Abstract
Introduction: The incidence of acquired laryngotracheal stenosis is on rise, being caused usually due to prolonged intubation or trauma. Its management has thus become a common clinical challenge for Otolaryngologists and Head and Neck surgeons. Further, with advances in Critical care medicine, Cardiopulmonary surgery and Neurosurgery, the number of intubation-related laryngotracheal injuries is increasing.
Objectives: To assess the outcome of patients who underwent Partial Cricotracheal Resection (PCTR) for subglottic stenosis on basis of pre-defined parameters.
Design of Study: This is a prospective study.
Materials and Methods: Four patients who came to Ear Nose Throat (ENT) department, All India Institute of Medical Sciences (AIIMS) Patna with complaints of either difficult decannulation or stridor, for which PCTR was planned, were included in the study. Surgical resection was done and all patients were followed up for a minimum of 6 months. Postoperatively certain parameters, such as respiration, voice, difficulty in swallowing, feeding and personal satisfaction, were used to evaluate the patients and analyse the efficacy of the surgery.
Results: Three out of four cases came up with complete cure with no dyspnoea, dysphagia, hoarseness of voice. Only one patient could not be extubated and was continued on Ryle’s tube for longer duration compared to other patients.
Conclusion: PCTR is an effective and reliable procedure for management of laryngotracheal stenosis caused due to trauma.
Similar content being viewed by others
Avoid common mistakes on your manuscript.
Introduction
Laryngotracheal stenosis is a complication of prolonged endotracheal intubation in 90% cases [1, 2], and a rare complication of tracheostomy.
Myer et al. proposed a grading system for subglottic stenosis (SGS) based on the size of the endotracheal tube that could be passed through the stenosis. Grade I stenosis has 50% of lumen obstructed, grade II has 50–70% obstruction, grade III with more than 70% obstruction and detectable lumen, while grade IV has no detectable lumen of subglottis [3].
Proper analysis of the stenotic segment guides the treatment adapted. The cause of the stenosis, its location (supraglottic,glottic, subglottic, or combined), the degree of obstruction it has caused, its craniocaudal length, and its association with vocal cord ankylosis or neurogenic paralysis are the factors to be assessed.
Treatment of laryngeal/tracheal stenosis ranges from intraluminal procedures such as endoscopic laser resection with or without dilatation or stenting for grades I and II of SGS;laryngotracheal reconstruction (LTR) with framework expansion by anterior or posterior grafting; or PCTRwith primary anastomosis for themost severe grades of stenosis; and extended PCTR for combined glotto-subglotticstenosis [2].
The assessment of the site, grade and length of the stenotic segment is done most accurately by rigid endoscopy under general anaesthesia, being the diagnostic tool of choice. CT imaging also provides a comprehensive evaluation of the laryngotracheal framework, and is eminently conducive when the lumen is too narrow to be traversed by the endoscope, as in grade IV stenosis, contributing to the length of the stenotic segment and also the condition of the trachea distal to the stenosis [4].
Resection of the stenotic fragment of the laryngotracheal framework gives way for the anastomosis between the healthy ends [5], with restoration of the mucosal lining of the lumen and a high success rate [6, 7]. This makes PCTR the treatment of choice for grades III and IV stenosis according to the Myer–Cotton grading system [8].
For poor surgical risk patients with airway stenosis, the only treatment option is life-long tracheostomy [9].
Cases with difficulty in mobilization of the trachea and when resection of the trachea is quite extensive (more than 5 tracheal rings), a laryngeal release is performed to avoid dehiscence and also restenosis. The formation of granulation tissue at the site of anastomosis increases the likelihood for restenosis and can be prevented by making the sutures emerge submucosally through the cartilage at the edge of the anastomosis [6, 10].
Another advantage of PCTR is preservation of voice quality since the anterior commissure of thelarynx is not manipulated and the posterior glottis is also maintained.
Intraoperative complications of PCTR encountered by various surgeons are vocal cord palsy, pneumothorax, pneumomediastinum, or hypoxia. Immediate post-operative period requires a check to development of subcutaneous emphysema, pneumothorax or pneumomediastinum, infection of the wound, and seroma/hematoma. The patient’s general condition might deteriorate in the post-operative period due to formation of granulation at the site of anastomosis or restenosis, dislodgement of stent, chondritis, aspiration, suprastomal stenosis, trachea-esophageal fistula, anterior commissure asymmetry/ glottis web, posterior glottis stenosis, prolapse of the arytenoids or the epiglottic petiole, or persistent tracheocutaneous fistula [10].
Postoperatively, voice study can be done by: (1) audio/video recorded speech sample; (2) fiberoptic laryngoscopy with stroboscopy; (3) electrolaryngographic recording; (4) standard questionnaire; and (5) spectral voice analysis [10].
Materials and Methods
This prospective study included four patients that presented to the Department of ENT, AIIMS Patna.
Detailed history and examination of each patient was done. One patient had history of cut throat injury by knife during a robbery. The other patient had history of road traffic accident followed by coma and prolonged intubation for more than 15 days. Third patient had history of penetrating injury to neck. Theses all patients had history of laryngotracheal trauma followed by primary repair and tracheostomy at peripheral hospitals. Decannulation was attempted but later presented with dyspnoea and stridor leading to reinsertion of tracheostomy tube.
The fourth patient had history of accidental strangulation by stole(piece of cloth) while on a bike ride. Patient was managed conservatively for 03 days following which she developed dyspnoea. She was then tracheostomised and laryngeal evaluation was done to detect laryngotracheal separation with oesophageal tear.
All these patients presented with difficult decannulation and on evaluation presented with Myer Cotton grade III and grade IV stenosis and were included for study and PCTR surgery. Exclusion crtiteria for surgery included patients with bilateral vocal cord palsy, patient refusing surgery, anterior commisure web, glottis scarring and cricoarytenoid fixation .
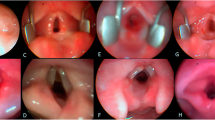
Radiological confirmation was followed by rigid endoscopic examination of each patient under general anaesthesia to assess the extent of stenosis; the location of the stenosis with respect to the vocal cords; and its degree.
The degree of the stenosis was measured by passing endoscope, endotracheal tubes and bougies of different sizes through the stenosed segment. Stenotic segment extended upto 3 tracheal ring length in one patient, two rings were involved in 2 patients and one segment was involved in 1 patient.
The plan for the surgery was finalised.
Surgical steps
For first three of our cases the surgical steps remained the same with minor modifications in each case as per the need. In the last case due to extensive injury following laryngotracheal separation and oesophageal tear, we had to modify surgical steps.
Following surgical steps were common to three cases who came with subglottic stenosis and tracheostomy. They had failed decannulation attempt.
Patients were put under general anaesthesia with neck fully extended.Ryle’s tube insertion was done to palpate oesophagus intraoperatively. New tracheostomy was done caudal to the previous tracheostomy site. Apron incision was given at the level of previously tracheostomised site, and superior and inferior subplatysmal flaps were elevated (Fig. 1). Strap muscles and thyroid isthmus were divided in the midline to expose the trachea (Fig. 2).The trachea was meticulously dissected all around avoiding injury to the recurrent laryngeal nerve and the oesophagus (Fig. 3). Upward advancement of trachea was done by releasing the cartilaginous rings from the mediastinal structures. Dissection of the stenosed segment and involved cricoid arch was done from the adjoining cartilage. Dissection was continued until identification of cricothyroid joints .Excision of stenosed segment was done (Fig. 4).The cricoid plate and the mucosa just below the cricoarytenoid joints were completely exposed after excising the stenotic segment .
Stay sutures from inferior and superior margins were pulled together and margins approximated. The membranous trachea was used to cover the denuded cricoid plate.3 − 0 vicryl interrupted sutures were used for the anastomosis with undermined knots. Care was taken to suture the mucosa of the subglottis inclose approximation with the mucosa of the trachea. Few tension-releasing sutures were also placed between superior and inferior anastomotic segments.Waterseal test was done at the anastomotic site for any leakage.After checking for haemostasisthe wound was closed in layers and a suction drain was placed. At the end of the procedure, the neck was maintained in a flexed position using guardian sutures placed from the chin to the chest. Ryle’s tube was removed after 2 weeks and decannulation of new tracheostomy tube was done on 21st post-operative day.
In fourth patient,laryngotracheal separation with oesophageal tear was encountered. Anterior laryngeal framework was crushed with loss of continuity. Severed cartilage pieces were excised and mobilisation of proximal and distal tracheal segments were done.After freshening of margins, anastomosis was done with reconstruction of anterior wall with myocutaneous flaps. Oesophageal tear was repaired and feeding jejunostomy done. Post-operative period was uneventful. Patient was evaluated after one month and bilateral vocal cord movements were intact. Feeding jejunostomy was removed after three months. Decannulation was tried but patient was unable to tolerate.Patient was re-evaluated under general anaesthesia with rigid endoscope after 6 months of surgery. Intraoperative findings consist of partially collapsed anterior tracheal wall with fibrotic bands. Fibrotic adhesive bands were removed and Montgomery T tube insertion was done. Patient was kept under regular follow up. Mitomycin C application was done for granulation tissue in situ. Patient was lost in follow up during COVID 19 pandemic in 2020. When the patient returned after a year, laryngeal evaluation was done with bilateral vocal cords mobile and T tube was removed.
The patients were followed up for a minimum of 6 months post operatively, all patients were subjected to laryngeal endoscopic examination along with adetailed analysis of selected parameters that included time for decannulation after primary repair, exertional dyspnoea after decannulation postoperatively, noisy breathing if any, voice quality, difficulty in swallowing and coughing if any.
Results
Two types of tracheal strictures following tracheostomy have been described - the first type are non-infected, fibrous strictures developing over a period of time; and the second type are soft strictures, appearing few days after removal of the tracheostomy tube, with granulation tissue at the site of stricture and possibilities of infection. Three cases included in our study had fibrous strictures that lead to stridor after a certain period of decannulation.
Decannulation was successfully done in 3 out of 4 patients (75%).One patient could not be decannulated owing to aspiration.Normal speech was achieved in 3 (75%) patients with effortless breathing and swallowing in 3(75%) of them. One patient had difficulty in swallowing, which improved at 6weeks of follow up. Duration of intubation, length of the resected segment and previous open airway interventions were reported to have a significant negative impact on the outcome of surgery.
Early detection and planned intervention is of paramount importance in arresting the progression to late stenosis. For each case, endoscopic examination of larynx beforedecannulation and 3 weeks postoperatively was performed to detect signs of restenosis. None of the patients developed dehiscence or restenosis over an average period of 6 months of follow up (Table 1 and 2).
Discussion
In 1953, Conley described cricotracheal resection in adults for the first time [11], while Gerwat and Bryce [12] did the first pediatric resection. Grillo et al. [13], and Monnier and co-workers, in 1990s, reported further advancements in the procedure [14, 15, 16, 17].
Laryngotracheal stenosis is a challenging complication related to endotracheal intubation and requires a multidisciplinary approach for diagnosis and management [30].
Rigid endoscopic evaluation of the larynx and trachea under general anesthesia remained the gold standardfor the assessment of the site, length and grade of the stenotic segment.
CT imaging is also an indespensible tool especially in grade IV stenosis when the lumen is too stenotic to be traversed by the endoscope. In this situation CT imaging is very helpful to assess the length of the stenotic segment and the condition of the distal trachea to exclude associated distal stenosis [4].
In our study, three out of four patients were decannulated successfully with normal voice and no complain in swallowing and breathing. All the four patients had both vocal cords mobile in post operative laryngeal evaluation. One patient with laryngeotracheal separation could not be decannulated due to aspiration.
Many studies have been done to investigate the potential role of the factors that affect the success of PCTR/TRA. Certain associations were found with the failure of the procedure, such as extremes of age, and comorbidities (cardiac pathologies, diabetes, pulmonary diseases and concomitant airway pathologies) [18, 19, 20, 21, 22]. Laryngeal or cricoid involvement [21], vocal fold paralysis [23, 24], grade of stenosis [25] and length of the stenotic segment [21, 25] were other factors considered. In our study,only one patient had laryngotracheal separation along with oesophageal tear as factors influencing the post operative outcome, leading to difficult decannulation, aphonia and delayed rehabilitation of swallowing. Hartley et al. [24] and Ludemann et al. [26] identified Methicillin-resistant Staphylococcus aureus (MRSA) [24], respiratory syncytial virus pneumonitis andpseudomonal wound infection26as the causative factors for failure in certain cases. Halstead [27] and Walner et al. [28] described gastroesophageal reflux (GER), to haveassociation with failure in PCTR.
In the study by Monnier et al. [29], there was improvement in voice quality in 70% of patients, which corresponds with our result.
In our study, none of our patients developed any complications postoperatively.
Conclusion
Treatment of post traumatic subglottic or upper tracheal stenosis by PCTR has a high success rate with preservation of quality of voice,but primarily depends on the preoperative condition of the patient, which includes comorbidities and previous history of any airway intervention; and the degree and length of stenosis.
The rate of decannulation remains the single most important parameter in surgical procedures intended for the treatment of subglottic stenosis [29]. According to this measure, PCTR compares favourably with other treatment modalities and should be considered as treatment of choice for grades III and IV stenoses [29].
References
Nakache G, Primov-Fever A, Alon E, Wolf M, Ref C (2015) ( https://doi.org/10.1007/s00405-015-3575-z)
See GB, Sankaran R, Baki MM, Mohamed AS (2014) Partial cricotracheal resection (PCTR), a rewarding outcome for paediatric subglottic stenosis: an early experience. Med J Malaysia. 69: pp. 13 Cross Ref https://doi.org/10.1177/201010581402300103)
Myer CM, OConnor DM, Cotton RT (1994) : Proposed grading system for subglottic stenosis based on endotracheal tube sizes. Ann OtolRhinolLaryngol103:319–323
El-Fattah A, Kamal E, Amer H, Fouda M, Elwahab A, Tawfik A (2011) : Cervical tracheal resection with cricotracheal anastomosis: experience in adults with grade III–IV tracheal stenosis. JLaryngol Otol ; 125: pp. 614–619 Cross Ref (https://doi.org/10.1017/S0022215110002537)
Piazza C, Del Bon F, Paderno A, Grazioli P, Mangili S, Lombardi D, Ref (2014) (https://doi.org/10.1177/0003489414538764)
Cordos I, Bolca C, Paleru C, Posea R, Stoica R, Ref C (2009) ( https://doi.org/10.1510/icvts.2008.184747).
Marques P, Leal L, Spratley J, Cardoso E, Santos M, Ref C (2009) ( https://doi.org/10.1016/j.amjoto.2008.08.008).
Myer CM, O’Connor DM, Cotton RT, Ref (1994) (https://doi.org/10.1177/000348949410300410)
Nandakumar R, Jagdish C, Prathibha C, Shilpa C, Sreenivas V, Balasubramanya A et al (2011) Tracheal resection with end-to-end anastomosis for post-intubation cervical tracheal stenosis: study of 14 cases. J LaryngolOtol 125:958–961. https://doi.org/10.1017/S002221511100137X). Cross Ref
Cotton Robin T (2000 Feb) Management of subglottic stenosis. Otolaryngol Clin North Am 33(1):111–130
Conley JJ, Ref C (1953) ( https://doi.org/10.1177/000348945306200219)
Gerwat J, Bryce DP (1974) The management of subglottic laryngeal stenosis by resection and direct anastomosis. Laryngoscope 84:940–957
Grillo HC, Mathisen DJ, Wain JC (1992) Laryngotracheal resection and reconstruction for subglottic stenosis. Ann ThoracSurg 53:54–63
Monnier P, Lang F, Savary M (1998) Partial cricotracheal resection for severe pediatric subglottic stenosis: update of the Lausanne experience. Ann OtolRhinolLaryngol 107:961–968
Monnier P, Savary M, Chapuis G (1993) Partial cricoid resection with primary tracheal anastomosis for subglottic stenosis in infants and children. Laryngoscope 103:1273–1283
Monnier P, Lang F, Savary M, Ref C (2003) ( https://doi.org/10.1007/s00405-002-0465-y)
Monnier P, Lang F, Savary M (1999) : Cricotracheal resection for pediatric subglottic stenosis. Int J PediatrOtorhinolaryngol ; 49: pp. S283-S286 Cross Ref (https://doi.org/10.1016/s0165-5876(99)00175-5)
White DR, Cotton RT, Bean JA, Rutter MJ (2005) Pediatriccricotracheal resection: surgical outcomes and risk factor analysis. Arch Otolaryngol Head Neck Surg 131:896–899
Wright CD, Grillo HC, Wain JC, Wong DR, Donahue DM, Gaissert HA et al (2004) Anastomotic complications after tracheal resection: prognostic factors and management. J ThoracCardiovasc Surg 128:731–739
Wolf M, Shapira Y, Talmi YP, Novikov I, Kronenberg J, Yellin A, Ref C (2001) ( https://doi.org/10.1097/00005537-200104000-00012)
Abbasidezfouli A, Akbarian E, Shadmehr MB, Arab M, Javaherzadeh M, Pejhan S, Ref (2009) (https://doi.org/10.1510/icvts.2009.202978)
Donahue DM, Grillo HC, Wain JC, Wright CD, Mathisen DJ, Ref C (1997) ( https://doi.org/10.1016/S0022-5223(97)70007-2)
Grillo HC, Mathisen DJ, Wright CD, Ashiku SK, Wain JC, Ref (2003) (https://doi.org/10.1177/000348940311200909)
Hartley BE, Rutter MJ, Cotton RT (2000) Cricotracheal resection as a primary procedure for laryngotracheal stenosis in children. Int J PediatrOtorhinolaryngol 54:133–136
Grillo HC, Donahue DM, Mathisen DJ, Wain JC, Wright CD (1995) Postintubation tracheal stenosis: treatment and results. J Thorac Cardiovasc Surg 109:486–493. https://doi.org/10.1016/S0022-5223(95)70279-2). Cross Ref
Ludemann JP, Noah Z, Hughes CA, Holinger LD, Ref (1999) (https://doi.org/10.1177/000348949910801101)
Halstead LA, Ref C (1999) ( https://doi.org/10.1053/hn.1999.v120.a91766)
Walner DL, Stern Y, Gerber ME, Rudolph C, Baldwin CY, Cotton RT (1998) Gastroesophageal reflux in patients with subglottic stenosis. Arch Otolaryngol Head Neck Surg 124:551–555. https://doi.org/10.1001/archotol.124.5.551). Cross Ref
Jacquet Y, Lang F, Pilloud R, Savary M, Monnier P (2005) Partial cricotracheal resection for pediatric subglottic stenosis: Long term outcome in 57 patients. J Thorac Cardiovasc Surg 130:726–732
Stauffer JL, Olson DE, Petty TL, Ref C (1981) ( https://doi.org/10.1016/0002-9343(81)90413-7)
Funding
This research did not receive any specific grant from funding agencies in the public, commercial, or not-for-profit sectors.
Author information
Authors and Affiliations
Corresponding author
Ethics declarations
Ethics
Approval was obtained from the ethics committee.
Informed Consent
Proper consent was taken from patients.
Declarations of interest
None.
Additional information
Publisher’s Note
Springer Nature remains neutral with regard to jurisdictional claims in published maps and institutional affiliations.
Rights and permissions
Springer Nature or its licensor holds exclusive rights to this article under a publishing agreement with the author(s) or other rightsholder(s); author self-archiving of the accepted manuscript version of this article is solely governed by the terms of such publishing agreement and applicable law.
About this article
Cite this article
Bhawana, K., Kumar, D. & Bharti, B. Partial Cricotracheal Resection – Our Experience. Indian J Otolaryngol Head Neck Surg 75, 292–298 (2023). https://doi.org/10.1007/s12070-022-03155-5
Received:
Accepted:
Published:
Issue Date:
DOI: https://doi.org/10.1007/s12070-022-03155-5