Abstract
The case of a 17-year-old boy diagnosed with dilated cardiomyopathy in end-stage heart failure is described here. The patient sustained a cardiac arrest and was resuscitated with extracorporeal membrane oxygenation during cardiopulmonary resuscitation (ECPR). He was maintained on a peripheral veno-arterial extracorporeal membrane oxygenation (ECMO) for 7 days before undergoing a heart transplant. He was discharged 1 month after his transplant. The role of ECMO in ECPR and as a bridge to transplant has been highlighted.
Similar content being viewed by others
Avoid common mistakes on your manuscript.
Introduction
Extracorporeal membrane oxygenation (ECMO) has been well established as a treatment modality in patients suffering from post cardiotomy cardiogenic shock, primary graft dysfunction after heart transplant, rejection episodes in transplant recipients, and as a bridge to decision in heart failure patients [1, 2]. The use of veno-arterial (VA) ECMO during cardiopulmonary resuscitation (ECPR) has been associated with improved survival and favorable neurologic outcomes [3]. Also, ECMO has been used as a bridge to heart transplant [4]. Veno-arterial ECMO provides survival benefit in patients awaiting transplant [5]. Here, we describe a patient who underwent ECPR, was maintained on VA ECMO for 7 days before undergoing heart transplant surgery.
Case report
A 17-year-old boy (weight 40 kg; body surface area 1.34 m2) diagnosed with dilated cardiomyopathy was admitted to our institute with class IV symptoms of heart failure. His left ventricular ejection fraction was 15% and had a cardiac resynchronization therapy (CRT) device implanted 6 months earlier. While waiting for heart transplant, he sustained a cardiac arrest in the cardiac care unit. Cardiopulmonary resuscitation (CPR) was done as per Advanced Cardiovascular Life Support (ACLS) guidelines and after 20 min of CPR, there was return of spontaneous circulation. The patient was on intravenous dopamine, dobutamine, adrenaline, and noradrenaline 10, 10, 0.1, and 0.1 μg/kg/min, respectively. His heart rate was 140 bpm and systemic pressure was 80/40 mmHg with a systemic oxygen saturation of 90% on 100% FiO2. The femoral pulses were not palpable. Therefore, a surgical cut open was done and an intra-aortic balloon pump (IABP) was inserted through the left femoral artery. After initiation of IABP, the mean augmented pressure was 60 mmHg. The patient was shifted to the cardiac surgical intensive care unit (CSICU) for further management. The patient’s blood group was AB +ve and keeping in mind his universal recipient status, an ECMO (ROTAFLOW centrifugal pump, Maquet with phosphorylcholine-coated polymethylpentene membrane oxygenator) was primed with crystalloid solution and kept as standby. Ten minutes after shifting to the CSICU, the patient again developed cardiogenic shock. The rhythm became ventricular (wide QRS complexes) and the mean augmented pressure dropped to 40 mmHg. Resuscitation was again started. Another surgical cut down was done to expose right femoral vessels. A 15 Fr arterial cannula was inserted in the right femoral artery and a 21 Fr venous cannula was inserted in the left femoral vein to initiate the peripheral veno-arterial ECMO. The flows on ECMO varied between 1.5 and 2.0 L/min and the mean augmented pressures increased to 55–60 mmHg. The tip of the peripheral venous cannula was positioned in the right atrium with the help of echocardiography. The IABP was kept to unload the left ventricle (LV) while on ECMO. A distal perfusion cannula (5 Fr sheath) was introduced in the right femoral artery and connected to the 15Fr arterial cannula. There was excessive bleeding from the surgical sites and therefore heparin infusion was withheld for 3–4 h initially. The activated coagulation time (ACT) of the patient was monitored hourly and found to be always above 200 s. Twelve hours later, the flows started decreasing from 1.5 l progressively to 900 ml/min. The low flows were managed initially with volume administration but the flows kept on decreasing progressively. The ACT of the patient was checked and found to be 250 s but when the ACT of the ECMO circuit was checked, it was 150 s only. This provoked us to think about the clotting of circuit. The ECMO circuit was clamped transiently and cannulae were disconnected to reveal large clots in the circuit. The whole circuit was changed with a new one (primed with blood). The clots in the cannulae were removed using wall suction till there was a free flow of blood from cannulae. The distal perfusion cannula was aspirated with a 50 ml syringe to remove clots and was connected again to the arterial cannula with a new one way line. Following the exchange, the flows increased to 1.5 l/min. No untoward event happened during the exchange. Henceforth, the ACT of both patient and ECMO were checked and maintained above 200 s with infusion of unfractionated heparin. The following cutoffs were followed—platelet count >100,000/mm3, INR <2, apt 70–100 s, fibrinogen >150 mg/dl, and ACT 200–240 s.
After 18 h of initiating ECMO, the patient regained consciousness and was extubated 48 h later. He was kept nil per orally for 6 h and then oral fluids were allowed. The ECMO was continued for 7 days and the patient was kept on liquid diet. He was encouraged to do active exercise on bed. There was a slight increase in the liver enzymes and bilirubin level but his kidney functional was normal. The procalcitonin levels were 2.5 ng/ml.
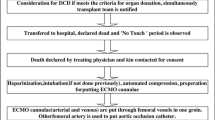
On day 8 of ECMO, he underwent heart transplant from a B negative donor. To perform the surgery, the circuit was disconnected from the ECMO oxygenator and connected to the reservoir and oxygenator of the CPB machine. The femoral venous cannula was pulled into the inferior vena cava at a level below the diaphragm (Fig. 1). A separate cannula was placed in the superior vena cava for upper body drainage. After surgery, the patient was decannulated and the femoral artery was repaired using a pericardial patch. Both the femoral site surgical wounds were closed with interrupted sutures. The IABP was left in place and removed the next day. As per institute protocol, no induction therapy was used in this patient before transplant.
In the postoperative period, the patient underwent re-exploration for increased mediastinal drainage. However, no surgical cause was found and the postoperative hemorrhage continued at 50 ml/h for 3 h. To stop this bleeding, 2 mg activated recombinant factor VII was administered. The postoperative bleeding stopped and the patient was extubated 20 h after the transplant.
For immunosuppression in the postoperative period, Cyclosporine, Mycophenolate Mofetil, and Prednisolone were used orally. Prophylaxis against Cytomegalovirus, Candida, and Pneumocystis jirovecii were given with oral Valganciclovir, Voriconazole, and Cotrimoxazole. For the initial 2 weeks, the levels of cyclosporine were maintained between 200 and 250 ng/ml against the conventional 300–350 ng/ml levels to avoid infection of the bilateral groin wounds. The levels were allowed to reach 300 ng/ml by third postoperative week. The total leukocyte count was maintained below the level of 10,000/ μl. His first two biopsies came negative for any rejection. The patient was discharged 1 month after his heart transplant.
Discussion
Extracorporeal membrane oxygenation has emerged as an efficient emergency tool for resuscitation of patients during cardiac arrest. Patients awaiting heart transplant often develop worsening of symptoms requiring hospital admission, diuretics, inotropic agents, implantation of pacemakers or combo devices (cardiac resynchronization therapy—defibrillators), IABP support, and mechanical ventilation. Because of shortage of donor hearts, some patients exhaust their therapeutic options while still waiting for a suitable heart. In such patients, ECMO serves as a bridge to transplant by providing additional circulatory support for 5–7 days and preserving end organ function [6]. In our patient, ECMO served both as an emergency resuscitating tool and as a circulatory support for 7 days till the heart transplant.
At our institute on an average, we receive a call about heart donor every 7–10 days. Because this patient was a universal recipient (blood group AB +ve), at the time of his cardiac arrest, we had primed and kept an ECMO at standby. We inserted an IABP in the cardiac care unit to stabilize the patient so that he can be shifted to the cardiac surgical ICU. Because of logistic reasons, it was not possible to initiate an ECMO in the cardiac care unit. In the cardiac surgical ICU as soon as the patient developed shock, arterial and venous cannula were inserted and the ECMO flow was initiated. At our institute, we assemble ECMO circuit using a ROTAFLOW centrifugal pump and polymethylpentene membrane oxygenator (EUROSETS s.r.l., Medolla, Italy) which requires some time to prime it. Because it is not practically feasible to keep an ECMO primed at all times, for emergency use, a system with less priming time is advantageous.
Another concern, while instituting ECMO during resuscitation, was the uncertain neurological status of our patient. The 2015 recommendations of American Heart Association state that in situations where it can be rapidly implemented, ECPR may be considered for selected patients for whom suspected etiology is potentially reversible and after conventional CPR of 10 min [7]. In our patient, the pathology was not reversible but a definite treatment was planned. In centers where heart transplant is done routinely at a fairly constant rate, such patients should be offered ECMO in case other resuscitation efforts fail. In case no organ was available, we would have opted for ventricular assist device.
We had used a 15 French arterial cannula and a 21 French venous cannula for establishing ECMO. Although as per the weight of the patient, they may seem to be smaller in size but we were able to achieve 1.5–2.0 l/min flows with these cannulae. With his failing heart, the cardiac output of our patient could not have been more than 2–2.2 l/min/m2 or about 2.5–3.4 l/min. Our target was to support 50% of this cardiac output with ECMO. Because with a peripheral VA ECMO, the afterload of the LV also increases and higher flows may impede left ventricular ejection. In a study by Bavaria et al., it was found that VA ECMO decreases wall stress of LV in normal hearts. However, in post ischemic hearts, there is an increase in LV wall stress with increase in flows of ECMO due to increased afterload [8]. To decrease the afterload of the LV and maintain efficient ejection, we left the IABP in situ while on ECMO. IABP has been used in conjunction with ECMO to reduce LV afterload [9]. The presence of IABP also provides pulsatile flow and counters the anti-diuretic effect of the nonpulsatile flow of ECMO. In our patient, no diuretics were required after the first day of ECMO. The IABP was removed 24 h after the heart transplant surgery.
Postoperative bleeding is a common complication of ECMO. Surgical insertion of cannulae is associated with more bleeding in comparison to percutaneous insertion of cannulae. In our patient, there was substantial bleeding from cannula insertion sites. Therefore, heparin infusion was withheld initially to prevent excessive bleeding. In our hospital, we use phosphorylcholine-coated polymethylpentene oxygenator (EUROSETS s.r.l., Medolla, Italy) in the ECMO circuit but the tubings of the ECMO circuit are not coated (routine tubings used during CPB are used in our assembled ECMO circuit). This may be the reason for clotting of the circuit later on. To prevent clotting of the second circuit, we maintained ACT of the circuit more than 200 s at all times. Intra-operatively, the ACT was maintained between 480 and 600 s. The excessive bleeding in the postoperative period was attributed to heparin-induced coagulopathy and was treated with fresh frozen plasma and platelet concentrates. As per our previous experience and institute protocol, recombinant-activated factor VII was given, only after one negative mediastinal re-exploration, in a dose of 32.71 μg/kg [10]. Platelet count is important for the action of recombinant-activated factor VII [10]. The platelet count in our patient at the time of rFVIIa administration was 81,000/mm3.
Prevention of infection in a patient on ECMO is of paramount importance. In our patient, we extubated the patient after 48 h to prevent ventilator-associated pneumonia. Intravenous Cefoperazone with Sulbactum and Teicoplanin were given throughout the duration of ECMO for prophylaxis. To prevent urinary tract infection, Foleys catheter was removed on day 2 of ECMO and an external urinary catheter (condom catheter) was placed. Infection surveillance was done by repeatedly sending cultures of blood, urine, endotracheal tube secretions, and intercostal chest tube. No evidence of infection was found till the time of patient’s discharge.
Also, as per our institute protocol, we did not use any induction therapy before transplant. But centers where it is routinely used, it may be beneficial to the patient to withhold it because it may predispose the recipient to severe infections, especially one who has multiple surgical wounds.
In conclusion, ECMO is an effective modality to provide circulatory support during resuscitation end-stage heart failure patients and can be extended to serve as a bridge to transplant in centers where heart transplant surgery is done in a regular predictable manner.
References
Kittleson MM, Patel JK, Moriguchi JD, et al. Heart transplant recipients supported with extracorporeal membrane oxygenation: outcomes from a single-center experience. J Heart Lung Transplant. 2011;30:1250–6.
Rousse N, Juthier F, Pinçon C, et al. ECMO as a bridge to decision: recovery, VAD, or heart transplantation? Int J Cardiol. 2015;187:620–7.
Shin TG, Choi JH, Jo IJ, et al. Extracorporeal cardiopulmonary resuscitation in patients with inhospital cardiac arrest: a comparison with conventional cardiopulmonary resuscitation. Crit Care med. 2011;39:1–7.
Gedik E, Ulaş A, Ersoy Ö, Atar F, Camkıran Fırat A, Pirat A. Venoarterial extracorporeal membrane oxygenation support as a bridge to heart transplant: report of 3 cases. Exp Clin Transplant. 2016;14:121–4.
Jasseron C, Lebreton G, Cantrelle C, et al. Impact of heart transplantation on survival in patients on venoarterial extracorporeal membrane oxygenation at listing in France. Transplantation. 2016;100:1979–87.
Poptsov VN, Spirina EA, Saitgareev RS, Zakharevich VM, Eremeeva OA, Masyutin SA. Peripheral veno-arterial ECMO as a bridge to heart transplantation: outcomes from a single-centre experience. J Heart Lung Transplant. 2014;33:S247–8.
Brooks SC, Anderson ML, Bruder E, et al. Part 6: alternative techniques and ancillary devices for cardiopulmonary resuscitation: 2015 American Heart Association guidelines update for cardiopulmonary resuscitation and emergency cardiovascular care. Circulation. 2015;132:S436–43.
Bavaria JE, Ratcliffe MB, Gupta KB, Wenger RK, Bogen DK, Edmunds LH Jr. Changes in left ventricular systolic wall stress during biventricular circulatory assistance. Ann Thorac Surg. 1988;45:526–32.
Petroni T, Harrois A, Amour J, et al. Intra-aortic balloon pump effects on macrocirculation and microcirculation in cardiogenic shock patients supported by venoarterial extracorporeal membrane oxygenation. Crit Care med. 2014;42:2075–82.
Singh SP, Chauhan S, Choudhury M, Malik V, Choudhary SK. Recombinant activated factor VII in cardiac surgery: single-center experience. Asian Cardiovasc Thorac Ann. 2014;22:148–54.
Author information
Authors and Affiliations
Corresponding author
Ethics declarations
Conflict of interest
All authors declare that they have no conflict of interest and do not receive any research grants from any company, have not received a speaker honorarium from any company, do not own any stock in any company and are not members of a committee.
Funding
The study did not receive any funding.
Ethical approval
All procedures performed in this study were in accordance with the ethical standards of the Institutional and National Research Committee and with the 1964 Helsinki Declaration and its later amendments or comparable ethical standards.
Informed consent
Informed consent was obtained from the patient included in this study.
Rights and permissions
About this article
Cite this article
Singh, S.P., Bansal, A., Parakh, N. et al. First successful experience of ECPR to heart transplant at a tertiary care institute. Indian J Thorac Cardiovasc Surg 34, 150–153 (2018). https://doi.org/10.1007/s12055-017-0563-5
Received:
Revised:
Accepted:
Published:
Issue Date:
DOI: https://doi.org/10.1007/s12055-017-0563-5