Abstract
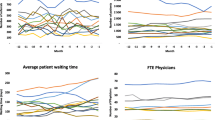
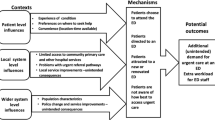
Timely access to dermatology care is poor across the US, especially in underserved geographical areas. Rural regions with fewer practising dermatologists and constrained resources often experience insufficient care access and health outcomes, underscoring the importance of addressing these disparities. However, potential interventions are difficult to compare due to their disruptiveness, time and resource requirements, and institutional resistance, given their uncertain impacts. Queueing and computer simulation models were used to analyse several potential interventions to reduce dermatology appointment delays and gain insights into dynamics and structural inter-relationships. Model logic, candidate interventions, and cost–benefit considerations were developed from mixed-methods analyses of rural access processes and barriers. Sensitivity analyses were conducted. The best of ten investigated interventions reduced internal dermatology access delays from roughly 150 weeks with 95% provider utilisation currently to 0.49 and 72%, respectively. Two other interventions reduced travel for external dermatology care by an estimated 68.1%. Model logic and inputs were developed from the literature and a six-facility rural health system, which may differ in other geographic regions. Model simplifications may not capture all access dynamics, and resources required for some interventions may not be available. Model-based analysis of rural care access disparities can help evaluate and screen potential interventions, develop useful insights, and identify policies worth further evaluating or testing in actual practise. In our rural setting, two interventions appear cost-effective in reducing patient access delays and provider over-utilisation; two others performed too poorly to warrant investing resources to implement or test in practise.



Similar content being viewed by others
Availability of data and material
This manuscript contains results from a secondary analysis of data collected for previously published work.
Code availability
Authors performed mathematical modelling and simulation analyses in Excel. Pseudocode is included in the Appendix.
References
Alghothani L, Jacks SK, Vander Horst A, Zirwas MJ (2012) Disparities in access to dermatologic care according to insurance type. Arch Dermatol 148(8):956–957 2p. https://doi.org/10.1001/archdermatol.2012.804
American Academy of Dermatology Association (2016) Position statement on teledermatology. Retrieved 15 Jul 2019 from https://server.aad.org/Forms/Policies/Uploads/PS/PS-Teledermatology.pdf
American College of Obstetricians and Gynecologists. (2003) Profile of Ob-Gyn Practice. Retrieved from https://www.acog.org/-/media/Departments/Practice/ProfileofOb-gynPractice1991-2003.pdf
American Urological Association (2016) The State of Urology Workforce and Practice in the United States 2016. Retrieved from http://www.auanet.org/common/pdf/research/census/State-Urology-Workforce-Practice-US.pdf
Association of American Medical Colleges (2019) 2019 Update: The Complexities of Physician Supply and Demand: Projections from 2017 to 2032. AAMC. Retrieved from https://aamc-black.global.ssl.fastly.net/production/media/filer_public/31/13/3113ee5c-a038-4c16-89af-294a69826650/2019_update_-_the_complexities_of_physician_supply_and_demand_-_projections_from_2017-2032.pdf
Baldassari C (2019) A day in the life of an academic otolaryngologist practitioner. Retrieved 12 Jul 2019 from https://www.entnet.org/content/day-life-academic-otolaryngologist-practitioner
Basarab T, Munn SE, Jones RR (1996) Diagnostic accuracy and appropriateness of general practitioner referrals to a dermatology outpatient clinic. Br J Dermatol 135(1):70–73. https://doi.org/10.1111/j.1365-2133.1996.tb03610.x
Burton RC, Howe C, Adamson L, Reid AL, Hersey P, Watson A, Armstrong BK (1998) General practitioner screening for melanoma: Sensitivity, specificity, and effect of training. J Med Screen 5(3):156–161. https://doi.org/10.1136/jms.5.3.156
Center for Medicare and Medicaid Services (2016) How to Use the Searchable Medicare Physician Fee Schedule (MPFS). Department of Health and Human Services. Retrieved from http://www.cms.gov/Outreach-and-Education/Medicare-Learning-Network-MLN/MLNProducts/downloads/How_to_MPFS_Booklet_ICN901344.pdf
Chaudhry SB, Armbrecht ES, Shin Y, Matula S, Caffrey C, Varade R, Siegfried E (2013) Pediatric access to dermatologists: Medicaid versus private insurance. J Am Acad Dermatol 68(5):738–748. https://doi.org/10.1016/j.jaad.2012.10.034
Chen SC, Pennie ML, Kolm P, Warshaw EM, Weisberg EL, Brown KM, Weintraub WS (2006) Diagnosing and managing cutaneous pigmented lesions: Primary care physicians versus dermatologists. J Gen Intern Med 21(7):678–682. https://doi.org/10.1111/j.1525-1497.2006.00462.x
Cho KW, Kim SM, Chae YM, Song YU (2017) Application of queueing theory to the analysis of changes in outpatients’ waiting times in hospitals introducing EMR. Healthcare Informatics Research 23(1):35–42. https://doi.org/10.4258/hir.2017.23.1.35
Chowdhury NM, Riddles L, Mackenzie R (2018) Using queueing theory to reduce wait, stay in emergency department
Cyr ME (2019) A Systems Science Approach to Understand and Address Access Barriers to Rural Dermatology Care [Dissertation]. Boston, MA
Cyr ME, Boucher D, Korona S, Guthrie BJ, Benneyan JC (2021) A mixed methods analysis of access barriers to dermatology care in a rural state. J Adv Nurs 77(1):355–366. https://doi.org/10.1111/jan.14604
Dall TM, Gallo PD, Chakrabarti R, West T, Semilla AP, Storm MV, West T (2013) An aging population and growing disease burden will require a large and specialized health care workforce by 2025. Health Aff 32(11):2013–2020. https://doi.org/10.1377/hlthaff.2013.0714
Dorner SC, Jacobs DB, Sommers BD (2015) Adequacy of outpatient specialty care access in marketplace plans under the Affordable Care Act. J Am Med Assoc 314(16):1749–1750. https://doi.org/10.1097/ogx.0000000000000288
Eide MJ, Weinstock MA, Clark MA (2009) Demographic and socioeconomic predictors of melanoma prognosis in the United States. J Health Care Poor Underserved 20(1):227–245. https://doi.org/10.1353/hpu.0.0113
Foster EM, Hosking MR, Ziya S (2010) A spoonful of math helps the medicine go down: An illustration of how healthcare can benefit from mathematical modeling and analysis. BMC Med Res Methodol 10(60):1–11. https://doi.org/10.1186/1471-2288-10-60
Giachetti RE (2008) A simulation study of interventions to reduce appointment lead-time and patient no-show rate. Proceedings - Winter Simulation Conference, (July), 1463–1468. https://doi.org/10.1109/WSC.2008.4736225
Glazer AM, Farberg AS, Winkelmann RR, Rigel DS (2017) Analysis of trends in geographic distribution and density of US dermatologists. JAMA Dermatol 153(4):322–325. https://doi.org/10.1001/jamadermatol.2016.5411
Gombolay M, Golen T, Shah N, Shah J (2019) Queueing theoretic analysis of labor and delivery: Understanding management styles and C-section rates. Health Care Manag Sci 22(1):16–33. https://doi.org/10.1007/s10729-017-9418-2
Goodspeed TA, Page RE, Koman LE, Hollenbeck AT, Gilroy AS (2019) Legal and regulatory issues with teledermatology. Current Dermatology Reports 8(2):46–51. https://doi.org/10.1007/s13671-019-0254-0
Google (2019) Google maps. Retrieved 25 Sept 2019 from https://www.google.com/maps
Green LV (2002) How many hospital beds? Inquiry - Blue Cross and Blue Shield Association 39(4):400–412. Retrieved from http://www.healthleadersmedia.com/finance/how-many-hospital-beds-enough
Green LV (2015) Using operations research to reduce delays for healthcare. State-of-the-Art Decision-Making Tools in the Information-Intensive Age 1–16. https://doi.org/10.1287/educ.1080.0049
Green LV, Savin S (2009) Reducing delays for medical appointments: A queueing approach. Oper Res 56(6):1526–1538. https://doi.org/10.1287/opre.1080.0575
Green LV, Savin S, Murray M (2007) Providing timely access to care: What is the right patient panel size? Jt Comm J Qual Patient Saf 33(4):211–218. https://doi.org/10.1016/S1553-7250(07)33025-0
Guy GP, Ekwueme DU, Tangka FK, Richardson LC (2012) Melanoma treatment costs: A systematic review of the literature, 1990–2011. Am J Prev Med 43(5):537–545. https://doi.org/10.1016/j.amepre.2012.07.031
Hillier FS, Lieberman GJ (2015) Introduction to Operations Research, 10th edn. McGraw-Hill Education, New York, NY
Institute of Medicine (2015) Transforming health care scheduling and access: Getting to now. (G. Kaplan, M. H. Lopez, & J. M. McGinnis, Eds.). Washington, D.C.: National Academies Press. https://doi.org/10.17226/20220
Jayakumar KL, Samimi SS (2018) Trends in US dermatology residency and fellowship programs and positions, 2006 to 2016. J Am Acad Dermatol 78(4):813–815. https://doi.org/10.1016/j.jaad.2017.09.072
Kaplan G, Carayon P, Pronovost P, Rouse W, Reid P, Saunders R (2013) Bringing a Systems Approach to Health. Washington, D.C. Retrieved from http://nam.edu/wp-content/uploads/2015/06/systemsapproaches
Kaplan GS (2015) Health care scheduling and access: A report from the IOM. J Am Med Assoc 314(14):1449–1450. https://doi.org/10.1001/jama.2015.9431
Kilinc MS, Bennett Milburn A (2016) A study of home telehealth diffusion among US home healthcare agencies using system dynamics. IIE Transactions on Healthcare Systems Engineering 6(3):140–161. https://doi.org/10.1080/19488300.2016.1195461
Kim B, Elstein Y, Shiner B, Konrad R, Pomerantz AS, Watts BV (2013) Use of discrete event simulation to improve a mental health clinic. Gen Hosp Psychiatry 35(6):668–670. https://doi.org/10.1016/j.genhosppsych.2013.06.004
Kimball AB, Resneck JS (2008) The US dermatology workforce: A specialty remains in shortage. J Am Acad Dermatol 59(5):741–745. https://doi.org/10.1016/j.jaad.2008.06.037
Lakshmi C, Iyer SA (2013) Application of queueing theory in health care: A literature review. Operations Research for Health Care 2(1–2):25–39. https://doi.org/10.1016/j.orhc.2013.03.002
Lam T, Yeung C, Lam K (2011) What are the learning outcomes of a short postgraduate training course in dermatology for primary care doctors? BMC Med Educ 11(20):1–7. https://doi.org/10.1186/1472-6920-11-20
Lasithiotakis K, Leiter U, Meier F, Eigentler T, Metzler G, Moehrle M, Garbe C (2008) Age and gender are significant independent predictors of survival in primary cutaneous melanoma. Cancer 112(8):1795–1804. https://doi.org/10.1002/cncr.23359
Law A (2014) Simulation Modeling and Analysis, 5th edn. McGraw-Hill Education, New York, NY
Lewis H, Becevic M, Myers D, Helming D, Mutrux R, Fleming DA, Edison KE (2018) Dermatology ECHO - An innovative solution to address limited access to dermatology expertise. Rural Remote Health 18(4415):1–8. https://doi.org/10.22605/rrh4415
Lin CC, Wu CC, Chen CD, Chen KF (2019) Could we employ the queueing theory to improve efficiency during future mass causality incidents? Scandinavian Journal of Trauma, Resuscitation and Emergency Medicine 27(1):1–9. https://doi.org/10.1186/s13049-019-0620-8
Lipworth AD, Park JM, Trefrey BL, Rubin KM, Geller AC, Sober AJ, Tsao H (2011) Urgent access to a specialty care melanoma clinic is associated with a higher rate of melanoma detection. J Am Acad Dermatol 64(6):1060–1067. https://doi.org/10.1016/j.jaad.2010.08.021
Liu KJ, Hartman RI, Joyce C, Mostaghimi A (2016) Modeling the effect of shared care to optimize acne referrals from primary care clinicians to dermatologists. JAMA Dermatol 152(6):655–660. https://doi.org/10.1001/jamadermatol.2016.0183
Liu W, Dowling JP, Murray WK, McArthur GA, Thompson JF, Wolfe R, Kelly JW (2006) Rate of growth in melanomas: Characteristics and associations of rapibly growing melanomas. Arch Dermatol 142(12):1551–1558. https://doi.org/10.1001/archderm.142.12.1551
Lorenzetti DL, Noseworthy T (2011) Patient choice systems and waiting times for scheduled services. Healthc Manage Forum 24(2):57–62. https://doi.org/10.1016/j.hcmf.2011.02.012
Meares HDD, Jones MP (2020) When a system breaks: Queueing theory model of intensive care bed needs during the COVID-19 pandemic. Med J Aust 212(10):470–471. https://doi.org/10.5694/mja2.50605
Merrit Hawkins Team (2017) 2017 Survey of Patient Appointment Wait Times an Medicare and Medicaid Acceptance Rates. Dallas, Texas. Retrieved from https://www.merritthawkins.com/uploadedFiles/MerrittHawkins/Content/Pdf/mha2017waittimesurveyPDF.pdf
Montgomery DC (2019) Design and Analysis of Experiments, 9th edn. John Wiley & Sons Inc., New York, NY
Moreau JF, Geller A, Winger D, Ferris L, Weinstock M (2014) Association between nodular melanoma depth and area-based socioeconomic status, healthcare access, and preventive services use in the United States. J Am Acad Dermatol 70(5):AB80. https://doi.org/10.1016/j.jaad.2014.01.332
Naka F, Lu J, Porto A, Villagra J, Wu ZH, Anderson D (2018) Impact of dermatology eConsults on access to care and skin cancer screening in underserved populations: A model for teledermatology services in community health centers. J Am Acad Dermatol 78(2):293–302. https://doi.org/10.1016/j.jaad.2017.09.017
National Cancer Institute (2019) SEER stat fact sheets: Melanoma of the skin. Retrieved 15 Sept 2019, from http://seer.cancer.gov/statfacts/html/melan.html
Noon CE, Hankins CT, Cote MJ (2003) Understanding the impact of variation in the delivery of healthcare services. J Healthc Manag 48(2):82–98. https://doi.org/10.1097/00115514-200303000-00004
Peter PO, Sivasamy R (2021) Queueing theory techniques and its real applications to health care systems–Outpatient visits. International Journal of Healthcare Management 14(1):114–122. https://doi.org/10.1080/20479700.2019.1616890
Pollack LA, Li J, Berkowitz Z, Weir HK, Wu XC, Ajani UA, Pollack BP (2011) Melanoma survival in the United States, 1992 to 2005. J Am Acad Dermatol 65(5 SUPPL. 1):S78.e1-S78.e10. https://doi.org/10.1016/j.jaad.2011.05.030
Probst JC, Laditka SB, Wang JY, Johnson AO (2007) Effects of residence and race on burden of travel for care: Cross sectional analysis of the 2001 US National Household Travel Survey. BMC Health Serv Res 7(40):1–13. https://doi.org/10.1186/1472-6963-7-40
Resneck J, Kimball AB (2004) The dermatology workforce shortage. J Am Acad Dermatol 50(1):50–54. https://doi.org/10.1016/j.jaad.2003.07.001
Resneck JS, Isenstein A, Kimball AB (2006) Few Medicaid and uninsured patients are accessing dermatologists. J Am Acad Dermatol 55(6):1084–1088. https://doi.org/10.1016/j.jaad.2006.07.012
Resneck JS, Kimball AB (2008) Who else is providing care in dermatology practices? Trends in the use of nonphysician clinicians. J Am Acad Dermatol 58(2):211–216. https://doi.org/10.1016/j.jaad.2007.09.032
Rodríguez Jáuregui GR, González Pérez AK, Hernández González S, Hernández Ripalda MD (2017) Analysis of the emergency service applying the queueing theory. Contaduria y Administracion 62(3):733–745. https://doi.org/10.1016/j.cya.2017.05.001
Rui P, Hing E, Okeyode T (2014) National Ambulatory Medical Care Survey: 2012 Summary Tables. Retrieved from https://www.cdc.gov/nchs/data/ahcd/namcs_summary/2014_namcs_web_tables.pdf
Shi L, Chen S, Sargen M (2016) The current and projected dermatology workforce in the United States. J Am Acad Dermatol 74(5):AB122. https://doi.org/10.1016/j.jaad.2016.02.478
Subramaniam P, Olsen CM, Thompson BS, Whiteman DC, Neale RE (2017) Anatomical distributions of basal cell carcinoma and squamous cell carcinoma in a population-based study in Queensland Australia. JAMA Dermatol 153(2):175–182. https://doi.org/10.1001/jamadermatol.2016.4070
The Center for Connected Health Policy (2019) State Telehealth Laws & Reimbursement Policy: A Comprehensive Scan of the 50 States and the District of Columbia. The National Telehealth Policy Resource Center 420
Tsang MW, Resneck JS (2006) Even patients with changing moles face long dermatology appointment wait-times: A study of simulated patient calls to dermatologists. J Am Acad Dermatol 55(1):54–58. https://doi.org/10.1016/j.jaad.2006.04.001
Uhlenhake E, Brodell R, Mostow E (2009) The dermatology work force: A focus on urban versus rural wait times. J Am Acad Dermatol 61(1):17–22. https://doi.org/10.1016/j.jaad.2008.09.008
US Census Bureau (2018) Quick facts: Aroostook County, Maine. Retrieved 5 May 2019 from https://www.census.gov/quickfacts/fact/table/aroostookcountymaine/PST045218
Warner EL, Montenegro RE, Stroup A, Kinney AY, Kirchhoff AC (2014) Health care concerns of rural childhood cancer survivors. J Health Care Poor Underserved 25(2):901–912. https://doi.org/10.1353/hpu.2014.0095
Williams N (2011) A day in the life of an ENT. Retrieved 7 Jul 2019 from https://www.mytexasent.com/a-day-in-the-life-of-an-ent
Yousefi M, Yousefi M, Fogliatto FS (2020) Simulation-based optimization methods applied in hospital emergency departments: A systematic review. SIMULATION 96(10):791–806
Acknowledgements
The authors thank Dr. Iulian Ilies for study guidance.
Funding
This research was partially supported by a dissertation award from the Sigma Theta Tau International (STTI) Honor Society of Nursing and the National Science Foundation (NSF) grant number IIP-1034990, although all findings and conclusions are solely those of the authors and do not necessarily represent the views of the STTI nor NSF.
Author information
Authors and Affiliations
Contributions
All authors made substantial contributions to concept and design, acquisition of data, or analysis and interpretation of data, and were involved in drafting the manuscript or revising it critically for important intellectual content, and provided final approval of the version to be published.
Corresponding author
Ethics declarations
Conflicts of interest
The authors declare that they have no conflict of interest.
Additional information
Publisher's Note
Springer Nature remains neutral with regard to jurisdictional claims in published maps and institutional affiliations.
Appendices
Appendix
Interventions
Table 4 summarises key themes that were observed from our mixed-methods analysis of patient surveys and staff interviews. Themes were grouped via thematic analysis into five primary categories (clinician education, scheduling, resource identification, patient education, and communication and technology) and informed the specific interventions evaluated in this study (Table 1). Numeric inputs for each intervention are summarised in Table 2.
Simulation Model
The pseudocode used in all simulation models is summarised in Figure 4.
Cost considerations
Table 5 summarises key patient and health system cost categories to consider for each intervention, although cost considerations will vary in any given setting (e.g., reimbursement rates, geographical location, overhead).
Rights and permissions
About this article
Cite this article
Cyr, M.E., Boucher, D., Holmes, A.A. et al. Modelling policy interventions to improve patient access to rural dermatology care. Oper Manag Res 14, 359–377 (2021). https://doi.org/10.1007/s12063-021-00211-1
Received:
Revised:
Accepted:
Published:
Issue Date:
DOI: https://doi.org/10.1007/s12063-021-00211-1