Abstract
Background and Aim The universal use of patient satisfaction as a measure of quality of healthcare cannot be overemphasized, but studies of healthcare satisfaction between older women and older men with multimorbidity in our contemporary society has been questioned over the years. This paper explores the disparities in patient satisfaction between older women and men with multimorbidity in Nigeria using survey data. Methods We analyzed data collected between October 2021 to February 2022 from a cross-section of randomly sampled 734 participants with multimorbidity with age 60 years and above who presented for routine check-ups and consented to participate in the study. The data were entered into JISC online data collection tool and exported to IBM Statistical Package for Social Science (SPSS) version 27 for analysis. Mann-Whitney U test analysis was performed to compare the participant’s mean satisfaction level and gender. Results Despite higher education among males, females utilize healthcare services more. Our study shows that females are less likely to be satisfied with factors that are linked to access and quality of healthcare, and financial burden of medical care. Whereas males are more likely to be satisfied with factors that relate to patient-physician interaction time and patient waiting time and confidence and trust in medical care. Conclusions Female and male patients may have different expectations regarding healthcare, especially in our society where men are more educated, but females utilize the healthcare services more. The development of appropriate strategies for the implementation of knowledge about patient gender differences will be crucial for the delivery of high-quality gender-sensitive healthcare.
Similar content being viewed by others
Avoid common mistakes on your manuscript.
Introduction
The coexistence of multiple chronic diseases in an individual at the same time a term known as multimorbidity is increasingly recognized as an imperative issue of public health and health care system in present-day societies (Nguyen et al., 2019). Despite the rise in life expectancy among lower- and middle-income countries over the last decades, the growing prevalence of multimorbidity has led to a decreased quality of life in patients with chronic diseases, especially in populations with limited resources (Reza et al., 2013), because most healthcare systems are not wholly intended nor satisfactorily prepared to provide personalized care to patients with multimorbidity (Boyd & Fortin, 2010; Hughes et al., 2013). Multimorbidity intensifies the physical complications, social hardships for patients, heavy burden for healthcare systems (Alimohammadian et al., 2017) and could affect overall perceived patient satisfaction with healthcare.
Patient satisfaction promote adherence to prescribed medical and follow-up (Zolnierek & DiMatteo, 2009), however, does not always signify the best outcomes in all cases (Chen et al., 2019). Overall, researchers have identified perceived patient satisfaction to improve healthcare (Chen et al., 2019; Oljira & Ajema, 2016; Ahmad, Nawaz and ud Din, 2011; Khamis & Njau, 2014; Mpinga & Chastonay, 2011; Batbaatar et al., 2015; Abdulsalam & Khan, 2020). Determinants of patient satisfaction are (i) the personal preference of the patient, (ii) the patient’s expectation, (iii) the response tendency of the patient due to personal characteristics, and the quality of care received (Coulter et al., 2009), (iv) the previous experience of the patient and the views of others, such as relatives and friends (Elliot et al., 2010). However, balancing between patients having a great healthcare experience and physicians providing great healthcare is almost always difficult to align. Studies in the USA(Moret et al., 2007) and the UK(Fox & Storms, 1981; Hekkert et al., 2009a) have found that patients with advanced age and literacy-deficient tend to have a higher degree of satisfaction than their younger and functionally literate peers. While some researchers argued that this could be due to lower expectations among older adults (Hekkert et al., 2009a), similarly others observed that their understanding of standard requirements for health facilities may be limited because of their low educational background, and their current experiences may be beyond their expectations (Ahmed et al., 2022a). Some believed that older patients are also likely to be treated with more respect by physicians (Hall & Dornan, 1990).
Gender differences in perception of patient satisfaction attract mixed feelings, with some claiming that female patients have a higher degree of satisfaction and others reaching an opposite conclusion (Hekkert et al., 2009a; Fox & Storms, 1981). Investigating patient satisfaction by gender is worthwhile not only because women are often the healthcare decision-makers in their families, but also, because quality improvement and research in women’s healthcare could benefit from a gender analysis of patient satisfaction data and gender-sensitive perception of patient satisfaction measures (Weisman et al., 2000). Patients have a wide range of expectations regarding organizational aspects of care which should be taken into reasoning when considering likely improvements to the quality of primary care (Sebo et al., 2015). This has important public health implications, and measures should be undertaken to promote equitable healthcare delivery (Okunrintemi et al., 2018). Lastly, improving patient perception of level of healthcare satisfaction positively is vital to high levels of life satisfaction, and studies have shown that it is essential to support the elderly to maintain a high level of life satisfaction, as the elderly with high life satisfaction tend to be more emotionally positive, maintain good health, and have a lower risk of mortality (Bai et al., 2018).
Previous studies have shown that prevalence of multimorbidity is higher among women than men (Ahmed et al., 2023), and that women use more healthcare facilities, particularly public funded healthcare, compared to men (Autenrieth et al., 2013). However, little is known on patient health care satisfaction based on gender among individuals living with multimorbidity in Niger state north central Nigeria. To boost patients’ satisfaction of older people with multimorbidity, it is necessary to investigate the relevant factors of patient satisfaction and to examine the contrasts in factors according to gender. This paper explores the disparities in patient satisfaction between older women and men with multimorbidity in Nigeria using survey data.
Methods
This institutional-based cross-sectional study analyzed data from 4 high-volume purposefully selected public secondary health facilities in Niger state north central Nigeria. We analyzed data from randomly selected 734 participants from these health facilities between October 2021 and February 2022. The inclusion criteria include patients with multimorbidity aged 60 years and above who presented for routine outpatient checkup and consented to participate in the study. Data were collected by a structured interviewer-administered questionnaire, entered into JISC online data collection tool, and exported to SPSS version 27 for analysis. Detailed of the data collection of this study have been described in our previous study (Ahmed et al., 2022a).
The sample size was calculated using the formula for sample size determination when the target population is more than 10,000 (Yamane, 1967). A purposive sampling method was used to select 4 high-volume general hospitals, one each in the 3 senatorial districts and one in the state capital, all having a good representative of multimorbid patients. The total average number of patients seen in 2020 at the four selected secondary health facility was 336,000 total patients and about 105,000 patients 60 years and above (sample frame) are seen at the outpatient department of the 4 sampled hospitals. Substituting the values in the formula.
n = N/1 + N (e)2.
Where n = sample size,
N is the population size (sample frame),
and e is the level of precision. e was defined from power calculations used in other calculation in other similar studies.
105,000/1 + 105,000 (0.05) * (0.05) = 396
To reduce the margin error and allow for drop out of the participants the sample size was increased to about double the calculated value to 800. A systematic random number of 5 was used to select every 5th patient, after identifying the first patient randomly daily. Of the 800 participants contacted for the studies, 734 consented and answered the questionnaire (response rate 91.8%), 66 refused to participate for personal reasons. All four secondary health facilities attained or surpassed the minimum required sample size.
Measures
The outcome variable patient satisfaction was measured with a patient satisfaction questionnaire (PSQ)-18(Marshall & Hays, 1994a) that was adopted on a Likert scale. It is the revised short-form version of PSQ-III and PSQ that retains many characteristics of its full-length counterpart. The PSQ is an assessment tool used to evaluate patients’ perspectives of their doctor’s communication and interpersonal skills (Henriksen et al., 2014). This includes general satisfaction, Technical Quality, Interpersonal Communication, Financial Aspects, Time spent with Doctor, Accessibility, and Convenience. The PSQ-18 has been validated for use in different settings (Marshall & Hays, 1994b). This was developed through rigorous research and abbreviated from much larger questionnaires maintaining internal consistency and reliability (Ware et al., 1976). And the socio-demographic feature i.e. Gender as the predicted variable.
The morbidity was assessed by adopting the list of chronic diseases used in prospective urban and rural epidemiology (PURE) studies (Teo et al., 2009) because the disease on the list fulfills WHO criteria for chronic diseases. For this study, multimorbidity is commonly defined as the co-occurrence of at least two long-term conditions in the same individual and simple disease count was used to measure multimorbidity.
Statistical Analysis
Descriptive statistics were used to summarize the overall characteristics of the participants including gender, age, marital status, family structure, educational level, ethnicity, occupation, and level of income. Mann-Whitney U test analysis was performed to compare the participant’s mean satisfaction level and gender. The assumption for this test was fulfilled because the dependent variable was measured as ordinal (non-parametric) and our independent variable consisted of two categorical (male and female), and there is no relationship between the observations in each group or between the groups themselves. Chi-square was used to test the statistical difference between gender and educational level. Unadjusted and adjusted analysis for gender with education and confounders was perform with Pearson’s correlation.
Results
The socio-demographic characteristics of the respondents for this study include gender, age, marital status, family structure, educational level, occupational level, ethnicity, level of income. Majority of the participants are female (60%), the mean age of the sample is 67.3 years (male 66.3 years and female 68.1 years), married (65.8%), in extended family structure (60%), without any form of education (62.9%), own a business as their occupation (38.1%) and are from the 3 major ethnic groups in the state, see Table 1. The association between sociodemographic features and multimorbidity is shown in Table 2.
Association Between Gender and Educational Level of the Respondents
Table 3 shows the association between gender and educational level. There is a statistically significant difference in educational level between males and females. Males are more educated even though females utilize healthcare services more. Table 4 shows multiple regression analysis for patients’ healthcare satisfaction. In the unadjusted model, gender, family structure, education and ethnicity were found to be associated with patient satisfaction. Moreover, all the factors after adjusted analysis were found to be still present conditional on patient satisfaction with healthcare services.
Association Between Gender and Patient Satisfaction
A statistically significant difference was observed in mean values of patient satisfaction level of males and female with their healthcare pathway experiences. There is a statistical difference in the mean of the males and females in all the items of access to quality healthcare, see Table 5. The mean values were mostly slightly higher in males than females. For items that relate to patients waiting time and patients-physician interaction time, the mean values were higher in females than males except for one item which is Doctors usually spend plenty of time with me. And in all items, except my medical bills are often beyond my reach, there is statistically significant difference in the means of males and females. For perceptions on the financial burden of healthcare the mean values of satisfaction are higher in males. And the item I feel confident that I can get the medical care I need without being set back financially was significant statistically. For perception of confidence and trust in medical care, the mean values were higher in females for 2 items, see Table 5. The item sometimes doctors make me wonder if their diagnosis is correct is statistically significant and the mean value is higher in the males than female.
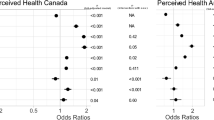
From our previous study (Ahmed et al., 2022b), patient satisfaction items were grouped into 4 dimensions: (1) accessing quality care, (2) patient-physician interaction time and waiting time (3) The financial burden of medical care (4) Confidence and trust in medical care.
Fig. 1 shows the mean summary of the dimension by gender. The overall mean satisfaction score of males is higher than that of females in 2 dimensions i.e., access to quality care and financial burden of treatment, it can be interpreted that females are less likely to be satisfied with access and the quality of healthcare, and financial burden of medical care. Similarly, males are more likely to be satisfied with the patient-physician interaction time and patient waiting time and confidence and trust in medical care.
Discussion
This paper explores the disparities in patient satisfaction between older women and men with multimorbidity in northern part of Nigeria using survey data. Patients’ satisfaction is said to be influenced by the literacy level of the patients and has been adopted widely in developed countries as an index of health care quality (Al-Abri & Al-Balushi, 2014). However, the use of patient’s satisfaction in low-and middle-income countries for quality measurement is inadequate (Kruk & Freedman, 2008). It is important to note that the role of gender in different cultures may vary considerably. Our study was conducted in northern part of Nigeria, where cultural beliefs influence how individuals perceive health and illness. These beliefs are shaped by factors such as religion, language, historical origin, and social constructs of race.
In this study males were found to be more educated than females, but females utilize healthcare services more. This might not be unconnected with the fact that the overall mean score satisfaction of females with medical care was higher in females than males. And the higher satisfaction level among women may justify the higher utilization of healthcare services despite their low education. Possibly, the low level of education among the participants might have contributed to the level of satisfaction seen in this study because two-thirds of the participants do not have any form of education. Our finding is in congruent with findings in the UK and USA that reported higher satisfaction among older adults and advance age/lower education for primary healthcare services (Moret et al., 2007). This was buttressed by researchers who stated that older patients have lower expectations (Hekkert et al., 2009b).
Gender differences in patient satisfaction are not straightforward because they vary according to underlying cultural and social factors (Foss, 2000). The inconsistency in the satisfaction score across items of satisfaction in studies may indicates that female and male patients may have different expectations regarding the practice of the organization (Schmittdiel et al., 2000). For this study, females were more statistically significantly satisfied than males mainly in all items of patient-physician relationship and timing except doctors usually spend plenty of time with me. Although patient satisfaction with healthcare studies across gender among multimorbidity patients is not popular, our findings are tantamount to (Delanois et al., 2018), which reported that staff responsiveness and communication with doctors and nurses were more influential factors of satisfaction for women. In single morbidity studies like patients with inflammatory bowel disease that measured quality of care, it was found that female patients reported lower satisfaction with their overall quality of care (Vasudevan et al., 2013). Also, of importance to note is that the gender disparities were generally larger for older patients with worse self-reported health status (Elliott et al., 2012), this in congruent with our study bearing in mind that the participants in our studies are older patients having 2 or more chronic medical conditions.
Only three items do not show statistically significant differences in the mean satisfaction score between males and females, which include My medical bills are often beyond my reach, I have some doubts about the ability of the doctors who treat me, and Doctors sometimes ignore what I tell them. Therefore, we recommend that practitioners, hospital administrators, relevant stakeholders, and policymakers look for the results based on the findings of every single item of the patient’s experience satisfaction as it is aggregated by gender instead of those based on overall patient satisfaction.
Conclusion and Limitations
Female and male patients may have different expectations regarding healthcare, and this should be taken seriously, especially in our society where men are more educated, but females utilize the healthcare services more. The development of appropriate strategies for the implementation of knowledge about patient gender differences will be crucial for the delivery of high-quality gender-sensitive healthcare. And exploring knowledge of patient-physician gender differences in the future will be paramount to high-quality healthcare. Although our study contributed new perspectives around patient satisfaction in Nigeria, its findings cannot be generalized, however, they can be replicated elsewhere to increase its impact.
References
Abdulsalam, A., & Khan, H. T. (2020). Hospital services for ill patients in the middle-belt geopolitical zone, Nigeria: Patient’s waiting time and level of satisfaction. Illness Crisis & Loss, 28(1), 18–37.
Ahmad, I., Nawaz, A. and ud, & Din, S. (2011). ‘Dynamics of patient satisfaction from health care services’, Gomal Journal of Medical Sciences, 9(1).
Ahmed, A., Khan, H. T., & Lawal, M. (2022a). Effective hospital care delivery model for older people in Nigeria with multimorbidity: Recommendations for practice (p. 1268). Multidisciplinary Digital Publishing Institute.
Ahmed, A., Khan, H. T., & Lawal, M. (2022b). Effective hospital care delivery model for older people in Nigeria with multimorbidity: Recommendations for practice (p. 1268). Multidisciplinary Digital Publishing Institute.
Ahmed, A., Khan, H. T., & Lawal, M. (2023). Systematic literature review of the prevalence, pattern, and determinant of multimorbidity among older adults in Nigeria. Health Services Research & Managerial Epidemiology.
Al-Abri, R., & Al-Balushi, A. (2014). Patient satisfaction survey as a tool towards quality improvement. Oman Medical Journal, 29(1), 3.
Alimohammadian, M., Majidi, A., Yaseri, M., Ahmadi, B., Islami, F., Derakhshan, M., Delavari, A., Amani, M., Feyz-Sani, A., & Poustchi, H. (2017). Multimorbidity as an important issue among women: Results of a gender difference investigation in a large population-based cross-sectional study in West Asia. BMJ open, 7(5), e013548.
Autenrieth, C. S., Kirchberger, I., Heier, M., Zimmermann, A., Peters, A., Döring, A., & Thorand, B. (2013). Physical activity is inversely associated with multimorbidity in elderly men: Results from the KORA-Age Augsburg Study. Preventive Medicine, 57(1), 17–19.
Bai, X., Yang, S., & Knapp, M. (2018). ‘Sources and directions of social support and life satisfaction among solitary Chinese older adults in Hong Kong: the mediating role of sense of loneliness’, Clinical interventions in aging,, pp. 63–71.
Batbaatar, E., Dorjdagva, J., Luvsannyam, A., & Amenta, P. (2015). Conceptualisation of patient satisfaction: A systematic narrative literature review. Perspectives in Public Health, 135(5), 243–250.
Boyd, C. M., & Fortin, M. (2010). Future of multimorbidity research: How should understanding of multimorbidity inform health system design? Public Health Reviews, 32(2), 451–474.
Chen, Q., Beal, E. W., Okunrintemi, V., Cerier, E., Paredes, A., Sun, S., Olsen, G., & Pawlik, T. M. (2019). The association between patient satisfaction and patient-reported health outcomes. Journal of Patient Experience, 6(3), 201–209.
Coulter, A., Fitzpatrick, R., & Cornwell, J. (2009). Measures of patients’ experience in hospital: purpose, methods and uses Citeseer.
Delanois, R. E., Gwam, C. U., Mistry, J. B., Chughtai, M., Khlopas, A., Yakubek, G., Ramkumar, P. N., Piuzzi, N. S., & Mont, M. A. (2018). Does gender influence how patients rate their patient experience after total hip arthroplasty? Hip International, 28(1), 40–43.
Elliot, R., Pearce, C. J., Seifert, C., & Calder, D. J. (2010). Continuous infusion versus single bolus popliteal block following major ankle and hindfoot surgery: A prospective, randomized trial. Foot & Ankle International, 31(12), 1043–1047.
Elliott, M. N., Lehrman, W. G., Beckett, M. K., Goldstein, E., Hambarsoomian, K., & Giordano, L. A. (2012). Gender differences in patients’ perceptions of inpatient care. Health Services Research, 47(4), 1482–1501.
Foss, C. (2000). Gender as a variable in patient satisfaction. Tidsskrift for den Norske Laegeforening: Tidsskrift for Praktisk Medicin Ny Raekke, 120(27), 3283–3286.
Fox, J. G., & Storms, D. M. (1981). A different approach to sociodemographic predictors of satisfaction with health care. Social Science & Medicine Part A: Medical Psychology & Medical Sociology, 15(5), 557–564.
Hall, J. A., & Dornan, M. C. (1990). Patient sociodemographic characteristics as predictors of satisfaction with medical care: A meta-analysis. Social Science & Medicine, 30(7), 811–818.
Hekkert, K. D., Cihangir, S., Kleefstra, S. M., van den Berg, B., & Kool, R. B. (2009a). Patient satisfaction revisited: A multilevel approach. Social Science & Medicine, 69(1), 68–75.
Hekkert, K. D., Cihangir, S., Kleefstra, S. M., van den Berg, B., & Kool, R. B. (2009b). Patient satisfaction revisited: A multilevel approach. Social Science & Medicine, 69(1), 68–75.
Henriksen, K. M., Heller, N., Finucane, A. M., & Oxenham, D. (2014). Is the patient satisfaction questionnaire an acceptable tool for use in a hospice inpatient setting? A pilot study. BMC Palliative care, 13, 1–6.
Hughes, L. D., McMurdo, M. E., & Guthrie, B. (2013). Guidelines for people not for diseases: The challenges of applying UK clinical guidelines to people with multimorbidity. Age and Ageing, 42(1), 62–69.
Khamis, K., & Njau, B. (2014). Patients’ level of satisfaction on quality of health care at Mwananyamala hospital in Dar Es Salaam, Tanzania. BMC Health Services Research, 14(1), 1–8.
Kruk, M. E., & Freedman, L. P. (2008). Assessing health system performance in developing countries: A review of the literature. Health Policy, 85(3), 263–276.
Marshall, G. N., & Hays, R. D. (1994a). The patient satisfaction questionnaire short-form (PSQ-18) Rand Santa Monica, CA.
Marshall, G. N., & Hays, R. D. (1994b). The patient satisfaction questionnaire short-form (PSQ-18) Rand Santa Monica, CA.
Moret, L., Nguyen, J., Volteau, C., Falissard, B., Lombrail, P., & Gasquet, I. (2007). Evidence of a non-linear influence of patient age on satisfaction with hospital care. International Journal for Quality in Health Care, 19(6), 382–389.
Mpinga, E. K., & Chastonay, P. (2011). Satisfaction of patients: A right to health indicator? Health Policy, 100(2–3), 144–150.
Nguyen, H., Manolova, G., Daskalopoulou, C., Vitoratou, S., Prince, M., & Prina, A. M. (2019). Prevalence of multimorbidity in community settings: A systematic review and meta-analysis of observational studies. Journal of Comorbidity, 9, 2235042X19870934.
Niger state Nigeria 2 College of Nursing, Midwifery, and Healthcare.
Okunrintemi, V., Valero-Elizondo, J., Patrick, B., Salami, J., Tibuakuu, M., Ahmad, S., Ogunmoroti, O., Mahajan, S., Khan, S. U., & Gulati, M. (2018). Gender differences in patient‐reported outcomes among adults with atherosclerotic cardiovascular disease. Journal of the American Heart Association, 7(24), e010498.
Oljira, H., & Ajema, A. (2016). Predictors of patient satisfaction with the Health Care Services Provided in Oromia Regional State Public Hospitals, Ethiopia. J Health Med Nurs, 31, 56–65.
Reza, A., Rusk, I. S., & Robab, S. (2013). Aging in Iran: Past, present and future. J Aging Em Economies, 4, 17–34.
Schmittdiel, J., Grumbach, K., Selby, J. V., & Quesenberry, C. P. (2000). Effect of physician and patient gender concordance on patient satisfaction and preventive care practices. Journal of General Internal Medicine, 15(11), 761–769.
Sebo, P., Herrmann, F. R., Bovier, P., & Haller, D. M. (2015). What are patients’ expectations about the organization of their primary care physicians’ practices? BMC Health Services Research, 15(1), 1–13.
Teo, K., Chow, C. K., Vaz, M., Rangarajan, S., Yusuf, S., & PURE Investigators-Writing Group. (2009). The prospective Urban Rural Epidemiology (PURE) study: Examining the impact of societal influences on chronic noncommunicable diseases in low-, middle-, and high-income countries. American Heart Journal, 158(1), 1–7. e1.
Vasudevan, A., Arachchi, A., & van Langenberg, D. R. (2013). Assessing patient satisfaction in inflammatory bowel disease using the QUOTE-IBD survey: A small step for clinicians, a potentially large step for improving quality of care. Journal of Crohn’s and Colitis, 7(9), e367–e374.
Ware, J. E., Snyder, M. K., & Wright, W. R. (1976). ‘Development and validation of scales to measure patient satisfaction with medical care services’, National Technical Information Service: Springfield VA,.
Weisman, C. S., Rich, D. E., Rogers, J., Crawford, K. G., Grayson, C. E., & Henderson, J. T. (2000). Gender and patient satisfaction with primary care: Tuning in to women in quality measurement. Journal of Women’s Health & gender-based Medicine, 9(6), 657–665.
Yamane, T. (1967). Statistics: An introductory analysis (2nd ed.). Harper and Row.
Zolnierek, K. B. H., & DiMatteo, M. R. (2009). Physician communication and patient adherence to treatment: A meta-analysis. Medical care, 47(8), 826.
Funding
No funding was received to assist with the preparation of this manuscript. No funding was received for conducting this study. No funds, grants, or other support was received.
Author information
Authors and Affiliations
Corresponding author
Ethics declarations
Ethical Approval
Ethical approval was obtained from the College of Nursing, Midwifery, and Healthcare, the Research Ethics Panel (Ethical Approval No. 1055), and authorization to collect data was sought from the Research, Ethics, and publication committee (REPC) of the Hospitals Management Board, Minna, Niger state of Nigeria.
Informed Consent
The researchers read out details of the research to participants and provided them in writing. Participants could freely sign an informed consent form prior to participating in the study, and the individual’s right to withdraw partially or completely was observed.
Compliance with Ethical Standards
I, the undersigned, give my consent for the publication of identifiable details, which can include text and/tables and/or figure and/or details within the article to be published in the above Journal. The authors confirm that the data supporting the findings of this study are available within the article [and/or] its supplementary materials.
Conflict of Interest
The authors declare no conflicts of interest.
Additional information
Publisher’s Note
Springer Nature remains neutral with regard to jurisdictional claims in published maps and institutional affiliations.
Rights and permissions
Open Access This article is licensed under a Creative Commons Attribution 4.0 International License, which permits use, sharing, adaptation, distribution and reproduction in any medium or format, as long as you give appropriate credit to the original author(s) and the source, provide a link to the Creative Commons licence, and indicate if changes were made. The images or other third party material in this article are included in the article’s Creative Commons licence, unless indicated otherwise in a credit line to the material. If material is not included in the article’s Creative Commons licence and your intended use is not permitted by statutory regulation or exceeds the permitted use, you will need to obtain permission directly from the copyright holder. To view a copy of this licence, visit http://creativecommons.org/licenses/by/4.0/.
About this article
Cite this article
Ahmed, A., Khan, H.T. & Lawal, M. Patients’ Satisfaction with Healthcare Services Among Older People with Multimorbidity: Subnational Gender Perspective. Population Ageing (2024). https://doi.org/10.1007/s12062-024-09455-8
Received:
Accepted:
Published:
DOI: https://doi.org/10.1007/s12062-024-09455-8