Abstract
Right ventricle (RV) dysfunction and failure are now increasingly recognized as an important cause of perioperative morbidity and mortality after cardiac surgery. Although RV dysfunction is common, RV failure is very rare (0.1%) after routine cardiac surgery. However, it occurs in 3% of patients after heart transplantation and in up to 30% of patients after left ventricular assist device implantation. Significant RV failure after cardiac surgery has high mortality. Knowledge of RV anatomy and physiology are important for understanding RV dysfunction and failure. Echocardiography and haemodynamic monitoring are the mainstays in the diagnosis of RV dysfunction and failure. While detailed echocardiography assessment of right heart function has been extensively studied and validated in the elective setting, gross estimation of RV chamber size, function, and some easily obtained quantitative parameters on transesophageal echocardiography are useful in the perioperative setting. However, detailed knowledge of echocardiography parameters is still useful in understanding the differences in contractile pattern, ventriculo-arterial coupling, and interventricular dependence that ensue after open cardiac surgery.










Similar content being viewed by others
References
Denault AY, Haddad F, Jacobsohn E, Deschamps A. Perioperative right ventricular dysfunction. Curr Opin Anaesthesiol. 2013;26:71–81. https://doi.org/10.1097/ACO.0b013e32835b8be2.
Voelkel NF, Quaife RA, Leinwand LA, et al. Right ventricular function and failure: report of a National Heart, Lung, and Blood Institute working group on cellular and molecular mechanisms of right heart failure. Circulation. 2006;114:1883–91. https://doi.org/10.1161/CIRCULATIONAHA.106.632208.
Estrada VHN, Franco DLM, Moreno AAV, Gambasica JAR, Nunez CCC. Postoperative right ventricular Failure in Cardiac Surgery. Cardiol Res. 2016;7:185–95. https://doi.org/10.14740/cr500e.
Lampert BC, Teuteberg JJ. Right ventricular failure after left ventricular assist devices. J Heart Lung Transplant. 2015;34:1123–30. https://doi.org/10.1016/j.healun.2015.06.015.
Mishra V, Svennevig JL, Bugge JF, et al. Cost of extracorporeal membrane oxygenation: evidence from the Rikshospitalet University Hospital, Oslo, Norway. Eur J Cardiothorac Surg. 2010;37:339–42. https://doi.org/10.1016/j.ejcts.2009.06.059.
Wang JMH, Rai R, Carrasco M, et al. An anatomical review of the right ventricle. TRIA. 2019;17:100049. https://doi.org/10.1016/j.tria.2019.100049.
Haddad F, Hunt SA, Rosenthal DN, Murphy DJ. Right ventricular function in cardiovascular disease, part I: anatomy, physiology, aging, and functional assessment of the right ventricle. Circulation. 2008;117:1436–48. https://doi.org/10.1161/CIRCULATIONAHA.107.653576.
Mori S, Tretter JT, Spicer DE, Bolender DL, Anderson RH. What is the real cardiac anatomy? Clin Anat. 2019;32:288–309. https://doi.org/10.1002/ca.23340.
Anderson RH, Cook AJ, Hlavacek J, et al. Normal cardiac anatomy. In: da Cruz EM, et al., editors. Pediatric and congenital cardiology, cardiac surgery and intensive care. London: Springer; 2014. p. 17–46.
Sanz J, Sánchez-Quintana D, Bossone E, Bogaard HJ, Naeije R. Anatomy, function, and dysfunction of the right ventricle: JACC state-of-the-art review. J Am Coll Cardiol. 2019;73:1463–82. https://doi.org/10.1016/j.jacc.2018.12.076.
Ho SY, Nihoyannopoulos P. Anatomy, echocardiography, and normal right ventricular dimensions. Heart. 2006;92:i2–13. https://doi.org/10.1136/hrt.2005.077875.
Farrer-Brown G. Vascular pattern of myocardium of right ventricle of human heart. Br Heart J. 1968;30:679–86. https://doi.org/10.1136/hrt.30.5.679.
Saremi F, Ho SY, Cabrera JA, Sánchez-Quintana D. Right ventricular outflow tract imaging with CT and MRI: part 1, morphology. AJR Am J Roentgenol. 2013;200:W39–50. https://doi.org/10.2214/AJR.12.9333.
Hayrapetyan H. Anatomical and physiological patterns of right ventricle. J Cardiol Curr Res. 2015;2:00049.
van Wolferen SA, Marcus JT, Westerhof N, et al. Right coronary artery flow impairment in patients with pulmonary hypertension. Eur Heart J. 2008;29:120–7. https://doi.org/10.1093/eurheartj/ehm567.
Goldstein JA. Pathophysiology and management of right heart ischemia. J Am Coll Cardiol. 2002;40:841–53. https://doi.org/10.1016/s0735-1097(02)02048-x.
Dell’Italia LJ. The right ventricle: anatomy, physiology and clinical importance. Curr Probl Cardiol. 1991;16:653–720.
Felner JM. The second heart sound. In: Walker HK, Hall WD, Hurst JW, editors. Clinical methods: the history, physical, and laboratory examinations. 3rd edition. Boston: Butterworths; 1990. Chapter 23. Available from: https://www.ncbi.nlm.nih.gov/books/NBK341/. Accessed 8 Apr 2021.
Walker LA, Buttrick PM. The right ventricle: biologic insights and response to disease: updated. Curr Cardiol Rev. 2013;9:73–81. https://doi.org/10.2174/157340313805076296.
Dell’Italia LJ, Walsh RA. Application of a time varying elastance model to right ventricular performance in man. Cardiovasc Res. 1988;22:864–74. https://doi.org/10.1093/cvr/22.12.864.
Redington AN. Right ventricular function. Cardiol Clin. 2002;20:341–9. https://doi.org/10.1016/s0733-8651(02)00005-x.
Ventetuolo CE, Klinger JR. Management of acute right ventricular failure in the intensive care unit. Ann Am Thorac Soc. 2014;11:811–22. https://doi.org/10.1513/AnnalsATS.201312-446FR.
Nootens M, Kaufmann E, Rector T, et al. Neurohormonal activation in patients with right ventricular failure from pulmonary hypertension: relation to hemodynamic variables and endothelin levels. J Am Coll Cardiol. 1995;26:1581–5. https://doi.org/10.1016/0735-1097(95)00399-1.
Fischer LG, Van Aken H, Bürkle H. Management of pulmonary hypertension: physiological and pharmacological considerations for anesthesiologists. Anesth Analg. 2003;96:1603–16. https://doi.org/10.1213/01.ane.0000062523.67426.0b.
Jardin F, Vieillard-Baron A. Right ventricular function and positive pressure ventilation in clinical practice: from hemodynamic subsets to respirator settings. Intensive Care Med. 2003;29:1426–34. https://doi.org/10.1007/s00134-003-1873-1.
Naeije R, Badagliacca R. The overloaded right heart and ventricular interdependence. Cardiovasc Res. 2017;113:1474–85. https://doi.org/10.1093/cvr/cvx160.
Haddad F, Doyle R, Murphy DJ, Hunt SA. Right ventricular function in cardiovascular disease, part II: pathophysiology, clinical importance, and management of right ventricular failure. Circulation. 2008;117:1717–31. https://doi.org/10.1161/CIRCULATIONAHA.107.653584.
Santamore WP, Dell’Italia LJ. Ventricular interdependence: significant left ventricular contributions to right ventricular systolic function. Prog Cardiovasc Dis. 1998;40:289–308. https://doi.org/10.1016/s0033-0620(98)80049-2.
Hsu S. Coupling right ventricular-pulmonary arterial research to the pulmonary hypertension patient bedside. Circ Heart Fail. 2019;12:e005715. https://doi.org/10.1161/CIRCHEARTFAILURE.118.005715.
Tello K, Dalmer A, Axmann J, et al. Reserve of right ventricular-arterial coupling in the setting of chronic overload. Circ Heart Fail. 2019;12:e005512. https://doi.org/10.1161/CIRCHEARTFAILURE.118.005512.
Vonk Noordegraaf A, Westerhof BE, Westerhof N. The relationship between the right ventricle and its load in pulmonary hypertension. J Am Coll Cardiol. 2017;69:236–43. https://doi.org/10.1016/j.jacc.2016.10.047.
Arrigo M, Huber LC, Winnik S, et al. Right ventricular failure: pathophysiology, diagnosis and treatment. Card Fail Rev. 2019;5:140–6. https://doi.org/10.15420/cfr.2019.15.2.
Piazza G, Goldhaber SZ. Acute pulmonary embolism: part I: epidemiology and diagnosis. Circulation. 2006;114:e28–32. https://doi.org/10.1161/CIRCULATIONAHA.106.620872.
Lualdi JC, Goldhaber SZ. Right ventricular dysfunction after acute pulmonary embolism: pathophysiologic factors, detection, and therapeutic implications. Am Heart J. 1995;130:1276–82. https://doi.org/10.1016/0002-8703(95)90155-8.
De Backer D, Vincent J-L. Should we measure the central venous pressure to guide fluid management? Ten answers to 10 questions. Crit Care. 2018;22:43. https://doi.org/10.1186/s13054-018-1959-3.
Inohara T, Kohsaka S, Fukuda K, Menon V. The challenges in the management of right ventricular infarction. Eur Heart J Acute Cardiovasc Care. 2013;2:226–34. https://doi.org/10.1177/2048872613490122.
Gidwani UK, Mohanty B, Chatterjee K. The pulmonary artery catheter: a critical reappraisal. Cardiol Clin. 2013;31:545–65, viii. https://doi.org/10.1016/j.ccl.2013.07.008.
Konstam MA, Kiernan MS, Bernstein D, et al. Evaluation and management of right-sided heart failure: a scientific statement from the American Heart Association. Circulation. 2018;137:e578–622. https://doi.org/10.1161/CIR.0000000000000560.
Kossaify A. Echocardiography assessment of the right ventricle, from the conventional approach to speckle tracking and three-dimensional imaging, and insights into the “Right Way” to explore the forgotten chamber. Clin Med Insights Cardiol. 2015;9:65–75. https://doi.org/10.4137/CMC.S27462.
Rudski LG, Lai WW, Afilalo J, et al. Guidelines for the echocardiography assessment of the right heart in adults: a report from the American Society of Echocardiography endorsed by the European Association of Echocardiography, a registered branch of the European Society of Cardiology, and the Canadian Society of Echocardiography. J Am Soc Echocardiogr. 2010;23:685–713. https://doi.org/10.1016/j.echo.2010.05.010.
Nguyen T, Cao L, Movahed A. Altered right ventricular contractile pattern after cardiac surgery: monitoring of septal function is essential. Echocardiography. 2014;31:1159–65. https://doi.org/10.1111/echo.12657.
Donauer M, Schneider J, Jander N, Beyersdorf F, Keyl C. Perioperative changes of right ventricular function in cardiac surgical patients assessed by myocardial deformation analysis and 3-dimensional echocardiography. J Cardiothorac Vasc Anesth. 2020;34:708–18. https://doi.org/10.1053/j.jvca.2019.08.026.
Wanner PM, Filipovic M. The right ventricle-you may forget it, but it will not forget you. J Clin Med. 2020;9:432. https://doi.org/10.3390/jcm9020432.
de Agustin JA, Martinez-Losas P, de Diego JJG, et al. Tricuspid annular plane systolic excursion inaccuracy to assess right ventricular function in patients with previous tricuspid annulopasty. Int J Cardiol. 2016;223:713–6. https://doi.org/10.1016/j.ijcard.2016.08.276.
Salehian O, Schwerzmann M, Merchant N, Webb GD, Siu SC, Therrien J. Assessment of systemic right ventricular function in patients with transposition of the great arteries using the myocardial performance index: comparison with cardiac magnetic resonance imaging. Circulation. 2004;110:3229–33. https://doi.org/10.1161/01.CIR.0000147284.54140.73.
Galea N, Carbone I, Cannata D, et al. Right ventricular cardiovascular magnetic resonance imaging: normal anatomy and spectrum of pathological findings. Insights Imaging. 2013;4:213–23. https://doi.org/10.1007/s13244-013-0222-3.
Sabe MA, Sabe SA, Kusunose K, Flamm SD, Griffin BP, Kwon DH. Predictors and prognostic significance of right ventricular ejection fraction in patients with ischemic cardiomyopathy. Circulation. 2016;134:656–65. https://doi.org/10.1161/CIRCULATIONAHA.116.022339.
Mozaffarian D, Caldwell JH. Right ventricular involvement in hypertrophic cardiomyopathy: a case report and literature review. Clin Cardiol. 2001;24:2–8. https://doi.org/10.1002/clc.4960240102.
Tello K, Dalmer A, Vanderpool R, et al. Cardiac magnetic resonance imaging-based right ventricular strain analysis for assessment of coupling and diastolic function in pulmonary hypertension. JACC Cardiovasc Imaging. 2019;12:2155–64. https://doi.org/10.1016/j.jcmg.2018.12.032.
Van Kriekinge SD, Berman DS, Germano G. Assessment of RV function using gated blood pool SPECT. J Nucl Cardiol. 2015;22:493–5. https://doi.org/10.1007/s12350-015-0091-x.
Dercle L, Ouali M, Pascal P, et al. Gated blood pool SPECT: the estimation of right ventricular volume and function is algorithm dependent in a clinical setting. J Nucl Cardiol. 2015;22:483–92. https://doi.org/10.1007/s12350-014-0062-7.
Murarka S, Movahed MR. Review of Movahed’s sign (D shaped left ventricle seen on gated SPECT) suggestive of right ventricular overload. Int J Cardiovasc Imaging. 2010;26:553–7. https://doi.org/10.1007/s10554-010-9600-9.
Mielniczuk LM, Birnie D, Ziadi MC, et al. Relation between right ventricular function and increased right ventricular [18F]fluorodeoxyglucose accumulation in patients with heart failure. Circ Cardiovasc Imaging. 2011;4:59–66. https://doi.org/10.1161/CIRCIMAGING.109.905984.
Oikawa M, Kagaya Y, Otani H, et al. Increased [18F]fluorodeoxyglucose accumulation in right ventricular free wall in patients with pulmonary hypertension and the effect of epoprostenol. J Am Coll Cardiol. 2005;45:1849–55. https://doi.org/10.1016/j.jacc.2005.02.065.
Tsai S-Y, Wu Y-W, Wang S-Y, et al. Clinical significance of quantitative assessment of right ventricular glucose metabolism in patients with heart failure with reduced ejection fraction. Eur J Nucl Med Mol Imaging. 2019;46:2601–9. https://doi.org/10.1007/s00259-019-04471-9.
Bindschadler M, Petek B, Elman S, et al. FDG uptake quantification and right ventricular dysfunction in cardiac sarcoidosis. J Nucl Med. 2017;58:514.
Funding
None.
Author information
Authors and Affiliations
Corresponding author
Ethics declarations
Ethics approval
Not required.
Informed consent
Not required.
Statement of human and animal rights
Not applicable being this is a review article.
Conflict of interest
The authors declare no competing interests.
Additional information
Publisher’s note
Springer Nature remains neutral with regard to jurisdictional claims in published maps and institutional affiliations.
Supplementary Information
Below is the link to the electronic supplementary material.
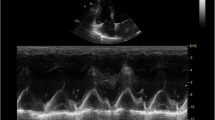
Transesophageal echocardiography 4 chamber view showing normal right ventricular movements. Majority of systolic function occurs by longitudinal contraction supplemented by inward movement of free wall. Additional ejection of right ventricle is contributed by bulging of Inter-ventricular septum to right. (WMV 1609 KB)
Severe right ventricular pressure load causing D shaped septum. The patient is a post operative case of Pulmonary Thromboendarterectomy. The right ventricular pressure was supra-systemic. (WMV 2009 KB)
Transesophageal echocardiography mid esophageal 4 chamber view showing Inter-ventricular septum flopping back and forth. This is typically seen in volume overloaded right ventricle (WMV 1969 KB)
Mid-esophageal 4 chamber view showing poor right ventricular contraction with right ventricular dilatation. Right ventricular size is almost similar to that of left ventricle. Right ventricular dilatation also causes stretching of tricuspid annulus leading to severe tricuspid valve regurgitation. (WMV 1270 KB)
This patient underwent aortic valve replacement with tricuspid valve annuloplasty for bicuspid aortic valve stenosis with severe left ventricular dysfunction and congestive heart failure with mild right ventricular dysfunction. After tricuspid valve annuloplasty the longitudinal movement of tricuspid annulus is restricted and tricuspid annular plane excursion was low. Fractional area change is a more reliable indicator of right ventricular function in these settings. (WMV 1270 KB)
Rights and permissions
About this article
Cite this article
Varma, P.K., Jose, R.L., Krishna, N. et al. Perioperative right ventricular function and dysfunction in adult cardiac surgery—focused review (part 1—anatomy, pathophysiology, and diagnosis). Indian J Thorac Cardiovasc Surg 38, 45–57 (2022). https://doi.org/10.1007/s12055-021-01240-y
Received:
Revised:
Accepted:
Published:
Issue Date:
DOI: https://doi.org/10.1007/s12055-021-01240-y