Abstract
Data on the burden of disease in the last years of life are an important basis for health policy decisions and the allocation of health care resources. Since dementia is one of the most expensive diseases, we ask the question whether dementia will ever be the most common disease at the time of death in older people? While international cause-of-death statistics report the underlying cause of death, dementia patients generally die from complications or sequelae. Instead of using causes of death, we identified the five most prevalent disease categories at age 70 and older at the time of death using German health claims data from 2004 to 2007 and 2014–2017, and combined their prevalence rates with the estimated number of deaths at age 70 and older up to the year 2060. We developed two scenarios, first, to represent the impact of population aging and increasing life expectancy. Second, to additionally examine the impact of morbidity trends among those who died. We found that dementia was already the most prevalent disease at the time of death among German women aged 70 years and older in 2014–2017, while it was still in fifth place among German men. Population aging and increasing life expectancy will result in dementia ranking first among women and second among men if the morbidity profile at the time of death remains constant. Extrapolating the observed time trends into the projections, cancer will be the most prevalent disease at the time of death for both sexes. Dementia will be second for women, and third for men after IHD. In addition to projections of causes of death, we also need projections of diseases at the time of death to better prepare for the needs of people in their final stages of life.
Similar content being viewed by others
Avoid common mistakes on your manuscript.
Introduction
Will dementia ever be the most prevalent disease at the time of death in the elderly? Dementia is one of the most expensive diseases (El-Hayek et al. 2019), and the care of people with dementia involves a considerable (in)formal care burden. As the disease progresses, people with dementia become increasingly dependent on support from others, and at some point, admission to a costly long-term care facility often becomes inevitable. Studies estimate that the average time from diagnosis to institutionalization is about 4 years(Joling et al. 2020) and survival is up to 5 years or more (Joling et al. 2020; Rait et al. 2010). Therefore, it is of utmost importance for society as well as for families and dementia patients that the health burden of dementia is adequately reflected in statistics. In 1993, Lilienfeld and colleague wrote an article projecting mortality from neurodegenerative diseases in the United States by the year 2040 (Lilienfeld and Perl 1993), and concluded that the number of deaths from neurodegenerative diseases would have to increase five- to sixfold from 1985 to 1988 levels to replace cancer as the second leading cause of death. They believed such an increase was possible, and the article, although not directly cited, found its way into the World Health Organization’s (WHO) Neurology Atlas 2004 (WHO 2004a). When we talk about the morbidity profile at the time of death as opposed to the causes of death, we need to think about the definition of causes of death and the relationship between dementia and death. In what follows, we will first discuss international cause-of-death statistics and examine literature whether, from a physiological point of view, dementia can lead to death. We will then extrapolate the morbidity profile of decedents. In doing so, we will explore the question of whether and when dementia might become the most common disease at the time of death.
Cause of death
When dementia is discussed as a cause of death, the question often arises as to whether it is possible to die from dementia, particularly Alzheimer’s disease, the most common neurodegenerative form of dementia (Winblad et al. 2016). According to the WHO definition (WHO 2004b) a distinction can be made between the immediate cause of death, antecedent causes and in particular the underlying cause of death, and the contributory causes of death (Eurostat 2021; WHO 2004b). The immediate cause of death is the “final disease, injury, or complication directly causing the death”, the underlying cause of death is defined as “ the disease or injury that initiated the train of morbid events leading directly to death or the circumstances of the accident or violence that produced the injury.”, and the contributory cause of death is defined as “any cause of death that is neither the immediate, intervening, originating antecedent nor underlying cause; hence these are other significant conditions that contributed to the fatal outcome, but were not related to the disease or condition directly causing death.“ WHO has proposed an international medical death certificate form that is the basis for reporting in national statistical offices. This form consists of two parts. In the first part, the physician notes the disease or condition that directly led to death and the antecedent causes. In the second part, other important circumstances contributing to death but unrelated to the disease or condition leading to death are noted. National and international tables use the underlying cause of death, commonly referred to as cause of death and death from disease. The contributing cause of death from the second part, if given at all, is usually referred to as death with disease.
Selected international rankings of dementia and Alzheimer’s disease based on the underlying cause of death
In its factsheet on the top 10 causes of death, the WHO reported that in 2019, Alzheimer’s disease and dementia ranked seventh among causes of death worldwide while ischaemic heart disease (IHD) remained the leading cause of death. In lower-middle-income countries Alzheimer’s disease and dementia did not rank among the top 10, in upper-middle-income countries they ranked eights, and in high-income countries, second (WHO 2021). In 2016, it ranked third in Europe (WHO 2018).
However, the ranking of dementia in high-income country reports varies widely, largely due to differences in coding practices and definitions, as shown in the three selected examples from England and Wales, Germany, and the United States. In 2019, the Office for National Statistics reported “dementia and Alzheimer’s disease” as the leading cause of death for England and Wales (Office for National Statistics 2020), ranked first for women and second for men (after IHD). In the same year, in Germany, the broad category of “dementia” ranked fifth (Destatis 2017) and the National Vitals Statistics Report (Heron 2021) reported “Alzheimer’s disease” as the sixth leading cause of death in the United States, ranking seventh in men and fourth in women.
Cause of death coding practices
Complex procedures, general principles, and classification rules are established by WHO (WHO 1979) for the selection of the underlying cause of death for the death statistic. In Germany, this selection is made by the 16 statistical offices of the “Länder”(Schelhase and Weber 2007). Thus, the resulting ranking of causes of death depends on the implementation of the WHO guidelines for determining the underlying cause of death by the statistical offices, and on the coding practices of physicians who complete the death certificate according to their clinical judgment. These coding practices may vary from country to country and may change over time.
Despite WHO guidelines, cause-of-death statistics are notoriously difficult to compare between countries and over time. This is even more true for dementia where death is not directly caused by the dementia, as may be the case, for example, with a heart attack. There is no linear mode of death (Küppers et al. 2021) where the underlying disease and the cause of death are assumed to be in the same organ system, resulting in a direct, clearly traceable causal chain, e.g., myocardial infarction in coronary heart disease. Dementia patients usually die from complications or sequelae where various underlying conditions unite on one final path (Küppers et al. 2021). This converging, nonlinear mode of death is also reflected in the quality of death certificates. Studies examining the frequency with which clinically diagnosed dementia was recorded on death certificates found severe underreporting: In South London, only 54% of dementia cases were reported on death certificates (Perera et al. 2016) and 45% in the United Kingdom (Gao et al. 2018).
Aim of the study
We estimated the number of deaths with one of the top five diseases, and projected them to the year 2060, examining the likelihood that, by 2060, dementia will rank first. We do not strive to identify the single underlying disease that charted the chain of diseases that led to death, but rather identified all diseases present at the time of death. In our projections we asked two questions: first, whether population aging combined with increasing life expectancy will inevitably lead to dementia being the number one disease at the time of death. And second, what happens if we include recent trends in pre-death morbidity in our projections.
Data & Methods
Population and data sources
For the base year 2015, we used population counts by sex and five-year age groups from the 13. coordinated population projection, variant G1-L2-W2, of the German Federal Statistical Office, which assumes a life expectancy at birth of 86.7 years for men and 90.4 years for women by the year 2060 (Destatis 2015). Sex specific death rates by five-year age groups and five-year period came from the Human Mortality Database (humanmortality.org) with a life expectancy of 78.13 years for men, and 82.98 years for women in 2015. We used claims data from Germany’s largest statutory health insurer, the Allgemeine Ortskrankenkassen (AOK), which insures about 30% of the German population and 50% at the highest age. In Germany, health insurance is mandatory and provided by two different systems: statutory health insurance which covers about 90% of the population in 105 different insurance funds, and private health insurance which covers the rest. Only self-employed persons, civil servants and all employees with a salary above the compulsory insurance limit of 62,550 euros per year are eligible for private health insurance. Thus, the AOK population has in general a lower socioeconomic status than the total German population. The data owner “Wissenschaftliches Institut der Ortskrankenkassen” (WidO), which is the research institute of the AOK, provided two mutually exclusive age-stratified random samples of 250,000 individuals aged 50 and older (2% of the AOK population). The first was drawn in 2004 and followed up through 2007; the second was drawn in 2014 and followed up through 2017. The quarterly data included inpatient and outpatient diagnoses and treatments for all insured individuals both living in community-dwellings and nursing homes. Claims data contain date of death but do not have information about the cause of death as recorded on the death certificate. Because our focus is on old age, we included all deaths aged 70 years and older for decedents who had been followed for at least eight quarters at the time of death. We used the last eight quarters because, independent of age, proximity to death significantly drives up health care utilization and spending (Felder 2008), with the last eight quarters being particularly expensive (Zweifel et al. 1999). This increased health care utilization is associated with a high likelihood of diagnosing both acute and chronic disease. This resulted in 11,738 deaths for men and 17,878 for women (Table 1).
Definition of morbidity at the time of death
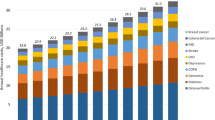
We determined the prevalence of the top five disease groups among those who had died and applied, with the exception of cancer, the WHO categorization (WHO 2018). We used all cancers instead of the WHO group “tracheal, bronchial, and lung cancers” to reconcile our results with Lilienfeld and Perl (Lilienfeld and Perl 1993). Diagnoses are based on ICD-10 classification and we differentiated between the first five major disease categories that were reported as leading causes of death in high income countries (WHO 2021): ischaemic heart disease (IHD: I20-I25), cerebrovascular disease including stroke (CerVD: I60-I69), Alzheimer’s disease and other dementias (Dementia: F01-F03, G30-G31), chronic obstructive pulmonary disease (COPD: J40-J47), and cancer (Cancer: C00-D49). In both time periods, the top five diseases cover 100% of deaths. For each period z (z 1 = 2004–2007, z 2 = 2014–2017) and disease group i, we calculated the age x and sex j specific prevalence \({F}_{xij}^{z}\) and their variances \({\sigma }_{xij}^{z 2}\) in the quarter of death (Fig. 1). We used the prevalence estimates from the second period, 2014–2017, as the starting point for our projections. In each period, the total sum of disease prevalence is always greater than 100% because more than one disease may be present at the time of death.
Projections
Population projections until 2060
Using the population projection tool “PDE Population Module Software”(IIASA 1994) we calculated P t xj which is the number of individuals aged 70 and above by sex j and five- year age groups (x = 70–74,75–79,80–84,85–89,90+), and for year t measured in five-year time steps until 2060. We interpolated the age-specific death rates in five-year steps arriving at the target life expectancies (LE) of 86.7 years for men, and 90.4 years for women in 2060. Since we are only interested in the age group 70 and older in our population projections, we have not taken fertility into account. Since the average age of immigrants is about 23 years (Destatis 2022), we have not considered migration either.
Projection of the number of deaths until 2060
To generate the expected number of deaths D t xj for age group x, sex j, and year t we transformed the interpolated death rates m t xj into death probabilities q t xj (Chiang 1984) and applied them to the projected population counts.
Projection of the morbidity profile at the time of death until 2060
The constant scenario assumes that the 2014–2017 prevalence rates remain constant: \({F}_{xij}^{t}\) =\({F}_{xij}^{2014/17}\) until 2060. The trend scenario assumes that the 2014 to 2017 prevalence rates change according to ratio observed between the two periods within the interval [0,1]: \({F}_{xij}^{t}\)= \({F}_{xij}^{2014/17}\) \(*{\left(\right(F}_{xij}^{2014/17}\)/ \({\left(\right(F}_{xij}^{2004/07}\))/10)n, with n = 5,10,15, …., 40 the step width of the projection. To measure the statistical uncertainty of the morbidity component we assume that the future prevalence of disease follows a random walk with the variance \({\sigma }_{xij}^{2 t}\) increasing by the square root of the projection step. For each projection year t and disease group i we drew five multivariate normally distributed random variables with means \({F}_{xij}^{t}\) and variance \({\sigma }_{xij}^{2 t}\) which were correlated for each age x by the correlation matrix C. C was observed by calculating the yearly age-specific correlations between the five disease groups over the period 2014–2017. We ran 2000 replications for each age group and combined the resulting proportions with the death projections. We used the median and the 10% and 90% quantiles to assess the individual projections and their uncertainties in terms of 80% prediction bands.
Results
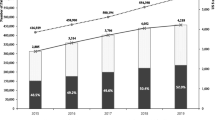
Population projections and number of deaths until 2060 (Fig. 2)
Our projections indicate that the population aged 70 and older will increase from about 13 million to 19.6 million by 2060, with the share of women declining from 58% to 2015 to 53%. Behind this general pattern is the aging wave of baby boomers born between the mid-1950s and mid-1960s, as shown in Fig. 2a. This aging wave will result in an ever-increasing proportion of people aged 85 and older. Our projections suggest that with female life expectancy at 90.4 years by 2060, mortality probabilities will fall between 30 and 40% of their 2015-levels in ages 70–75 (2015 = 0.0150; 2060 = 0.0058), and to 30% in ages 95+ (2015 = 0.2981; 2060 = 0.0975) (Fig. 2b). For men, a life expectancy of 86.7 years by 2060 was modelled, implying a decline to levels of about 28% (ages 70–75: 2015 = 0.0282; 2060 = 0.0081) to 38% (ages 95+: 0.3333; 2060 = 0.1262). For women, such a scenario results in a decline in the number of deaths starting in 2030, with 3.9 million deaths in 2015 and 2.8 million by 2060 (Fig. 2c). The number of deaths (Fig. 2c) will decrease in the under-80 age group and increase in the over-90 age group. Among men, the number of deaths will continue to increase from 3.2 million in 2015 to 3.4 million in 2040 and then decline to 2.6 million in 2060. The age-specific trends will be similar to those for women.
Projection of the number of population (in 1000), death probabilities and the number of deaths (in 1000) for German women 2015/2020 to 2055/2060. Base population 2015: 13th coordinated population projection, variant G1-L1-W2 High, 31.12.2015, Statistisches Bundesamt (Destatis), 2018; LE 2060: men: 86.7 years; women: 90.4 years
Morbidity profile at the time of death
In 2004–2007 (Table 2), IHD was the most common disease at the time of death in all age groups over 70 years and in both sexes (men: 58.3%; women: 54.4%). In women, dementia was second (52.1%), and in men, COPD (46.1%). In men, dementia ranked fifth (36.5%). This sex difference is partly explained by differences in life expectancy. In men aged 85–89 years, dementia ranked third (48.8%), and in those aged 90 years and older, it ranked first (64.9%). For women, dementia always ranked first in these age groups (85–89 years: 59%; 90 + years: 68.8%).
In 2014–2017 (Table 2), for all age groups over 70 years, IHD still ranked first in men (54%) but second in women (44.3%), whereas dementia already ranked first (55%) and was always the most common disease at the time of death from age 80 years onwards.
Time trends indicate that the prevalence of IHD at the time of death decreased in both sexes, whereas the prevalence of CerVD remained unchanged in men (about 44% in both periods) and decreased in women (from 47.9 to 41.7%). The prevalence of dementia increased, with a greater increase in men (from 36.5 to 41.7%) than in women (from 52.1 to 55.0%). COPD decreased in men (from 46.1 to 30.7%) and increased in women (from 30.7 to 32.3%), and cancers increased in both sexes (men: from 42.2 to 45.0%; women from 29.2 to 32.4%).
Projection of the morbidity profile at the time of death until 2060
Constant Scenario.
In this scenario, since future trends in morbidity at the time of death remain on constant levels, any change in the relative disease frequencies for all ages combined is solely due to increases in life expectancy and the ageing of large cohorts such as the baby-boomers born between mid-1950s and mid-1960s and the World War II cohorts born between mid-1930s and mid-1940s. By 2060, among men IHD will still be the first ranking disease (Fig. 3; Table 3). Dementia, however, will rank second, followed by CerVD, cancer and COPD. While the statistical prediction band places IHD safely in first place for most of the period, it overlaps with that of dementia in 2060. Among women, dementia has already occupied rank one in 2014–2017, and will continue to do so by 2060. IHD will rank second, followed by CerVD, COPD and cancer.
Trend scenario.
The results change significantly when we consider morbidity trends at the time of death. This change is largely due to cancer. Among men, cancer will already rank first in 2030 and will continue to do so in 2060. All other diseases shift down one rank, i.e., IHD will be second, dementia third, CerVD fourth, and COPD fifth. Looking at the confidence bands (Fig. 4), the leading role of cancer is confirmed from around 2035, with all other confidence bands overlapping throughout the projection period. Among women, dementia will continue to lead (Table 3), but cancer will begin to overtake dementia around 2050 (Fig. 4).
Discussion
In 2014–2017, dementia was already the most prevalent disease at the time of death among German women aged 70 years and older, while it was still in fifth place among German men. Our projections for 2060 show that population aging and increasing life expectancy will result in dementia remaining first among women and taking second place among men if the morbidity profile at the time of death remains constant. If we extrapolate recent time trends in the prevalence of diseases at the time of death into the projections, cancer will be the most prevalent disease for both sexes, and dementia will be second for women; for men, it will be third after IHD. We came to this conclusion by analysing claims data of the largest German public health insurer which we combined with population forecasts to project the number of deaths. Different to cause-of-death statistics reported by the WHO and individual countries, we do not strive to identify the single underlying disease that charted the chain of diseases that led to death, but rather identified all diseases present in the quarter of death. In official statistics, cause-specific mortality statistics are presented using country-specific groupings of causes of death, which makes cross-country comparison difficult. For better comparison, we used the WHO grouping, but we have replaced lung cancer with all cancers.
Several diseases have either become less frequent or less lethal over time, or both. The Global Burden of Disease Study reported (Morovatdar et al. 2021), that the global age-standardized incidence rates of IHD, stroke, and dementia decreased with even sharper downward trends in the OECD countries. For IHD the relative change was greater for mortality than for incidence and the largest decreases in incidence and mortality occurred between 1990 and 2009 with a much slower decrease thereafter (Vancheri et al. 2021).
In terms of dementia prevalence and incidence most recent studies have observed declining trends (for a review see e.g. (Wu et al. 2017; Gao et al. 2019)). In our previous research based on claims data we showed that this was also true for dementia prevalence (Doblhammer et al. 2015a) and incidence (Doblhammer et al. 2015b) in Germany. In the latter study we concluded that dementia incidence was shifted into higher ages, rather than that there was a general decrease of dementia incidence. In the current study we do not observe a decline in the prevalence of dementia in the two years before death which supports our earlier conclusion of an age-delay rather than a decline in the incidence. This is supported by the finding that in Denmark over a 20-year period, the excess mortality of patients with dementia as compared those without dementia did not change. Whereas the excess mortality gap for acute IHD and cancer declined significantly (Taudorf et al. 2021). Thus, acute IHD and cancer have become less lethal over time, which was not the case for dementia.
The current and future difference in disease ranking between sexes may largely reflect sex-specific cohort patterns in smoking (Westphal and Doblhammer 2012). In Germany, male cohorts born between 1926 and 1956 had declining ever-smoking prevalence among the high educated, and stable prevalence among the low educated while among those born after 1956, prevalence declined in both educational groups. On the contrary, highly educated women born between 1920 and 1930 were the first to take up smoking, and among those born between 1931 and 1950 the less educated women approached the ever smoking levels of their higher educated counterparts. This cohort pattern is reflected in this study in the higher prevalence of COPD at the time of death among men, while it is of less importance among women. In Europe, COPD mortality rates have been declining among males in most countries, while, among females, COPD mortality rates have been increasing in half of the studied countries (Lortet-Tieulent et al. 2019). Again, this is reflected in our data with COPD prevalence declining among men, but increasing among women for the two periods.
In our trend scenario, we find that cancer could be the most common disease at the time of death by 2060. The sharp increase is mainly due to increasing prevalence rates for lung, breast, and pancreatic cancers in women, and to prostate, pancreatic, and, to a lesser extent, lung cancers in men. This increase in prevalence can be explained by both the rising incidence of certain cancers and the decline in mortality from many cancers. Patients survive longer after the initial cancer diagnosis and eventually die from another disease. However, since cancer is considered a chronic disease in our projections, a cancer diagnosis in the last two years before death automatically means that cancer was present at the time of death. In 2018, the most common cancer sites in Europe were cancers of the female breast, followed by colorectal, lung and prostate cancer. These four cancers represent half of the overall burden of cancer in Europe. With 1.93 million deaths, the most common causes of death from cancer were cancers of the lung, colorectal, breast and pancreatic cancer(Ferlay et al. 2018). Survival trends after cancer incidence are generally increasing, even for some of the more lethal cancers such as cancers of the liver, pancreas, and lung. In Germany, the age-standardized five-year relative survival in breast cancer increased strongly between 1979 and 1983 and 2013–2015(Jansen et al. 2020) and in the United States population-level mortality from non–small-cell lung cancer fell sharply from 2013 to 2016, and survival after diagnosis improved substantially (Howlader et al. 2020). PSA testing and mammographic screening, and increasing use of colonscopy and faecal blood testing together with improving cancer care are probably the major underlying reasons (Verdecchia et al. 2009). Whether past trends can be extrapolated into the future needs to be examined in light of future changes in lifestyle, medical treatments and other risk or health factors.
Limitations
There are a number of limitations in our study arising from the model assumptions and data used. When we extrapolate past disease trends into the future, we neglect potential changes in behavioral, environmental, occupational, and metabolic risk factors that are not captured by our data (Jeffrey D Stanaway et al. 2018). The ability to explain changes in mortality from changes in these risk factors varies substantially by disease and age. However, environmental, occupational, and behavioral risks have generally led to decreases in disability-adjusted life years (DALYs), while metabolic risk factors have led to increases (Jeffrey D Stanaway et al. 2018).
Medical claims data have limitations that should be kept in mind when interpreting the results of our projections. The primary aims of medical claims data are cost calculation and reimbursement. In the German medical system, only diagnoses leading to treatment are relevant for the purposes of cost calculation. Thus, a patient’s cognitive impairment may not be documented if no further treatment is given. This might be particularly true for mild cases of dementia and cognitive impairment. Since this would result in an underdiagnoses of dementia, we previously compared dementia prevalence and incidence from our data with figures reported in other studies (Doblhammer et al. 2015a; Doblhammer et al. 2015b). Our results fit very well with these other studies, which can be explained by the fact that our data include information on objectively measured need for long-term care according to the German statutory long-term care insurance system. In this system, an objective assessment of support needs based on physical and cognitive limitations is made and documented. Linkage studies have shown that dementia diagnoses appear in secondary health data with a time lag, as compared to population-based surveys (Chen et al. 2019; Rizzuto et al. 2018). Thus, although the first dementia diagnosis may be delayed compared with the onset of the disease, severe dementia is not expected to be severely underrepresented at the time of death.
In general, diagnoses may be less accurate in the oldest age groups because a large proportion of people with physical and cognitive impairments live in nursing homes (Jakob et al. 2002). However, this inaccuracy may not be limited to dementia. The possible lack of accuracy also explains why we limited our final age group to 90 years and older, even though a large proportion of deaths occur in this age group.
Temporal trends in medical claims data may be subject to a number of confounding factors that are independent of changes in health. Benefit data are affected not only by regulatory changes and changes in costing software, but also by physician knowledge, and the range of treatment options. In addition, patients may have become more aware of certain diseases and seek diagnosis more frequently or earlier.
Since the option of treatment is a necessary condition for the inclusion of a diagnoses in claims data, the diseases leading to sudden deaths occurring out-of-hospital are not included in the data. For example, cardiac events, the most common causes of out-of-hospital cardiac arrests, have a survival rate of less than 14% (Gässler et al. 2019), and the information about the cardiac event will be missing, if death occurred before medical help was present. These events, however, are rare and do not bias our results.
The socio-economic status of the AOK population is lower than that of the general population (Geyer and Peter 2000), however, this difference is larger among younger than older people. This is reflected in the comparison of death rates between the AOK and the German population aged 50 years and older, which indicates only marginal differences, as shown in Nerius et al. (2017). In addition, any over- or underestimation of disease in the AOK population might affect the prevalence of disease to a larger extent than the rank of the disease since all major disease categories used in this study are subject to large socioeconomic gradients.
Conclusions
Our study showed that the 1993-prognosis of Lilienfeld and colleague for the year 2040 has already come true at the beginning of the 21st century. Among elderly German women dementia has outranked cancer at the time of death by far and with population aging and increasing life expectancy this might also be the case for men. However, when factoring in recent trends in morbidity at the time of death, then death with cancer will rank first among both sexes by the mid of the century. But even under this scenario, dementia will be the second most frequent disease at the time of death and a major public health challenge in terms of care need and care provision in the coming decades.
Death certificates and the resulting cause-of-death statistics are an important basis for health policy decisions and allocation of health care resources (Küppers et al. 2021). However, they do not adequately reflect the burden of disease in the last years of life. A dementia prevalence of up to 70% among the deceased in the oldest age groups (Doblhammer and Barth 2018) and the aging of large cohorts along with increasing life expectancy makes more detailed studies of the disease burden before death ever more urgent. Therefore, we argue, that in addition to cause of death projections we also need projections of the diseases at the time of death to better prepare for the need of individuals in their final phase of their lives.
Acknowledgements:
References
Chen, Y., Tysinger, B., Crimmins, E., & Zissimopoulos, J. M. (2019). Analysis of dementia in the US population using Medicare claims: insights from linked survey and administrative claims data. Alzheimer’s & Dementia: Translational Research & Clinical Interventions, 5, 197–207
Chiang, C. L. (1984). The Life Table and Its Applications. R.E. Krieger Publishing Company
Destatis (2015). Bevölkerung Deutschlands bis 2060: 13. koordinierte Bevölkerungsvorausberechnung. Federal Statistical Office of Germany. https://www.destatis.de/DE/Themen/Gesellschaft-Umwelt/Bevoelkerung/Bevoelkerungsvorausberechnung/Publikationen/Downloads-Vorausberechnung/bevoelkerung-deutschland-2060-presse-5124204159004.pdf?__blob=publicationFile#:~:text=Bev%C3%B6lkerungsvorausberechnungen%20ihre%20G%C3%BCltigkeit.-,Die%2013.,Varianten%20der%20zuk%C3%BCnftigen%20Entwicklung%20ergeben. Accessed 23 February 2022
Destatis (2017). Gesundheit: Todesursachen in Deutschland. 2015. Federal Statistical Office of Germany. https://www.destatis.de/DE/Themen/Gesellschaft-Umwelt/Gesundheit/Todesursachen/Publikationen/Downloads-Todesursachen/todesursachen-2120400157004.pdf?__blob=publicationFile. Accessed 23 February 2022
Destatis (2022). Zugewanderte Bevölkerung in Privathaushalten nach Einreisealter und Aufenthaltsdauer 2020. Federal Statistical Office of Germany. https://www.destatis.de/DE/Themen/Gesellschaft-Umwelt/Bevoelkerung/Migration-Integration/Tabellen/migrationshintergrund-zugewanderte-privathaushalte.html. Accessed 23 February 2022
Doblhammer, G., & Barth, A. (2018). Prevalence of morbidity at extreme old age in Germany: An observational study using health claims data. Journal of the American Geriatrics Society, 66(7), 1262–1268
Doblhammer, G., Fink, A., & Fritze, T. (2015a). Short-term trends in dementia prevalence in Germany between the years 2007 and 2009. Alzheimer’s & Dementia, 11(3), 291–299
Doblhammer, G., Fink, A., Zylla, S., & Willekens, F. (2015b). Compression or expansion of dementia in Germany? An observational study of short-term trends in incidence and death rates of dementia between 2006/07 and 2009/10 based on German health insurance data. Alzheimer’s research & therapy, 7(1), 1–11
El-Hayek, Y. H., Wiley, R. E., Khoury, C. P., Daya, R. P., Ballard, C., Evans, A. R., et al. (2019). Tip of the iceberg: assessing the global socioeconomic costs of Alzheimer’s disease and related dementias and strategic implications for stakeholders. Journal of Alzheimer’s Disease, 70(2), 323–341
Eurostat (2021). Glossary: Cause of death. Statistics Explained. Eurostat. https://ec.europa.eu/eurostat/statistics-explained/index.php?title=Glossary:Cause_of_death. Accessed 13 October 2021
Felder, S. (2008). Im Alter krank und teuer?-Gesundheitsausgaben am Lebensende.G + G Wissenschaft(4),23–30
Ferlay, J., Colombet, M., Soerjomataram, I., Dyba, T., Randi, G., Bettio, M., et al. (2018). Cancer incidence and mortality patterns in Europe: Estimates for 40 countries and 25 major cancers in 2018. European journal of cancer, 103, 356–387
Gao, L., Calloway, R., Zhao, E., Brayne, C., Matthews, F. E., & Medical Research Council Cognitive Function and Ageing Collaboration. (2018). Accuracy of death certification of dementia in population-based samples of older people: analysis over time. Age and ageing, 47, 589–594. doi:https://doi.org/10.1093/ageing/afy068
Gao, S., Burney, H. N., Callahan, C. M., Purnell, C. E., & Hendrie, H. C. (2019). Incidence of dementia and Alzheimer disease over time: A meta-analysis. Journal of the American Geriatrics Society, 67(7), 1361–1369
Gässler, H., Fischer, M., Wnent, J., Seewald, S., & Helm, M. (2019). Outcome after pre-hospital cardiac arrest in accordance with underlying cause. Resuscitation, 138, 36–41
Geyer, S., & Peter, R. (2000). Income, occupational position, qualification and health inequalities—competing risks?(Comparing indicators of social status). Journal of Epidemiology & Community Health, 54(4), 299–305
Heron, M. P. (2021). Deaths: Leading causes for 2019: National Vital Statistics Reports. doi:https://doi.org/10.15620/cdc:107021
Howlader, N., Forjaz, G., Mooradian, M. J., Meza, R., Kong, C. Y., Cronin, K. A., et al. (2020). The effect of advances in lung-cancer treatment on population mortality. New England Journal of Medicine, 383(7), 640–649
IIASA. PDE Population Projection Software. World Population Program, International Institute for Applied Systems Analysis (IIASA). https://previous.iiasa.ac.at/web/home/research/researchPrograms/WorldPopulation/PublicationsMediaCoverage/Software/software.html. Accessed 23 February 2022
Jakob, A., Busse, A., Riedel-Heller, S. G., Pavlicek, M., & Angermeyer, M. C. (2002). Prävalenz und Inzidenz von Demenzerkrankungen in Alten-und Altenpflegeheimen im Vergleich mit Privathaushalten. Zeitschrift für Gerontologie und Geriatrie, 35(5), 474–481
Jansen, L., Holleczek, B., Kraywinkel, K., Weberpals, J., Schröder, C. C., Eberle, A., et al. (2020). Divergent Patterns and Trends in Breast Cancer Incidence, Mortality and Survival Among Older Women in Germany and the United States. Cancers, 12(9), 2419
Jeffrey, D., Stanaway, A., Afshin, E., Gakidou, S. S., Lim, D., Abate, K. H., Abate, et al. (2018). Global, regional, and national comparative risk assessment of 84 behavioural, environmental and occupational, and metabolic risks or clusters of risks for 195 countries and territories, 1990–2017: a systematic analysis for the Global Burden of Disease Study 2017. The Lancet, 392, 1923–1994. doi:https://doi.org/10.1016/S0140-6736(18)32225-6
Joling, K. J., Janssen, O., Francke, A. L., Verheij, R. A., Lissenberg-Witte, B. I., Visser, P. J., et al. (2020). Time from diagnosis to institutionalization and death in people with dementia. Alzheimer’s & Dementia, 16(4), 662–671
Küppers, L., Ritz-Timme, S., & Hartung, B. (2021). Died from or with dementia? The relationship between dementia and cause of death. Deutsche Medizinische Wochenschrift (1946), 146(10), 677–682
Lilienfeld, D. E., & Perl, D. P. (1993). Projected neurodegenerative disease mortality in the United States, 1990–2040. Neuroepidemiology, 12, 219–228. doi:https://doi.org/10.1159/000110320
Lortet-Tieulent, J., Soerjomataram, I., López-Campos, J. L., Ancochea, J., Coebergh, J. W., & Soriano, J. B. (2019). International trends in COPD mortality, 1995–2017.European Respiratory Journal, 54(6)
Morovatdar, N., Avan, A., Azarpazhooh, M. R., Di Napoli, M., Stranges, S., Kapral, M. K., et al. (2021). Secular trends of ischaemic heart disease, stroke, and dementia in high-income countries from 1990 to 2017: the Global Burden of Disease Study 2017. Neurological Sciences, 1–10
Nerius, M., Fink, A., & Doblhammer, G. (2017). Parkinson’s disease in Germany: prevalence and incidence based on health claims data. Acta Neurologica Scandinavica, 136(5), 386–392
Perera, G., Stewart, R., Higginson, I. J., & Sleeman, K. E. (2016). Reporting of clinically diagnosed dementia on death certificates: retrospective cohort study. Age and ageing, 45(5), 668–673
Rait, G., Walters, K., Bottomley, C., Petersen, I., Iliffe, S., & Nazareth, I. (2010). Survival of people with clinical diagnosis of dementia in primary care: cohort study. Bmj, 341
Rizzuto, D., Feldman, A. L., Karlsson, I. K., Aslan, D., Gatz, A. K., M., & Pedersen, N. L. (2018). Detection of dementia cases in two Swedish health registers: a validation study. Journal of Alzheimer’s Disease, 61(4), 1301–1310
Schelhase, T., & Weber, S. (2007). Mortality statistics in Germany. Problems and perspectives. Bundesgesundheitsblatt, Gesundheitsforschung, Gesundheitsschutz, 50(7), 969–976
Taudorf, L., Nørgaard, A., Waldemar, G., & Laursen, T. M. (2021). Mortality in dementia from 1996 to 2015: a national registry-based cohort study.Journal of Alzheimer’s Disease(Preprint),1–12
Vancheri, F., Tate, A. R., Henein, M., Backlund, L., Donfrancesco, C., Palmieri, L., et al. (2021). Time trends in ischaemic heart disease incidence and mortality over three decades (1990–2019) in 20 Western European countries: systematic analysis of the Global Burden of Disease Study 2019. European Journal of Preventive Cardiology
Verdecchia, A., Guzzinati, S., Francisci, S., de Angelis, R., Bray, F., Allemani, C., et al. (2009). Survival trends in European cancer patients diagnosed from 1988 to 1999. European journal of cancer, 45(6), 1042–1066
Westphal, C., & Doblhammer, G. (2012). The diffusion of smoking in East and West Germany: Smoking patterns by birth year. Population, 67(4), 653–670
WHO (1979). Medical certification of cause of death: instructions for physicians on use of international form of medical certificate of cause of death (4th ed.)
WHO. (2004a). Atlas - country resources for neurological disorders 2004: Results of a collaborative study of the World Health Organization and the World Federation of Neurology. Geneva: World Health Organization
WHO (2004b). The International Statistical Classification of Diseases and Health Related Problems: ICD-10: Volume 2: Instruction Manual (2nd ed.)
WHO. (2018). Global Health Estimates 2016: Deaths by Cause, Age, Sex, by Country and by Region, 2000–2016. World Health Organization. www.who.int/healthinfo/global_burden_disease/GHE2016_Deaths_WHOReg_2000_2016.xls?ua=1 Accessed 23 February 2022
WHO (2021). The top 10 causes of death. World Health Organization. https://www.who.int/news-room/fact-sheets/detail/the-top-10-causes-of-death
Winblad, B., Amouyel, P., Andrieu, S., Ballard, C., Brayne, C., Brodaty, H., et al. (2016). Defeating Alzheimer’s disease and other dementias: a priority for European science and society. The Lancet Neurology, 15(5), 455–532
Wu, Y. T., Beiser, A. S., Breteler, M. M. B., Fratiglioni, L., Helmer, C., Hendrie, H. C., et al. (2017). The changing prevalence and incidence of dementia over time—current evidence. Nature Reviews Neurology, 13(6), 327–339
Zweifel, P., Felder, S., & Meiers, M. (1999). Ageing of population and health care expenditure: a red herring? Health economics, 8(6), 485–496
Funding
No funding was received to assist with the preparation of this manuscript.
Open Access funding enabled and organized by Projekt DEAL.
Author information
Authors and Affiliations
Corresponding authors
Ethics declarations
Conflict of interest
The authors have no competing interests to declare that are relevant to the content of this article.
Conflict of interest
None.
Additional information
Publisher’s note
Springer Nature remains neutral with regard to jurisdictional claims in published maps and institutional affiliations.
Rights and permissions
Open Access This article is licensed under a Creative Commons Attribution 4.0 International License, which permits use, sharing, adaptation, distribution and reproduction in any medium or format, as long as you give appropriate credit to the original author(s) and the source, provide a link to the Creative Commons licence, and indicate if changes were made. The images or other third party material in this article are included in the article’s Creative Commons licence, unless indicated otherwise in a credit line to the material. If material is not included in the article’s Creative Commons licence and your intended use is not permitted by statutory regulation or exceeds the permitted use, you will need to obtain permission directly from the copyright holder. To view a copy of this licence, visit http://creativecommons.org/licenses/by/4.0/.
About this article
Cite this article
Doblhammer, G., Fritze, T., Reinke, C. et al. Can dementia become the most prevalent disease at the time of death in Germany? Projections up to the year 2060 for the five most important diseases at the time of death. Population Ageing 15, 523–540 (2022). https://doi.org/10.1007/s12062-022-09365-7
Received:
Revised:
Accepted:
Published:
Issue Date:
DOI: https://doi.org/10.1007/s12062-022-09365-7