Abstract
Frailty is a common syndrome affecting older adults. While frailty has well-established relationships with multiple adverse health outcomes and death, the role of the social and economic environment in the development of frailty is less clear. We consider this relationship in India, which has a growing population of older adults whose environments have undergone extensive social and economic changes over the last few decades. We compare the distributions of frailty among older adults across the states of India and explore the influence of both current social and economic indicators and historical indicators at the state level. We find substantial variation in the state-level prevalence of frailty, which remains even after sex stratification and age standardization. We also find significant associations between frailty and current (2018) and historic (1981) state-level socioeconomic variables. We conclude with a discussion of the scientific and policy implications of early-life and contemporaneous social and economic conditions for the frailty of older adults.
Similar content being viewed by others
Avoid common mistakes on your manuscript.
Introduction
With a population of 1.38 billion—almost 18% of the world population—India is undergoing an unprecedented demographic transition due to decreasing birth and death rates and increasing life expectancy. Consequently, the number and proportion of Indians aged 65 and older are rising rapidly. Projections indicate that the proportion of the 65 and older population will double from 7% to 2022 to 15% in 2050. The absolute number of this population will also more than double from 90 million in 2020 to 225 million in 2050.(UNPD 2022) The aging of India’s population has significant implications for the provision of health and social services and for India’s continued economic growth.
While much work on healthy aging has focused on individual-level factors, such as health behaviors or socioeconomic status, ecological exposures such as the physical environment, governmental policies, and neighborhood characteristics are also critical (Gill et al., 2021; Wilker et al., 2023; Modrek et al., 2022). Understanding these links is key for efforts to improve the health of older adults, particularly through health-related policy. Many studies to date have focused on either sub-national populations (e.g. individual states in the United States of America) that may have more limited variation, or cross-national comparisons that have greater concerns for unmeasured confounding (Modrek et al., 2022; Gill et al., 2021; Theou et al., 2013). India provides a particularly rich setting for this work: a single country with shared historical experiences and national policies that may limit some unmeasured confounding. However, its 36 states and union territories (UTs) have significant power to set their own policies, including health policies. In addition, these regions differ widely in age structure, language, religion, wealth, and economic base. These comprise a broad array of ecological-level variations that can be considered in studying the health of older adults (See Supplementary Table 5).
Frailty, which is a common health condition affecting 7–24% of older adults, provides a useful framework for the overall health of older adults (O’Caoimh et al., 2021). Defined as impaired recovery from physiologic stress, frailty has been associated with many adverse health outcomes and higher mortality (Clegg et al., 2013; Hoogendijk et al., 2019). Its distribution in populations has been associated with national-level measures of wealth, and it may serve as an indicator of the health of an aging population (Theou et al., 2013). Frailty is typically operationalized using one of two approaches (Walston et al., 2019). The first approach, physical or phenotypic frailty, treats frailty as a discrete state that manifests as weakness, slowing, and reduced energy expenditure defined by specific criteria. The Fried frailty phenotype is the main example of this and defines frailty in terms of reduced grip strength, slowed gait speed, reduced physical activity, weight loss, and exhaustion or fatigue (Fried et al., 2001). The other major approach, deficit accumulation, treats frailty as an emergent property of the development of multiple problems with physical health, mental health and cognition, function and self-care, and other domains related to wellbeing (Rockwood and Mitnitski 2007). This is assessed using a fixed index of potential deficits spanning these domains, with the proportion of deficits identified for an individual serving as their frailty index, a continuous score ranging from 0 to 1 (Searle et al., 2008). Both phenotypic and deficit-accumulation frailty are valid tools for assessing frailty in populations, though they may identify different individuals as frail (Rockwood et al., 2007).
Previous studies in India have reported frailty prevalences ranging from 11 to 59% (Jotheeswaran et al., 2015; Srivastava & Muhammad, 2022; Kendhapedi and Devasenapathy 2019; Biritwum et al., 2016; Kashikar and Nagarkar 2016) in various urban and rural areas. However, these studies are limited by sample size and by different operational definitions of frailty, making cross-state comparisons challenging. The most recent data available on frailty are from the 2015 WHO-SAGE survey (Arokiasamy et al. 2020), which surveyed 6,000 adults aged 50 years or older in six states of India. The investigators, using the Fried frailty phenotype (Fried et al., 2001), reported 55% of the sample to be pre-frail and 20% frail. However, representative estimates of frailty across all states are lacking. Additionally, the associations between frailty and historic and current state-level social and economic indicators have not been assessed.
In this paper we look at the relationship between frailty and state-level ecological exposures among older Indians. We first consider the variation in frailty across India’s states and UTs. Then, we look at how three measures of state-level economic, health, and social wellbeing are associated with frailty after adjustment for individual-level factors. We consider contemporaneous and lagged measures to clarify how timing of exposure may affect subsequent outcomes.
Methods
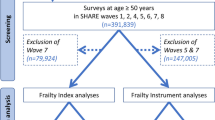
Data
Data are from wave 1 of the Longitudinal Aging Study in India (LASI), a representative, population-based longitudinal study modeled on the Health and Retirement Study in the United States. In the first wave, 72,262 community-dwelling adults aged 45 years and older (including their spouses irrespective of age) were interviewed in 2017–2019. Participants were from 35 to 36 states and UTs of India, except for Sikkim. We restricted our analytical sample to those aged 50 and older.
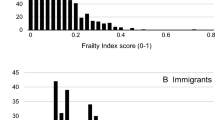
Frailty was assessed using a deficit-accumulation frailty index based on a standard procedure (Searle et al., 2008; Rockwood and Mitnitski 2007). Starting with 57 variables drawn from areas of health, cognition, mental health, (instrumental) activities of daily living, and mobility, variables were scaled to range from 0 to 1. Variables were then excluded from the index if more than 10% of values were missing, if prevalence was less than 10%, if correlation with age was less than 0.05, or if prevalence reached 80% before age 80. The final index comprised 47 variables covering three domains: physical health, mental health and cognition, and function. Supplementary Table 1 lists the variables used. Frailty index (FI) for participant i summing over the 47 deficits denoted j was calculated using the following formula, resulting in values between 0 and 1:
When categorized, we used the following cut-offs: robust was defined as an FI of 0–0.1, pre-frail was > 0.1–0.2, mildly frail > 0.2–0.3, moderately frail > 0.3–0.4, and severely frail was > 0.4. When dichotomized, non-frail was defined as 0–0.2, while frail was defined as > 0.2.
Demographic and socioeconomic variables used in the regression analyses were age, gender, religion, caste, education, household income, household wealth, and household consumption. We additionally considered three state-level measures—state gross domestic product (GDP) per capita, infant mortality rate (IMR), and literacy rate (literacy)—indicating the economic, health, and social situation of the states, respectively. State GDP data were obtained from the Reserve Bank of India (RBI) and the Ministry of Statistics and Programme Implementation; IMR data were obtained from the Office of Registrar General of India, Ministry of Home Affairs, and RBI; and literacy rates were obtained from the 2011 Census of India (Office of the Registrar General of India, 2003; Ministry of Statistics and Programme Implementation, 1999; “Reserve Bank of India - Handbook of Statistics on Indian Economy” n.d.; Office of the Registrar General & Census Commissioner n.d.). Due to limitations in the availability of state-wise historical data before 1980, we used data for the year 1981 to get an historical overview of social and economic indicators, and for contemporary indicators, we used 2018 data (for literacy we used census data from 2011). The LASI respondents who were 50 years old in 2017–2019 would have been in their 20s in 1981. Geospatial data for India to produce choropleth maps were obtained from GADM (a free online resource for administrative maps) (GADM, 2018).
Theoretical Model
Several studies document a strong association between the frailty of older adults and their socio-economic status and life experiences (Maharani et al., 2023; Brunner et al., 2018; Zimmer et al., 2021; Wang and Hulme 2021). Additionally, as noted above, there is ample evidence that ecological factors such as economic, health, and infrastructure policies, are associated with the health of older adults (Gill et al., 2021; Modrek et al., 2022; Wilker et al., 2023; Theou et al., 2013). In this paper, we test these propositions in the India country context exploiting cross-state ecological variations and individual variations in wealth and education. In keeping with the literature, we hypothesize that state-level social and economic policy influence frailty among older Indians who are similarly situated in terms of their wealth and education. To test this hypothesis, we use IMR as a proxy for health care, literacy rates as a proxy for education, and GDP per capita as a proxy for wealth. Frailty is used as a representation of health for older adults. The association between state-level policies and frailty may change, either in magnitude or direction, depending on when they are encountered over the life-course. To consider different points in the life course, we look at the three state-level measures at two time points. We outline this diagrammatically as a timeline of the exposures and outcome in Supplementary Fig. 1.
Analytic Approach
We first considered the prevalence of frailty by sex and by state/UT in India. We looked at crude distributions and age-/sex-standardized distributions to represent the sex-specific age distribution of India. These data were then used to produce statistical thematic maps.
To assess the association between state-level characteristics and frailty, we conducted beta regression of the frailty index values of LASI participants on each state-level indicator (GDP, IMR, and literacy). We included age, gender, religion, caste, education, household income, household wealth, and household consumption as covariates and used individual survey weights. For the national-level estimates, we also used state fixed effects. To investigate cohort effects, we also ran these models separately for those aged 50 to 59, 60 to 69, 70 to 79, and 80 or older at the time of the survey in 2017–2019.
We used beta regression as index values are bounded between 0 and 1. Like a logistic regression, where exponentiated coefficients represent the change in the odds of the outcome for a unit change in the independent variable, the coefficients in a beta regression can be interpreted as the change in the odds that a randomly selected deficit in the index is present. Thus, we present regression coefficients as odds ratios. Analysis and adjustments were conducted in STATA 15 (StataCorp, 2017) and choropleth maps were produced in R version 4.1.1 (R Core Team, 2021).
Results
Table 1 shows the characteristics of our sample of participants in the first wave of LASI. A majority of participants were female, Hindu, not of scheduled castes, and had no education or less than a high school level of education. 55% of participants were frail.
Figure 1 and Supplementary Table 2 show the prevalence of frailty by state/UT for combined sexes of adults aged 50 and older. Certain zones of India appear to have a greater prevalence of frailty, particularly eastern and western zones. Figure 2 and Supplementary Table 3 show sex-stratified, age-standardized frailty prevalence by state. The prevalence of age-standardized frailty is greater among females than among males. Geographical patterns resemble unadjusted results: states in the eastern and western zones have a greater prevalence of frailty for either sex.
To identify which domains of the frailty index drive these findings, Supplementary Tables 4a–c present results for each frailty index domain. These tables present the mean proportion of deficits within each domain by state and separated by sex. Sex differences are larger for function and cognition than for physical health, with females generally having more deficits than males. For both sexes, cognition had the largest proportion of items showing deficits.
Table 2 presents regression results for the full sample with state-level indicators and state fixed effects. The presence of the odds ratio for deficits, which is consistent with greater frailty, increases with increasing age and female gender. Identification as Muslim is associated with greater frailty; however, other identities that face discrimination, i.e., scheduled tribe, scheduled caste, and other backward class, are associated with lower odds ratios. At the household level, lower income and wealth are both associated with greater frailty, while lower consumption is associated with lower frailty. State-level indicators show a statistically significant but small increase in frailty with greater IMR for both 1981 and 2018 measures. State GDP per capita and literacy have similar patterns, with 1981 values being associated with greater frailty and 2018 (2011 for literacy) values associated with lower frailty. These associations are more prominent for state GDP per capita, while the results for literacy are small. Additionally, we conducted an F-test to see the joint effect of state-level indicators at both time points on frailty and found a significant effect F(6, 44,847) = 127.10, p < 000.1.
Table 3 shows age-stratified results. Variables assessed at the individual and household levels maintain similar relationships as observed in the combined results. Among state-level variables, the most notable difference is an apparent attenuation in the associations between state GDP per capita and frailty with increasing age, for values from both 1981 and 2018. However, the direction of effect remains the same as the combined results, with greater GDP per capita in 1981 associated with greater frailty and greater GDP per capita in 2018 associated with lower frailty.
Discussion
Our study is the first to provide recent estimates of frailty for India and 35 states and UTs, except for Sikkim. Around 55% of adults aged 50 + in India are frail. However, prevalence varies widely across states: the lowest prevalence is 28% in Nagaland (a northeastern state) and the highest is nearly 67% in West Bengal. The Indian population is aging; frailty is a useful tool for understanding its changing health. There have been multiple efforts in the past to measure frailty in India; however, due to the lack of state-representative data (until now), no state-level estimates of frailty have been available for the country. Earlier epidemiological studies have reported frailty prevalences ranging from 11 to 59% for different urban and rural areas (Srivastava & Muhammad, 2022; Kashikar and Nagarkar 2016; Jotheeswaran et al., 2015; Biritwum et al., 2016; Kendhapedi and Devasenapathy 2019). A 2019 study conducted in Haryana by researchers at the All India Institute of Medical Science estimated the prevalence of frailty at around 47% using a 12-item frailty instrument from the World Health Organization (Rath et al., 2021). Another study in the Thanjavur district of Tamil Nadu in southern India in 2019 found a prevalence of frailty of around 59% in that population using a 40-item frailty index (Kendhapedi and Devasenapathy 2019), which is similar to the estimated prevalence in Tamil Nadu (57%) in our study. Further, a study based on the WHO-SAGE 2007 data used a 40-item frailty index and found 82% of adults aged 50 or older in Uttar Pradesh to be frail (a frailty score of > 0.2) (Chaudhary and Arokiasamy 2019), which is much higher than the prevalence found in our study (55%). Nonetheless, all studies, including ours, have estimated a high prevalence of frailty among adults aged 50 + in India.
We found substantial variation in the state-level prevalence of frailty, which remained even after sex stratification and age standardization. This finding suggests that population structure alone does not explain the heterogeneity in frailty prevalence across states. Because health is a state matter in India, our study provides crucial information about the prevalence of frailty and its subdomains. This may aid state-level policymakers by identifying focus areas for interventions, particularly given the high prevalence of deficits related to mental health and cognition.
Our findings align with other studies that have investigated the association between socioeconomic and demographic variables and frailty. We found statistically significant associations of frailty with greater age, female sex, no or less education, lower income, and lower wealth. However, the relationship between poverty and frailty at the state level is unclear: while some states, such as Bihar, have high poverty rates and a high prevalence of frailty, other states with high rates of poverty, such as Chhattisgarh, do not. As age structure does not explain these differences, understanding the role of state-level policies may identify ways to improve the health of poorer older adults.
In addition to individual-level socioeconomic circumstances, regional and national social and economic environments have been found to affect health. However, the literature investigating the association between frailty and historical and contemporaneous social and economic indicators at the ecological level is limited. Regression modeling of individuals using state-level IMR, literacy, and GDP per capita shows significant associations with frailty for both contemporaneous (2018) and lagged (1981) variables. The directions of association—greater frailty with more favorable values of the lagged variables (i.e., lower IMR and higher literacy and GDP) and lower frailty for the contemporaneous variables—merits further exploration. To further control for age, we repeated these regressions on age-stratified portions of our sample with broadly similar findings. Several explanations for this finding are possible. Lagged indicators may reflect survival to develop frailty, while contemporaneous ones reflect maintenance of health by medical care. Lagged indicators could potentially represent early-life conditions leading to a propensity for frailty; however, favorable social conditions in early life are typically associated with a lower risk of illness in later life (Mallinson et al., 2020). These findings emphasize that aging-related policies should not only target older populations but should also focus on the younger population given that the social and economic environment at a younger age contributes to old-age health and wellbeing. These findings are novel and should be investigated in other cohorts.
This study has some notable limitations. We assumed that respondents’ current state of residence was the same as their state of residence in 1981 for lagged indicators. Lagged indicators could not be obtained at specific ages for all participants, particularly at birth or in early childhood when sensitivity to the exposure may be greater. This limits the conclusions that can be drawn about the timing of exposure and development of frailty. Additionally, as we only can observe individuals who survived to older age, the role of mortality selection in explaining our findings cannot be determined. Finally, because we used cross-sectional data, any causal or temporal relationship between frailty and socioeconomic indicators cannot be established. However, future longitudinal waves of LASI will allow us to delve deeper into the causal pathways of frailty in the country.
Focus on frailty research is increasing globally, as frailty is expected to have implications for both clinical practice and public health. In India, immediate family members largely care for elders, but this system faces significant challenges amid rapid social change. As the population ages, home and community care services will need to increase to support older adults in remaining healthy and at home, as will long-term care for those unable to safely remain independent (Agarwal and Bloom 2022). Meeting these needs will require great investments in social and medical care. Frailty assessment will help clinicians and policymakers understand the health of older adults and strategize future investments.
In conclusion, we find wide variation in the age-standardized prevalence of frailty among India’s states using the frailty index. Further explorations are needed to compare the different measures of physical disability and frailty to check for concordance. Among individuals, frailty is associated with state-level indicators of social and economic wellbeing, though this association appears to change with time. Further work that examines early-life conditions using longitudinal cohorts will help clarify how such indicators are linked to frailty and how policies affecting them can improve the health of older adults.
References
“Reserve Bank of India - Handbook of Statistics on Indian Economy.” n.d. Accessed March 31 (2022). https://www.rbi.org.in/scripts/AnnualPublicationsaspx?head=Handbook of Statistics on Indian Economy.
Agarwal, A., and David E. Bloom (2022). Long-term care in India: Capacity, need and future. International Social Security Review, 75(3–4), 167–186. https://doi.org/10.1111/ISSR.12312.
Arokiasamy, Perianayagam, T. V., Sekher, H., Lunghdim, M., Dhar, & Roy, A. K. (2020). INDIA Study on Global AGEing and Adult Health (SAGE), Wave 2 WHO SAGE WAVE 2.”.
Biritwum, R. B., Minicuci, N., Yawson, A. E., Theou, O., Mensah, G. P., Naidoo, N., Wu, F., et al. (2016). Prevalence of and Factors Associated with Frailty and disability in older adults from China, Ghana, India, Mexico, Russia and South Africa. Maturitas, 91(September), 8–18. https://doi.org/10.1016/J.MATURITAS.2016.05.012.
Brunner, E. J., Martin, J., Shipley, S., Ahmadi-Abhari, C. V., Hernandez, J. G., Abell, A., Singh-Manoux, I., & Kawachi, and Mika Kivimaki (2018). Midlife contributors to socioeconomic differences in Frailty during later life: A prospective cohort study. The Lancet Public Health, 3(7), e313–e322. https://doi.org/10.1016/S2468-2667(18)30079-3.
Chaudhary, M., and Perianayagam Arokiasamy (2019). Patterns of Frailty and Quality of Life among older adults: Comparative analysis using SAGE States of India. Journal of Population Ageing, 12(1), 1–23. https://doi.org/10.1007/S12062-017-9201-7/TABLES/4.
Clegg, A., Young, J., Iliffe, S., & Rikkert, M. O., and Kenneth Rockwood (2013). Frailty in Elderly people. Lancet, 381(9868), 752–762. https://doi.org/10.1016/S0140-6736(12)62167-9.
R Core Team (2021). “R: A Language and Environment for Statistical Computing.” R Foundation for Statistical Computing, Vienna, Austria. 2021. https://www.r-project.org/.
Fried, L. P., Tangen, C. M., Walston, J., Newman, A. B., Hirsch, C., Gottdiener, J., Seeman, T., et al. (2001). Frailty in older adults: Evidence for a phenotype. Journals of Gerontology - Series A Biological Sciences and Medical Sciences, 56(3), https://doi.org/10.1093/GERONA/56.3.M146.
GADM (2018). “GADM Data (Version 3.6).” 2018. https://gadm.org/download_country_v3.html.
Gill, T. M., Emma, X., Zang, T. E., Murphy, L., Leo-Summers, E. A., Gahbauer, N., Festa, J. R., & Falvey, and Ling Han (2021). Association between Neighborhood Disadvantage and Functional Well-being in community-living older persons. JAMA Internal Medicine, 181(10), 1297–1304. https://doi.org/10.1001/JAMAINTERNMED.2021.4260.
Hoogendijk, E. O., Afilalo, J., Ensrud, K. E., Kowal, P., Onder, G., & Fried, L. P. (2019). Frailty: Implications for Clinical Practice and Public Health. Lancet. https://doi.org/10.1016/S0140-6736(19)31786-6.Lancet Publishing Group.
Jotheeswaran, A. T., Bryce, R., Prina, M., Acosta, D., Ferri, C. P., Guerra, M., Huang, Y., et al. (2015). Frailty and the prediction of dependence and mortality in low- and Middle-Income countries: A 10/66 Population-based Cohort Study. BMC Medicine, 13(1), https://doi.org/10.1186/S12916-015-0378-4.
Kashikar, Y., and Aarti Nagarkar (2016). Prevalence and determinants of Frailty in older adults in India. Indian Journal of Gerontology, 30(3), 364–381.
Kendhapedi, K. K., and Niveditha Devasenapathy (2019). Prevalence and Factors Associated with Frailty among Community-Dwelling Older people in Rural Thanjavur District of South India: A cross-sectional study. British Medical Journal Open, 9(10), https://doi.org/10.1136/BMJOPEN-2019-032904.
Maharani, A., Sinclair, D. R., Chandola, T., Bower, P., Clegg, A., Hanratty, B., Nazroo, J., et al. (2023). Household Wealth, Neighbourhood deprivation and Frailty amongst Middle-aged and older adults in England: A longitudinal analysis over 15 years (2002–2017). Age and Ageing, 52(3), 1–10. https://doi.org/10.1093/AGEING/AFAD034.
Mallinson, P., Lieber, J., & Bhogadi, S. (2020). Childhood Socio-Economic conditions and Risk of Cardiovascular Disease: Results from a pooled sample of 14 011 adults from India. J Epidemiol Community Health, 74, 831–837. https://doi.org/10.1136/jech-2020-214016.
Ministry of Statistics and Programme Implementation (1999). State domestic product (State Series) 1980-81. 1999. http://www.mospi.gov.in/publication/state-domestic-product-state-series-1980-81.
Modrek, S., Roberts, E., Warren, J. R., & Rehkopf, D. (2022). Long-Term effects of local-area New Deal Work Relief in Childhood on Educational, Economic, and Health outcomes over the Life Course: Evidence from the Wisconsin Longitudinal Study. Demography, 59(4), 1489–1516. https://doi.org/10.1215/00703370-10111856.
O’Caoimh, R., Sezgin, D., Mark, R., O’Donovan, D. W., Molloy, A., Clegg, K., Rockwood, A., Liew, et al. (2021). Prevalence of Frailty in 62 Countries across the World: A systematic review and Meta-analysis of Population-Level studies. Age and Ageing, 50(1), 96–104. https://doi.org/10.1093/ageing/afaa219.
Office of the Registrar General & Census Commissioner, Government of India. n.d (2023). “Census Tables | Government of India.” Accessed May 30, https://censusindia.gov.in/census.website/data/census-tables.
Office of the Registrar General of India (2003). “State-Wise Infant Mortality Rate.” https://www.indiabudget.gov.in/economicsurvey/doc/stat/tab82.pdf.
Rath, R., Kumar, R., Amarchand, R., Gopal, G., Purakayastha, D., Chhokar, R., Narayan, V., & Dey, A., and Anand Krishnan (2021). Frailty, disability, and Mortality in a Rural Community-Dwelling Elderly Cohort from Northern India. Indian Journal of Community Medicine: Official Publication of Indian Association of Preventive & Social Medicine, 46(3), 442. https://doi.org/10.4103/IJCM.IJCM_616_20.
Rockwood, K., and Arnold Mitnitski (2007). Frailty in Relation to the Accumulation of deficits. The Journals of Gerontology Series A Biological Sciences and Medical Sciences, 62(7), 722–727. https://doi.org/10.1093/GERONA/62.7.722.
Rockwood, K., Andrew, M., & Mitnitski, A. (2007). A comparison of two approaches to measuring Frailty in Elderly people. Journals of Gerontology. Series A, Biological Sciences and Medical Sciences, 62A(7), M738–M743. https://doi.org/10.1093/gerona/62.7.738.
Searle, S. D., Arnold Mitnitski, E. A., Gahbauer, Thomas, M., & Gill, and Kenneth Rockwood (2008). A Standard Procedure for creating a Frailty Index. BMC Geriatrics, 8(1), 24. https://doi.org/10.1186/1471-2318-8-24.
Srivastava, S., & Muhammad, T. (2022). “Socioeconomic Vulnerability and Frailty among Community-Dwelling Older Adults: Cross-Sectional Findings from Longitudinal Aging Study in India, 2017–18.” BMC Geriatrics 2022 22:1 22 (1): 1–11. https://doi.org/10.1186/S12877-022-02891-1.
StataCorp (2017). Stata Statistical Software: Release 15. College Station. StataCorp LLC.” College Station, TX: StataCorp LLC.
Theou, O., Brothers, T. D., Rockwood, M. I. C. H. A. E. L. R., Haardt, D., & Mitnitski, A., and Kenneth Rockwood (2013). Exploring the relationship between National Economic Indicators and relative fitness and Frailty in Middle-aged and older europeans. Age and Ageing, 42(5), 614. https://doi.org/10.1093/AGEING/AFT010.
UNPD. (2022). “World Population Prospects.” Department of Economic and Social Affairs, United Nations Population Division. 2022. https://population.un.org/wpp/.
Walston, J., Buta, K. B. R. B., Bergman, H., Gill, T. M., Morley, J. E., Fried, L. P. (2019). “Moving Frailty Toward Clinical Practice: NIA Intramural Frailty Science Symposium Summary.” Journal of the American Geriatrics Society 67 (8): 1559–64. https://doi.org/10.1111/JGS.15928.
Wang, J. (2021). and Claire Hulme. “Frailty and Socioeconomic Status: A Systematic Review.” Journal of Public Health Research 10 (3): 2036. https://doi.org/10.4081/JPHR.2021.2036.
Wilker, E. H., Osman, M., & Weisskopf, M. G. (2023). Ambient air Pollution and Clinical Dementia: Systematic review and Meta-analysis. Bmj, 381(April), e071620. https://doi.org/10.1136/BMJ-2022-071620.
Zimmer, Z., Saito, Y., Theou, O., & Haviva, C., and Kenneth Rockwood (2021). Education, Wealth, and duration of Life Expected in various degrees of Frailty. European Journal of Ageing, 18(3), 393. https://doi.org/10.1007/S10433-020-00587-2.
Acknowledgements
AA and DEB were supported by the U.S. National Institute on Aging (5R01AG042778). BS was supported by the Innovations in Positive Health pilot grant from the Lee Kum Sheung Center for Health and Happiness at the Harvard T.H. Chan School of Public Health and the USC/UCLA Center on Biodemography and Population Health through a grant from the National Institute on Aging (P30AG017265). This publication does not represent the views of the Department of Veterans Affairs or the U.S. Government.
Author information
Authors and Affiliations
Corresponding authors
Additional information
Publisher’s Note
Springer Nature remains neutral with regard to jurisdictional claims in published maps and institutional affiliations.
Electronic supplementary material
Rights and permissions
Open Access This article is licensed under a Creative Commons Attribution 4.0 International License, which permits use, sharing, adaptation, distribution and reproduction in any medium or format, as long as you give appropriate credit to the original author(s) and the source, provide a link to the Creative Commons licence, and indicate if changes were made. The images or other third party material in this article are included in the article’s Creative Commons licence, unless indicated otherwise in a credit line to the material. If material is not included in the article’s Creative Commons licence and your intended use is not permitted by statutory regulation or exceeds the permitted use, you will need to obtain permission directly from the copyright holder. To view a copy of this licence, visit http://creativecommons.org/licenses/by/4.0/.
About this article
Cite this article
Seligman, B., Agarwal, A. & Bloom, D.E. Frailty Among Older Indians: State-Level Factors. Population Ageing 17, 149–163 (2024). https://doi.org/10.1007/s12062-023-09433-6
Received:
Accepted:
Published:
Issue Date:
DOI: https://doi.org/10.1007/s12062-023-09433-6