Abstract
Scotland’s population has become increasingly ethnically diverse. The aim of this study was to better understand future changes to the ethnic profile of the population and the implications for population health. The literature regarding ethnicity and health, particularly in the Scottish context, was reviewed alongside analyses of past trends and new future projections (2011–2031) of the size of the non-White ethnic minority population in Scotland and Glasgow (Scotland’s largest and most ethnically diverse city). The literature emphasises that the relationships between ethnicity, socioeconomic position (SEP) and health are extremely complex. In Scotland this complexity is arguably enhanced, given the different, less disadvantaged, SEP profile of many ethnic minority groups compared with those in other countries. Although indicators of overall health status have been shown to be better among many non-White ethnic minority groups compared with the White Scottish population, such analyses mask varying risks of particular diseases among different groups. This complexity extends to understanding the underlying causes of these differences, including the ‘healthy migrant’ effect, ‘acculturation’, and the impact of different types and measures of SEP. The proportion of the population belonging to a non-White ethnic group increased four-fold in both Scotland and Glasgow between 1991 and 2011. New projections suggest that by 2031, around 20% of Glasgow’s total population (and 25% of children) will belong to a non-White minority group. Given this, there is a clear need for policy-makers and service-planners to seek to understand the implications of these changes to the Scottish population.
Similar content being viewed by others
Avoid common mistakes on your manuscript.
Introduction
Different ethnic population groups can often experience very different health outcomes, representing stark inequalities. The evidence for, and implications of, this are important to understand for the formulation of public health policy in all societies with ethnically diverse populations, and/or where the ethnic composition of the population is changing rapidly. Scotland, the focus of this paper, is one country that is experiencing such change. Across the country as a whole, but particularly in its largest city, Glasgow, there have been notable increases in the number of people identifying as belonging to an ethnic minority in recent years. The overall aim of this work, therefore, was to gain a better understanding of the changing ethnic profiles of Scotland and Glasgow, and their related population health implications.
The specific research questions were:
- 1.
What is known about the links between ethnicity and health (including their interactions with socioeconomic position, a key health determinant) (a) in high income countries; (b) in Scotland in particular?
- 2.
How have Scotland’s, and Glasgow’s, populations changed recently in relation to ethnic composition, and what are the likely future changes?
- 3.
What are the potential implications of these changes for future health status?
Methods
Defining Ethnicity and Ethnic Minorities
The concept of ethnicity is one that is contested, and which encompasses a broad range of factors including race (itself contested), culture (which is often itself associated with religious differences) and context-specific factors such as discrimination and stigma against minority populations. As such, ethnicity can mean different things to different audiences and has different implications (Aspinall 2011). In this paper, we use ethnic groups based on how individuals identify themselves in response to census questions.
The paper also employs a narrow definition of ‘ethnic minority’. Partly on account of the nature of some of the (Scottish-based) evidence found in the research literature, and also because of the available population projection data discussed later in the paper, this project has focused on the non-White ethnic minority population. In discussing the specific Scottish context, therefore, it does not consider (for example) the White Irish or White Polish population (both of whom accounted for significant proportions of the Scottish population in 2011Footnote 1), nor the White Gypsy/Traveller population, the numbers of whom are small (0.1% of Scottish population in 2011), but who are characterised by having a high prevalence of a number of particular health issues (Gordon et al. 2010; Scottish Government 2015).
Ethnicity, Health and Health Determinants: Reviewing the Evidence
There is considerable research evidence on the links between ethnicity and health status. However, the geographical context for that evidence is highly important. Notably, a lot of evidence for poorer health among particular ethnic minorities in developed countries has come from the USA, where minority groups are also more likely to live in poverty compared with the majority White population (Stronks and Kunst 2009; Krieger 2011). The same is also true of minority ethnic groups in England (Fitzpatrick et al. 2005; Scottish Government 2014; Darlington et al. 2015). However, since a different socioeconomic context applies in Scotland (Gordon et al. 2010; Scottish Government 2014), the review of the literature focused primarily (although not exclusively) on the Scottish context. The research was also limited primarily to studies which examined health-specific outcomes. There is a wealth of valuable Scottish research into ethnicity and other important topics such as housing (Netto 2012), homelessness (Netto et al. 2004), service provision (Simpson and Parsons 2016) and more, but these were not the principal focus of the study. Similarly, smaller, more qualitative, local studies were largely excluded.
The main source of health data for ethnic minorities was the Scottish Health and Ethnicity Linkage Study (SHELS) (Bhopal et al. 2011). Based on the linkage of data for the entire Scottish population recorded in the 2001 Census to routinely collected morbidity and mortality records, this study has been able to provide unique insights into the health profiles of ethnic groups living in Scotland. All published SHELS journal papers were examined. This was augmented by consulting various articles on ethnicity and health (including other work cited within those papers) from personal collections, supplemented by a search of literature databases for reviews of the subject.Footnote 2
The Changing Ethnic Profile of Glasgow and Scotland
Data from the census were examined for Scotland, Glasgow, and Glasgow’s neighbourhoodsFootnote 3 to examine change over time in the size of the population classed as belonging to a non-White ethnic minority groupFootnote 4 between 1991 and 2011.
Future projections of the size of ethnic minority population groups were obtained from data made available by the University of Leeds and partners (Wohland et al. n.d). Projections have been produced for different ethnic groups, by UK local authority, age and sex for the period 2011–2061. They were calculated by means of a complex set of modelling analyses using existing census data on population, internal migration and immigration, and linked estimates of mortality, fertility, and emigration. Two sets of projections were produced, one based on an additional assumption regarding the impact of ‘Brexit’ (the withdrawal of the United Kingdom from the European Union) on international migration – and it is this set of projections that have been used here. Although the data cover a 50 year period, we have – for reasons outlined later in the paper – limited our analyses to 2011–2031. Data were analysed for Scotland and Glasgow: the latter is the largest, and most ethnically diverse, city in Scotland.
Results 1: Ethnicity, Health and Health Determinants: Reviewing the Evidence
The evidence presented here is summarised within 4 sections: the socioeconomic profile of ethnic minority groups; understanding the associations between socioeconomic position, ethnicity and health; health outcomes; maternal, child health and behavioural factors.
Socioeconomic Profile of Ethnic Minority Groups
In most developed countries, ethnic minority groups tend to have a more disadvantaged socioeconomic profile, and thus among some populations (in particular, the USA) ethnic inequalities in health are to a large degree a reflection of socioeconomic inequalities in health (Stronks and Kunst 2009; Krieger 2011).
A different and more complex interaction between ethnicity and socio-economic position is evident in Scotland. Analysis of the 2011 Census by the Scottish Government (Scottish Government 2014) (reproduced in Fig. 1 below) shows that among minority groups, those describing themselves as Indian, Chinese and mixed/multiple ethnic group are more likely to live in the least deprived areas of Scotland. High proportions of those of ‘other’ (non-White) and ‘other Asian’ ethnic groups live in both the least and most deprived areas. The deprivation profile of the Pakistani group is more similar to that of the White population, but with higher numbers also living in ‘middle’ areas.Footnote 5 However, people describing themselves as African, Caribbean or Black are much more likely to be living in the most deprived areas. Further analysis comparing Scottish and English census data highlights the differences between the countries in terms of the percentages of the population living in the most deprived neighbourhoods,Footnote 6 particularly in relation to Indian, Pakistani, Bangladeshi and mixed/multiple origin groups (as illustrated in Fig. 2).
Percentage of each ethnic group in each Scottish Index of Multiple Deprivation (SIMD) decile, 2011 (source: Scottish Government 2014)
Percentage of each ethnic group living in the most deprived 10% of neighbourhoods (datazones in Scotland, LSOAs in England) of Scotland and England, 2011 (source: Scottish Government 2014)
These differences are potentially important, given that in Scotland as a whole in 2011, 23% of the minority non-White population identified themselves as Pakistani, 18% as Indian or Bangladeshi, and 9% as being of mixed/multiple race (Scotland's census 2011). The equivalent figures for Glasgow were 33%, 14% and 4% respectively. However, it is also notable that 17% of the Scottish ethnic minority population (21% in Glasgow) described themselves as African, Caribbean or Black – and much higher numbers of people from those groups live in the most deprived areas (and other census analyses have shown that they also have much higher unemployment rates than the White population) (Kelly and Ashe 2014). Other individual (as opposed to area-based) analyses have also shown that there are much higher percentages of AsiansFootnote 7 (compared with the White population) in social classes I and II (60% of male Asians compared with 30% of the White population; 47% compared with 28% for females) (Millard et al. 2015), and that there are higher percentages of the Indian and Black populations with high levels of educational attainment, and being in managerial/professional qualifications, compared with the White Scottish population (Fischbacher et al. 2014).
Understanding the Associations between Socioeconomic Position, Ethnicity and Health
As stated, much of the international evidence has emphasised the contribution of socioeconomic circumstances in explaining differences in health outcomes between particular ethnic groups. In one recent example from England, Mindell and colleagues showed that the higher levels of poor self-reported health among the vast majority of minority ethnic groups compared with the White population were entirely explained by differences in SEP (Mindell et al. 2014). However, other English studies were less conclusive (Harding and Maxwell 1997; Nazroo 1997), and in analyses for Scotland the role of SEP appears much more complex. Although a number of the early SHELSFootnote 8 papers either did not appear to explicitly control for SEP (or did not report those analyses: these included analyses in relation to all cancer and site-specific cancersFootnote 9 (Bhopal et al. 2012a), acute myocardial infarctionFootnote 10 (Fischbacher et al. 2007a) and life expectancy (Gruer et al. 2016)), later analyses did control for different measures, but results were varied and controlling for SEP often only slightly altered the higher or lower risks of particular disease categories for particular ethnic groups. For example, this was the case with: the lower risk (compared with the White Scottish population) of stroke among male and female Chinese (Bhopal et al. 2012b); the greater risk of chest pain (Bhopal et al. 2012c) and heart failure (Bhopal et al. 2012d) among Pakistani men; and differences between certain ethnic groups for particular psychiatric outcomes (Bansal et al. 2014a). However, in some cases controlling for SEP did have important effects. For example, adjustment increased, and made significant, the higher risk of: stroke among African men (Bhopal et al. 2012b); heart failure among Indian men (Bhopal et al. 2012d); and alcoholic liver disease among Indian men (Bhala et al. 2016).
From the wider literature – as well as specific Scottish evidence – it is clear that the choice, and indeed the meaning and interpretation, of specific indicators of SEP are important. In one of the SHELS analyses (which focused on cardiovascular disease), Fischbacher et al. confirmed that there were different relations between different indicators of SEP and particular ethnic groups (Fischbacher et al. 2014). The authors recommended preliminary exploratory analyses to determine what type of indicator was most appropriate for different analyses (advice that subsequent SHELS papers have followed). Other authors (e.g. Kelaher et al. 2008; Stronks and Kunst 2009) have made similar points regarding the multidimensional, complex nature of SEP, and the importance of selecting indicators that are the most appropriate for the analysis in question. This echoes comment by Davey Smith (Davey Smith et al. 2000; Davey Smith 2000), who suggested that although routinely available measures of SEP can be used (to an extent) for comparisons within the same ethnic groups, they cannot be used across different groups (“they are of little use for ‘controlling out’ the impact of socioeconomic differences when attempting to reveal a pure ‘ethnicity’ effect” (Davey Smith et al. 2000)). The author discusses a number of reasons why the relationship between SEP, ethnicity and health is so complex (these are summarised later in this paper), but suggests that the complexity is such that there is no simple solution: “the only productive way forward is through studies that recognize the contingency of the relations between socioeconomic position, ethnicity, and particular health outcomes”. To paraphrase the title of the review, when it comes to understanding the links between ethnicity and health, there is a need ‘to learn to live with complexity’ (Davey Smith 2000).
Health Outcomes
‘General’ Health
Overall measures of health such as life expectancy (Gruer et al. 2016)Footnote 11 and all-cause mortality (Millard et al. 2015)Footnote 12 have been shown to be better among non-White ethnic groups compared with the White Scottish population. However, it is notable that studies have also shown that lower all-cause mortality among many non-White groups compared with both White Scottish (Bhopal et al. submitted) and White English (Wallace 2016) has been observed among those born outside the UK, but not among those born in the UK, suggesting the potential influence of a ‘healthy migrant’ effect in comparisons of overall health status (Davey Smith et al. 2000; Razum 2008; Singh and Siahpush 2001). This, and other proposed explanations for differences in health status between ethnic groups, are discussed later in the paper. Overall better health has also been observed for most (but not allFootnote 13) minority groups in relation to self-assessed health (as recorded, for example, in the census (Gordon et al. 2010; Scottish Government 2015)), albeit that there are known difficulties in comparing self-reported health between different cultures which make interpretation even more difficult than other comparative analyses of ethnic health (Sen 2002; Jürges 2007; O'Reilly and Rosato 2010; Salomon et al. 2009; Bostan et al. 2014; Au and Johnston 2014; Layes et al. 2012). More complex findings emerged from recent analyses of acute hospital admission rates in Scotland (Knox et al. 2016). Based on records which now have ethnicity recorded at admission in almost 80% of cases, they showed a varied picture: compared with White Scottish, higher admission rates were observed for males and females of Pakistani origin, males classed as ‘other Asian’ and female Bangladeshis, but lower admission rates among males of Indian, Chinese and Caribbean/Black origin, and among females classed as Chinese or African. Admission rates were standardised by age, but not by any measure of SEP.
Cancer
Lower cancer incidence rates (i.e. for all types of cancer combinedFootnote 14) were observed for the majority of ethnic minority groups (Indian and Pakistani males and females, Other South Asian, African, and Chinese males) compared with the White Scottish population. There were also differences among groups in relation to specific cancers: for example, lower rates of lung cancer and colorectal cancer among male and female Pakistanis respectively; and also of breast cancer among the latter. Rates of prostate cancer were lower among Indian and Pakistani men. As stated earlier, the reported results of analyses were not adjusted for SEP (Bhopal et al. 2012a).
It is worth highlighting that other research has also highlighted relatively lower rates of breast cancer incidence among UK South Asian women – but also showed that rates were increasing towards the level of the UK White population (Winter et al. 1999; Ali et al. 2010).
Diseases of the Circulatory System
A number of circulatory system conditions have been the focus of recent analyses. For example, the SHELS study showed that a number of ethnic minority groups (e.g. Pakistani and Indian males and females, African origin femalesFootnote 15) exhibit a similar risk of stroke (cerebrovascular disease) to White Scots: this is unlike what has been observed elsewhere (e.g. England), partly reflecting the high prevalence rates among the White Scottish population. However, the risk was lower among male and female Chinese. These analyses adjusted for levels of educational attainment as one measure of SEP (Bhopal et al. 2012b).
In terms of heart disease, the evidence shows a consistently greater risk for males and females of Pakistani origin, and a lower risk for male and female Chinese. This has been shown in SHELS studies of chest pain (Bhopal et al. 2012c), angina (Bhopal et al. 2012c), heart failure (Bhopal et al. 2012d) and acute myocardial infarction (AMI) (Fischbacher et al. 2007a; Bansal et al. 2013).Footnote 16 Controlling for SEP did not impact greatly on these results. Similar results were shown in separate (non-SHELS) analyses of hospital admissions for coronary heart disease (CHD) (Knox et al. 2016). Higher risks of some forms of heart disease have also been shown for Indian males e.g. the above CHD hospital admissions analyses (Knox et al. 2016) as well as – once SEP was taken into account – heart failure (Bhopal et al. 2012d). Higher rates of CHD hospital admission were also noted for males and females of Bangladeshi origin.Footnote 17 The findings in relation to the greater risks associated with males and females of Pakistani origin are consistent with other studies (Douglas et al. 2016; Fischbacher et al. 2007b; Wild et al. 2007).
Diabetes
The SHELS study has not published incidence rates for diabetes for the whole Scottish population. However, a previous study based on the population of the NHS Tayside area suggested that the prevalence of diabetes was 3–4 times higher among South Asians than non-South Asians in the area (Fischbacher et al. 2009), which is consistent with the evidence from other populations (Gordon et al. 2010). Similarly, SHELS pilot analyses of primary care data for selected GP practices within NHS Board areas of Lothian and Greater Glasgow & Clyde showed prevalence rates (unadjusted for SEP) to be 2–3 times higher among males and females of Indian and Pakistani populations compared with White Scottish (Douglas et al. 2016).
Liver Disease, Alcoholic Liver Disease, and all Alcohol-Related Diseases
In contrast to most disease-specific analyses reported by SHELS, Chinese men and women were shown to be at much greater risk of all liver disease than the White Scottish population. A higher risk was also observed for females of Pakistani origin and ‘other’ South Asian men.
For alcoholic liver disease (ALD) and the broader category of alcohol-related diseases (ARD), Indian men were observed to be at considerably greater risk than White Scots (for example, 60% greater risk of hospitalisation or death from ALD). Men and, in particular, women of mixed origin were also at much greater risk of ARD than the White Scottish population. However, many other ethnic groups had lower risks of these conditions than White Scots, for example Pakistani men (ALD, ARD) and women (ARD), and Chinese men and women (ARD). All analyses adjusted for a measure of SEP (Bhala et al. 2016).
Respiratory Conditions
A fairly complex set of results emerged from SHELS analyses of various respiratory conditions. However, there were some consistent findings in terms of observed lower risks (compared with the White Scottish) for Chinese males and females, and higher risks for males and females of Pakistani origin, for respiratory disorders generally (Bhopal et al. 2015) and, more specifically, for asthma (Sheikh et al. 2016) and lower respiratory tract infections (which include pneumonia and influenza) (Simpson et al. 2015). In addition, a higher risk of chronic obstructive pulmonary disease (COPD) was shown for those of mixed background (males and females), while Indian men were shown to be at higher risk of asthma but lower risk of COPD. All analyses controlled for measures of SEP.
Mental Health Disorders
One SHELS study analysed psychological disorders based on admissions to psychiatric hospitals. No clear patterns by ethnic group emerged with the exception of notably lower risks of hospitalisation for Indian females and Chinese males and females, and a higher risk among females of African origin. These differences (compared with White Scots) persisted after adjustment for SEP (Bansal et al. 2014a).
Other research, however, has highlighted the fact that levels of unreported psychological distress are high among certain Asian communities, particularly so among women (Gordon et al. 2010). Within the UK, levels of self-harm are known to be higher among South Asian women (compared with White UK women) (Bhui et al. 2007), while it is also well known that racism can impact severely on mental wellbeing among minority groups (Gordon et al. 2010). Such discrimination is one of the facets of stigma faced by minority groups, and as such can be seen as a ‘fundamental cause’ of poor health and, therefore, health inequalities (Hatzenbuehler et al. 2013).
Gastrointestinal Diseases
Analyses examined a range of both lower (e.g. Crohn’s Disease, appendicitis) and upper (e.g. pancreatitis, oesophagitis) gastrointestinal diseases. No particularly clear patterns emerged across the different ethnic groups, and for many conditions risk of hospitalisation or death was similar to that of the White Scottish population (Bhopal et al. 2014; Cezard et al. 2016).
Summarising the Evidence
Evidence taken from seven of the aforementioned SHELS studies – those which focus on some of the more common disease categories – is summarised in Fig. 3. For each condition the Figure shows (separately for males (Fig. 3a) and females (Fig. 3b)) the calculated rate ratios, in comparison with White Scots, for each of the five largest non-White ethnic groups.
Age- and (in most cases) SEP-adjusted rate ratios (in comparison to White Scots) for seven specific diagnoses and five major non-White ethnic groups, males (Fig. 3a) and females (Fig. 3b), Scotland 2001–2008/2010 (note that the follow-up periods for the analyses were either 2001–2008 (cancer, stroke, AMI, heart failure, psychiatric disorders) or 2001–2010 (alcohol related diseases, respiratory disease)). With the exception of cancer, the ratios relate to the risk of either admission to hospital or death with the specified diagnosis/es; for cancer, it relates to a cancer registration or death. Rate ratios for cancer and psychiatric disorders are unadjusted for SEP; for all other conditions they are adjusted for different measures of SEP. ‘All cancer’ excludes non-melanoma skin cancer. AMI refers to acute myocardial infarction. (Source: derived from various SHELS publications)
Maternal, Child Health and Behavioural Factors
Although the focus of much of the research has been on morbidity- and mortality-related health outcomes, ethnicity research has also been undertaken into maternity-related and other general health behavioural factors. Clearly, such research must be examined within the context of the public health understanding of the extent to which such behavioural factors are influenced by broader social, economic and environmental aspects (Dahlgren and Whitehead 1993; Evans and Stoddart 1994; WHO Commission on Social Determinants of Health 2008; Marmot and Wilkinson 2003; Black et al. 1980; McCartney et al. 2013; Link and Phelan 2002; Scott et al. 2013).
A number of maternity-related characteristics were analysed in one set of SHELS analyses. These showed that compared with a number of ethnic minority groups, White Scottish first-time mothers tended to be younger, less likely to breastfeed and more likely to have smoked during pregnancy. However, mean birthweight of non-White minority ethnic mothers tended to be lower even after adjustment for a range of potential confounders. Most analyses controlled for measures of SEP (education and housing tenure), although smoking in pregnancy was an exception (Bansal et al. 2014).
The birthweight findings echo the results of other UK research which showed there was a greater likelihood of low birthweight among Indian, Bangladeshi and Pakistani babies compared with the White population (Kelly et al. 2009). (Other studies (e.g. Margetts et al. 2002) have highlighted the consistently lower birthweight among South Asians in the UK, which arguably makes comparisons with the White UK population problematic).
In terms of more general behavioural factors, Scottish national survey data have shown that those of Pakistani, Chinese and ‘other’ Asian origin are significantly less likely to smoke than the White population (Whybrow et al. 2012).Footnote 18 However, many minority groups are also less likely to take part in physical activity (Gordon et al. 2010; Fischbacher et al. 2004). Most non-White minority groups are characterised by lower levels of alcohol consumption (including higher rates of abstinence); however, there is also evidence that generational differences have emerged over time e.g. with increases in levels of frequent and heavy drinking among Indian women and Chinese men. It is also known that some groups (e.g. Sikh men) are at greater risk of alcohol harmFootnote 19 than the White population (Hurcombe et al. 2010) – findings confirmed by the SHELS research reported earlier (Bhala et al. 2016).
All these results are discussed further below.
Results 2: The Changing Ethnic Profile of Glasgow and Scotland
Past Trends
The size of the ethnic minority population in Scotland, and particularly in Glasgow, has increased considerably in the last two decades. Between 1991 and 2011 there was a near four-fold increase in the proportion of the total population resident in both the city and the country belonging to non-White ethnic group: from 1.3% to 4.0% in Scotland, and from 3.2% to 11.6% in Glasgow. The latter figure accounts for a total of just under 70,000 people. Although the national 2011 figure is small in proportionate terms, it still equates to more than 210,000 people.
It is worth noting that part of the increase in the size of the non-White ethnic minority population in Glasgow between 2001 and 2011 is likely to relate to the arrangement between Glasgow City Council and the UK government Home Office which has seen thousands of asylum seekers housed in the city from 2000 (Crawford et al. 2012). However, it was not possible to quantify the precise contribution of this group to the increase.
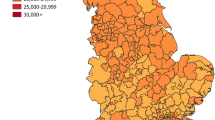
Across Glasgow’s neighbourhoods, the relative size of the ethnic minority population varies considerably. Figure 4 shows trends between 1991 and 2011 for four selected neighbourhoods in the cityFootnote 20 (alongside the comparative figures for Glasgow as a whole and Scotland). In part of Pollokshields East, for example, in 2011 over half the approximately 7000 population were from a non-White ethnic group. In a number of other areas ethnic minority groups account for over one third of the total population. Across all Glasgow’s neighbourhoods, the size of the non-White population in 2011 ranged from 2% (Springboig and Barlanark) to 56% (Pollokshields East). Previous analyses have shown that each of these neighbourhoods saw an increase in the size of the minority non-White population between 2001 and 2011 (Nixon 2016). Note that as contextual background, Fig. 4 also shows the location of the neighbourhoods in the city, as well as levels of area deprivation from the Scottish Index of Multiple Deprivation (SIMD) (SIMD 2016).
Percentage of total population from a non-White ethnic group: Scotland, Glasgow and four selected Glasgow neighbourhoods, 1991–2011, with map showing location of selected neighbourhoods alongside Scottish Index of Multiple Deprivation deciles (source: Census data; Scottish Index of Multiple Deprivation)
Previous analyses of census data (Understanding Glasgow, the Glasgow indicators project n.d) have shown that in Glasgow as a whole, the biggest increase in the size of different ethnic minority groups between 2001 and 2011 was – in proportionate terms – among those of African origin. However, in absolute terms, the biggest individual non-White group was that of Pakistani origin, with more than 22,000 resident in the city at the time of the last census (approximately one third of the total non-White population in the city).
Future Projections
Clearly any projections of population size are subject to a whole range of uncertainties, limitations and assumptions, and in the case of ethnicity-based projections, yet more uncertainties (e.g. in relation to future immigration policy in Scotland and the UK) apply. Thus we must be cautious in our use and interpretation of these data. That said, the projections take a complex set of factors into account, and comparisons with previous 2001-based projections suggested a reassuring level of accuracy, at least over a shorter period (Prof. Phil Rees, University of Leeds. Personal communication, February 2017).
Limiting our analyses to a 20-year period, Fig. 5 shows the projected increases in the percentages of the total populations of Scotland and Glasgow classed as non-White ethnic minority groups between 2011 and 2031. As can be seen, nationally the figure is forecast to increase from 4% to 7%. In absolute terms this equates to an increase from approximately 212,000 to 411,000 individuals. The equivalent figures for Glasgow predict an increase from 12% to 19% of the total population (approximately 69,000 to 123,000 individuals).
Non-White ethnic minority population projections, Glasgow and Scotland, 2011–2031 (Source: Wohland et al., ETHPOP Database (www.ethpop.org))
Figures 6 and 7 suggest that broadly similar increases will be seen among males and females (Fig. 6) and different age groups (Fig. 7). In Glasgow in particular, there will continue to be greater numbers of non-White males than females. It is also notable that Fig. 6 suggests that by 2031 around a quarter of children in Glasgow will be from a non-White ethnic minority group.
Non-White ethnic minority population projections, 2011–2031, Glasgow and Scotland, by gender (source: Wohland et al., ETHPOP database (www.ethpop.org))
Non-White ethnic minority population projections, 2011–2031, Glasgow and Scotland, by age (source: Wohland et al., ETHPOP database (www.ethpop.org))
Finally, Table 1 shows the projected changes in the size of the White and non-White ethnic groups in Glasgow between 2011 and 2031. In contrast to the White group, the sizes of all the non-White groups are predicted to increase considerably. The biggest single non-White ethnic minority group will continue to be those of Pakistani origin: by 2031, it is predicted that this group will account for over 5% of the total population of the city (just under 35,000 individuals, approximately 28% of the non-White population). The equivalent figures for Scotland are shown in Online Appendix 1.
As stated earlier, the projections are derived from complex modelling of population, fertility, internal migration and immigration, mortality and emigration data. Across the UK, the projected increase in the numbers of some ethnic minority groups (e.g. Pakistanis) is in large part explained by higher fertility rates and younger age structures, while the growth of other groups (e.g. Chinese) relates more to increases in international migration (Rees et al. 2016).
Discussion
Summary of Main Findings
The ethnic composition of the population of Glasgow and Scotland is changing, and it is almost certain that in future years the population will become much more ethnically diverse. This is particularly true in Glasgow, and it has potentially important consequences for population health.
Research evidence from across the globe consistently highlights the fact that the relationships between ethnicity, socioeconomic circumstances, and health are extremely complex. This complexity is arguably enhanced within a Scottish context given the quite different SEP profile of many ethnic minority groups compared with those in other countries such as England and the USA. Proportionately, much higher numbers of some of the key ethnic minority groups (e.g. Chinese, Indian, those of mixed/multiple ethnic origin) live in much less socioeconomically disadvantaged circumstances in Scotland compared with the rest of Britain. General health (as measured, for example, by life expectancy) tends to be better in those groups compared with White Scots, although that picture is much less clear when different indicators such as hospital admissions are used, and when country of birth is taken into account. An extremely complex picture emerges from analyses of individual diseases and ethnic groups in Scotland. There is a lower risk of cancer among many groups (compared with White Scots) but a similar risk of stroke. Those of Pakistani origin have a much greater risk of heart disease and diabetes, and the latter is also true of the Indian population. Chinese men and women tend to have a lower risk of many diseases (although some exceptions – e.g. liver disease – do apply). For many conditions (e.g. respiratory, mental health-related, gastrointestinal), the relationships are complex, with no clear patterns across ethnic minority groups emerging.
Explaining Differences in Health across Ethnic Groups
The higher life expectancy of some non-White groups compared to the White Scots has arguably led to an over-simplistic and misleading view of underlying causes being presented in the Scottish media – a view which ignores both important disease-specific variation in health status between different ethnic groups, as well as its important socioeconomic context:
“High levels of smoking and alcohol consumption have most probably contributed to the lower life expectancy of White Scots, along with poor diet... I hope we can learn lessons from ethnic minority communities that can be used to improve the health of the whole population.” (Philip 2016)
From the wealth of research evidence now available, it is clear that the reality is much more complex than such statements suggest. This complexity extends to understanding the reasons for differences in health between ethnic groups. Davey Smith and colleagues have previously provided a useful summary of the most frequently proposed ‘models of explanation’ for differences in health status between different ethnic groups in Britain. These include a number of issues already discussed above, for example the complex relationship between SEP and ethnic health. An additional aspect of this, however, is social class (an important component of SEP) artefact. This includes evidence of limitations and inaccuracies associated with traditional social class categories, as well as the results of downward social mobility related to migration i.e. migrants of original ‘high’ social class engaged in ‘low’ social class occupations which can impact on SEP-related analyses. Also included are cultural factors, both in terms of different health-related behaviours already discussed, but also other issues relating to strong family support networks and religious activities, both of which have been shown to be associated with protective effects for health (Kawachi 1999; Kawachi et al. 1997; Skrabski et al. 2003; Kripper and Sapag 2009; Murayama et al. 2012; Maselko et al. 2011; Koenig et al. 2001; McCullough et al. 2000; Coruh et al. 2005; Hummer et al. 2004). The importance of the impact of racism has also already been alluded to. Migration is also important: there is a considerable amount of evidence to support the ‘healthy migrant effect’ i.e. the better health characteristics associated with those who have the resources to migrate (this relates primarily to international migration, rather than sub-national migration). However, it is also known that these tend to diminish over time and over generations. There is less evidence for what has been referred to as ‘salmon bias’ i.e. the notion of older migrants returning to their country of birth before death (and which would, therefore, impact on ethnic mortality rates both in their country of birth and their previous country of residence). Other potential explanations discussed by Davey Smith et al. for which there is either very little supporting evidence, or which are deemed to have only a minor impact are: genetic factors (these are deemed to play a minor role, in part because there tends to be greater genetic differences within ethnic groups, rather than between them); worse access to health and social services (for which little evidence was identified at the time of publication); and artefact (a theory that Davey Smith et al. discounted).
Implications of the Changing Ethnic Profile of Scotland and Glasgow
In the light of the evidence from SHELS and other research discussed above, what can we say about the population health implications of the projected trends in the size of the ethnic minority population? In truth, it is extremely difficult to arrive at meaningful conclusions with any degree of certainty. This is for a number of important reasons. First, the population projections presented earlier are, as already stated, subject to considerable uncertainties. Second, the issue of ‘acculturation’ among particular ethnic groups – whereby health-related behaviours and, therefore, outcomes among migrants change over time to be more like the existing population – is well evidenced (Hawkins et al. 2008; Ajetunmobi et al. 2014; Delavari et al. 2013; Thomson and Hoffman-Goetz 2009) but its impact is difficult to predict. One potential example of this – rates of breast cancer incidence among UK South Asian women increasing to the level of the UK White population – was discussed earlier; other evidence relating to, for example, obesity and maternity related factors (breastfeeding, smoking during pregnancy) has been published in recent times. Third, as the summary of the SHELS evidence showed, the whole picture of ethnic minority health in Scotland is complex, with greater and lesser risks of particular diseases evident across different groups, and with the relationship between health and social and economic circumstances difficult to fathom: this renders future predictions even more problematic. Fourth, any analysis of the potential impact of changes in the size of the ethnic minority population on the health profile of the whole population clearly has to be undertaken alongside a deep understanding of changes to the health profile of the majority White population. As is well understood, this is determined by a complex set of factors operating and interacting across the lifecourse. Key among these determinants are socioeconomic and political factors, and in an era of political and economic uncertainty, where the long-term effects of – for example – the recent global recession, the politics of so-called ‘austerity’ including important changes to the UK social security system and other cuts to services, and ‘Brexit’ are still under discussion, it would be foolish to predict any future changes to the health status of the whole population, and to particular sections of it.
All that said, we can be reasonably confident of certain facts. The size of the non-White population is likely to continue increasing in future years. This will include increases in the number of ageing and elderly members of that population. We know that different ethnic groups have different risks of particular diseases (e.g. considerably higher risk of heart disease and diabetes among South Asians) compared with the White Scottish population. We know that some minority groups (e.g. those of African origin, as shown in Fig. 1) are more likely than other groups to live in disadvantaged circumstances – and that such living conditions have implications for individuals’ health and wellbeing. For some groups, the projected population increase relates (in part) to higher fertility rates and younger age structures, while for others it is more attributable to increases in international migration (suggesting potential differences in numbers of English speakers in different groups). These facts all have relevance to policy-makers and those involved in health and social service provision. The implications are multiple and include: increased needs for health services for cardiovascular disease and diabetes from amongst the ethnic minority population; an increased need for culturally-sensitive health and social care practice as the size and age distribution of the ethnic minorities increases and changes; and potential increased demand for translation and interpreting services. There are broader implications for Scotland to ensure that inequalities in opportunity or outcomes do not become ingrained, and which might feed discriminatory or racist attitudes and actions. This is likely to require consideration and action across the public sector, and in particular the housing and education systems.
Implications for Research
The uncertainties outlined above highlight the clear need for further research in this area. In Scotland SHELS has provided an important, detailed, ‘baseline’ picture of morbidity and mortality among different ethnic groups. However, given the speed at which such research can become out of date – the SHELS cohort was based on the 2001 census – combined with the changing size and nature of Scotland’s ethnic minority population, and the fact no linkage of health data to the 2011 census is currently available, suggests there is an urgent need for further work. This would enable a clearer understanding of the impact of these population changes on future health service demand, as well as associated social policy and planning requirements. It would also be important to consider the particular socio-economic and health profiles of Glasgow within any such future work: the city is among the most deprived in the UK, and recent work has highlighted the most likely – principally political and historical – underlying causes of the city’s excess levels of mortality (Walsh et al. 2017). Understanding the interactions between these important contextual factors and the changing nature of the population (as described in this paper) would be an important undertaking.
Recent statistical and data developments also offer the potential for further research in this area which could reduce the levels of uncertainty associated with projections in population composition and associated disease prevalence. For example, recent UK research has used microsimulation modelling techniques, based on a combination of administrative data and evidence from a nationally representative longitudinal study, to model the future prevalence of important disease categories (Clark and Rees 2017), while various recent methodological advances employed in the development of projections in New Zealand may also offer relevant opportunities to researchers and policymakers in Scotland to better understand the implications of the changes to the Scottish population discussed in this paper (Statistics New Zealand 2016; Statistics New Zealand 2017).
Strengths and Weaknesses of this Research
There are some important weaknesses of the research reported in this paper. Most notably, the literature review was limited in its scope, focussing primarily (although not exclusively) on the Scottish context. This was arguably a short-sighted approach; however, it can equally be argued that it would be potentially more problematic to apply evidence from other settings, especially when important differences in socioeconomic context have not been taken into account. As already stated, there are a number of uncertainties associated with the use of population projections. The majority of SHELS studies have measured the risk of hospitalisation or death among ethnic minority groups compared with the White Scottish population: they have not, therefore, measured the prevalence of disease among the different groups; furthermore, for some conditions (e.g. respiratory conditions such as asthma), limiting measurement to hospitalisation or death clearly captures only the extreme end of the spectrum of disease. Comparison with White Scots entails additional complications of interpretation, given the well-known poor health profile of Scotland compared to other high income countries (McCartney et al. 2012; Whyte and Ajetunmobi 2012).
However, there is also a strength in (partly) limiting the review to Scottish evidence, given both the different socioeconomic profile of the country’s ethnic minority population compared with England and other developed countries, and the complex relationships between ethnicity, health and SEP, as have been discussed. Furthermore, despite the stated limitations, the use of the SHELS study itself is a considerable strength, given the rich insights it has provided into ethnicity and health in a Scottish context that were previously not available. Finally, despite the aforementioned uncertainties, the ethnic population projections are a valuable resource for research and planning purposes, and we limited analyses of the data to a reasonably short (and therefore, potentially less uncertain) time period.
Conclusions
The relationship between ethnicity and health is a complex one. Overall levels of population health, as measured by indicators such as life expectancy, have been shown to be better among many non-White ethnic minority groups in Scotland compared with the White Scottish population. However, such analyses mask a highly complicated set of varying risks of particular diseases among different groups. The complexity extends to understanding the underlying causes of these differences in health status, including the impact of the ‘healthy migrant’ effect, how that may or may not change over time, and, not least, the association between ethnicity and socioeconomic circumstances. This is arguably even more complex in Scotland, compared with, for example, England or the USA, given the quite different SEP profile of many of Scotland’s ethnic minority groups. Despite a number of uncertainties in relation to precise estimates, the size of Scotland’s non-White minority population looks set to increase. This poses a challenge to researchers in seeking to understand the changing health profile of this important, and growing, section of the population – a challenge made greater by the lack of any planned follow-up to the unique SHELS study. More importantly, however, it presents an increasingly urgent challenge to policy-makers and service-planners, given their need to understand, and address, the possible implications of these changes to the population.
Notes
In the 2011 Census, just over 54,000 people in Scotland identified themselves as ‘White: Irish’ (1% of the total), and over 61,000 identified themselves as ‘White: Polish’ (1.2% of the total).
Titles only (not abstracts) of papers in the EMBASE and MEDINFO databases (only for the period 1996 to the present) were searched using the following search terms: ethnic* and (health or mortality or morbidity or disease*) and (review or summary).
There are 56 such ‘neighbourhoods’ across the city of Glasgow. Previously known as housing forum areas, and created by Glasgow City Council in consultation with housing associations, these have been used extensively in analyses of health and wellbeing in the city, including within the Understanding Glasgow indicators project (www.understandingglasgow.com). They have an average population size of approximately 11,000 people.
For the 2011 Census, this includes the following ethnic groups: Mixed or multiple ethnic groups; Asian, Asian Scottish or Asian British; African; Caribbean or Black; other ethnic groups.
‘Middle’ areas refers to the fact that, as Figure 1 shows, in 2011 the highest percentage of Pakistanis were resident in Decile 4 (where Decile 1 represents the most deprived 10% of the population, and Decile 10 represents the least deprived).
These areas are datazones in Scotland and Lower Super Output Areas (LSOAs) in England. These are small geographical units used for a number of administrative purposes in each country, including the measurement of neighbourhood deprivation.
Note that in this paper by Millard et al. (2015) the analyses focussed on comparisons of Whites and ‘Asians’: the latter group was comprised of those of ‘Indian, Pakistani, Bangladeshi and any other Asian background except Chinese’.
It is worth noting that because the SHELS study is based on the linkage of individual census records, it is possible to take account of a number of individual socioeconomic measures e.g. educational attainment, employment status, occupational social class.
In this paper (by Bhopal et al. 2012a.) no SEP indicators were included in the modelling because the eight variables which were looked at “did not meet the requirement of a confounding variable for our purposes”. This was reported as being on account of the inconsistent relationships between the different indicators, different ethnic groups and different outcomes (i.e. types of cancer) of interest.
In this paper (by Fischbacher et al. 2007a) incidence rates are presented without adjustment for area deprivation, although some other survival-based analyses are reported as having adjusted for this. Note also that a later (2013) SHELS paper on myocardial infarction by Bansal et al. did adjust for a measure of education.
The cited SHELS research did not calculate life expectancy for all ethnic groups, only those with sufficient numbers including males and females of Indian, Pakistani and Chinese origin. The analyses did not adjust for SEP.
The cited research by Millard et al. (based on analyses of the Scottish Longitudinal Study) only compared mortality between the White population and those of Asian origin (but excluding Chinese). Mortality rates were generally higher among Whites.
For example, those of Pakistani origin reported worse general health in the 2001 and 2011 Censuses, and by far the worst levels of self-reported poor health were by Gypsy travellers.
The analyses included all types of cancer with the exception of non-melanoma skin cancer.
It is notable that although African origin females were observed to have a similar risk of stroke, African origin males had a notably higher risk (almost 40%) compared to the White Scottish group.
Note that the lower risk of hospitalisation or death from heart failure was shown for Chinese men (age and education adjusted risk ratio: 42.3 (29.5 to 60.6)) but not women (77.3 (50.2 to 119.0)). For the other heart disease-related measures reported, a lower risk was observed for Chinese males and females.
Most of the SHELS studies cited here adjusted for a measure of SEP. However, the analyses of routine hospital admissions data did not.
There are also notable differences in smoking rates between Pakistani men and women, with much higher rates among men.
This relates to higher rates of ‘heavy drinking’ and associated health harm (rates of liver cirrhosis) (Hurcombe et al. 2010)
These areas were selected for illustrative purposes, and on the basis of having among the highest percentage figures for the minority non-White population in 2011.
References
Ajetunmobi, O., Whyte, B., Chalmers, J., Fleming, M., Stockton, D., & Wood, R. (2014). Informing the "early years" agenda in Scotland: Understanding infant feeding patterns using linked datasets. Journal of Epidemiology & Community Health, 68(1), 83–92.
Ali, R., Barnes, I., Kan, S. W., & Beral, V. (2010). Cancer incidence in British Indians and British whites in Leicester, 2001-2006. British Journal of Cancer, 103(1), 143–148.
Aspinall, P. J. (2011). The utility and validity for public health of ethnicity categorization in the 1991, 2001 and 2011 British censuses. Public Health, 125(10), 680–687.
Au, N., & Johnston, D. W. (2014). Self-assessed health: What does it mean and what does it hide? Social Science & Medicine, 121, 21–28.
Bansal, N., Fischbacher, C. M., Bhopal, R. S., Brown, H., MFC, S., Capewell, S., & on behalf of the Scottish Health and Ethnicity Linkage Study. (2013). Myocardial infarction incidence and survival by ethnic group: Scottish health and ethnicity linkage retrospective cohort study. BMJ Open, 3, e003415.
Bansal, N., Chalmers, J., Fischbacher, C., Steiner, M., Bhopal, R., & on behalf of the SHELS researchers. (2014). Ethnicity & First Birth: Age, smoking, delivery, gestation, Weight & Feeding: Scottish Health & Ethnicity Linkage Study. European Journal of Public Health, 24(6), 910–915.
Bansal, N., Bhopal, R., Netto, G., Lyons, D., Steiner, M. F. C., & Sashidharan, S. P. (2014a). Disparate patterns of hospitalisation reflect unmet needs and persistent ethnic inequalities in mental health care: The Scottish health and ethnicity linkage study. Ethnicity & Health, 19(2), 217–239.
Bhala, N., Cézard, G., Ward, H. J. T., Bansal, N., Bhopal, R., & on behalf of the Scottish Health and Ethnicity Linkage Study (SHELS) Collaboration. (2016). Ethnic variations in liver- and alcohol-related disease Hospitalisations and mortality: The Scottish health and ethnicity linkage study. Alcohol and Alcoholism, 51(5), 593–601.
Bhopal, R., Fischbacher, C., Povey, C., Chalmers, J., Mueller, G., Steiner, M., Brown, H., Brewster, D. H., & Bansal, N. (2011). Cohort profile: Scottish health and ethnicity linkage study of 4.65 million people exploring ethnic variations in disease in Scotland. International Journal of Epidemiology, 40(5), 1168–1175.
Bhopal, R. S., Bansal, N., Steiner, M., Brewster, D. H., & on behalf of the Scottish Health and Ethnicity Linkage Study. (2012a). Does the 'Scottish effect' apply to all ethnic groups? All cancer, lung, colorectal, breast and prostate cancer in the Scottish Health and Ethnicity Linkage Cohort Study. BMJ Open, 2(5), e001957.
Bhopal, R. S., Bansal, N., Fischbacher, C. M., Brown, H., Capewell, S., & on behalf of the Scottish Health and Ethnic Linkage Study. (2012b). Ethnic variations in the incidence and mortality of stroke in the Scottish health and ethnicity linkage study of 4.65 million people. European Journal of Preventive Cardiology, 19(6), 1503–1508.
Bhopal, R. S., Bansal, N., Fischbacher, C. M., Brown, H., Capewell, S., & on behalf of the Scottish Health and Ethnic Linkage Study. (2012c). Ethnic variations in chest pain and angina in men and women: Scottish ethnicity and health linkage study of 4.65 million people. European Journal of Preventive Cardiology, 19(6), 1250–1257.
Bhopal, R. S., Bansal, N., Fischbacher, C. M., Brown, H., Capewell, S., & on behalf of the Scottish Health and Ethnic Linkage Study. (2012d). Ethnic variations in heart failure: Scottish health and ethnicity linkage study (SHELS). Heart, 98(6), 468–473.
Bhopal, R. S., Cezard, G., Bansal, N., Ward, H. J. T., Bhala, N., & on behalf of the SHELS Researchers. (2014). Ethnic variations in five lower gastrointestinal diseases: Scottish Health and Ethnicity Linkage Study. BMJ Open, 4(10), e006120.
Bhopal, R., Steiner, M. F., Cezard, G., Bansal, N., Fischbacher, C., Simpson, C. R., Douglas, A., Sheikh, A., & on behalf of the SHELS Researchers. (2015). Risk of respiratory hospitalization and death, readmission and subsequent mortality: Scottish health and ethnicity linkage study. European Journal of Public Health, 25(5), 769–774.
Bhopal R.S., Gruer L., Cezard G. , Douglas A., Steiner M.F.C., Millard A., Buchanan D., Katikireddi S.V., Sheikh A (submitted). Mortality, ethnicity and country of birth on a national scale 2001–2013: the Scottish Health and Ethnicity Linkage Study. Submitted to PLOS Medicine 2017.
Bhui, K., McKenzie, K., & Rasul, F. (2007). Rates, risk factors and methods of self harm among minority ethnic groups in the UK: A systematic review. BMC Public Health, 7, 336.
Black, D., Morris, J., Smith, C., & Townsend, P. (1980). Inequalities in health: Report of a research working group. London: Department of Health and Social Security.
Bostan, C., Oberhauser, C., Stucki, G., Bickenbach, J., & Cieza, A. (2014). Biological health or lived health: Which predicts self-reported general health better? BMC Public Health, 14, 189.
Cezard, G. I., Bhopal, R. S., Ward, H. J., Bansal, N., Bhala, N., & on behalf of the SHELS researchers. (2016). Ethnic variations in upper gastrointestinal hospitalizations and deaths: The Scottish health and ethnicity linkage study. European Journal of Public Health, 26(2), 254–260.
Clark SD, Rees, PH (2017). The drivers of health trends: a decomposition of projected health for local areas in England. In: Swanson, DA, (E.). Frontiers in Applied Demography. Applied Demography Series, 9 . Springer , pp. 21–40.
Coruh, B., Ayele, H., Pugh, M., & Mulligan, T. (2005). Does religious activity improve health outcomes? A critical review of the recent literature. Journal of Science and Healing, 1(3), 186–191.
Crawford F, Beck S, McLean J, Walsh D, Tannahill C (2012). Migration and health in Glasgow and its relevance to GoWell. Glasgow: GoWell. Available from: http://www.gowellonline.com/publications/97_migration_and_health_in_glasgow_and_its_relevance_to_gowell (accessed August 2017).
Dahlgren G, Whitehead M (1993). Tackling inequalities in health: what can we learn from what has been tried? Working paper prepared for the King's Fund International Seminar on Tackling Inequalities in Health, September 1993. Ditchley Park, Oxfordshire: King's Fund.
Darlington, F., Norman, P., Ballas, D., & Exeter, D. (2015). Exploring ethnic inequalities in health: Evidence from the health survey for England, 1998-2011. Diversity & Equality in Health & Care, 12(2), 54–65.
Delavari, M., Sønderlund, A. L., Swinburn, B., Mellor, D., & Renzaho, A. (2013). Acculturation and obesity among migrant populations in high income countries - a systematic review. BMC Public Health, 13, 458.
Douglas, A., Cézard, G., Simpson, C. R., Steiner, M. F., Bhopal, R., Bansal, N., Sheikh, A., Ward, H. J., Fischbacher, C. M., & on behalf of the SHELS researchers. (2016). Pilot study linking primary care records to census, cardiovascular hospitalization and mortality data in Scotland: Feasibility, utility and potential. Journal of Public Health, 38(4), 815–823.
Evans, R. G., & Stoddart, G. L. (1994). Producing health, consuming health care. In R. G. Evans, M. L. Barer, & T. R. Marmor (Eds.), Why are some people healthy and others not? The determinants of health of populations. Berlin, New York: Walter de Gruyter.
Fischbacher, C. M., Hunt, S., & Alexander, L. (2004). How physically active are south Asians in the United Kingdom? A literature review. Journal of Public Health, 26(3), 250–258.
Fischbacher, C. M., Bhopal, R., Povey, C., Steiner, M., Chalmers, J., Mueller, G., Jamieson, J., & Knowles, D. (2007a). Record linked retrospective cohort study of 4.6 million people exploring ethnic variations in disease: Myocardial infarction in south Asians. BMC Public Health, 7, 142.
Fischbacher, C. M., Steiner, M., Bhopal, R., Chalmers, J., Jamieson, J., Knowles, D., & Povey, C. (2007b). Variations in all cause and cardiovascular mortality by country of birth in Scotland, 1997-2003. Scottish Medical Journal, 52(4), 5–10.
Fischbacher, C. M., Bhopal, R., Steiner, M., Morris, A. D., & Chalmers, J. (2009). Is there equity of service delivery and intermediate outcomes in south Asians with type 2 diabetes? Analysis of DARTS database and summary of UK publications. Journal of Public Health, 31(2), 239–249.
Fischbacher, C. M., Cezard, G., Bhopal, R. S., Pearce, J., Bansal, N., & on behalf of Scottish Health and Ethnicity Linkage Study. (2014). Measures of socioeconomic position are not consistently associated with ethnic differences in cardiovascular disease in Scotland: Methods from the Scottish health and ethnicity linkage study (SHELS). International Journal of Epidemiology, 43(1), 129–139.
Fitzpatrick J, Jacobson B, Aspinall P (2005). Indications of public health in the English regions 4: Ethnicity and health. Association of Public Health Observatories. Available from: http://webarchive.nationalarchives.gov.uk/20170106093837/http://www.apho.org.uk/resource/item.aspx?RID=39367 (accessed July 2017).
Gordon, D. S., Graham, L., Robinson, M., & Taulbut, M. (2010). Dimensions of diversity: Population differences and health improvement opportunities. Glasgow: NHS Health Scotland.
Gruer, L., Cézard, G., Clark, E., Douglas, A., Steiner, M., Millard, A., Buchanan, D., Katikireddi, S. V., Sheikh, A., & Bhopal, R. (2016). Life expectancy of different ethnic groups using death records linked to population census data for 4.62 million people in Scotland. Journal of Epidemiology & Community Health, 70(12), 1251–1254.
Harding, S., & Maxwell, R. (1997). Differences in mortality of migrants. In F. Drever & M. Whitehead (Eds.), Health inequalities. London: The Stationary Office.
Hatzenbuehler, M. L., Phelan, J. C., & Link, B. G. (2013). Stigma as a fundamental cause of population health inequalities. American Journal of Public Health, 103(5), 813–821.
Hawkins, S. S., Lamb, K., Cole, T. J., & Law, C. (2008). Influence of moving to the UK on maternal health behaviours: Prospective cohort study. BMJ, 336(7652), 1052–1055.
Hummer, R. A., Ellison, C. G., Rogers, R. G., Moulton, B. E., & Romero, R. R. (2004). Religious involvement and adult mortality in the United States: Review and perspective. Southern Medical Journal, 97(12), 1223–1230.
Hurcombe R, Bayley M, Goodman A (2010). Ethnicity and alcohol: A review of the UK literature. York: Joseph Rowntree Foundation. Available from https://www.jrf.org.uk/report/ethnicity-and-alcohol-review-uk-literature (accessed July 2017).
Jürges, H. (2007). True health vs response styles: Exploring cross-country differences in self-reported health. Health Economics, 16, 163–178.
Kawachi, I. (1999). Social capital and community effects on population and individual health. Annals of the New York Academy of Sciences, 896(1), 120–130.
Kawachi, I., Kennedy, B., Lochner, K., & Prothrow-Stith, D. (1997). Social capital, income inequality, and mortality. American Journal of Public Health, 87(9), 1491–1498.
Kelaher, M., Paul, S., Lambert, H., Ahmad, W., & Smith, G. D. (2008). The impact of different measures of socioeconomic position on the relationship between ethnicity and health. Annals of Epidemiology, 18(5), 351–356.
Kelly B, Ashe S (2014). Geographies of deprivation and diversity in Glasgow. Manchester: ESRC Centre on Dynamics of Ethnicity (CoDE). Available from: http://www.ethnicity.ac.uk/medialibrary/briefings/localdynamicsofdiversity/geographies-of-deprivation-and-diversity-in-glasgow.pdf (accessed July 2017).
Kelly, Y., Panico, L., Bartley, M., Marmot, M., Nazroo, J., & Sacker, A. (2009). Why does birthweight vary among ethnic groups in the UK? Findings from the millennium cohort study. Journal of Public Health, 31(1), 131–137.
Knox S, Bhopal R, Buchanan D, Thomson CS, Millard A, Fraser A, Gruer L (2016). Using routinely collected data to compare hospital admission rates by ethnic group in Scotland. Glasgow: ScotPHO. Available from: http://www.scotpho.org.uk/publications/reports-and-papers/1916-using-routinely-collected-data-to-compare-hospital-admission-rates-by-ethnic-group-in-scotland (accessed July 2017).
Koenig, H., McCullough, M., & Larson, D. (2001). Handbook of religion and health. New York: Oxford University Press.
Krieger, N. (2011). Epidemiology and the People's health. Theory and context. Oxford: Oxford University Press.
Kripper, C. E., & Sapag, J. C. (2009). Social capital and health in Latin America and the Caribbean: A systematic review. Pan American Journal of Public Health, 25(2), 162–170.
Layes, A., Asada, Y., & Kepart, G. (2012). Whiners and deniers - what does self-rated health measure? Social Science & Medicine, 75, 1–9.
Link, B. G., & Phelan, J. C. (2002). McKeown and the idea that social conditions are fundamental causes of disease. American Journal of Public Health, 92(5), 730–732.
Margetts, B. M., Mohd Yusof, S., Al Dallal, Z., & Jackson, A. A. (2002). Persistence of lower birth weight in second generation south Asian babies born in the United Kingdom. Journal of Epidemiology & Community Health, 56, 684–687.
Marmot, M., & Wilkinson, R. G. (2003). Social determinants of health: The solid facts (Second edition). Denmark: World Health Organization.
Maselko, J., Hughes, C., & Cheney, R. (2011). Religious social capital: Its measurement and utility in the study of the social determinants of health. Social Science & Medicine, 73(5), 759–767.
McCartney, G., Walsh, D., Whyte, B., & Collins, C. (2012). Has Scotland always been the 'sick man' of Europe? An observational study from 1855 to 2006. European Journal of Public Health, 22(6), 756–760.
McCartney, G., Collins, C., & Mackenzie, M. (2013). What (or who) causes health inequalities: Theories, evidence and implications? Health Policy, 113(3), 221–227.
McCullough, M. E., Hoyt, W. T., Larson, D. B., Koenig, H. G., & Thorensen, C. E. (2000). Religious involvement and mortality: A meta-analytic review. Health Psychology, 19(3), 211–222.
Millard, A. D., Raab, G., Lewsey, J., Eaglesham, P., Craig, P., Ralston, K., & McCartney, G. (2015). Mortality differences and inequalities within and between 'protected characteristics' groups, in a Scottish cohort 1991-2009. International Journal for Equity in Health, 14, 142.
Mindell, J. S., Knott, C. S., Ng Fat, L. S., Roth, M. A., Manor, O., Soskolne, V., & Daoud, N. (2014). Explanatory factors for health inequalities across different ethnic and gender groups: Data from a national survey in England. Journal of Epidemiology & Community Health, 68(12), 1133–1144.
Murayama, H., Fujiwara, Y., & Kawachi, I. (2012). Social capital and health: A review of prospective multilevel studies. Journal of Epidemiology, 22(3), 179–187.
Nazroo, J. Y. (1997). The health of Britain's ethnic minorities: Findings from a national survey. London: PSI.
Netto, G. (2012). Minority ethnic communities and housing: Access, experiences and participation. In G. Craig, K. Atkin, S. Chattoo, & R. Flynn (Eds.), Understanding race and ethnicity: Theory, history, policy and practice (understanding welfare: Social issues, policy and practice series). Bristol: Policy Press.
Netto G, Fancy C, Pawson H, Lomax D, Singh S, Power S (2004). Black and minority ethnic communities and homelessness in Scotland. Edinburgh: Scottish Executive Social Research. Available from: http://www.gov.scot/Publications/2004/07/19610/39940 (accessed August 2017).
Nixon R (2016). Comparisons of aspects of Glasgow's 56 neighbourhoods. Glasgow: Glasgow Centre for Population Health. Available from: http://www.gcph.co.uk/assets/0000/5492/Comparisons_of_aspects_of_Glasgows_56_neighbourhoods.pdf (accessed August 2017).
O'Reilly, D., & Rosato, M. (2010). Dissonances in self-reported health and mortality across denominational groups in Northern Ireland. Social Science & Medicine, 71, 1011–1017.
Philip B (2016). Ethnic minorities live longer than their white scots neighbours. The Scotsman. Sunday 21 august 2016. (Quoting Laurence Gruer, University of Edinburgh) http://www.scotsman.com/news/ethnic-minorities-live-longer-than-their-White-scots-neighbours-1-4208934 (accessed July 2017).
Razum, O. (2008). Migrant mortality, healthy migrant effect. In W. Kirch (Ed.), Encyclopedia of public health volume 2. New York: Springer.
Rees, P., Wohland, P., & Norman, P. (2016). The United Kingdom's Multi-ethnic Future: How fast is it arriving? In J. Lombard, E. Stern, & G. P. Clarke (Eds.), Applied Spatial Modelling and Planning (pp. 157–171). London: Routledge.
Salomon, J. A., Nordhagen, S., Oza, S., & Murray, C. J. (2009). Are Americans feeling less healthy? The puzzle of trends in self-rated health. American Journal of Epidemiology, 170, 343–351.
Scotland's census (2011). http://www.scotlandscensus.gov.uk/ (accessed July 2017).
Scott, S., Curnock, E., Mitchell, R., Robinson, M., Taulbut, M., Tod, E., & McCartney, G. (2013). What would it take to eradicate health inequalities? Testing the fundamental causes theory of health inequalities in Scotland. Glasgow: NHS Health Scotland.
Scottish Government (2014). Overview of equality results from the 2011 census release 2. Edinburgh: Scottish Government. Available from: http://www.gov.scot/Publications/2014/03/7340 (accessed July 2017).
Scottish Government (2015). Which ethnic groups have the poorest health? An analysis of health inequality and ethnicity in Scotland. Edinburgh: Scottish Government; http://www.gov.scot/Publications/2015/08/7995 (accessed July 2017).
Scottish Index of Multiple Deprivation (SIMD) (2016). Available from: https://www.gov.scot/Topics/Statistics/SIMD (Accessed August 2018).
Sen, A. (2002). Health: Perception versus observation: Self-reported morbidity has severe limitations and can be extremely misleading. BMJ, 324, 860–861.
Sheikh, A., Steiner, M. F. C., Cezard, G., Bansal, N., Fischbacher, C., Simpson, C. R., Douglas, A., & Bhopal, R. (2016). Ethnic variations in asthma hospital admission, readmission and death: A retrospective, national cohort study of 4.62 million people in Scotland. BMC Medicine, 14, 3.
Simpson L, Parsons E (2016). National research report identifying existing services and gaps in provision for ethnic minority communities in Scotland. Perth & Kinross Association of Voluntary Service (PKAVS). Available from: http://www.cpag.org.uk/sites/default/files/Mind%20the%20Gap%20Report%20Jan%202016.pdf (accessed August 2017).
Simpson, C. R., Steiner, M. F., Cezard, G., Bansal, N., Fischbacher, C., Douglas, A., Bhopal, R., Sheikh, A., & on behalf of the SHELS researchers. (2015). Ethnic variations in morbidity and mortality from lower respiratory tract infections: A retrospective cohort study. Journal of the Royal Society of Medicine, 108(10), 406–417.
Singh, G. K., & Siahpush, M. (2001). All-cause and cause-specific mortality of immigrants and native born in the United States. American Journal of Public Health, 91(3), 392–399.
Skrabski, A., Kopp, M., & Kawachi, I. (2003). Social capital in a changing society: Cross sectional associations with middle aged female and male mortality rates. Journal of Epidemiology & Community Health, 57(2), 114–119.
Smith, G. D. (2000). Learning to live with complexity: Ethnicity, socioeconomic position, and health in Britain and the United States. American Journal of Public Health, 90(11), 1694–1698.
Smith, G. D., Chaturvedi, N., Harding, S., Nazroo, J., & Williams, R. (2000). Ethnic inequalities in health: A review of UK epidemiological evidence. Critical Public Health, 10(4), 404–408.
Statistics New Zealand (2016). How accurate are population estimates and projections? An evaluation of Statistics New Zealand population estimates and projections, 1996–2013. Retrieved from www.stats.govt.nz (Accessed August 2018).
Statistics New Zealand (2017). National ethnic population projections: 2013(base)–2038 (update). Avaialable from: https://www.stats.govt.nz/information-releases/national-ethnic-population-projections-2013base2038-update (Accessed August 2018).
Stronks, K., & Kunst, A. E. (2009). The complex interrelationship between ethnic and socio-economic inequalities in health. Journal of Public Health, 31(3), 324–325.
Thomson, M. D., & Hoffman-Goetz, L. (2009). Defining and measuring acculturation: A systematic review of public health studies with Hispanic populations in the United States. Social Science & Medicine, 69(7), 983–991.
Understanding Glasgow, the Glasgow indicators project. (n.d.) www.understandingglasgow.com (accessed July 2017).
Wallace, M. (2016). Adult mortality among the descendants of immigrants in England and Wales: Does a migrant mortality advantage persist beyond the first generation? Journal of Ethnic and Migration Studies, 42(9), 1558–1577.
Walsh, D., McCartney, G., Collins, C., Taulbut, M., & Batty, G. D. (2017). History, politics and vulnerability: Explaining excess mortality in Scotland and Glasgow. Public Health, 151, 1–12.
WHO Commission on Social Determinants of Health. (2008). Closing the gap in a generation: Health equity through action on the social determinants of health. Geneva: World Health Organization.
Whybrow P, Ramsay J, MacNee K (2012). Scottish health survey topic report: Equality groups. Edinburgh: Scottish Government. Available from: http://www.gov.scot/Publications/2012/10/8988/0 (accessed July 2017).
Whyte B, Ajetunmobi T (2012). Still 'The sick man of Europe'? Scottish mortality in a European context 1950–2010: An analysis of comparative mortality trends. Glasgow: GCPH. Available at: http://www.gcph.co.uk/publications/391_still_the_sick_man_of_europe (accessed November 2015).
Wild, S. H., Fischbacher, C., Brock, A., Griffiths, C., & Bhopal, R. (2007). Mortality from all causes and circulatory disease by country of birth in England and Wales 2001-2003. Journal of Public Health, 29(2), 191–198.
Winter, H., Cheng, K. K., Cummins, C., Maric, R., Silcocks, P., & Varghese, C. (1999). Cancer incidence in the south Asian population of England (1990-92). British Journal of Cancer, 79(3–4), 645–654.
Wohland P, Burkitt M, Norman P, Rees P, Boden P and Durham H. (n.d.) ETHPOP database, ESRC follow on fund "ethnic group population trends". See www.ethpop.org (accessed February 2017).
Author information
Authors and Affiliations
Corresponding author
Ethics declarations
Conflict of Interest
The authors declare that they have no conflict of interest.
Electronic supplementary material
ESM 1
(DOCX 15 kb)
Rights and permissions
Open Access This article is distributed under the terms of the Creative Commons Attribution 4.0 International License (http://creativecommons.org/licenses/by/4.0/), which permits unrestricted use, distribution, and reproduction in any medium, provided you give appropriate credit to the original author(s) and the source, provide a link to the Creative Commons license, and indicate if changes were made.
About this article
Cite this article
Walsh, D., Buchanan, D., Douglas, A. et al. Increasingly Diverse: the Changing Ethnic Profiles of Scotland and Glasgow and the Implications for Population Health. Appl. Spatial Analysis 12, 983–1009 (2019). https://doi.org/10.1007/s12061-018-9281-7
Received:
Accepted:
Published:
Issue Date:
DOI: https://doi.org/10.1007/s12061-018-9281-7