Abstract
Total endoscopic thyroidectomy (TET) using low CO2 insufflation provides cosmetic advantage, excellent working space and visibility. On the contrary, suctioning blood or mist/smoke produced by energy device application causes narrowing of working space especially in neck surgery. In this regard, AirSeal intelligent flow system would be particularly suitable in TET. However, the benefit of AirSeal is unknown in TET unlike abdominal surgery. Therefore, the impact of AirSeal was evaluated in TET in this study. Twenty patients who underwent total endoscopic hemithyroidectomy were retrospectively analyzed. Insufflation was conducted by either conventional or AirSeal system according to the surgeon’s preference. Short-term surgical outcomes including operation time, bleeding, frequency of scope cleaning, and disappearance of subcutaneous emphysema were compared as well as actual visibility. AirSeal application dramatically reduced obstacle smoke/mist and prevented narrowing working space by suctioning. Frequency of scope cleaning was significantly less in AirSeal group than that in conventional group (p = 0.016). In patients with nodule < 5 cm, intraoperative hemorrhage was less in AirSeal group than that in the counterpart (p = 0.077) regardless of larger nodule size in AirSeal group (p = 0.058). Notably, subcutaneous emphysema around surgical cavity disappeared significantly earlier in AirSeal group than in the counter parts (p = 0.019). On the contrary, AirSeal application did not shorten operation time in the current study. AirSeal provided excellent visibility and seamless operation. AirSeal has great potential to decrease not only surgeon’s stress but surgical invasion on patients. The results in this study give rational to AirSeal application to TET.
Similar content being viewed by others
Avoid common mistakes on your manuscript.
Introduction
Although an endoscopic surgery was described with relative delay in thyroid diseases compared to other organs because of the narrow operative field, cosmetic advantages of endoscopic thyroidectomy are inarguably accepted [1]. After video-assisted neck surgery (VANS), a gasless endoscopic surgical approach, was described [2], VANS method has been widely applied. The VANS method allows manual palpation of the tumor from the chest wall incision, and excellent bleeding control. On the other hand, total endoscopic thyroidectomy (TET) by the axillary approach or else enables high degree of freedom in surgical incision that leads to further cosmetic advantage [3,4,5] than VANS method. Low pressure CO2 gas insufflation provides excellent working space and hemostatic effect on minor bleeding, contributing to excellent visibility. These are also great advantages of TET compared to a gasless VANS method. However, suction of blood or mist/smoke produced by energy device use causes narrowing of working space in TET, which may lead to extended operation time or unexpected complication due to poor visibility. Accordingly, ensuring stable working space is required to maximize the advantages of TET. AirSeal™ intelligent flow system (SurgiQuest, Milford, USA; ConMed Japan, Tokyo) is an insufflation system that can maintain a fixed pressure in surgical field by continuously monitoring and adjusting CO2 flow rates. AirSeal system consists of a contiguous trilumen filter tube set that connects to one valveless access port. AirSeal system allows immediate response to slight changes in the set pressure by automatically adjusting flow rate in real time. Such immediate and automatic compensation of CO2 pressure and volume loss provides great benefit in reducing effects on working space by intraoperative suctioning. AirSeal system is widely used in abdominal surgery especially in robotic surgery [6,7,8,9]. Taking the narrower space of neck into account, AirSeal system would provide great advantages in visibility of TET further than abdominal surgery. Therefore, we aimed to clarify whether AirSeal system can provide benefits in TET in this study.
Patients and Methods
We evaluated consecutive 20 patients who underwent endoscopic hemithyroidectomy at Kitasato University Hospital from January 2017 to December 2019. Preoperative diagnosis for hemithyroidectomy was as follows: 15 patients, adenomatous nodule(s); 3 patients, follicular tumor; 1 patient, papillary thyroid cancer; 1 patient, intrathyroidal parathyroid adenoma (Table 1). TET was performed by one surgeon similarly as previously described [10,11,12]. Briefly, a 20–30 mm incision was placed in the axilla or the lateral anterior chest. After making working space under the platysma muscle by blunt dissection and inflation of a PDB™ round balloon (Medtronic), either two 5 mm trocars (without AirSeal) or one 5 mm trocar and AirSeal port (with AirSeal) were placed through XS-size FREE ACCESS™ (TOP, Tokyo) fixed to the outer ring of a XS-size SMART RETRACTOR™ (TOP) that was inserted through the skin incision. Carbon dioxide (CO2) was insufflated to 6–8 mmHg. An additional 5 mm trocar was inserted supraclavicular and near the incision. HARMONIC HD 1000i (36 mm) (Ethicon Japan) was applied as an energy device, and the seven-mode was used to seal superior/inferior thyroid arteries. The anterior border of the sternocleidomastoid muscle was dissected from the sternohyoid muscle, then the omohyoid muscle was dissected. The sternothyroid muscle was dissected from the sternohyoid muscle and the working space was made for subsequent hemithyroidectomy. The information on operation including (endoscopic) operation time, blood loss, and frequency of scope cleaning were evaluated (Table 1).
This study was approved by the ethics committee (IRB) of the Kitasato University School of Medicine (the IRB approved #B22-004), and was performed in accordance with the clinical research guidelines of the IRB of the Kitasato University School of Medicine. All individuals gave written informed consent for pathologic assessment and routine blood sample analyses on their samples, and clinical data. The study was conducted in accordance with the Declaration of Helsinki (as revised in 2013).
Mann–Whitney’s U test was used to compare continuous variables. A p value < 0.05 was considered significant. All statistical analyses were conducted using a JMP Pro14 (SAS Institute, Cary, NC).
Results
There was no significant difference in preoperative patient characteristics (Table 1). Nodule sizes were marginally larger in AirSeal group without statistical significance (p=0.181). Average nodule sizes were 36.6 ± 5.9 (s.e.m.) mm and 44.6 ± 2.9 mm in patients without AirSeal and with AirSeal, respectively.
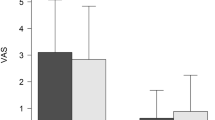
CO2 insufflation was performed at 6 mmHg in most of cases of AirSeal group (8/11) and 6 mmHg pressure was sufficient for working space. On the contrary, 8 mmHg insufflation was required for all of cases of conventional group to obtain enough working space. Application of AirSeal system dramatically reduced smoke and mist caused by an energy device, providing excellent visibitily (Fig. 1A–D, Supplementary videos 1 and 2). On suctioning mist/smokes produced by an energy device, AirSeal system prevented narrowing working space and greatly contributed to keep wide and clear visibility, leading to seamless operation (Fig. 1E, F, Supplementary videos 1 and 2). Indeed, AirSeal application significantly decreased frequency of scope cleaning from 11.8 ± 1.9 times to 6.5 ± 0.8 times per operation (p=0.016, Table 1, Fig. 2 left). Frequency of scope cleaning corrected by endoscopic operation time (hr) further showed remarkable improvement by AirSeal system which reduced the cleaning frequency during endoscopic procedure from 4.8 ± 0.6 times to 2.6 ± 0.4 times (p = 0.006, Fig. 2 right). AirSeal application only marginally contributed to reduction of intraoperative blood loss (19.2 ± 7.6 ml in non−AirSeal group vs. 12.7 ± 7.4 ml in AirSeal group, p = 0.161). In patients with nodule size < 5 cm, AirSeal decreased intraoperative blood loss from 23.3 ± 9.2 ml to 8.6 ± 6.1 ml (p = 0.077) regardless of larger nodule size (40.3 ± 2.3 cm in AirSeal group vs. 29.7 ± 4.6 cm in non−AirSeal group, p = 0.058). Notably, time to disappearance of subcutaneous emphysema around surgical cavity was significantly shorter in AirSeal group (2.82 ± 0.18 days) than in the counter parts (4.22 ± 0.52 days) (p = 0.019). On the other hand, total operation time and endoscopic operation time were not improved by AirSeal application in the current study.
Representative images of total endoscopic right hemi-thyroidectomy taking into account AirSeal application. Smoke/mist caused by energy device (Harmonic HD) obstructs visibility in non-AirSeal used conventional group (A and C). AirSeal application dramatically improved visibility by decreasing smoke/mist (B and D). Suctioning of smoke/mist narrows working space in non-AirSeal group (E). AirSeal system prevents narrowing on suctioning by retaining stable pressure (F). Video presentations demonstrate excellent visibility by AirSeal use
Discussion
In the present study, clinical impact of AirSeal intelligent flow system was first evaluated in total endoscopic thyroidectomy (TET). We report that AirSeal application dramatically improves visibility and further suggested possibility to decrease surgical stress on patients.
Recently, AirSeal system have been widely applied in laparoscopic or intraabdominal robotic surgery since Herati et al. first clinically evaluated in urologic laparoscopic surgery [13]. The hallmark of AirSeal system is its control unit which comprises a triple lumen filter tube set connected to one valveless AirSeal trocar. CO2 inflow is supplied from one lumen of the filter tube set, the second lumen provides CO2 outflow, and real−time monitoring and compensation of pressure in the surgical space is performed via the third lumen. In laparoscopy and intraabominal robitic surgery, such delicate pressure control has allowed a stable pneumoperitoneum and excellent visibility which leaded to reduction of blood loss, and further decreased laparoscopy−associated shoulder pain [6,7,8,9, 14, 15]. In TET, the insufflated operating field is much smaller than abdominal surgery. Because of the smaller working space, less smoke/mist produced by energy device easily obstruct the view and suctioning can further cause narrowing space. Therefore, AirSeal application to TET can contribute to improvement of visibility more than to abdominal surgery. Indeed, AirSeal use dramatically improved visibility in patients who underwent TET in our study (Fig. 1 and Video presentation), statistically confirmed by reduction of scope cleaning frequency (Table 1 and Fig. 2). In addition, intraoperative blood loss was decreased by AirSeal use although it is not statistically significant. On the other hand, contribution to shortening operation time has been still contradictory [14, 16]. Similarly, AirSeal application did not improve both total and endoscopic operation time in this study (Table 1).
Of note, subcutaneous emphysema around surgical cavity disappeared significantly earlier in AirSeal group, maybe because 6 mmHg CO2 insufflation was sufficient in most of patients by AirSeal application compared to 8 mmHg in conventional group. This result is consistent with a previous report in pediatric laparoscopic appendectomy [17]. Sroussi et al. reported that lower pressure resulted in less postoperative shoulder pain in gynecological laparoscopy [18]. These results suggest that AirSeal not only improve visibility but surgical invasion on patients. The valveless trocar allows to release excessive gas on the unexpected pressure elevation as a pop−off valve. This may also explain earlier disappearance of subcutaneous emphysema around surgical cavity. Previous studies reported that the valveless trocar system reduces CO2 absorption during laparoscopy by keeping intraabdominal pressures within the acceptable range longer than the conventional system [16, 19]. Additionally, Galizia et al. alerted that pulsatile flow fluctuation in conventional CO2 insufflators affects vessel tone regulation, triggering hypoperfusion and reperfusion injury, inducing oxidative stress, cellular injury, and organ dysfunction in laparoscopy [20].
Along with reducing smoke, the filter component of the AirSeal tube set minimizes the hazards of surgical smoke by removing carcinogens and pathogens from smoke down to 0.01 μm [16]. This is great advantage of AirSeal system especially in COVID−19 pandemic as well.
The limitation of this study is that this report is based on retrospective setting in small number of patients in one institution. Future studies from case−matching its cohorts and larger, multi−center, randomized control trials are needed to demonstrate the impact of AirSeal system on intraoperative and postoperative patient outcomes.
In conclusion, AirSeal system provides great benefits in visibility in TET, leading to seamless procedure and mitigating surgeon’s stress. AirSeal may have benefits in surgical invasion on patients as well. Further investigation would define the clinical impact of AirSeal on TET.
Data Availability
All data generated or analyzed during this study are included in the article. Further enquiries can be directed to the corresponding author.
Change history
28 July 2023
A Correction to this paper has been published: https://doi.org/10.1007/s12070-023-04080-x
References
Pisanu A, Podda M, Reccia I, Porceddu G, Uccheddu A (2013) Systematic review with meta-analysis of prospective randomized trials comparing minimally invasive video-assisted thyroidectomy (MIVAT) and conventional thyroidectomy (CT). Langenbecks Arch Surg 398(8):1057–1068
Shimizu K, Akira S, Tanaka S (1998) Video-assisted neck surgery: endoscopic resection of benign thyroid tumor aiming at scarless surgery on the neck. J Surg Oncol 69(3):178–180
Ikeda Y, Takami H, Niimi M, Kan S, Sasaki Y, Takayama J (2001) Endoscopic thyroidectomy by the axillary approach. Surg Endosc 15(11):1362–1364
Ikeda Y, Takami H, Sasaki Y, Kan S, Niimi M (2000) Endoscopic resection of thyroid tumors by the axillary approach. J Cardiovasc Surg (Torino) 41(5):791–792
Ikeda Y, Takami H, Sasaki Y, Kan S, Niimi M (2000) Endoscopic neck surgery by the axillary approach. J Am Coll Surg 191(3):336–340
Fadel W, Kazanowski M, Al Furajii H, Cahill RA (2016) Solitary trocar laparoscopic loop sigmoid colostomy using the AirSeal IFS system–a video vignette. Colorectal Dis 18(3):318–319
Feng TS, Heulitt G, Islam A, Porter JR (2020) Comparison of valve-less and standard insufflation on pneumoperitoneum-related complications in robotic partial nephrectomy: a prospective randomized trial. J Robot Surg 15:381–388
Horstmann M, Horton K, Kurz M, Padevit C, John H (2012) Prospective comparison between the AirSeal(R) System valve-less Trocar and a standard Versaport Plus V2 Trocar in robotic-assisted radical prostatectomy. J Endourol 27(5):579–582
Miyano G, Morita K, Kaneshiro M, Miyake H, Nouso H, Yamoto M, Koyama M, Nakano R, Tanaka Y, Fukumoto K et al (2015) Laparoscopic toupet fundoplication using an air seal intelligent flow system and anchor port in a 1.8-kg infant: a technical report. Asian J Endosc Surg 8(3):357–360
Ikeda Y, Takami H, Niimi M, Kan S, Sasaki Y, Takayama J (2002) Endoscopic thyroidectomy and parathyroidectomy by the axillary approach. A prelim Rep Surg Endosc 16(1):92–95
Ikeda Y, Takami H, Sasaki Y, Takayama J, Niimi M, Kan S (2003) Clinical benefits in endoscopic thyroidectomy by the axillary approach. J Am Coll Surg 196(2):189–195
Ikeda Y, Takami H, Tajima G, Sasaki Y, Takayama J, Kurihara H, Niimi M (2002) Total endoscopic thyroidectomy: axillary or anterior chest approach. Biomed Pharmacother 56(Suppl 1):72s–78s
Herati AS, Atalla MA, Rais-Bahrami S, Andonian S, Vira MA, Kavoussi LR (2009) A new valve-less trocar for urologic laparoscopy: initial evaluation. J Endourol 23(9):1535–1539
Luketina R, Luketina TLH, Antoniou SA, Kohler G, Konneker S, Manzenreiter L, Wundsam H, Koch OO, Knauer M, Emmanuel K (2020) Prospective randomized controlled trial on comparison of standard CO2 pressure pneumoperitoneum insufflator versus AirSeal(R). Surg Endosc 35:3670–3678
Nicholson G, Knol J, Houben B, Cunningham C, Ashraf S, Hompes R (2015) Optimal dissection for transanal total mesorectal excision using modified CO2 insufflation and smoke extraction. Colorectal Dis 17(11):O265-267
Herati AS, Andonian S, Rais-Bahrami S, Atalla MA, Srinivasan AK, Richstone L, Kavoussi LR (2011) Use of the valveless trocar system reduces carbon dioxide absorption during laparoscopy when compared with standard trocars. Urology 77(5):1126–1132
Miyano G, Nakamura H, Seo S, Sueyoshi R, Okawada M, Doi T, Koga H, Lane GJ, Yamataka A (2016) Pneumoperitoneum and hemodynamic stability during pediatric laparoscopic appendectomy. J Pediatr Surg 51(12):1949–1951
Sroussi J, Elies A, Rigouzzo A, Louvet N, Mezzadri M, Fazel A, Benifla JL (2017) Low pressure gynecological laparoscopy (7mmHg) with AirSeal((R)) system versus a standard insufflation (15mmHg): a pilot study in 60 patients. J Gynecol Obstet Hum Reprod 46(2):155–158
Bucur P, Hofmann M, Menhadji A, Abedi G, Okhunov Z, Rinehart J, Landman J (2016) Comparison of pneumoperitoneum stability between a valveless trocar system and conventional insufflation: a prospective randomized trial. Urology 94:274–280
Galizia G, Prizio G, Lieto E, Castellano P, Pelosio L, Imperatore V, Ferrara A, Pignatelli C (2001) Hemodynamic and pulmonary changes during open, carbon dioxide pneumoperitoneum and abdominal wall-lifting cholecystectomy. A prospective, randomized study. Surg Endosc 15(5):477–483
Acknowledgements
Not applicable.
Funding
This work was supported, in part, by the Kanae Foundation for the Promotion of Medical Science Grant (to H.K.), and the Yasuda Memorial Foundation (Grants−in−Aid for Cancer Research by Young Investigators) (to H.K.).
Author information
Authors and Affiliations
Contributions
KH and IY conceived and designing the study; KH and YM collected and analyzed the data; KH, IY, SY, and ST interpreted the data; KH wrote the manuscript; IY, SY, KM, FK, SN, and ST provided critical revisions that are important for the intellectual content; IY, YM and ST approved the final version of the manuscript. The all authors read and approved the final version of the manuscript.
Corresponding author
Ethics declarations
Conflict of interests
The authors have no relevant financial or non−financial interests to disclose.
Ethical Approval
This study was approved by the ethics committee (IRB) of the Kitasato University School of Medicine (#B22−004), and was performed in accordance with the clinical research guidelines of the IRB of the Kitasato University School of Medicine. All individuals gave written informed consent for pathologic assessment and routine blood sample analyses on their samples, and clinical data. The study was conducted in accordance with the Declaration of Helsinki (as revised in 2013).
Informed Consent
Not applicable.
Additional information
Publisher's Note
Springer Nature remains neutral with regard to jurisdictional claims in published maps and institutional affiliations.
The original online version of this article was revised due to Retrospective Open Access Order plus the same explanatory text of the problem as in the erratum/correction article.
Supplementary Information
Below is the link to the electronic supplementary material.
Supplementary file2 (MP4 12513 KB)
Supplementary file3 (MP4 14166 KB)
Rights and permissions
Open Access This article is licensed under a Creative Commons Attribution 4.0 International License, which permits use, sharing, adaptation, distribution and reproduction in any medium or format, as long as you give appropriate credit to the original author(s) and the source, provide a link to the Creative Commons licence, and indicate if changes were made. The images or other third party material in this article are included in the article's Creative Commons licence, unless indicated otherwise in a credit line to the material. If material is not included in the article's Creative Commons licence and your intended use is not permitted by statutory regulation or exceeds the permitted use, you will need to obtain permission directly from the copyright holder. To view a copy of this licence, visit http://creativecommons.org/licenses/by/4.0/.
About this article
Cite this article
Katoh, H., Ikeda, Y., Saito, Y. et al. The Usefulness of AirSeal™ Intelligent Flow System in Gas Insufflation Total Endoscopic Thyroidectomy. Indian J Otolaryngol Head Neck Surg 75, 115–120 (2023). https://doi.org/10.1007/s12070-022-03257-0
Received:
Accepted:
Published:
Issue Date:
DOI: https://doi.org/10.1007/s12070-022-03257-0