Abstract
Objective
Minimally invasive procedures have been developed to reduce surgical trauma after cardiac surgery. Clinical recovery is the main focus of most research. Still, patient-centred outcomes, such as the quality of life, can provide a more comprehensive understanding of the impact of the surgery on the patient’s life. This systematic review aims to deliver a detailed summary of all available research investigating the quality of recovery, assessed with quality of life instruments, in adults undergoing minimally invasive cardiac surgery.
Methods
All randomised trials, cohort studies, and cross-sectional studies assessing the quality of recovery in patients undergoing minimally invasive cardiac surgery compared to conventional cardiac surgery within the last 20 years were included, and a summary was prepared.
Results
The randomised trial observed an overall improved quality of life after both minimally invasive and conventional surgery. The quality of life improvement in the minimally invasive group showed a faster course and evolved to a higher level than the conventional surgery group. These findings align with the results of prospective cohort studies. In the cross-sectional studies, no significant difference in the quality of life was seen except for one that observed a significantly higher quality of life in the minimally invasive group.
Conclusions
This systematic review indicates that patients may benefit from minimally invasive and conventional cardiac surgery, but patients undergoing minimally invasive cardiac surgery may recover sooner and to a greater extent. However, no firm conclusion could be drawn due to the limited available studies. Therefore, randomised controlled trials are needed.
Similar content being viewed by others
Avoid common mistakes on your manuscript.
Introduction
Although traditional cardiac surgery is performed via median sternotomy, this surgical access route can be associated with major complications. These complications include mediastinitis in 0.3 to 5% of patients, with a mortality rate of 14 to 47% [1]. Since the sternum is divided, sternal instability is another possible complication, which is the leading cause of postoperative morbidity and mortality [2, 3]. These complications can result in a prolonged hospital stay and subsequently a higher healthcare cost [4, 5]. Furthermore, poor cosmetic results of the long midline scar and a significant risk of chronic post-sternotomy pain may negatively affect patient experience [6, 7]. As a result, less invasive surgical access routes to the heart have been investigated [8,9,10,11,12,13,14,15,16,17].
Based on physiological parameters and clinical outcomes, including the length of hospital stay and return to work status, it appears that minimally invasive cardiac surgery (MICS) facilitates faster recovery compared to conventional surgery [18,19,20,21]. However, these studies often do not assess the quality of recovery (QoR). QoR is a complex phenomenon covering many dimensions of physical, psychological, and social health [22]. It is a subjective experience by the patient without interpretation by a professional [23, 24].
Several instruments have been developed to assess QoR after surgery, such as the QoR-40. This QoR-40 is a good measure for short-term postoperative recovery (1–7 days) [25, 26]. However, quality of life (QoL) questionnaires fulfill the requirements for assessing late QoR (1 month to 1 year) [22, 26]. The 36-item Short-Form health survey (SF-36) and the EuroQol instrument (EQ-5D) are examples of generic instruments. Additionally, disease-specific instruments such as HeartQoL and Seattle Angina Questionnaire can be used. There is no consensus on which questionnaire is best, since disease-specific instruments perform better in certain diseases but limit the comparability with other populations [27]. The most widely used validated generic QoL questionnaire is SF-36 which comprises 36 questions grouped into eight domains: physical functioning, role-physical (limitations on routine activities due to physical problems), pain, general health, role-emotional (limitations on everyday activities due to emotional problems), energy, emotional well-being, and social functioning. Another commonly used generic questionnaire is the validated EQ-5D Questionnaire, developed to analyse QoL on five dimensions (i.e., mobility, self-care, usual activity, pain/discomfort, and anxiety/depression) [22].
This systematic review aims to deliver a detailed summary of all available research investigating the QoR, assessed with QoL instruments in adults undergoing MICS. The aim is to compare the QoR profile after MICS and conventional cardiac surgery.
Methods
This systematic review is conducted and reported following the Preferred Reporting Items for Systematic Reviews and Meta-Analyses (PRISMA) checklist. A review protocol was published in the PROSPERO register (http://www.crd.york.ac.uk/PROSPERO) in December 2019 with registration number CRD42020163093.
Search strategy
PubMed, EMBASE, and Cochrane Library databases were searched for relevant articles between December 31, 2019, and December 31, 2020. Articles published before 1999 were excluded. The search was limited to articles written in English.
The appropriate Medical Subject Headings (MeSH) were determined using pilot searches. The following keywords were used: cardiac surgical procedures (MeSH terms), aortic valve/therapy (MeSH terms), mitral valve/therapy (MeSH terms), coronary artery bypass (MeSH terms), Aortic root replacement (MeSH terms), Minimally invasive surgical procedures (MeSH terms), Totally endoscopic (all fields), Health-related Quality of life (all fields), SF-36 (all fields), and EQ-5D (all fields). The final search algorithm was established using Boolean logic operators (“AND” and “OR”).
Eligibility criteria
We included all published randomised controlled trials (RCTs), cohort studies, and cross-sectional studies assessing the QoR assessed through the QoL in patients undergoing MICS compared to conventional cardiac surgery. We considered studies if participants were adults undergoing specific types of MICS (aortic valve replacement, coronary artery bypass graft, mitral valve repair or replacement, and aortic root replacement) and if QoR has been assessed with SF-36 or EQ-5D. Exclusion criteria included reviews, abstracts, case reports, editorials, retrospective studies, paediatric patients, or no MICS group.
The primary outcome was defined as the QoR measured with SF-36 or EQ-5D at various time points after MICS compared to conventional surgery. Secondary outcomes included clinical endpoints after MICS.
Data collection and extraction
Selection of studies
First, two authors (JC, RR) independently screened article titles based on the exclusion and inclusion criteria. Irrelevant titles were excluded; discrepancies were resolved by discussion with a third party (BS). Next, abstracts of potentially relevant articles were subsequently assessed, and non-relevant articles were excluded. Lastly, the full-text manuscripts of the remaining articles were evaluated. A hand check of reference lists of included studies was performed to identify additional relevant articles.
Data extraction and management
Two independent reviewers (JC, RR) performed data extraction and quality assessment of relevant studies using a standard data extraction form. Disagreements were resolved after discussion and consensus by requesting a third reviewer (BS).
Assessment of the study quality
The quality assessment tool for controlled intervention studies and observational cohort and cross-sectional studies from the National Institutes of Health was used [28]. This tool includes 14 criteria with a final rating scale of poor, fair, and good. According to their importance, these criteria were sorted to make the articles’ ratings as transparent as possible based on the guidance document. Three levels were used: “primary” when criteria are considered crucial as part of a qualitative study; “secondary” when criteria are not crucial, but if not met, the risk of bias is significantly increased; “tertiary” when not meeting these criteria are not considered to increase the risk of bias. A detailed description of this sorting can be found in the addendum.
In studies where all primary criteria are met, and a maximum of two of the secondaries are not met, a rating of “good” is provided. When a study does not meet the maximum of the primary criteria, and a maximum of two of the secondary criteria are not met, it is assessed as a “fair” study. A “poor” study is identified when more than one of the primary criteria and more than two of the secondary criteria are not met. Although these cross-sectional studies could be considered “good”, we decided to cap the rating of these studies at “fair” as these studies’ design inherently causes less powerful results than controlled interventions or observational cohort studies.
JC and RR assessed the quality of the articles independently. Variability and discrepancies were resolved by discussion with a third party (BS).
Statistical analysis
Due to enormous heterogeneity in the study population and MICS types included, a meta-analysis could not be performed. Study findings are documented in the form of a “Summary of Findings” table.
Results
Study selection
The search results are presented in a PRISMA flow chart in Fig. 1. After removing the duplicates, 249 records were obtained out of 263 items. A total of 231 manuscripts were excluded based on title and abstract. The number of full-text articles assessed for eligibility was 18. Of these 18 studies, 10 were included in the qualitative synthesis.
Study characteristics
Two studies focused on coronary artery bypass grafting (CABG), while valve procedures were performed in the other eight studies. Characteristics of all studies are listed in Tables 1 and 2. Only Nasso et al. conducted a randomised trial. Three prospective observational cohort studies assessed QoL before surgery at different follow-up moments [7, 29, 30]. Six studies were performed in a cross-sectional manner [31,32,33,34,35,36].
Assessment of the study quality
Based on the National Institutes of Health (NIH) quality assessment tool, four studies were rated as “good” [7, 29, 30, 37], while four cross-sectional studies received the rating of “fair” [31, 32, 34, 35] (Table 3). Two studies were identified as “poor” due to methodological issues, including the small sample size, low participation rate, and no description of the patient selection process or follow-up [33, 36].
Study outcomes
The available data regarding the QoL of all included studies are presented in Tables 4 and 5.
Domains of SF-36
Physical functioning
CABG
Bonaros et al. reported a more prominent physical functioning improvement after MICS (robotic totally endoscopic coronary artery bypass (TECAB)) than sternotomy. Three months after MICS, it reached almost 100% [30]. Regarding robotic-assisted minimally invasive direct coronary artery bypass (MIDCAB), the cross-sectional study reported significantly better physical functioning after MICS (MICS: 80.44 ± 19.85, sternotomy: 63.4 ± 19.82, p = 0.008; Table 4) [33].
Valve surgery
In the sole included RCT looking at mitral valve repair, physical functioning improved significantly in the MICS group compared to conventional cardiac surgery patients after 6 months (MICS: 64.9 ± 8.3, sternotomy: 53.1 ± 7, p < 0.001; Table 5) [37]. Additionally, a cross-sectional study reported significantly better physical functioning after MICS for the Ross procedure (MICS: 85.1 ± 18.4, sternotomy: 76.8 ± 21.6, p = 0.027; Table 5 [36]). In contrast, three other studies regarding valve surgery did not observe a significant difference between MICS and sternotomy [32, 34, 35].
Role limitations
CABG
The role-emotional scores significantly improved after both robotic TECAB and conventional CABG [30]. On the other hand, a significantly better role-physical was seen after robotic-assisted MIDCAB compared to conventional CABG in the cross-sectional study (MICS: 82.79 ± 55.11 sternotomy: 45.42 ± 55.63, p < 0.001; Table 4) [33].
Valve surgery
The mitral valve repair RCT observed a significantly better role-emotional score in the MICS group compared to sternotomy after 6 months (MICS: 67.4 ± 9.1, sternotomy: 51.7 ± 6.6, p < 0.001; Table 5) [37].
The role-physical score was significantly better in the MICS group compared to conventional cardiac surgery in the Ross procedure (MICS: 79.2 ± 35.8, sternotomy: 63.0 ± 41.3, 69, p = 0.024; Table 5 [36]). The other studies reporting on this topic observed no significant difference [32, 34, 35].
Pain
CABG
After robotic TECAB, patients stated equivalent pain scores 1 month after surgery compared to baseline. They reported significantly less pain (a higher score) at 3 months after MICS compared to baseline (baseline: 67.3 ± 31.4, 3 months: 94 ± 8.4, p = 0.006; Table 4). Patients who received a sternotomy proclaimed more pain (a lower score) in comparison to MICS patients after 3 months (MICS: 94 ± 8.4, sternotomy: 79.0 ± 21.0, p = 0.037; Table 4) [30]. Significantly less pain (a higher score) was noted in the robotic-assisted MIDCAB patients (MICS: 74.22 ± 23.57, sternotomy: 53.4 ± 27.12, p < 0.001; Table 4) [33].
Valve surgery
A cross-sectional study noted significantly less pain (a higher score) in the MICS group after mitral valve surgery (MICS: 77.05 ± 14.78 and sternotomy: 70.12 ± 12.58; Table 5) [34]. However, all other studies regarding valve surgery observed no significant improvement [32, 35, 36]. The RCT did not report anything regarding pain [37].
General health
CABG
Bonaros et al. reported a significantly better general health score than sternotomy 1 month after robotic TECAB (MICS: 72 ± 9.2, sternotomy: 60 ± 11.9, p = 0.047; Table 4) [30]. The cross-sectional study reported superior long-term general health after MICS in robotic-assisted MIDCAB (MICS: 63.89 ± 22.44, sternotomy: 45.49 ± 21.19, p = 0.001; Table 4) [33].
Valve surgery
The RCT, looking at mitral valve repair, found significantly better general health in the MICS group 6 months after surgery (MICS: 70.2 ± 8.7, sternotomy:52.3 ± 7, p < 0.001; Table 5) [37]. In contrast, in several cross-sectional studies, no significant difference in general health was observed between MICS and the control group after valve surgery [32, 34,35,36].
Energy
CABG
The energy score improved after MICS as well as after conventional cardiac surgery after 3 months post robotic TECAB [30], but was significantly better in the MICS group in the cross-sectional study investigating robotic-assisted MIDCAB (MICS: 55.56 ± 24.76, sternotomy: 45.24 ± 22.16, p = 0.02; Table 4) [33].
Valve surgery
The energy levels were significantly in favour of the MICS group after 6 months post mitral valve repair (MICS: 80.4 ± 9.3, sternotomy: 76.4 ± 8.5, p < 0.001; Table 5) [37]. In contrast, four other cross-sectional studies observed no significant difference [32, 34,35,36].
Emotional well-being
CABG
No significant difference was seen between MICS and sternotomy after CABG at 6 months postoperatively (MICS: 79.4 ± 9.3 and sternotomy: 79.1 ± 8.8, respectively, p = 0.56; Table 4) [30]. However, an improvement in emotional well-being was observed after robotic-assisted MIDCAB compared to sternotomy (MICS: 71.56 ± 21.23, sternotomy: 61.24 ± 22.43, p = 0.007; Table 4)[33].
Valve surgery
The RCT, investigating mitral valve repair, reported no significant difference in emotional well-being between baseline and follow-up after MICS (76.8 ± 7 and 79.4 ± 9.3, respectively; Table 5) [37]. A cross-sectional study observed an improvement in emotional well-being after MICS compared to sternotomy after mitral valve surgery (MICS: 74.62 ± 13.63, sternotomy: 68.42 ± 17.95, p = 0.015; Table 5) [34] while other valve-related studies observed no significant difference [32, 35, 36].
Social functioning
CABG
Social functioning did not differ between MICS and sternotomy after robotic TECAB at 6 months postoperatively (MICS: 73.4 ± 6.8 and sternotomy: 71.9 ± 7, p = 0.1; Table 4), nor after robotic-assisted MIDCAB [30, 33].
Valve surgery
A significant difference in social functioning could not be detected by the RCT between baseline and follow-up after MICS in mitral valve repair [37]. Additionally, in the other studies, no significant improvement was seen [32, 34,35,36].
Domains of EQ-5D
Two prospective cohort studies reported an overall improved QoL through the EQ-5D Questionnaire after valve procedures. In Moscarelli et al., the immediate postoperative QoL was superior in the MICS group. However, no difference in QoL was observed 6 and 12 months after the surgery between MICS and sternotomy [29]. Secondly, Piarulli et al. observed a significantly better QoL in the MICS group than in the sternotomy patients [7]. The specific QoL data is displayed in Table 5.
Clinical outcome
The summary of relevant clinical outcomes of all included studies is presented in Tables 6 and 7.
Discussion
MICS has been developed to reduce surgical trauma caused by sternotomy during conventional cardiac surgery. A good clinical outcome after MICS has already been demonstrated by a lower morbidity and mortality rate [19, 21]. However, patient-reported outcomes have become essential endpoints in medical care. To our knowledge, this is the first systematic review to date to summarise all the available primary research investigating the QoR, assessed with QoL instruments, from the patient’s perspective in adults undergoing MICS.
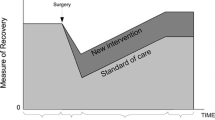
Both sternotomy and MICS patients benefited from the surgery regarding their QoL. In previous studies assessing the QoL after conventional cardiac surgery, the different scales of the SF-36 Questionnaire significantly improved after surgery. One month after the surgery, the QoL improved after conventional surgery but inadequately. After 1 year, satisfactory QoL results were obtained; after 10 years, even the elderly patients had an improved QoL [38, 39]. According to the studies in this systematic review, MICS patients may recover faster and probably to a greater extent. The only RCT available concluded that physical functioning, role limitations, general health, and energy were significantly better in the MICS group 6 months after mitral valve repair surgery, indicating faster re-establishing of the QoL after MICS than sternotomy. However, most cross-sectional studies observed no significant difference between MICS and conventional surgery, varying from 1 to 5 years after the surgery [31, 33, 35, 36].
Improvement in physical functioning was more prominent in MICS patients, and pain scores of patients undergoing sternotomy improved significantly slower. Overall, general health, as well as energy score, improved in both groups after surgery. However, the MICS patients had an earlier improvement in their general health and indicated that they have significantly more energy than conventional surgery patients. In Gjeilo et al. series, no significant improvement in general health or energy score was seen in conventional cardiac patients after 10 years [39]. Scores on social functioning varied among the various studies. As a result, no firm conclusion could be drawn regarding this subscale. In the study by Pačarić et al., the social functioning did not improve significantly, but was not as low as other subscales at baseline [38]. This same trend is seen in the RCT included in this review [37].
Limitations
There are several limitations to this systematic review. First, only studies published in English were included, causing a severe risk of language bias. Second, only one RCT comparing QoR after MICS and conventional cardiac surgery could be included making firm conclusions impossible. The lack of RCTs indicates the need for more research regarding the QoL. Without RCTs, a significant selection bias is present. Patients would have been selected based on their age, fragility, number of procedures, preoperative status, and comorbidities to obtain better results. Furthermore, most included studies had a cross-sectional design which does not allow temporal or causal interpretation [40]. No common timepoints were available to calculate summary QoL scores. Finally, the inclusion of studies with different methodologies and different surgeries are significant limitations of this systematic review.
For these reasons, the studies were not directly comparable, and a meta-analysis could not be conducted. However, this comprehensive approach provides a complete overview of the research field and might be helpful for further studies. Future research in QoL after MICS should focus on prospective studies with sufficient sample sizes. A RCT with a MICS arm and a conventional arm would be the best design.
Conclusion
This systematic review indicates that patients benefit from both MICS and conventional cardiac surgery, but patients undergoing MICS may recover sooner and to a greater extent. However, no firm conclusion could be drawn due to the limited available studies with mainly a cross-sectional design. Therefore, this systematic review’s results should be critically interpreted. More high-quality RCTs comparing QoR after MICS and conventional cardiac surgery should be performed to draw more firm conclusions on differences in QoR.
References
Losanoff JE, Richman BW, Jones JW. Disruption and infection of median sternotomy: a comprehensive review. Eur J Cardiothorac Surg. 2002;21:831–9.
Küçükdurmaz F, Ağır I, Bezer M. Comparison of straight median sternotomy and interlocking sternotomy with respect to biomechanical stability. World J Orthop. 2013;4:134–8.
El-Ansary D, Waddington G, Adams R. Measurement of non-physiological movement in sternal instability by ultrasound. Ann Thorac Surg. 2007;83:1513–6.
Iribarne A, Easterwood R, Russo MJ, et al. A minimally invasive approach is more cost-effective than a traditional sternotomy approach for mitral valve surgery. J Thorac Cardiovasc Surg. 2011;142:1507–14.
Rao C, Aziz O, Deeba S, et al. Is minimally invasive harvesting of the great saphenous vein for coronary artery bypass surgery a cost-effective technique? J Thorac Cardiovasc Surg. 2008;135:809–15.
Massetti M, Nataf P, Babatasi G, Khayat A. Cosmetic aspects in minimally invasive cardiac surgery. Eur J Cardiothorac Surg. 1999;16:S73–5.
Piarulli A, Chiariello GA, Bruno P, et al. Psychological effects of skin incision size in minimally invasive valve surgery patients. Innovations (Phila). 2020;15:532–40.
Benetti FJ, Ballester C, Sani G, Doonstra P, Grandjean J. Video assisted coronary bypass surgery. J Card Surg. 1995;10:620–5.
Subramanian VA, McCabe JC, Geller CM. Minimally invasive direct coronary artery bypass grafting: two-year clinical experience. Ann Thorac Surg. 1997;64:1648–55.
Cohn LH, Adams DH, Couper GS, et al. Minimally invasive cardiac valve surgery improves patient satisfaction while reducing costs of cardiac valve replacement and repair. Ann Surg. 1997;226:421–8.
Svensson LG, D’Agostino RS. “J” incision minimal-access valve operations. Ann Thorac Surg. 1998;66:1110–2.
Konertz W, Waldenberger F, Schmutzler M, Ritter J, Liu J. Minimal access valve surgery through superior partial sternotomy: a preliminary study. J Heart Valve Dis. 1996;5:638–40.
Rodríguez JE, Cortina J, Pérez de la Sota E, Maroto L, Ginestal F, Rufilanchas JJ. A new approach to cardiac valve replacement through a small midline incision and inverted L shape partial sternotomy. Eur J Cardiothorac Surg. 1998;14:S115–6.
Sharony R, Grossi EA, Saunders PC, et al. Minimally invasive aortic valve surgery in the elderly: a case-control study. Circulation. 2003;108:II43–7.
De Amicis V, Ascione R, Iannelli G, Di Tommaso L, Monaco M, Spampinato N. Aortic valve replacement through a minimally invasive approach. Tex Heart Inst J. 1997;24:353–5.
Doty DB, DiRusso GB, Doty JR. Full-spectrum cardiac surgery through a minimal incision: mini-sternotomy (lower half) technique. Ann Thorac Surg. 1998;65:573–7.
Karimov JH, Santarelli F, Murzi M, Glauber M. A technique of an upper V-type ministernotomy in the second intercostal space. Interact Cardiovasc Thorac Surg. 2009;9:1021–2.
Tokoro M, Ito T, Maekawa A, et al. Trans-right axillary aortic valve replacement: propensity-matched comparison with standard sternotomy approach. Interact Cardiovasc Thorac Surg. 2017;25:521–5.
Miceli A, Gilmanov D, Murzi M, et al. Minimally invasive aortic valve replacement with a sutureless valve through a right anterior mini-thoracotomy versus transcatheter aortic valve implantation in high-risk patients. Eur J Cardiothorac Surg. 2016;49:960–5.
Ezelsoy M, Caynak B, Bayram M, et al. The comparison between minimally invasive coronary bypass grafting surgery and conventional bypass grafting surgery in proximal LAD lesion. Heart Surg Forum. 2015;18:E042-E46.
Stoliński J, Plicner D, Grudzień G, et al. A comparison of minimally invasive and standard aortic valve replacement. J Thorac Cardiovasc Surg. 2016;152:1030–9.
Stessel B, Fiddelers AA, Joosten EA, Hoofwijk DMN, Gramke H-F, Buhre WFFA. Prevalence and predictors of quality of recovery at home after day surgery. Medicine (Baltimore). 2015;94:e1553.
Desomer A, Van den Heede K, Triemstra Mattanja T, Paget J, De Boer D, Kohn L, Cleemput I. Use of patient-reported outcome and experience measures in patient care and policy. KCE; 2018. https://kce.fgov.be/sites/default/files/2021-11/KCE_303C_Patient_reported_outcomes_Short_Report_0.pdf. Accessed 31 Dec 2020.
Stessel B, Hendrickx M, Pelckmans C, et al. One-month recovery profile and prevalence and predictors of quality of recovery after painful day case surgery: secondary analysis of a randomized controlled trial. PloS one. 2021;16:e0245774.
Kluivers KB, Riphagen I, Vierhout ME, Brölmann HAM, de Vet HCW. Systematic review on recovery specific quality-of-life instruments. Surgery. 2008;143:206–15.
Myles PS, Hunt JO, Fletcher H, Solly R, Woodward D, Kelly S. Relation between quality of recovery in hospital and quality of life at 3 months after cardiac surgery. Anesthesiology. 2001;95:862–7.
De Smedt D, Clays E, De Bacquer D. Measuring health-related quality of life in cardiac patients. Eur Heart J Qual Care Clin Outcomes. 2016;2:149–50.
NIH. Study quality assesment tools 2020. Available from: https://www.nhlbi.nih.gov/health-topics/study-quality-assessment-tools. Accessed on 31 Dec 2020.
Moscarelli M, Lorusso R, Abdullahi Y, et al. The effect of minimally invasive surgery and sternotomy on physical activity and quality of life. Heart Lung Circ. 2021;30:882–7.
Bonaros N, Schachner T, Wiedemann D, et al. Quality of life improvement after robotically assisted coronary artery bypass grafting. Cardiology. 2009;114:59–66.
Lange R, Voss B, Kehl V, Mazzitelli D, Tassani-Prell P, Gunther T. Right minithoracotomy versus full sternotomy for mitral valve repair: a propensity matched comparison. Ann Thorac Surg. 2017;103:573–9.
Wachter K, Franke UFW, Yadav R, et al. Feasibility and clinical outcome after minimally invasive valve-sparing aortic root replacement. Interact Cardiovasc Thorac Surg. 2017;24:377–83.
Ezelsoy M, Oral K, Caynak B, Bayramoglu Z, Akpinar B. Pain and the quality of life following robotic assisted minimally invasive surgery. Heart Surg Forum. 2016;19:E165–8.
Huang LC, Chen DZ, Chen LW, Xu QC, Zheng ZH, Dai XF. Health-related quality of life following minimally invasive totally endoscopic mitral valve surgery. J Cardiothorac Surg. 2020;15:194.
Detter C, Deuse T, Boehm DH, Reichenspurner H, Reichart B. Midterm results and quality of life after minimally invasive vs. conventional aortic valve replacement. Thorac Cardiovasc Surg. 2002;50:337–41.
Franke UFW, Ursulescu A, Göbel N, et al. Results and quality of life after minimally invasive ross procedure. J Heart Valve Dis. 2015;24:295–301.
Nasso G, Bonifazi R, Romano V, et al. Three-year results of repaired Barlow mitral valves via right minithoracotomy versus median sternotomy in a randomized trial. Cardiology (Switzerland). 2014;128:97–105.
Pačarić S, Turk T, Erić I, et al. Assessment of the quality of life in patients before and after coronary artery bypass grafting (CABG): a prospective study. Int J Environ Res Public Health. 2020;17:1417.
Gjeilo KH, Stenseth R, Wahba A, Lydersen S, Klepstad P. Long-term health-related quality of life and survival after cardiac surgery: a prospective study. J Thorac Cardiovasc Surg. 2018;156:2183-90.e2.
Setia MS. Methodology series module 3: cross-sectional studies. Indian J Dermatol. 2016;61:261–4.
Funding
None.
Author information
Authors and Affiliations
Corresponding author
Ethics declarations
Ethical committee approval and informed consent.
Not applicable in systematic reviews.
Human and animal rights statement
No human participants or animals were included in this systematic review.
Conflict of interest
The authors declare that they have no conflicting interests.
Additional information
Publisher's note
Springer Nature remains neutral with regard to jurisdictional claims in published maps and institutional affiliations.
Rights and permissions
Open Access This article is licensed under a Creative Commons Attribution 4.0 International License, which permits use, sharing, adaptation, distribution and reproduction in any medium or format, as long as you give appropriate credit to the original author(s) and the source, provide a link to the Creative Commons licence, and indicate if changes were made. The images or other third party material in this article are included in the article's Creative Commons licence, unless indicated otherwise in a credit line to the material. If material is not included in the article's Creative Commons licence and your intended use is not permitted by statutory regulation or exceeds the permitted use, you will need to obtain permission directly from the copyright holder. To view a copy of this licence, visit http://creativecommons.org/licenses/by/4.0/.
About this article
Cite this article
Claessens, J., Rottiers, R., Vandenbrande, J. et al. Quality of life in patients undergoing minimally invasive cardiac surgery: a systematic review. Indian J Thorac Cardiovasc Surg 39, 367–380 (2023). https://doi.org/10.1007/s12055-023-01501-y
Received:
Revised:
Accepted:
Published:
Issue Date:
DOI: https://doi.org/10.1007/s12055-023-01501-y