with one patient having extension of ulcer to the midline. Skin was involved in one of the patients where there was necrosis of cheek area extending lower eyelid on right side.
During COVID-19 infection, 54.4% required hospitalization. Among the hospitalized, 51.5% required oxygen support and 16.5% took injection Remdesivir (six doses). A total of 66 patients were given corticosteroid therapy during COVID-19 treatment. Among the home quarantine 23% took oral steroids for COVID-19 infection.
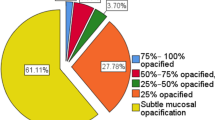
All the patients underwent Endoscopic Sinus Surgery (ESS) and debridement of the both the sides. The most common findings included pale or necrotic mucosa, nasal crusting, thick mucopurulent discharge more on the right side (Figs. 1 and 2). Endoscopic debridement included uncinectomy, wide middle meatal antrostomy, resection of inferior and middle turbinate, anterior and posterior ethmoidectomy, sphenoidotomy, frontal sinusotomy with Table 2 showing most commonly involved site along with their percentage.
Orbital involvement was managed by orbital decompression, intra-orbital / retro-orbital amphotericin injections, orbital enucleation and orbital exenteration (1.9% for right side and 1.0% for left side). Palatal involvement was managed by Maxillectomy which included either of partial or subtotal (8.8% with right 2.9%, left 4.9% and 1% bilateral) followed by temporary obturator insertion.
Mycological analysis by potassium hydroxide (KOH) mount revealed 50.7% as no fungal elements and fungal culture revealed Mucor species in 40.3%. Histopathological examination showed numerous broad ribbon-like, aseptate hyphae with right angle branching surrounded by acute inflammatory cells and presence of angioinvasion suggestive of Mucormycosis (Fig. 3). Special fungal stains such as Gomori Methenamine Silver (GMS) stain was also used to confirm the diagnosis.
Liposomal Amphotericin injections were given to all the patients who underwent debridement. The dosage depended on the intraoperative findings (3–5 mg/kg* body weight, intravenous, once daily) and the duration ranged from 3 to 14 days. In patients with suspected intracranial extension, the dose of Liposomal Amphotericin injections ranged from 5 to 10 mg/kg body weight for a duration up to three weeks. At the time of discharge, the patients were prescribed tablet Posaconazole 300 mg (twice daily on day 1 and once daily from day 2 onwards until clinically negative).
The overall survival rate was 95.32% and mortality rate was 4.68%. Early cases showed better results with surgical debridement and Amphotericin injections unlike the late cases with intracranial extension.
On applying P test, there was no statistically significant association between usage of steroids, diabetes mellitus status and presentation of symptoms with duration of hospitalisation.
*mg/kg = milligram/kilogram.
DISCUSSION:
Fungal infections were observed in severe acute respiratory syndrome (SARS) patients and were considered the leading cause of death in 25–73.7% of patients [4][5][6]. The notably rise in number of mucormycosis has gained attention in post COVID-19 due to its immunocompromised state. The incidence of invasive fungal sinusitis is still unknown [7]. deShazo et al. described three forms of invasive fungal rhinosinusitis: granulomatous, chronic, and acute fulminant. Acute Invasive Fungal Rhinosinusitis (AIFRS) is an opportunistic infection that affects severely the immunocompromised individuals. The AIFRS is used to describe fungal sinusitis when vascular invasion is histopathologically prominent and the disease duration is less than 4 weeks [8]. The most common fungal agents that cause AIFRS are Mucoraceae and Aspergillus though Mucoraceae are less frequent [9,10,11,12]. Patients with poorly controlled diabetes mellitus are susceptible to mucormycosis [9]. An acidic environment and high glucose concentration, such as in diabetic ketoacidosis, are ideal conditions for Mucoraceae [13, 14]. In other pre COVID studies, the most common concomitant disease was diabetes mellitus [15,16,17,18,19,20,21,22]. This is in accordance with my present study as the most common associated risk factor was diabetes mellitus (88.2%) [7].
The most common presenting complaints in the present study were eye swelling (periorbital edema 20.5%), headache (20.3%), gingival swelling (18.5%), facial pain (18.4%) and facial swelling (18.2%). According to Noha et al. [7] the presenting complaints were headache and facial pain (75%), facial numbness (66.7%), ophthalmoplegia and visual loss (63.9%). Previous publications discussing the non-COVID AIFRS by Abu El-Naaj reported resembling sinusitis, facial swelling, fever [23], Kursun et al. [15] listed fever (79%), periorbital cellulitis (75%) and periorbital edema (70%) while Ketenci et al. reported fever, facial edema, facial pain and nasal obstruction [18].
Disease limited to nasal cavity occurs during the early stages therefore nasal examination with endoscope should be done in patients with clinical suspicion. White discoloration of the mucosa is indicative of ischemia while black discoloration is indicative of necrosis [9][24]. Non-COVID AIFRS publications by Gillespie et al. [24] reported that mucosal abnormalities were most commonly seen on the middle turbinate (67%), followed by the septum (24%), hard palate (19%), and inferior turbinate (10%) while study by Ahmet et al. [9] the lesions were most commonly observed in the septum (12 patients, 63.2%), the middle turbinate in 11 (57.9%) patients, of the inferior turbinate (8 patients, 42.1%) and hard palate (3 patients, 15.8%). In contrast to the previous studies, our study showed involvement of the maxillary sinus (78.4%), anterior ethmoids (35.3%), posterior ethmoids (35.3%) and middle turbinate (21.6%) more on right side.
The mainstay of treatment includes antifungal agents and aggressive surgical debridement [10, 25, 26]. In the present study all the patients were surgically treated by endoscopic debridement but were 88.23% were exclusive debridement unlike the study conducted by Noha et al. [7] where 66.7% of cases underwent exclusive endoscopic debridement and in non-COVID AIFRS study by Turner et al. [3] performed endoscopic approach in 46.4% of their patients. Orbital exenteration were performed in 2.9% in our study while 16.7% of cases in study by Noha et al. [7]
The majority of patients in Noha et al. [7] study received Liposomal Amphotericin B (80.56%) and eight patients with Aspergillus received Voriconazole on other the hand my study primarily focuses on mucormycosis therefore the antifungal medication of choice was Liposomal Amphotericin B.
AIFRS has high morbidity and mortality rates (18-80%) despite improvements in medical and surgical management protocols [7]. The survival rates reported in studies ranges from 20 to 80% [15, 18, 24, 27]. The overall survival rate of non-COVID AIFRS cases reviewed by Turner et al. 11 was 49.7%, COVID AIFRS by Noha et al. [7] was 63.89% while my present study had 95.32%. The relatively better survival rate was due to early diagnosis, aggressive surgical debridement and early use of antifungal medications.
Conclusion
Early diagnosis of AIFRS (Mucormycosis) requires a high index of suspicion because of non-specific initial symptoms and radiological signs. Biopsies of mucosal tissue from suspected sites should be performed as early as possible. Complete endoscopic debridement should be the treatment of choice for highly suspected lesions limited to nasal cavity. More radical excision including maxillectomy and orbital exenteration may be necessary in severe cases. Aggressive surgical debridement followed by antifungal medications are the mainstay of AIFRS treatment. The extent of AIFRS and the underlying medical disease (uncontrolled diabetes) are the main factors related to the prognosis.
Data Availability
Not applicable.
References
Coronaviridae Study Group of the International Committee on Taxonomy of Viruses, Gorbalenya AE, Baker SC et al (2020) The species severe acute respiratory syndrome-related coronavirus: classifying 2019‐nCoV and naming it SARS‐CoV‐2. Nat Microbiol 5:536
Yang W, Cao Q, Qin L et al (2020) Clinical characteristics and imaging manifestations of the 2019 novel coronavirus disease (COVID-19): a multi‐center study in Wenzhou city, Zhejiang, China. J Infect 80:388–393
Turner JH, Soudry E, Nayak JV, Hwang PH (2013) Survival outcomes in acute invasive fungal sinusitis: a systematic review and quantitative synthesis of published evidence. Laryngoscope 123:1112–1118
Yin C, Wang C, Tang Z, Zhang S, Wang B (2004) Clinical analysis of 146 patients with critical severe acute respiratory syndrome in Beijing areas. Clin J Emerg Med 1:12–14
Zhang Y, Li W, Huang K, Cao Z, Hao J (2003) Hospital acquired pneumonia occurring after acute stage of the serious SARS and its treating strategies. Chin J Nosocomiol 11:1081–1087
Li C, Pan S (2003) Analysis and causation discussion of 185 severe acute respiratory syndrome dead cases. Zhongguo Weizhongbing Jijiuyixue 15:582–584
Invasive Fungal Sinusitis in Post COVID-19 Patients (2021) A New Clinical Entity. Noha Ahmed El‐Kholy, MD,1 Ahmed Musaad Abd El‐Fattah, MD, 1 and Yasser W. Khafagy, MD 1.Laryngoscope. 22. https://doi.org/10.1002/lary.29632
deShazo RD, O’Brien M, Chapin K, Soto-Aguilar M, Gardner L, Swain R (1997) A new classification and diagnostic criteria for invasive fungal sinusitis. Arch Otolaryngol Head Neck Surg 123:1181–1188
Acute invasive fungal (2009) rhinosinusitis: our experience with 19 patients. Ahmet Emre Süslü · Ofuz Öfretmenoflu ·Nilda Süslü · Ömer TaokÂn Yücel · TevWk Metin Önerci. Eur Arch Otorhinolaryngol 266:77–82
Talbot GH, Huang A, Provencher M (1991) Invasive aspergillus rhinosinusitis in patients with acute leukemia. Rev Infect Dis 13:219–232
Eucker J, Sezer O, Graf B, Possinger K (2001) Mucormycoses Mycoses 44:253–260
Bodey GP, Vartivarian S (1989) Aspergillosis. Eur J Clin Microbiol Infect Dis 8:413–437
Blitzer A, Lawson W (1993) Fungal infections of the nose and paranasal sinuses. Otolaryngol Clin N Am 26:1007–1035
Peterson KL, Wang M, Canalis RF, Abemayor E (1997) Rhinocerebral mucormycosis: evolution of the disease and treatment options. Laryngoscope 107:855–862
Kursun E, Turunc T, Demiroglu YZ, Alışkan HE, Arslan AH (2015) Evaluation of 28 cases of mucormycosis. Mycoses 58:82–87
Bellazreg F, Hattab Z, Meksi S et al (2015) Outcome of mucormycosis after treatment: report of five cases. New Microbes New Infect 6:49–52
Kermani W, Bouttay R, Belcadhi M, Zaghouani H, Ali MB, Abdelkéfi M (2016) ENT mucormycosis. Report of 4 cases. Eur Ann Otorhinolaryngol Head Neck Dis 133:83–86
Ketenci I, Ünlü Y, Kaya H et al (2011) Rhinocerebral mucormycosis: experience in 14 patients. J Laryngol Otol 125:e3
Mohammadi R, Meidani M, Mostafavizadeh K et al (2015) Case series of rhinocerebral mucormycosis occurring in diabetic patients. Casp J Intern Med 6:243
Saedi B, Sadeghi M, Seilani P (2011) Endoscopic management of rhinocerebral mucormycosis with topical and intravenous amphotericin B. J Laryngol Otol 125:807–810
Vaezi A, Moazeni M, Rahimi MT, de Hoog S, Badali H (2016) Mucormycosis in Iran: a systematic review. Mycoses 59:402–415
El-Naaj IA, Leiser Y, Wolff A, Peled M (2013) The surgical management of rhinocerebral mucormycosis. J Craniomaxillofac Surg 41:291–295
Gillespie MB, O’Malley BW, Francis HW (1998) An approach to fulminant invasive fungal rhinosinusitis in the immunocompromised host. Arch Otolaryngol Head Neck Surg 124:520–526
DelGaudio JM, Swain RE, Kingdom TT, Muller S, Hudgins PA (2003) CT findings in patients with invasive fungal sinusitis. Arch Otolaryngol Head Neck Surg 129:236–240
Goering P, Berlinger NT, Weisdorf DJ (1988) Aggressive combined modality treatment of progressive sinonasal fungal infections in immunocompromised patients. Am J Med 85:619–623
Chen C-Y, Sheng W‐H, Cheng A et al (2011) Invasive fungal sinusitis in patients with hematological malignancy: 15 years’ experience in a single university hospital in Taiwan. BMC Infect Dis 11:250
Mohindra S, Mohindra S, Gupta R, Bakshi J, Gupta SK (2007) Rhinocerebral mucormycosis: the disease spectrum in 27 patients. Mycoses 50:290–296
Funding
The author(s) received no financial support for the research, authorship and/or publication of this article.
Conflicts of interest/Competing InterestsThe author(s) declared no potential conflicts of interest with respect to the research, authorship and/or publication of this article.
Author information
Authors and Affiliations
Contributions
All authors contributed to the study conception and design. Material preparation, data collection and analysis were performed by Joshi Anto Tommi. J, L. Sudarshan Reddy. The first draft of the manuscript was written by Joshi Anto Tommi. J and all the authors commented on preview versions of the manuscript. All authors read and approved the final manuscript.
Corresponding author
Ethics declarations
Acknowledgemnts
We thank the Superintendent of Government ENT Hospital, Hyderabad for allowing us to use the hospital records in the study and guiding us. We thank all the faculty members and residents of our hospital for their cooperation in the smooth conduct of the study. We thank the patients and their attendants for their permission to use their data and for their cooperation in the completion of the study.
Funding
The study was conducted without any funding or sponsorship.
Ethical Approval
The study protocol was approved by the Institutional Ethics Committee.
Conflict of interest
The authors declare there is no conflict of interest.
Consent to Participate and consent for publication
As this was a retrospective analysis of medical charts, no informed consent was taken.
Additional information
Publisher’s Note
Springer Nature remains neutral with regard to jurisdictional claims in published maps and institutional affiliations.
Rights and permissions
Springer Nature or its licensor (e.g. a society or other partner) holds exclusive rights to this article under a publishing agreement with the author(s) or other rightsholder(s); author self-archiving of the accepted manuscript version of this article is solely governed by the terms of such publishing agreement and applicable law.
About this article
Cite this article
J, J.A.T., Reddy, L.S. Post COVID-19 Mucormycosis-The Horizon. Indian J Otolaryngol Head Neck Surg 75, 517–522 (2023). https://doi.org/10.1007/s12070-022-03315-7
Received:
Accepted:
Published:
Issue Date:
DOI: https://doi.org/10.1007/s12070-022-03315-7