Abstract
This research investigates the mediation of resilience abilities on the relationship between Industry 4.0 technologies adoption and healthcare supply chain performance during the COVID-19 outbreak in Brazil and India. We surveyed 179 practitioners from organizations at different tiers of the healthcare supply chain (e.g., manufacturers, distributors, and care providers) in July 2021. Multivariate data techniques are used to the collected data to verify the hypotheses anchored on concepts from resource dependence theory. We identify two constructs of Industry 4.0 technologies (named after their predominant roles) and two constructs of resilience abilities (named according to the main abilities encompassed). Our findings indicate that resilience abilities mediate the impact of Industry 4.0 technologies on the performance of the healthcare supply chain since the beginning of the COVID-19 pandemic. However, the role played by adaptive and restorative abilities seems more prominent than the one played by anticipation and monitoring abilities. Further, sensing and communication technologies directly affect the healthcare supply chain’s performance. Our study brings together three emerging topics related to the literature on the healthcare supply chain (Industry 4.0 adoption, resilience abilities development, and the disruptions caused by the COVID-19 pandemic). Although digitalization of the healthcare supply chain does improve its performance, our research indicated that its impact could be significantly enhanced when resilience abilities are concurrently developed, particularly in the Indian and Brazilian contexts.
Similar content being viewed by others
Avoid common mistakes on your manuscript.
1 Introduction
The occurrence of severe disruptive events over the past decades, such as the 9/11 terrorist acts in New York, USA, in 2001 (Bueno-Solano and Cedillo-Campos 2014) and the Tohoku earthquake in Japan in 2011 (Matsuo 2015), have raised the attention of organizations and academics to the existing vulnerability of global supply chains. Such severe disruptions usually imply significant financial and operational losses to various industry sectors across multiple countries (Snyder et al. 2016; Zaman et al. 2016). More recently, the worldwide pandemic of a new coronavirus infection (COVID-19) has caused unexpected disruptions that vary from reducing demand for some firms to increasing it for others (Krammer 2021). Globally, it resulted in uncertainty in getting raw materials, impacting the capability to send and receive goods in time due to shortages and logistics bottlenecks and lack of labor capacity to manufacture products (Ivanov and Das 2020; Zanni 2020).
Expectedly, being the pandemic a health disaster, the healthcare supply chain was one of the most affected sectors. The COVID-19 pandemic has raised significant glitches in the healthcare supply chain (Mirchandani 2020), particularly regarding services involved in the containment of the infection and those related to preventive care (Govindan et al. 2020; Gereffi 2020; Sharma et al. 2020). According to World Health Organization (2020), tough decisions have been made to adequate the demands of timely response to the pandemic with the need to keep the essential health treatments. Such a scenario aggravated the urgency for consistently developing resilience throughout the healthcare supply chain (Rosa et al. 2021). Resilience is the system’s capacity to cope with the implications of risk events that cannot be avoided, returning to its original state or moving to a post-disruption state equivalent to or improved in terms of efficiency (Hosseini et al. 2019). Thus, a resilient healthcare supply chain would address countermeasures that allow it to absorb the impacts of the COVID-19 pandemic, adapt to them and, eventually, at least recover its normal performance (Rosa et al. 2021; Usman et al. 2022).
Among the existing countermeasures, the digital transformation promoted by the Fourth Industrial Revolution (a.k.a. Industry 4.0) has been claimed as an effective way to foster supply chain resilience (Ivanov et al. 2019; Ivanov and Dolgui 2020). Because traditional supply chain management practices may be very basic to address the complexities of supply chain risk interactions (Pettit et al. 2019), the integration of new technologies from Industry 4.0 can help maintain (or even improve) supply chain performance in disruptive scenarios (Cavalcante et al. 2019). A few empirical studies (e.g., Ralston and Blackhurst, 2020; Narayanamurthy and Tortorella, 2021) have already indicated the benefits of Industry 4.0 adoption to cope with disruptions, such as the pandemic. Industry 4.0 technologies can support more assertive forecasting and identification of phenomena, assuring a proactive and more responsive supply chain (Frederico et al. 2020). Thus, Industry 4.0 technologies enable supply chain agents to cope more effectively with disruptions, thereby minimizing their undesired implications (Shao et al., 2020).
Nevertheless, the digital transformation of supply chains is still in its early stages (Queiroz and Telles 2018; Shao et al., 2020; Awan et al., 2022; Shaheen et al., 2022), particularly the healthcare supply chain. Additionally, evidence on the contribution of Industry 4.0 integration to the resilience of the healthcare supply chain is scarce (Tortorella et al. 2021a, b, c), impairing the achievement of a comprehensive understanding of the topic and characterizing a theoretical gap in the literature. Against this backdrop, two research questions (RQs) emerge:
RQ 1
What is the impact of Industry 4.0 adoption on the development of resilience throughout the entire healthcare supply chain during the COVID-19 outbreak?
RQ 2
What is the role of resilience development in the relationship between Industry 4.0 adoption and healthcare supply chain performance during the COVID-19 outbreak?
To address those RQs, this research investigates the mediating role of resilience abilities on the relationship between Industry 4.0 technologies adoption and healthcare supply chain performance during the COVID-19 pandemic. 179 practitioners from organizations at multiple tiers of the healthcare supply chain (e.g., manufacturers, distributors, and care providers) in countries severely affected by the pandemic, such as Brazil and India, were surveyed. Multivariate data analysis was adopted to verify the validity of our hypotheses. This research is grounded on concepts from the resource dependence theory, which states that the external resources of organizations affect their behavior (Pfeffer and Salancik 1978). This theory has been used to frame many studies on supply chain management (e.g., Lavassani and Movahedi 2010; Sarkis et al., 2011; Manzouri and Rahman, 2013), justifying its adoption in our research.
The contribution of this research is two-fold. First, in theoretical terms, this study helps bridge the knowledge gap on topics still relatively new to researchers and academics, such as Industry 4.0, resilience development, and implications of the COVID-19 pandemic. Since the pandemic’s beginning, the healthcare supply chain has faced significant challenges that resulted in different strategies to reduce uncertainty and rapidly return to pre-pandemic operational performance (Khan et al. 2021a, b, c; Kumar et al. 2022). The empirical verification of the roles of Industry 4.0 technologies and resilience abilities on the performance of the healthcare supply chain help mitigate the effect of power and uncertainty in the supply chain during disruptive events. Second, from a practical standpoint, this research provides practitioners from the healthcare supply chain arguments to systemically guide and prioritize their digitalization efforts towards a more resilient supply chain. Since both Industry 4.0 adoption and the development of resilience abilities demand great efforts (Sriyanto et al. 2021; Khan et al. 2022a, b), the sooner the healthcare supply chain collaboratively addresses these initiatives, the more prepared it will be to cope with future disruptive events. Although digitalization of the healthcare supply chain does improve its performance, our research indicated that its impact could be significantly enhanced when resilience abilities are concurrently developed, particularly in the Indian and Brazilian contexts.
The remaining of this paper is structured as follows. Section 2 provides the background on the main concepts discussed in this research. Based on such concepts, Sect. 3 formulates the hypotheses investigated. Section 4 describes the research method, whose results are presented and discussed in Sect. 5. Section 6 concludes the paper and offers future research opportunities.
2 Background
This section offers the theoretical background on the topics that form the fundamental concepts approached in our study. Hence, it is divided into five different and interrelated sections to properly present the body of knowledge on (i) Industry 4.0 and supply chain management, (ii) resilient supply chain, (iii) Industry 4.0 and healthcare, (iv) the healthcare supply chain, and (v) resource dependence theory.
2.1 Industry 4.0 and Supply Chain management
The integration of Industry 4.0 technologies into supply chain management has allowed higher interconnectivity between businesses, extending from an isolated, local, and single-company adoption to a supply chain-comprehensive application (Wu et al. 2016). In other words, digital transformation has forced supply chain management to evolve from a linear model to a more integrated one in which data moves in several directions (Ivanov and Dolgui 2020). That has promoted an intense collection of data, communication in real-time among tiers, smart decision-making, and effective and adaptive processes (Shao et al., 2020).
Many researchers have developed guidelines to properly incorporate Industry 4.0 technologies into supply chains. For instance, Shao et al. (2020) proposed four implementation stages: (i) visualization, (ii) first-level linkage, (iii) connected supply chain, and (iv) smart supply chain. Similarly, Frederico et al. (2020) presented a framework for integrating Industry 4.0 into supply chains that encompasses 21 dimensions categorized into four main constructs: (i) managerial and capability supporters, (ii) technology levers, (iii) processes performance requirements, and (iv) strategic outcomes. Queiroz et al. (2019) developed a framework comprised of seven supply chain capabilities supported by six Industry 4.0 technologies: big data analytics, blockchain, artificial intelligence, cloud computing, cyber-physical systems, and the Internet-of-Things (IoT). Despite certain specificities, studies were usually grounded on a common set of technologies with diversified applications. Table 1 synthesizes frequently reported technologies in Industry 4.0 and supply chain management literature.
2.2 Resilient supply chain
Resilience in the supply chain refers to the ability to restore the operational condition (or an improved one) within a reasonable period after disruptive events (Brandon-Jones et al. 2014). Coping with unplanned disruptions is a characteristic of resilient supply chains (Krause et al. 2009) accomplished by continuous control of the context in which the supply chain is inserted so that it can anticipate and adapt accordingly (Ambulkar et al. 2015), yielding the expected performance (Dolgui et al. 2020). The development of supply chain resilience has been fostered through different mechanisms, such as reinforcing vertical and horizontal collaboration in the supply chain, purchasing from redundant suppliers, ensuring capacity slack, determining a demand pool, balancing the import and export of goods, and considering the trade-offs between vertical integration and outsourcing (Tang 2006; Pettit et al. 2010; Wieland and Wallenburg 2013; Scholten and Schilder 2015; Gu et al. 2020).
Despite the apparent consensus on the meaning of resilience in supply chains, information on its formative components is somewhat sparse due to the overlaps in the concepts. In general, the components detail the readiness, response, and restorative abilities necessary to supply chain resilience (Jüttner and Maklan 2011; Hollnagel 2014, 2017), for instance, suggested four interrelated abilities of resilient systems (i.e., monitor, anticipate, respond, and learn), while Briano et al. (2009) complemented them with flexibility, velocity, visibility, and collaboration. Hosseini et al. (2019) built on Biringer et al.‘s (2013) work to conceptualize three supply chain resilience capabilities: absorptive, adaptive, and restorative. Despite the variety of terminologies, the inherent abilities of supply chain resilience are relatively intuitive, and eight main abilities were consolidated in Table 2, providing a conceptual basis for our study.
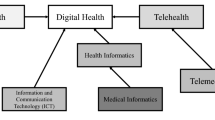
2.3 Industry 4.0 and healthcare
The application of Industry 4.0 technologies into healthcare seeks to provide customized care in real-time, moving hospitals to organizations centered on patients, whose departments actively engage towards the achievement of the best health service (Sannino et al. 2018; Tortorella et al. 2020a; Massaro 2021). Industry 4.0 technologies (e.g., cloud computing, IoT, and big data) have been combined and integrated into healthcare treatments and processes so that healthcare systems can monitor, track and store records from patients for better care (Elhoseny et al. 2018; Wu et al. 2018; Khodadad-Saryazdi 2021). Such integration has also been denoted Healthcare 4.0 (H4.0) (Thuemmler and Bai, 2017).
Motivated by the digitalization frenzy from the Fourth Industrial Revolution, researchers’ interest in Healthcare 4.0 has increased over the last few years, leading them to explore the topic from complementary perspectives and at different levels. In terms of health treatments, most studies applied Healthcare 4.0 to measure and control vital parameters of patients, such as body fat (Kim and Choi 2016), physiological biometrics (Hamidi 2019), heartbeat rate (Jeong et al. 2016), and blood pressure (Wan et al. 2018). When considering administrative processes, a similar set of technologies has been introduced into the management of diseases and drugs (Elhoseny et al. 2018) and clinical factors (Garai et al. 2017), evidencing the versatility of Healthcare 4.0 implementation. At an organizational level, Tortorella et al. (2020b) examined the effects of contextual factors on the overall adoption of H4.0. Rosa et al. (2021) studied the association between Healthcare 4.0 adoption and the achievement of resilience in healthcare.
As the principles and technologies from Industry 4.0 are increasingly extended to Healthcare 4.0, new challenges and benefits also emerge for its full implementation. Regarding challenges, Tortorella et al. (2020c) indicated that understanding the implications of social (e.g., misalignment with hospital’s strategy) and technical (e.g., information security risks) barriers are equally relevant. Pan et al. (2019) corroborated this by stating that Healthcare 4.0 adoption might find resistance from physicians, who often see automated systems for clinical decision-making as their substitutes. Concerning benefits, Pramanik et al. (2017) argued that Healthcare 4.0 promotes innovative and transforming health services, reducing their costs (Tortorella et al. 2020d) and increasing the effectiveness of internal and cross-hospital processes (Alloghani et al. 2018). Overall, integrating Industry 4.0 into healthcare treatments is claimed to positively impact hospitals’ performance in the short term. In addition, Industry 4.0 incorporation into administrative processes might influence performance in the longer term (Das et al. 2011).
2.4 The healthcare supply chain
Health systems are conceptualized as all organizations, people, and actions that primarily aim to foster, recover or provide health, including, for instance, a mother taking care of a sick son (World Health Organization, 2007). The concept of a health system also encompasses the interrelationships throughout the healthcare supply chain, focusing on improving health, equity, and responsiveness to legitimate expectations (White 2015). Such a concept reinforces the need for systemically addressing improvement opportunities throughout the healthcare supply chain (Rosa et al. 2021; Tortorella et al. 2021a), as materials represent between 25% and 30% of a hospital’s cost (Roark 2005).
The healthcare supply chain is denoted by its intricacies, resulting from the various utilized supplies and the numerous distribution channels (Borges et al. 2019). The structure of the healthcare supply chain might change depending on the emphasis given by researchers. For instance, Haszlinna Mustaffa and Potter (2009), and Matthew et al. (2013) divided the healthcare supply chain into: (i) manufacturers, which involve the manufacturing of medical equipment, materials, and goods for health treatment; (ii) distributors, who manage the logistics of those items; (iii) wholesalers, who consolidate the items and sell them in large quantities at lower prices; and (iv) caregivers, such as hospitals and medical clinics, that use the items to treat patients. Kritchanchai (2014) considered the tier levels above and added another, denoted as payers, represented by government, patients, and employers. However, because most hospitals need to handle their own supplies and patients at each unit, healthcare supply chains may also be viewed as external or internal. The external supply chain includes negotiation, purchasing and logistics of supplies, and technical assistance and maintenance (Rakovska and Stratieva 2018). The internal supply chain consists of storing, consolidating, distributing, and managing these supplies (Moons et al. 2019).
The healthcare supply chain deals with various challenges inherent to the sector (Ageron et al. 2018). First, the constant technological advances result in shorter product life cycles and higher costs of medical items. Second, it is challenging to predict patients’ frequency and duration of care and primary diagnoses (McKone-Sweet et al. 2005). Further, the unstandardized nomenclature and coding of goods create confusion and misguidance in the sector. Low supply chain orientation and scarcity of capital to establish an adequate infrastructure for information technologies are also barriers to higher efficiency (Mathur et al. 2018). Finally, agents usually operate solely in their own best interests, which significantly limits the development of the healthcare supply chain (Yanamandra 2018). The impact of those challenges is even greater when considering the occurrence of disruptions (Aldrighetti et al. 2019), which motivates the development of resilience in healthcare settings (Tortorella et al. 2021b). In this sense, adopting an adequate theoretical lens may support understanding the intricacies of the healthcare supply chain and its challenges for developing resilience and digitizing while coping with COVID-19 implications. The resource dependence theory is adopted in our study due to the suitability of its concepts and assumptions to the investigated phenomenon.
2.5 Resource dependence theory
Since the seminal proposition by Pfeffer and Salancik in 1978, resource dependence has been deemed an important theory in organizational and strategic management (Hillman et al. 2009). It assumes that organizations are open systems dependent on exogenous contingencies, although managers can mitigate such environmental uncertainty and dependence (Pfeffer and Salancik 1978). In this sense, organizations are expected to develop countermeasures to reduce others’ influence while simultaneously enhancing their own influence capability (Ulrich and Barney 1984). Thus, resource dependence theory provides the fundamental arguments for understanding inter-organizational relationships, indicating that organizations are not autonomous but limited by a network of interdependencies (Biermann and Harsch 2017). Such interdependencies affect both inter-organizational and intra-organizational power, yielding changes in organizational behavior (Drees and Heugens 2013).
Due to its generalizability, resource dependence theory has been widely used to frame studies on supply chain management, as pointed out in a literature review by Lavassani and Movahedi 2010. In another literature review, Sarkis et al. (2011) focused on green supply chain management and identified concepts from resource dependence theory in most studies surveyed. Similarly, Manzouri and Rahman (2013) investigated lean supply chain management studies and classified five lean principles according to the resource dependence theory. More recently, Kim et al. (2020) used the theory’s assumptions to identify three antecedents of logistics integration: trust, commitment, and satisfaction. Overall, the versatility and pervasiveness of resource dependence theory concepts have supported the advance of the body of knowledge on supply chain management. As the development of resilience and digitalization of the healthcare supply chain are relatively recent topics, we anchored our study on this theory to empirically verify and better understand the underlying relationships.
3 Hypotheses development
The adoption of Industry 4.0 technologies is claimed to improve the supply chain, particularly regarding procurement, production, management of inventory, and trading (Fosso Wamba et al. 2018; Frederico et al. 2020). Such adoption fosters more effective information sharing throughout the supply chain (Factorachian and Kazemi, 2021). Industry 4.0’s effects are evidenced at different supply chain tiers since they allow for precise forecasts and plans, enhance the traceability of supplies, and establish smart warehouses and distribution (Hahn 2020). Such Industry 4.0 contributions have been reported as critical for companies willing to cope with the implications of the pandemic (Narayanamurthy and Tortorella 2021).
Although studies have suggested a positive relationship between Industry 4.0 technologies and healthcare services’ resilience (Rosa et al. 2021; Tortorella et al. 2021a), they solely approached hospitals or medical clinics, neglecting the broader impacts of Industry 4.0 on the resilience of other supply chain agents. Moreover, as Yanamandra (2018) indicated, due to the diversified interests among agents and stakeholders, the contribution of Industry 4.0 technologies might occur differently throughout the healthcare supply chain tiers. Nevertheless, the severe disruptions implied by the COVID-19 outbreak have triggered closer collaboration among the healthcare supply chain agents, whose improvement efforts seemed to align with the same goal (Paché 2020). In addition, the wide geographic distribution of the healthcare supply chain agents, the surge in demand for materials, equipment, and medical products, and the restrictions on social and business interactions to contain the pandemic (Gereffi 2020; Sharma et al. 2020) have framed a scenario in which technologies that favor a more effective communication and information sharing are likely to support a more resilient system.
Based on resource dependence theory (Pfeffer and Salancik 1978), organizations depend on multiple resources (e.g., labor, capital, raw material), making it challenging to develop all-embracing countervailing initiatives. Hence, organizations must deal with the criticality and scarcity principle (Hillman et al. 2009), which pushes them to adopt various balancing strategies in closer collaboration with suppliers, partners, or customers. The healthcare supply chain encompasses various organizations and flows that add a significant amount of complexity for its effective management (Aldrighetti et al. 2019). The performance of such fragmented and complex supply chain can be easily affected by the disruption of a single product or agent. The criticality and scarcity of those resources observed during the pandemic have compelled organizations to collaborate beyond their individual interests, propelling a more resilient healthcare supply chain. Therefore, the ability to cope and adjust to those disruptions supported by the integration of Industry 4.0 technologies is likely to positively affect the healthcare supply chain performance, as conceptually illustrated in Fig. 1. To examine that, we formulate the following hypotheses:
H 1
The adoption of Industry 4.0 technologies positively impacts the development of resilience in the entire healthcare supply chain during disruptive events, such as the COVID-19 outbreak.
H 2
The development of resilience abilities positively mediates the relationship between the adoption of Industry 4.0 technologies and the performance of the healthcare supply chain during disruptive events, such as the COVID-19 outbreak.
4 Method
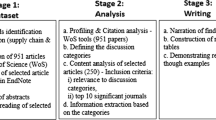
The methodological procedure of our study followed an empirical approach, which is a recommended way of capturing knowledge by directly and/or indirectly observing the phenomenon (Goodwin 2005). Quantifying data based on the perceptions of specifically selected participants is quite frequent and might support the investigation of our research questions. Survey is one of the methods most commonly used to collect empirical evidence, as it usually presents potentially good representativeness and statistical significance, lower costs, and is a standardized instrument for data collection (Montgomery 2013). Therefore, the method conducted in our survey-based research consisted of four main steps: (i) development of instrument and measures; (ii) selection and characterization of sample; (iii) verification of constructs’ validity and reliability; and (iv) data analysis. These steps are described below.
4.1 Development of the instrument and measures
The survey instrument was comprised of four parts (see Appendix). In the first part, we asked respondents about the characteristics of their organizations and themselves to determine the profile of our sample. Then, the adoption level of Industry 4.0 technologies was assessed based on a 5-point scale, in which ‘1’ represented no adoption and ‘5’ indicated full adoption. The nine technologies consolidated in Table 1 were used as measures. Although the adoption of Industry 4.0 may involve other aspects beyond technologies (e.g., system design principles), utilizing the adoption level of new technologies (e.g., IoT, cloud computing, and big data) as a proxy for Industry 4.0 implementation level has been already evidenced in previous studies of similar nature (e.g., Rossini et al., 2019; Tortorella et al., 2020c). In the third part, we gathered data on the development level of the eight resilience abilities listed in Table 2 in the respondents’ organizations. We adopted a 5-point scale, varying from 1 (not developed) to 5 (fully developed). Finally, participants were invited to score the variation in performance in their organizations since the COVID-19 outbreak (i.e., January 2020). Changes in performance are often more easily noticed; hence, utilizing this data as a proxy for performance enhances the validity of answers, particularly when those consist of opinions from middle managers (Tortorella et al. 2019). Further, in designing our survey instrument, we followed the guidelines from Stone (1993) and Boparai et al. (2018), which particularly stated the issues related to very long questionnaires. Based on the works from Akyuz and Erkan (2010) and Guersola et al. (2018) on supply chain performance, we selected four performance indicators (i.e., quality, cost, delivery, and inventory level) that were more likely to be relevant for all tiers and organizations included in the healthcare supply chain. Those indicators were evaluated through a 5-point scale that varied from 1 (significantly worsened) to 5 (significantly improved).
Three experts (two academicians and one practitioner) tested the instrument to evaluate its face and content validity, following recommendations in Kothari (2004). They proposed minor improvements in the terminology of some measures. Common method variance was potentially an issue since we applied psychometric scales to collect perceptions from multiple participants (Huber and Power 1985). To curb that, we designed the questionnaire to ensure the dependent and independent variables were far apart (Podsakoff and Organ 1986). Anonymity and confidentiality of responses were informed upfront. Also, participants were told that there were no correct answers (Podsakoff et al. 2003). Finally, we used Harman’s single-factor test (Malhotra et al. 2006), including all variables, to check whether a single factor represented most of the responses’ variance. Results indicated that the first factor explained 21.56% of the total variance, implying that we could disregard common method bias.
4.2 Selection and characterization of the sample
We used a non-random approach based on five pre-established criteria (Smith 1983). First, respondents should be practitioners from organizations that belong to the healthcare supply chain, such as manufacturers (e.g., pharmaceutical, medical device, surgical or medical equipment), distributors or group purchasing organizations (GPO), and care providers (e.g., hospital, clinic, pharmacy). Second, as our goal was to verify the performance variation of those organizations since the COVID-19 outbreak, we targeted respondents located in countries highly affected by the pandemic. At the time of this research, the three countries with the highest number of infected cases and deaths due to COVID-19 were the USA, India, and Brazil (Worldometer 2021). Two factors drove our choice of restricting data collection to Indian and Brazilian organizations: (i) the American socioeconomic context (developed economy) differs from India and Brazil (emerging economies), which might affect the likelihood of Industry 4.0 adoption (Tortorella et al. 2021d), and (ii) the healthcare systems in Brazil and India share similar challenges and characteristics (Marten et al. 2014), offering a relevant and consistent context for analysis and justifying the sole inclusion of respondents located in both countries. Third, we aimed at participants who were middle managers in their respective organizations. Middle managers are usually in charge of deploying organizational strategies into operational processes and activities, leading the organization’s actual changes (Van Dun et al. 2017). Fourth, all surveyed organizations should already have some digitalization initiatives. Meeting this criterion would ensure a minimum familiarity with Industry 4.0 technologies. Finally, due to its high level of complexity, we involved respondents with diversified backgrounds (i.e., clinician and non-clinician), allowing a more holistic perception of the healthcare supply chain.
Based on the characteristics of the healthcare supply chain, we followed the procedure proposed in previous studies (e.g., Tortorella et al., 2017; 2018; Marodin et al., 2019; Moyano-Fuentes et al., 2019), in which researchers considered the respondents’ organizations as the unit of analysis and analyzed the data controlling for the effect of contextual characteristics, such as firm size and tier level. In this sense, we collected information from selected key informants (i.e., middle managers with different backgrounds working in organizations from the healthcare supply chain undergoing digitalization) who provided perceptions about their own organizations. That ensured a more legitimate opinion.
Data were collected during July 2021. An e-mail with the questionnaire link was sent to potential participants. In total, 687 respondents were initially contacted, from which 179 (26.1% response rate) fully responded to the questionnaire (see Table 3). Most participants were in India (56.2%) and had a non-clinician background (74.3%). A well-balanced sample was obtained regarding the healthcare supply chain tiers; i.e., 27.4% were categorized as manufacturers, 36.9% were distributors, and 35.7% were care providers. Finally, participants were predominantly from organizations with less than 100 employees (42.4%).
4.3 Verification of constructs’ validity and reliability
To verify the latent constructs using the questionnaire responses, three Exploratory Factor Analysis (EFA) using Principal Component (PC) extraction were conducted (Fabrigar et al. 1999). EFA is often adopted when no a priori hypothesis on factors or patterns of measured variables is known (Finch and West 1997). A similar approach has been adopted in research of the same nature (e.g., Tortorella et al., 2020c; Narayanamurthy and Tortorella, 2021).
An initial EFA was run using the four operational performance indicators as measures (see Table 4). The first PC resulted in high factor loadings (> 0.45; Hair et al., 2014) for all performance indicators, with an eigenvalue of 2.089 and explaining 52.216% of the total variance of the dataset. Cronbach’s alpha was applied to check the reliability of the construct. High reliability was verified as we obtained an alpha value of 0.821 (i.e., > 0.6; Meyers et al., 2006).
Another EFA was performed with responses related to the adoption of Industry 4.0 technologies. Using a Varimax rotation, we found two PCs with eigenvalues greater than 1 (3.410 and 2.119, respectively), as displayed in Table 5. We replicated the results via an oblique rotation to check for orthogonality, which led to similar components. The analysis of Cronbach’s alphas indicated high reliability of the constructs, yielding values of 0.811 and 0.788, respectively. Based on the factor loadings for each component, two constructs of technologies emerged and were denominated after their main roles (Aceto et al. 2018). The first component consisted of Industry 4.0 technologies that seek to capture (sense) and communicate data from a patient, equipment, material, or processes, such as wireless sensors, IoT, and cloud computing. Due to their similar purpose, the construct was named ‘Sensing-Communication’ [SENS_COMM] technologies. The second component involved Industry 4.0 technologies that might affect or process data, generating useful information, and controlling systems and mechanisms (Tortorella et al. 2020d). The construct was denoted as ‘Processing-Actuation’ [PROC_ACT] technologies.
Finally, an EFA with varimax rotation was carried out using the collected data on the development level of the eight resilience abilities presented in the questionnaire. We extracted two components with eigenvalues ≥ 1, explaining 60.97% of the responses’ variance (as shown in Table 6). Similar results were found based on an oblique rotation. The values for Cronbach’s alpha for each component were 0.765 and 0.804, indicating the high reliability of both constructs. The first component comprises abilities that help organizations to anticipate actions and monitor the occurrence of potential disruptions. According to Hollnagel (2017), the ability of anticipation consists in “knowing what to expect”, while monitoring refers to “knowing what to focus on so that it does not become a threat in the future”. Therefore, we named this first construct ‘Anticipation and Monitoring’ [ANT_MON] abilities. The second component encompassed abilities that help organizations adapt and recover from disruptive events. Based on Hosseini et al.‘s (2019) indications, we denominated this construct ‘Adaptive and Restorative’ [ADAP_REST] abilities.
Composite reliability (CR) was assessed. All CR values resulted > 0.7, assuring the constructs’ convergent validity (Hair et al. 2014). Standardized scores for each construct given on a continuous scale were then obtained, and pairwise correlations between constructs were analyzed, with results displayed in Table 7. Positive and negative coefficients were found (p-value < 0.01).
4.4 Data analysis
To analyze the data, we performed a set of Ordinary Least Square (OLS) hierarchical linear regression models. Three main models were tested. Models 1 and 2 regressed the mediating variables (constructs of resilience abilities) on the control (tier level and organization size) and independent (constructs of Industry 4.0 technologies) variables. Both models were also checked with country and respondent’s background as dummy variables. No significant association was found, and results were equal when these variables were removed. Hence, country and respondents’ backgrounds were disregarded to enhance our tests’ degrees of freedom and significance. Model 3 regressed performance variation since the COVID-19 outbreak on the control, independent, and mediating variables.
According to Hair et al. (2014), all variables’ assumptions of normality, linearity, and homoscedasticity were checked. We assessed residuals to verify the normality of the error term distribution. Linearity was examined with scatterplots of dependent and independent variables; evidence of nonlinearity was not found in any partial regression plot. Homoscedasticity was visually examined by plotting standardized residuals versus the predicted values. These verifications underpinned the requirements for an OLS regression analysis.
5 Results and discussion
Table 8 displays the unstandardized \(\widehat{\beta }\) coefficients for the OLS regression analyses, as variables were standardized before running the analyses. The regression models’ variance inflation factors (VIFs) were all < 3.0, indicating that multicollinearity could be disregarded (Hair et al. 2014). Models 1 and 2 tested the effect of [SENS_COMM] and [PROC_ACT] on [ANT_MON] and [ADAP_REST], respectively, which were conceptualized as mediating variables. [PROC_ACT] technologies appear to be positively and significantly associated with the development of both constructs of resilience abilities (\(\widehat{\beta }\) = 0.562; p-value < 0.01; and \(\widehat{\beta }\) = 0.185; p-value < 0.05, respectively). However, [SENS_COMM] technologies seem to be positively associated only with [ADAP_REST] abilities (\(\widehat{\beta }\) = 0.472; p-value < 0.01).
In Model 3, performance variation in organizations from the healthcare supply chain since the COVID-19 outbreak was regressed on the control (Model 3 A), independent (Model 3B), and mediating variables (Model 3 C), which yielded significant models (p-value < 0.05). However, Model 3 C displayed the highest predicting capacity with an adjusted R2 of 0.202, overcoming the prediction capacity of Model 3B. In Model 3 C, both resilience abilities constructs were positively related to performance (\(\widehat{\beta }\) = 0.135; p-value < 0.10; and \(\widehat{\beta }\) = 0.225; p-value < 0.01, respectively). Further, [SENS_COMM] technologies were also found to be significantly associated with performance (\(\widehat{\beta }\) = 0.324; p-value < 0.01), while no significant direct association was found for [PROC_ACT] technologies. None of the contextual characteristics tested in Model 3 C (i.e., tier level and organization size) were significant in explaining performance variation of healthcare supply chain organizations since the beginning of the COVID-19 outbreak.
We now discuss our findings, which partially support our hypotheses, and the relationships empirically validated and displayed in Fig. 2. Concerning the impact of Industry 4.0 technologies on the development of resilience abilities in the healthcare supply chain during the COVID-19 outbreak, our results indicated that [PROC_ACT] technologies positively contribute to both [ANT_MON] and [ADAP_REST] abilities, as proposed in H1. In turn, [SENS_COMM] technologies seem to be positively associated only with [ADAP_REST] abilities. This outcome was particularly surprising in light of the role played by these Industry 4.0 technologies, which comprises the capturing and sharing of the data collected from processes, treatments, products, services, equipment, and patients across the entire healthcare supply chain. Supposedly, a high adoption level of [SENS_COMM] technologies would provide the means to achieve greater awareness of the current situation during the pandemic, facilitating the foresight of additional disruptions and proactive development of necessary countermeasures. Our findings do not validate such assumption. Nevertheless, we found a positive direct effect of [SENS_COMM] technologies on the performance variation of the healthcare supply chain since the COVID-19 outbreak.
An explanation for the counterintuitive result above may refer to how unprecedented the interruption caused by COVID-19 was. Gereffi (2020) and Govindan et al. (2020) indicated that the COVID-19 pandemic is an unprecedented disruptive event due to its impact and pervasiveness across the globe and its duration. According to WHO (2021), on December 31st, 2019, information on cases of pneumonia of unknown cause in Wuhan City, China, was first reported, and the new coronavirus was identified as the cause by Chinese authorities on January 7th, 2020. Since then, the COVID-19 pandemic has caused millions of deaths, severely impacting communities, businesses, supply chains, and countries up to this day. Such uniqueness may hinder the proper development of anticipation actions, jumping directly to a reactive mode in terms supply chain management.
Moreover, the resource dependence theory states that when the resources an organization needs are scarce, not readily obtainable, or under the control of uncollaborative agents, the resulting unbalanced exchanges lead to distinction in power, authority, and access to such resources (Hillman et al. 2009). This behavior was particularly observed at the beginning of the COVID-19 outbreak, in which organizations, governments, and the healthcare supply chain as a whole were not collaborating as cohesively as nowadays (Friday et al. 2021). That might justify the significant impact of [SENS_COMM] technologies on the performance of the healthcare supply chain and the poor association of these technologies with the [ANT_MON] abilities, partially supporting H2.
Concerning the mediating role of resilience abilities, the [ADAP_REST] abilities appear to significantly and positively mediate the relationship between [SENS_COMM] and [PROC_ACT] technologies and the performance of the healthcare supply chain since the COVID-19 outbreak, as initially envisioned. The prominence of resilience abilities that help to adapt and recover from the COVID-19 disruptions can be partially justified by the unprecedented characteristics of the pandemic, as aforementioned. The concurrent development of those abilities and the high adoption of Industry 4.0 technologies across the healthcare supply chain seem to lead to greater performance improvements and mitigate the negative implications of the pandemic. Such a result may also emerge from the fact that organizations generally determine their strategies to cope with shifts in power relationships with other organizations. According to Archibald (2021), uncertainty clouds resources control, leading to the development of dependence-lessening strategies. As uncertainty and dependencies increase, so does the necessity for close relationships with other agents. Industry 4.0 technologies tend to favor more effective management of the healthcare supply chain, reducing uncertainties, increasing flexibility, and supporting more assertive decisions (Hossain and Thakur 2021). That supports the alignment between internal organizational needs and elements with external pressures and influences from the supply chain, which, together with an increased responsiveness ability, can yield a faster adaptation to the new scenario imposed by the disruptive event (e.g., COVID-19 pandemic) and the maintenance or even improvement of performance.
6 Conclusions
Our research investigated the role of resilience abilities in the relationship between Industry 4.0 technologies adoption and healthcare supply chain performance during the COVID-19 pandemic. We performed a survey with practitioners from organizations of the healthcare supply chain in Brazil and India, framing our hypotheses and discussion on concepts from resource dependence theory. This study connected three emerging topics related to the healthcare supply chain: resilience development, Industry 4.0 adoption, and the COVID-19 disruptions. As discussed next, our findings contribute to both theory and practice on these topics.
6.1 Implications to theory
Our investigation contributed to the state-of-the-art on healthcare supply chain management by bridging the knowledge on topics still relatively new to researchers and academics, such as Industry 4.0, resilience development, and implications from the COVID-19 pandemic. We framed our hypotheses’ development by concepts from the resource dependence theory, also used to discuss our main findings. Since the pandemic’s beginning, organizations in the healthcare supply chain have displayed different behaviors mainly driven by the availability of resources used to fight the pandemic (e.g., materials, labor, and personal protective equipment). That led to strategies to reduce uncertainty in the supply chain (aligned with the resource dependence theory principles) and quickly return to pre-pandemic operational performance, searching for a more resilient operation. We empirically verified that the impact of Industry 4.0 technologies on performance is positively mediated by the development of resilience abilities in the healthcare supply chain, emphasizing the need for an alignment of interests across the healthcare supply chain towards greater effectiveness. Our results contribute to the existing body of knowledge on the resource dependence theory, suggesting that resilience development through digitalization can mitigate the effect of power and uncertainty in the supply chain even during disruptive events. To the best of our knowledge, no similar investigation in the literature has empirically analyzed such relationships in the pandemic scenario and from the healthcare supply chain perspective.
6.2 Contributions to practice
From a practical perspective, our study offers managers and organizations from the healthcare supply chain arguments to achieve higher performance levels based on digitalization and resilience development when disruptive events occur. The COVID-19 pandemic has imposed extreme challenges on the healthcare supply chain worldwide, raising the need to accelerate improvement initiatives, such as digital transformation. Although digitalization of the healthcare supply chain does improve its performance, our research indicated that its impact could be significantly enhanced when resilience abilities are concurrently developed, particularly in the Indian and Brazilian contexts. Such a result is relevant for the organizations embedded in the healthcare supply chain and governments and institutions in charge of developing policies and regulations related to improving healthcare systems in emerging economies.
At the company level, our results should appeal to managers since they translate the well-known four resilient abilities of healthcare systems (i.e., monitor, anticipate, respond, and learn) proposed by Braithwaite et al. (2015) and Hollnagel (2017) in the context of clinical operations to the healthcare supply chain context. Many healthcare organization managers come from a clinical background (Sarto and Veronesi 2016) and are challenged by managerial activities they were not formally trained to perform. Bridging such knowledge gap by establishing connections between activities they are familiar with (e.g., monitoring patients’ signals and anticipating their needs) and supply chain good practices (e.g., maintaining high situational awareness and being financially adept to meet contingencies proactively) should aid in improving their performance and communication with other organization actors.
Our results show the significant positive impact of sensing and communicating (SENS_COMM) technologies on supply chain performance after the COVID-19 outbreak. Within the SENS_COMM factor, wireless sensors stand out with the highest associated loading. Such a result is aligned with the technological improvements observed in healthcare logistics in the past decade. There has been an increase in the use of mobile wireless sensor networks to monitor transport conditions inside containers, particularly in transatlantic cargo vessels, which are exposed to uneven environmental conditions (Becker et al. 2010). The online monitoring of shipments allowed healthcare providers to better control inventories and highlighted the practical importance of efficient communication among supply chain actors, a trend already verified in the literature (VanVactor 2011). New forms of transportation are also being devised to reduce disruptions in healthcare supplies delivery, e.g., the use of drones for small and medium-sized shipments (Jaekel 2021). The practical takeaway of our result for healthcare procurement departments is that suppliers’ delivery speed and cargo remote monitoring capability are key in improving supply chain performance. Since both Industry 4.0 adoption and the development of resilience abilities require great efforts, the sooner the organizations from the healthcare supply chain collaboratively work on those initiatives, the more prepared they will be to cope with future disruptive events.
6.3 Limitations and future research
A few limitations of our study should be highlighted. Initially, we focused on respondents located in emerging economies (i.e., India and Brazil). Although enhancing the replicability of our results to healthcare supply chains located in similar socioeconomic contexts, it also limits the generalization of findings to a broader audience (e.g., developed economies). Another limitation concerning the data collection refers to the performance indicators adopted in our study. Although cost, quality, delivery, and inventory level are widely used in the literature to investigate supply chain performance (e.g., Marodin et al., 2016; 2017; Guersola et al., 2018; Borges et al., 2020), other indicators could complement our analysis. Particularly, the use of the supply chain operations reference (SCOR) model (Supply Chain Council, 2004) could help address this issue. Thus, further research could expand the data collection by performing a multinational study and including other performance metrics, raising complementary indications. Second, we verified the relationships between Industry 4.0 adoption, resilience development, and healthcare supply chain performance under the disruptive scenario caused by the COVID-19 pandemic. Despite its unique relevance, the pandemic disruptions are unique, which somewhat constrains our findings to this disruptive event. Future studies could verify how learnings could be extended to different disruptive events, such as natural disasters and socio-political conflicts. Finally, we remark that the survey-based method adopted here does not support an in-depth analysis of the Industry 4.0 adoption pathways in the healthcare supply chain, which could be a relevant research question for future investigation. Hence, the conduction of multi-case studies could complement our findings, potentially raising new insights into the literature body.
7 Appendix—Applied questionnaire
1- Please, provide below the following information:
(a) The number of employees of your organization:
( ) < 100 employees
( ) between 100 and 250 employees
( ) between 250 and 1,000 employees
( ) > 1,000 employees
(b) Country where your organization is located: ______________________
(c) Your tier of the healthcare supply chain:
( ) Manufacturer (pharmaceutical, medical device, surgical or medical equipment).
( ) Distributor or Group of Purchasing Organization (GPO).
( ) Care provider (hospital, clinic, pharmacies).
(d) Your role in the organization: ______________________
(e) Your academic background: ______________________
2- Please, indicate below the adoption level of the following technologies in your organization:
Scale: from 1 (no adoption) to 5 (fully adopted).
Technology | 1 | 2 | 3 | 4 | 5 |
|---|---|---|---|---|---|
Enterprise Resource Planning (ERP) | |||||
Big data | |||||
Radio Frequency Identification (RFID) | |||||
Internet of Things (IoT) | |||||
Sensors | |||||
Cloud computing | |||||
Cyber-physical systems | |||||
Blockchain | |||||
Augmented and virtual reality | |||||
Additive manufacturing | |||||
Digital twin | |||||
Machine learning |
3- Please, indicate below the readiness level of your organization regarding the following abilities:
Scale: from 1 (not developed) to 5 (fully developed).
Abilities | 1 | 2 | 3 | 4 | 5 |
|---|---|---|---|---|---|
Learning from experience | |||||
Financially adept to proactively meet contingencies | |||||
Always maintain high situational awareness | |||||
Provide a quick response to SC disruption | |||||
Cope with changes brought by SC disruption | |||||
Adapt to SC disruption easily | |||||
Recovery to normal operations speedily after SC disruption | |||||
Easy and fast access to knowledge when facing an operational failure |
4- Please, indicate the evolution of the following performance indicators in your organization since the COVID-19 outbreak (January 2020):
Scale: from 1 (significantly worsened) to 5 (significantly improved).
Performance indicators | 1 | 2 | 3 | 4 | 5 |
|---|---|---|---|---|---|
Quality | |||||
Cost | |||||
Delivery | |||||
Inventory level |
Data Availability
Due to the nature of this research, participants of this study did not agree for their data to be shared publicly, so supporting data is not available.
References
Aceto G, Persico V, Pescapé A (2018) The role of information and Communication Technologies in healthcare: taxonomies, perspectives, and challenges. J Netw Comput Appl 107:125–154
Ageron B, Benzidia S, Bourlakis M (2018) Healthcare logistics and supply chain–issues and future challenges. Supply Chain Forum: An International Journal 19(1):1–3
Akyuz G, Erkan T (2010) Supply chain performance measurement: a literature review. Int J Prod Res 48(17):5137–5155
Aldrighetti R, Zennaro I, Finco S, Battini D (2019) Healthcare supply chain simulation with disruption considerations: a case study from Northern Italy. Global J Flex Syst Manage 20(1):81–102
Alloghani M, Al-Jumeily D, Hussain A, Aljaaf A, Mustafina J, Petrov E (2018) “Healthcare services innovations based on the state-of-the-art technology trend Industry 4.0.“ In 2018 11th International Conference on Developments in eSystems Engineering (DeSE) (pp.64–70). IEEE
Ambulkar S, Blackhurst J, Grawe S (2015) Firm resilience to Supply Chain Disruptions: Scale Development and empirical examination. J Oper Manag 33–34:111–122
Archibald M (2021) “Resource dependence theory.“ Britannica. Available at: https://www.britannica.com/topic/resource-dependency-theory (accessed on July 30th 2021)
Awan U, Gölgeci I, Makhmadshoev D, Mishra N (2022) “Industry 4.0 and circular economy in an era of global value chains: what have we learned and what is still to be explored?.“Journal of Cleaner Production,133621
Becker M, Wenning B, Görg C, Jedermann R, Timm-Giel A (2010) “Logistic applications with wireless sensor networks.“ In Proceedings of the 6th Workshop on Hot Topics in Embedded Networked Sensors (HotEmNets ‘10), Article 6: 1–5
Becue A, Maia E, Feeken L, Borchers P, Praca I (2020) A new concept of digital twin supporting optimization and resilience of factories of the future. Appl Sci 10(13):4482
Biermann R, Harsch M (2017) Resource dependence theory. Palgrave handbook of inter-organizational relations in world politics. Palgrave Macmillan, London, pp 135–155
Biringer B, Vugrin E, Warren D (2013) Critical infrastructure system security and resiliency. CRC press, London
Boparai J, Singh S, Kathuria P (2018) How to design and validate a questionnaire: a guide. Curr Clin Pharmacol 13(4):210–215
Borges GA, Tortorella G, Martínez F, Thurer M (2020) “Simulation-based analysis of lean practices implementation on the supply chain of a public hospital.“ Production, 30
Borges GA, Tortorella G, Rossini M, Portioli-Staudacher A (2019) Lean implementation in healthcare supply chain: a scoping review. J Health Organ Manag 33(3):304–322
Braithwaite J, Wears R, Hollnagel E (2015) Resilient health care: turning patient safety on its head. Int J Qual Health Care 27(5):418–420
Brandon-Jones E, Squire B, Autry C, Petersen K (2014) A contingent resource-based perspective of Supply Chain Resilience and Robustness. J Supply Chain Manage 50(3):55–73
Briano E, Caballini C, Revetria R (2009) “Literature review about supply chain vulnerability and resilience.“ Proceedings of the 8th WSEAS International Conference on System Science and Simulation in Engineering, 191–197
Bueno-Solano A, Cedillo-Campos M (2014) Dynamic impact on global supply chains performance of disruptions propagation produced by terrorist acts. Transp Res E 61:1–12
Cadavid J, Lamouri S, Grabot B, Pellerin R, Fortin A (2020) “Machine learning applied in production planning and control: a state-of-the-art in the era of industry 4.0.“Journal of Intelligent Manufacturing, (forthcoming).
Cavalcante I, Frazzon E, Forcellini F, Ivanov D (2019) A supervised machine learning approach to data-driven simulation of resilient supplier selection in digital manufacturing. Int J Inf Manag 49:86–97
Colicchia C, Creazza A, Menachof D (2019) Managing cyber and information risks in supply chains: insights from an exploratory analysis. Supply Chain Management: An International Journal 24(2):215–240
Das S, Yaylacicegi U, Menon N (2011) The effect of information technology investments in healthcare: a longitudinal study of its lag, duration, and economic value. IEEE Trans Eng Manage 58(1):124–140
Dolgui A, Ivanov D, Rozhkov M (2020) Does the ripple effect influence the bullwhip effect? An integrated analysis of structural and operational dynamics in the supply chain. Int J Prod Res 58(5):1285–1301
Drees JM, Heugens P (2013) Synthesizing and extending resource dependence theory: a meta-analysis. J Manag 39(6):1666–1698
Dubey R, Gunasekaran A, Childe S, Fosso Wamba S, Roubaud D, Foropon C (2021) Empirical investigation of data analytics capability and organizational flexibility as complements to supply chain resilience. Int J Prod Res 59(1):110–128
Elhoseny M, Abdelaziz A, Salama A, Riad A, Muhammad K, Sangaiah A (2018) A hybrid model of internet of things and cloud computing to manage big data in health services applications. Future Generation Computer Systems 86:1383–1394
Fabrigar L, Wegener D, MacCallum R, Strahan E (1999) Evaluating the use of exploratory factor analysis in psychological research. Psychol Methods 4(3):272
Finch J, West S (1997) The investigation of personality structure: statistical models. J Res Pers 31(4):439–485
Fosso Wamba S, Gunasekaran A, Papadopoulos T, Ngai E (2018) Big data analytics in logistics and supply chain management. Int J Logistics Manage 29(2):478–484
Frederico G, Garza-Reyes J, Anosike A, Kumar V (2020) Supply Chain 4.0: concepts, maturity and research agenda. Supply Chain Management: An International Journal 25(2):262–282
Friday D, Savage D, Melnyk S, Harrison N, Ryan S, Wechtler H (2021) A collaborative approach to maintaining optimal inventory and mitigating stockout risks during a pandemic: capabilities for enabling health-care supply chain resilience. J Humanitarian Logistics Supply Chain Manage 11(2):248–271
Garai Á, Péntek I, Adamkó A, Németh A (2017) A clinical system integration methodology for bio-sensory technology with Cloud architecture. Acta Cybernetica 23(2):513–536
Gereffi G (2020) What does the COVID-19 pandemic teach us about global value chains? The case of medical supplies. J Int Bus Policy 3(3):287–301
Goodwin C (2005) Research in psychology: methods and design. John Wiley & Sons, Inc., New York
Govindan K, Mina H, Alavi B (2020) “A decision support system for demand management in healthcare supply chains considering the epidemic outbreaks: a case study of coronavirus disease 2019 (COVID-19).“Transportation Research Part E: Logistics and Transportation Review, 101967
Gružauskas V, Vilkas M (2017) Managing capabilities for supply chain resilience through IT integration. Econ Bus 31(1):30–43
Gu M, Yang L, Huo B (2020) “The impact of information technology usage on supply chain resilience and performance: an ambidexterous view.“International Journal of Production Economics,107956
Guersola M, Lima E, Steiner M (2018) Supply chain performance measurement: a systematic literature review. Int J Logistics Syst Manage 31(1):109–131
Hahn G (2020) Industry 4.0: a supply chain innovation perspective. Int J Prod Res 58(5):1425–1441
Hair J, Black W, Babin B, Anderson R (2014) Multivariate Data Analysis. Pearson New International Edition (Seventh edition), Harlow, Essex, Pearson
Hamidi H (2019) An approach to develop the smart health using internet of things and authentication based on biometric technology. Future Generation Computer Systems 91:434–449
Haszlinna Mustaffa N, Potter A (2009) Healthcare supply chain management in Malaysia: a case study. Supply Chain Management: An International Journal 14(3):234–243
Hillman AJ, Withers M, Collins B (2009) Resource dependence theory: a review. J Manag 35(6):1404–1427
Hollnagel E (2014) Resilience engineering and the built environment. Building Res Inform 42(2):221–228
Hollnagel E (2017) Safety-II in Practice: developing the resilience potentials. Routledge, London
Hossain MK, Thakur V (2021) Benchmarking health-care supply chain by implementing industry 4.0: a fuzzy-AHP-DEMATEL approach. " Benchmarking: An International Journal 28(2):556–581
Hosseini S, Ivanov D, Dolgui A (2019) Review of quantitative methods for supply chain resilience analysis. Transp Res E 125:285–307
Huber G, Power D (1985) Retrospective reports of strategic-level managers: guidelines for increasing their accuracy. Strateg Manag J 6:171–180
Ivanov D, Das A (2020) Coronavirus (COVID-19/SARS-CoV-2) and supply chain resilience: a research note. Int J Integr Supply Manage 13(1):90–102
Ivanov D, Dolgui A (2020) A digital supply chain twin for managing the disruption risks and resilience in the era of industry 4.0. Production Planning & Control. (forthcoming)
Ivanov D, Dolgui A, Sokolov B (2019) The impact of digital technology and industry 4.0 on the ripple effect and supply chain risk analytics. Int J Prod Res 57(3):829–846
Ivanov D, Sethi S, Dolgui A, Sokolov B (2018) A survey on control theory applications to operational systems, supply chain management, and industry 4.0. Annu Rev Control 46:134–147
Jaekel B (2021) “Healthcare Logistics Sees Futuristic Advancement.“ SDC Supply Chain and Demand Executive. Available at: https://www.sdcexec.com/software-technology/emerging-technologies/news/21590752/air-methods-healthcare-logistics-sees-futuristic-advancement (accessed on March 15th 2022)
Jeong JS, Han O, You Y (2016) A design characteristics of smart healthcare system as the IoT application. Indian J Sci Technol 9(37):52
Jüttner U, Maklan S (2011) Supply chain resilience in the global financial crisis: an empirical study. Supply Chain Management: An International Journal 16(4):246–259
Khan SAR, Godil D, Jabbour C, Shujaat S, Razzaq A, and Z. Yu (2021a) “Green data analytics, blockchain technology for sustainable development, and sustainable supply chain practices: evidence from small and medium enterprises.“Annals of Operations Research,1–25
Khan SAR, Ponce P, Tanveer M, Aguirre-Padilla N, Mahmood H, Shah S (2021b) Technological innovation and circular economy practices: business strategies to mitigate the effects of COVID-19. Sustainability 13(15):8479
Khan SAR, Ponce P, Thomas G, Yu Z, Al-Ahmadi M, Tanveer M (2021c) Digital technologies, circular economy practices and environmental policies in the era of COVID-19. Sustainability 13(22):12790
Khan SAR, Yu Z, Umar M, Lopes de Sousa A, Jabbour, Mor R (2022a) Tackling post-pandemic challenges with digital technologies: an empirical study. J Enterp Inform Manage 35(1):36–57
Khan SAR, Yu Z, Umar M, Tanveer M (2022b) “Green capabilities and green purchasing practices: A strategy striving towards sustainable operations.“ Business Strategy and the Environment, (forthcoming)
Khodadad-Saryazdi A (2021) Exploring the telemedicine implementation challenges through the process innovation approach: a case study research in the french healthcare sector. Technovation 107:102273
Kim W, Choi J (2016) Challenges for wearable healthcare services. Int J Web Grid Serv 12(4):407–417
Kim ST, Lee H, Hwang T (2020) Logistics integration in the supply chain: a resource dependence theory perspective. Int J Qual Innov 6(1):1–14
Kothari CR (2004) Research methodology: methods and techniques. New Age International
Krammer SM (2021) “Navigating the New Normal: Which firms have adapted better to the COVID-19 disruption?.“ Technovation, 102368
Krause D, Vachon S, Klassen R (2009) Special topic forum on sustainable supply chain management: introduction and reflections on the role of purchasing management. J Supply Chain Manage 45(4):18–25
Kritchanchai D (2014) A framework for healthcare supply chain improvement in Thailand. Oper Supply Chain Management: Int J 5(2):103–113
Kumar S, Raut R, Priyadarshinee P, Mangla S, Awan U, Narkhede B (2022) “The impact of IoT on the performance of vaccine supply chain distribution in the COVID-19 context.“IEEE Transactions on Engineering Management, (forthcoming).
Kwak D, Seo Y, Mason R (2018) Investigating the relationship between supply chain innovation, risk management capabilities and competitive advantage in global supply chains. Int J Oper Prod Manage 38(1):2–21
Lavassani KM, Movahedi B (2010) “Critical analysis of the supply chain management theories: toward the stakeholder theory.“ In POMS 21st Annu. Conf., Vancouver, Canada (pp.7–10)
Malhotra N, Birks D, Wills P (2006) Marketing research: an applied approach. Pearson Education, London
Mandal S (2019) Exploring the influence of IT capabilities on agility and resilience in tourism: moderating role of technology orientation. J Hospitality Tourism Technol 10(3):401–414
Mandal S (2017) The influence of organizational culture on healthcare supply chain resilience: moderating role of technology orientation. J Bus Industrial Mark 32(8):1021–1037
Manzouri M, Rahman M (2013) Adaptation of theories of supply chain management to the lean supply chain management. Int J Logistics Syst Manage 14(1):38–54
Marodin GA, Frank A, Tortorella G, Fetterman D (2019) Lean production and operational performance in the brazilian automotive supply chain. Total Qual Manage Bus Excellence 30(3–4):370–385
Marodin GA, Frank A, Tortorella G, Saurin T (2016) Contextual factors and lean production implementation in the brazilian automotive supply chain. Supply Chain Management: An International Journal 21(4):417–432
Marodin GA, Tortorella G, Frank A, Godinho Filho M (2017) The moderating effect of lean supply chain management on the impact of lean shop floor practices on quality and inventory. Supply Chain Management: An International Journal 22(6):473–485
Marten R, McIntyre D, Travassos C, Shishkin S, Longde W, Reddy S, Vega J (2014) An assessment of progress towards universal health coverage in Brazil, Russia, India, China, and South Africa (BRICS). The Lancet 384(9960):2164–2171
Massaro M (2021) “Digital transformation in the healthcare sector through blockchain technology. Insights from academic research and business developments.“ Technovation, 102386
Mathur B, Gupta S, Meena M, Dangayach G (2018) Healthcare supply chain management: literature review and some issues. J Adv Manage Res 15(3):265–287
Matsuo H (2015) Implications of the Tohoku earthquake for Toyota׳ s coordination mechanism: Supply chain disruption of automotive semiconductors. Int J Prod Econ 161:217–227
McKone-Sweet KE, Hamilton P, Willis S (2005) The ailing healthcare supply chain: a prescription for change. J Supply Chain Manage 41(1):4–17
Meyers L, Gamst G, Guarino A (2006) Applied multivariate research. Sage Publications, Thousand Oaks
Mirchandani P (2020) Health care supply chains: COVID-19 challenges and pressing actions. Available at: https://www.acpjournals.org/doi/full/10.7326/M20-1326 (accessed on July 14th 2021)
Montgomery D (2013) Design and analysis of experiments. Wiley, New York
Moons K, Waeyenbergh G, Pintelon L (2019) Measuring the logistics performance of internal hospital supply chains–a literature study. Omega 82:205–217
Moyano-Fuentes J, Bruque-Cámara S, Maqueira-Marín J (2019) Development and validation of a lean supply chain management measurement instrument. Prod Plann Control 30(1):20–32
Narayanamurthy G, Tortorella G (2021) Impact of COVID-19 outbreak on employee performance–moderating role of industry 4.0 base technologies. Int J Prod Econ 234:108075
Paché G (2020) Covid-19: the two sides of healthcare supply chain management. Eur J Manage 20(1):79–84
Pan J, Ding S, Wu D, Yang S, Yang J (2019) Exploring behavioural intentions toward smart healthcare services among medical practitioners: a technology transfer perspective. Int J Prod Res 57(18):5801–5820
Pettit T, Croxton K, Fiksel J (2019) The evolution of resilience in supply chain management: a retrospective on ensuring supply chain resilience. J Bus Logistics 40(1):56–65
Pettit T, Fiksel J, Croxton K (2010) Ensuring supply chain resilience: development of a conceptual framework. J Bus Logistics 31(1):1–21
Pfeffer J, Salancik G (1978) The External Control of Organizations: a resource dependence perspective. Harper and Row, New York, NY
Podsakoff P, Organ D (1986) Self-reports in organizational research: problems and prospects. J Manag 12(4):531–544
Podsakoff P, MacKenzie S, Lee J, Podsakoff N (2003) Common method biases in behavioral research: a critical review of the literature and recommended remedies. J Appl Psychol 88(5):879
Pramanik M, Lau R, Demirkan H, Azad M (2017) Smart health: big data enabled health paradigm within smart cities. Expert Syst Appl 87:370–383
Queiroz MM, Telles R (2018) Big data analytics in supply chain and logistics: an empirical approach. Int J Logistics Manage 29(2):767–783
Queiroz MM, Telles R, Bonilla S (2019) Blockchain and supply chain management integration: a systematic review of the literature. Supply Chain Management: An International Journal 25(2):241–254
Rakovska MA, Stratieva S (2018) A taxonomy of healthcare supply chain management practices. Supply Chain Forum: An International Journal 19(1):4–24
Ralston P, Blackhurst J (2020) Industry 4.0 and resilience in the supply chain: a driver of capability enhancement or capability loss? Int J Prod Res 58(16):5006–5019
Roark DC (2005) Managing the healthcare supply chain. Nurs Manag 36(2):36–40
Rosa V, Saurin T, Tortorella G, Fogliatto F, Tonetto L, Samson D (2021) Digital technologies: an exploratory study of their role in the resilience of healthcare services. Appl Ergon 97:103517
Rossini M, Costa F, Tortorella G, Staudacher A (2019) The interrelation between industry 4.0 and lean production: an empirical study on european manufacturers. Int J Adv Manuf Technol 102(9–12):3963–3976
Rossit D, Tohmé F, Frutos M (2019) Production planning and scheduling in Cyber-Physical Production Systems: a review. Int J Comput Integr Manuf 32(4–5):385–395
Rubbio I, Bruccoleri M, Pietrosi A, Ragonese B (2019) Digital health technology enhances resilient behaviour: evidence from the ward. Int J Oper Prod Manage 40(1):34–67
Sannino G, De Falco I, De Pietro G (2018) A continuous noninvasive arterial pressure (CNAP) Approach for Health 4.0 Systems. " IEEE Transactions on Industrial Informatics 15(1):498–506
Sarkis J, Zhu Q, Lai K (2011) An organizational theoretic review of green supply chain management literature. Int J Prod Econ 130(1):1–15
Sarto F, Veronesi G (2016) Clinical leadership and hospital performance: assessing the evidence base. BMC Health Serv Res 16(Suppl 2):169
Scholten K, Schilder S (2015) The role of collaboration in supply chain resilience. Supply Chain Management: An International Journal 20(4):471–484
Shaheen F, Lodhi M, Rosak-Szyrocka J, Zaman K, Awan U, Asif M, … and, Siddique M (2022) Cleaner Technology and Natural Resource Management: an environmental sustainability perspective from China. Clean Technol 4(3):584–606
Shao X, Liu W, Li Y, Chaudhry H, Yue X (2020) Multistage implementation framework for smart supply chain management under industry 4.0. Technol Forecast Soc Chang 162:120354
Sharma A, Gupta P, Jha R (2020) COVID-19: impact on health supply chain and lessons to be learnt. J Health Manage 22(2):248–261
Smith T (1983) On the validity of inferences from non-random samples. J Royal Stat Society: Ser (General) 146(4):394–403
Snyder L, Atan Z, Peng P, Rong Y, Schmitt A, Sinsoysal B (2016) OR/MS models for supply chain disruptions: a review. IIE Trans 48(2):89–109
Sriyanto S, Lodhi M, Salamun H, Sardin S, Pasani C, Muneer G, Zaman K (2021) The role of healthcare supply chain management in the wake of COVID-19 pandemic: hot off the press. Foresight 24(3/4):429–444
Stone DH (1993) Design a questionnaire. BMJ 307(6914):1264–1266
Supply Chain Council (2004) Supply Chain Operations Reference Model. Available at: https://www.ascm.org/corporate-transformation/ (accessed on March 7th 2022)
Tang C (2006) Robust strategies for mitigating supply chain disruptions. Int J Logistics: Res Appl 9(1):33–45
Thuemmler C, Bai C (eds) (2017) Health 4.0: how virtualization and big data are revolutionizing healthcare. Springer, New York
Tortorella GL, Fogliatto F, Espôsto K, Vergara A, Vassolo R, Tlapa D, Narayanamurthy G (2020d) “Healthcare costs’ reduction through the integration of Healthcare 4.0 technologies in developing economies.“Total Quality Management & Business Excellence, (forthcoming).
Tortorella GL, Fogliatto F, Espôsto K, Vergara A, Vassolo R, Tlapa D, Narayanamurthy G (2020c) “Measuring the effect of Healthcare 4.0 implementation on hospitals’ performance.“Production Planning & Control, (forthcoming).
Tortorella GL, Fogliatto F, Espôsto K, Vergara A, Vassolo R, Tlapa D, Narayanamurthy G (2020b) Effects of contingencies on healthcare 4.0 technologies adoption and barriers in emerging economies. Technol Forecast Soc Chang 156:120048
Tortorella GL, Fogliatto F, Saurin T, Tonetto L, McFarlane D (2021c) “Contributions of Healthcare 4.0 digital applications to the resilience of healthcare organizations during the COVID-19 outbreak.“ Technovation, 102379
Tortorella GL, Fogliatto F, Sunder V, Vergara MA, Vassolo R (2021a) “Assessment and prioritisation of Healthcare 4.0 implementation in hospitals using quality function Deployment.“International Journal of Production Research, (forthcoming).
Tortorella GL, Fogliatto F, Vergara A, Vassolo R, Sawhney R (2020a) Healthcare 4.0: trends, challenges and research directions. Prod Plann Control 31(15):1245–1260
Tortorella GL, Giglio R, Limon-Romero J (2018) Supply chain performance: how lean practices efficiently drive improvements. J Manuf Technol Manage 29(5):829–845
Tortorella GL, Giglio R, van Dun D (2019) Industry 4.0 adoption as a moderator of the impact of lean production practices on operational performance improvement. Int J Oper Prod Manage 39(6/7/8):860–886
Tortorella GL, Miorando R, Marodin G (2017) Lean supply chain management: empirical research on practices, contexts and performance. Int J Prod Econ 193:98–112
Tortorella GL, Rossini M, Costa F, Staudacher A, Sawhney R (2021d) A comparison on industry 4.0 and lean production between manufacturers from emerging and developed economies. Total Qual Manage Bus Excellence 32(11–12):1249–1270
Tortorella GL, Saurin T, Fogliatto F, Rosa V, Tonetto L, Magrabi F (2021b) “Impacts of Healthcare 4.0 digital technologies on the resilience of hospitals.“ Technological Forecasting and Social Change, 166: 120666
Ulrich D, Barney J (1984) Perspectives in organizations: resource dependence, efficiency, and population. Acad Manage Rev 9(3):471–481
Usman B, Zaman K, Nassani A, Haffar M, Muneer G (2022) The impact of carbon pricing, climate financing, and financial literacy on COVID-19 cases: go-for-green healthcare policies. Environ Sci Pollut Res 29(24):35884–35896
Van Dun DH, Hicks J, Wilderom C (2017) Values and behaviors of effective lean managers: mixed-methods exploratory research. Eur Manag J 35(2):174–186
VanVactor JD (2011) A case study of collaborative communications within healthcare logistics. Leadersh Health Serv 24(1):51–63
Wan J, Al-awlaqi M, Li M, O’Grady M, Gu X, Wang J, Cao N (2018) Wearable IoT enabled real-time health monitoring system. EURASIP J Wirel Commun Netw 2018(1):298
White F (2015) Primary health care and public health: foundations of universal health systems. Med Principles Pract 24(2):103–116
Wieland A, Wallenburg C (2013) The influence of relational competencies on supply chain resilience: a relational view. Int J Phys Distribution Logistics Manage 43(4):300–320
World Health Organization (2007) Everybody’s business–strengthening health systems to improve health outcomes: WHO’s framework for action Available at: https://apps.who.int/iris/bitstream/handle/10665/43918/9789241596077_eng.pdf (accessed on November 19th 2019)
World Health Organization (2020) Maintaining essential health services: operational guidance for the COVID-19 context. Available at: WHO-2019-nCoV-essential_health_services-2020.2-eng.pdf (accessed on November 3rd 2020)
World Health Organization (2021) Coronavirus disease (COVID-19) pandemic Available at: https://www.euro.who.int/en/health-topics/health-emergencies/coronavirus-covid-19/novel-coronavirus-2019-ncov (accessed on July 18th 2021)
Worldometer (2021) Countries where COVID-19 has spread. Available at: https://www.worldometers.info/coronavirus/countries-where-coronavirus-has-spread/ (accessed on July 29th 2021)
Wu L, Yue X, Jin A, Yen D (2016) Smart supply chain management: a review and implications for future research. Int J Logistics Manage 27(2):395–417
Wu F, Li X, Xu L, Kumari S, Sangaiah A (2018) A novel mutual authentication scheme with formal proof for smart healthcare systems under global mobility networks notion. Comput Electr Eng 68:107–118
Yanamandra R (2018) Development of an integrated healthcare supply chain model. Supply Chain Forum: An International Journal 19(2):111–121
Zaman K, Awan U, Islam T, Paidi R, Hassan A, bin Abdullah A (2016) Econometric applications for measuring the environmental impacts of biofuel production in the panel of worlds’ largest region. Int J Hydrog Energy 41(7):4305–4325
Zanni T (2020) Technology supply chain disruption, KPMG, April. Available at: https://home.kpmg/xx/en/blogs/home/posts/2020/04/technology-supply-chain-disruption.html (accessed on July 1st 2020)
Author information
Authors and Affiliations
Corresponding author
Ethics declarations
Competing of interest
The authors declare that they have no known competing financial interests or personal relationships that could have appeared to influence the work reported in this paper.
Additional information
Publisher’s Note
Springer Nature remains neutral with regard to jurisdictional claims in published maps and institutional affiliations.
Rights and permissions
Springer Nature or its licensor (e.g. a society or other partner) holds exclusive rights to this article under a publishing agreement with the author(s) or other rightsholder(s); author self-archiving of the accepted manuscript version of this article is solely governed by the terms of such publishing agreement and applicable law.
About this article
Cite this article
Tortorella, G.L., Prashar, A., Antony, J. et al. Industry 4.0 adoption for healthcare supply chain performance during COVID-19 pandemic in Brazil and India: the mediating role of resilience abilities development. Oper Manag Res (2023). https://doi.org/10.1007/s12063-023-00366-z
Received:
Revised:
Accepted:
Published:
DOI: https://doi.org/10.1007/s12063-023-00366-z