Abstract
Perioperative neurocognitive disorders (PNDs) are now considered the most common neurological complication in older adult patients undergoing surgical procedures. A significant increase exists in the incidence of post-operative disability and mortality in patients with PNDs. However, no specific treatment is still available for PNDs. Recent studies have shown that exercise may improve cognitive dysfunction-related disorders, including PNDs. Neuroinflammation is a key mechanism underlying exercise-induced neuroprotection in PNDs; others include the regulation of gut microbiota and mitochondrial and synaptic function. Maintaining optimal skeletal muscle mass through preoperative exercise is important to prevent the occurrence of PNDs. This review summarizes current clinical and preclinical evidence and proposes potential molecular mechanisms by which perioperative exercise improves PNDs, providing a new direction for exploring exercise-mediated neuroprotective effects on PNDs. In addition, it intends to provide new strategies for the prevention and treatment of PNDs.
Similar content being viewed by others
Avoid common mistakes on your manuscript.
Introduction
Perioperative neurocognitive disorders (PNDs) are associated with cognitive changes after anesthesia and surgery, particularly in older adults. They are defined as alterations in neuropsychiatric function that occur in the perioperative period, including preoperative cognitive impairment, postoperative delirium (POD), delayed neurocognitive recovery (dNCR), and postoperative cognitive dysfunction (POCD) [1]. PNDs can significantly prolong patient hospitalization and increase post-operative patient disability and mortality and aggravate the burden of patient and family medical care, leading to serious social problems [2].
In the latest recommendations, PNDs are classified into several different stages based on specific time intervals [1]. Specifically, POD refers to neuropsychiatric disorder characterized by inattention, disorganized thinking, and altered levels of consciousness, which is associated with cognitive impairment and commonly diagnosed in the first week following surgery. The term “dNCR” refers to cognitive dysfunction within 30 days after the procedure. POCD is defined as neurocognitive disorders during the period from 30 days postoperatively to 12 months. The incidence of POD is between 5.1 and 30.3% in patients who undergo different procedures [3,4,5]. Multiple studies have shown that the incidence of dNCR after major non-cardiac surgery is approximately 25–34.5%. However, most of the patients with early post-operative cognitive decline recover over time, and only one-fifth to one-third develop POCD during follow-up [6, 7]. Unfortunately, no existing drugs can effectively treat this disorder because its mechanism remains unclear. Animal and human studies have proposed several hypotheses about the pathophysiology of PNDs and have developed novel treatments based on these hypotheses [8]. However, currently, available treatment options are limited and appear unable to reduce the mortality and incidence rate of PNDs. Furthermore, studies have shown that physical activity prevents and reduces cognitive impairment and improves cognitive function [9]. Therefore, non-pharmacological treatment options, such as exercise, are promising alternative intervention strategies for preventing and treating PNDs in older adults. This works through the inhibition of neuroinflammation, regulation of gut microbiota, maintenance of skeletal muscle mass, amelioration of mitochondrial dysfunction, and modulation of synaptic plasticity. This review summarizes recent progress in exercise and PNDs to provide a theoretical basis and potential molecular mechanism for preventing and treating PNDs and evidence for developing relevant clinical trials.
Exercise Decrease the Risk and Severity of POD
Preoperative exercise capacity as an independent predictor of POD has been demonstrated in elective cardiac surgery. Ogawa et al. [10] found that the 6-minute walking distance (6MWD) test results can be used for predicting incidence. The cut-off value of 6MWD determined by the receiver operating characteristic (ROC) curve was 345 m. Therefore, POD prevention may be achieved by improving the outcome of 6MWD during preoperative rehabilitation exercises. In another retrospective study, preoperative low physical activity was suggested in patients with gastrointestinal cancer as a predictor of POD, independent of confounding factors [11]. Similarly, preoperative low skeletal muscle mass (LSMM) [12] and exercise intensity [13] are associated with POD in older adult patients undergoing colorectal cancer (CRC) surgery. Patients with LSMM can be identified based on gender and skeletal muscle index (SMI) by assessing the cross-sectional area of skeletal muscle at the third lumbar vertebra (L3) level on computed tomography (CT) [14]. LSMM was associated with POD based on multivariate analysis, and a significantly stronger association was found in patients who were malnourished or physically dependent and undergoing CRC surgery. Additionally, patients with sarcopenia have a higher risk of developing delirium after a major thoracolumbar spine surgery [15]. A retrospective study explored the relationship between skeletal muscle mass and POD in patients undergoing surgery for head and neck cancer, and a decrease in SMI was found to be a significant independent risk factor for hypoactive and mixed-type POD in these patients [16]. Preventing such POD may be possible in free flap repair for oral cancer by increasing skeletal muscle mass preoperatively through exercise and nutritional therapy. Lee et al. showed that in patients undergoing elective orthopedic surgery, regular preoperative exercise significantly reduced the risk of POD and was associated with the severity of POD in a secondary analysis of prospective studies. Interestingly, the effects of exercise on POD appeared to have significant gender differences [17]. According to the above studies (Table 1), the skeletal muscle mass and preoperative exercise capacity can be improved by proper preoperative exercise to prevent POD in elderly patients. Furthermore, determining the preoperative exercise capacity to predict and prevent POD is an essential novel research direction.
Mechanisms of Exercise Interventions for POD and POCD
The common mechanism of cognitive dysfunction is irreversible neuronal loss and dysfunction. Currently, the known factors contributing to PNDs include neuroinflammation, mitochondrial dysfunction, and reduction of brain-derived neurotrophic factors (BDNF). In preclinical studies, exercise has a significant positive impact on PNDs by regulating neuroinflammation, gut microbiota, skeletal muscle, mitochondria, and synapses (Table 2).
Neuroinflammation
The body’s innate immune system, as the primary defense system, is vital for fighting infections and exogenous pathogens. Nevertheless, in the absence of infection, the innate immune system may be triggered by endogenous danger signals, such as damage-associated molecular patterns (DAMPs) [22]. When the immune system identifies an exogenous or endogenous trigger, immune cells recognize and eliminate them through cytokine release, antigen presentation, and phagocytosis [23, 24]. DAMPs can be activated to act on pattern recognition receptors (PRRs) to activate the intrinsic immune system after aseptic mechanical injuries such as a surgical operation, which in turn causes a multi-protein signal transduction cascade response and secretion of pro-inflammatory factors. Activated macrophages can penetrate across the damaged blood–brain barrier (BBB) and further produce inflammatory cytokines in the hippocampus, resulting in neuroinflammatory responses and neuronal cell injury [25]. An over-activated immune system may lead to chronic neuroinflammation, thus adversely impacting the central nervous system (CNS).
As immune cells in the CNS, microglia can differentiate into two types after being activated: M1 phenotype and M2 phenotype. “M1 microglia” mainly produce pro-inflammatory cytokines to exert neurotoxic effects, such as interleukin-1β (IL-1β). Conversely, “M2 microglia” are critically involved in the anti-inflammatory response and promote tissue homeostasis and extracellular matrix reconstruction [26]. Some neurodegenerative diseases, however, cause chronic neuroinflammatory conditions by adversely activating glial cells due to persistent pathological formations [27, 28]. Owing to the “non-specific” innate immune system, such chronic inflammation and overactivation of glial cells have been classified as detrimental processes. It has been shown that these responses cause damage to other surrounding neurons as well as glial cells, delaying the recovery of disease [29].
After peripheral surgery, multiple humoral and neural pathways modulate the interactions between the immune response and the brain. Various cytokines secreted from the periphery enter the CNS across the disrupted BBB to activate microglia [30]. Furthermore, in a prospective cohort study of patients undergoing non-intracranial surgery, it was observed that a peripheral inflammatory response that increased with the degree of surgical trauma was able to exacerbate breakdown of the BBB and thereby induce POD [31]. In addition, in another clinical study, patients diagnosed with POD after undergoing elective spine surgery had higher levels of pro-inflammatory cytokines compared to non-POD patients [32]. In a preclinical study, not only was the inflammatory response exacerbated in the periphery and hippocampus, but behavioral tests performed poorly with increasing time the mice underwent surgery [33]. Surgical stress can alter the dynamic balance of microglia activation by shifting to the M1 phenotype, creating a vicious cycle of neuroinflammatory progression and inducing consequent cognitive dysfunction [34, 35]. Importantly, modulation of neuroinflammation not only attenuates POD-like behavior induced by anesthesia and surgery in elderly mice [36] but also prevents the development of POD in older adult patients undergoing non-cardiac surgery [37].
Exercise has been found to have benefits for neurodegenerative diseases and cognitive function by influencing markers of inflammation systemically, including the CNS. It is noteworthy that the impact on peripheral inflammatory factors varies depending on the type of exercise. In clinical study, endurance exercise reduces levels of proinflammation in the periphery, while resistance and concurrent exercise only decrease TNF-α levels, which may be linked to a reduction in adiposity [38]. In preclinical studies, short- and long-term free wheel running exercise decreased IL-6 levels in the CNS in aged mice [39]. Short-term resistance training inhibits the activation of microglia and astrocytes in the hippocampus in Alzheimer’s disease (AD) mice. It also reduced pro-inflammatory cytokine levels and increase the level of anti-inflammatory mediators in the brain, thereby improving cognitive function in AD mice [40].
Treadmill exercise induces microglial M1-to-M2 polarization shift in APP/PS1 mice, which in turn inhibits pro-inflammatory response and promotes anti-inflammatory response, improving cognitive dysfunction in mice through suppression of the neuroinflammatory response [41]. In a separate study, compared with high-capacity runner (HCR) rats, low-capacity runner (LCR) rats undergoing isoflurane anesthesia and experiencing tibia fracture with internal fixation exhibited excessive cognitive impairment at 3 days and at 3 months postoperatively, which could be improved by preoperative treadmill exercise lasting 6 weeks. Furthermore, treadmill training in LCR rats significantly attenuates the increase in protein and mRNA expression of pro-inflammatory cytokines in post-operative LCR rats [18]. Similarly, an additional preclinical study showed that anesthesia and surgery increased microglia activation [42] and pro-inflammatory cytokines in the hippocampus, and exercise attenuated this increase [19]. These results reveal that exercise can modulate neuroinflammatory responses on CNS and can reduce the risk of suffering from PNDs.
Gut Microbiota
Gut microbes are microorganisms that exist in the gastrointestinal system in a symbiotic relationship [43]. The gut microbiota communicates with the brain in a bidirectional manner through multiple pathways, thereby establishing the gut–brain axis, which has recently been shown to play a critical role in many neurological disorders [44]. In a microbial community, the α diversity index represents species richness and the relative abundance. The β diversity index estimates the diversity of species in different environments and indicates species’ response to the environment. Several taxa have been revealed to be involved in altered cognitive function in the gut microbiota. The genus Streptococcus serves an essential role in causing neurological damage and is also a risk factor for cognitive decline [45]. As an essential member of the gut microbiota, Lachnospiraceae may improve cognitive impairment and inflammatory responses in the hippocampus by producing metabolites [46]. Moreover, decreased abundance of Trichophytonaceae in the gut microbiota is correlated with a higher frequency of cognitive impairment [47].
Alterations in gut microbiota composition are involved in mice’s anesthesia and surgery-induced cognitive impairment. Liu et al. observed that aging mice exhibited more significant POD-like behavior after undergoing anesthesia and surgery compared to young mice. This appears to be related to a more significant reduction in the relative abundance of Lactobacilli in the gut microbiota of elderly mice. By feeding probiotic not only improved the inflammatory response in the hippocampus but also improved cognitive function after anesthesia and surgery in aging mice [48]. In sevoflurane-treated young mice, Lachnospiraceae exhibited an increase in relative abundance, whereas Trichophytonaceae exhibited a decrease in relative abundance [49]. In a prospective clinical study, it was concluded by analyzing the gut microbiota of elderly patients after surgery, in which Parabacteroides distasonis was associated with POD. However, Prevotella and Colinella were not statistically associated with the occurrence of POD [50]. This appears to imply that alterations of gut microbiota diversity are influenced by factors such as age, species, and mode of intervention. Therefore, identifying PNDs may be possible through quantitative analysis of specific intestinal bacteria and will facilitate the development of new therapeutic strategies based on these findings.
Exercise can induce neurochemical changes in the brain by modulating the gut microbiota. Voluntary exercise ameliorates high-fat diet-induced cognitive dysfunction by elevating the relative abundance of Lactobacillus, and Eubacterium nodatum in the intestinal flora of mice [51]. Similarly, in APP/PS1 mice, persistent treadmill exercise for 12 weeks increased the diversity of the intestinal flora and also increased the relative abundance of probiotics thereby declining AD-associated pathological markers [52]. Furthermore, in a randomized controlled trial, 12 weeks of moderate-intensity training modulated the abnormal composition of gut microbiota and improved depressive symptoms [53]. Therefore, regulating the gut microbiota through exercise is a promising therapeutic direction to ameliorate diseases caused by abnormal disorders of gut bacteria.
Exercise can ameliorate the adverse impact of anesthesia and surgery on cognitive function through the modulation of gut flora metabolites. Short-chain fatty acids (SCFAs) are products of the gut microbiota [54]. The concentration of valeric acid, a SCFA, increased in the blood of mice undergoing anesthesia and surgery, and preoperative exercise can attenuate this increase [19]. Brain structural modifications, such as neurogenesis and synaptic structure, are often necessary for learning and memory [55]. The intraperitoneal administration of valeric acid reversed exercise’s beneficial impact on mice’s cognitive performance after anesthesia and surgery. Moreover, the decrease in pro-inflammatory cytokines, increase in brain cell genesis, and improvement in synaptic plasticity after anesthesia and surgery caused by exercise were also attenuated by intraperitoneal injection of valeric acid [19]. In general, these findings reveal that valeric acid, derived from gut microbiota, significantly promoted PND progression, which could be addressed through exercise.
Skeletal Muscle Mass
Sarcopenia is a degenerative change in skeletal muscle mass and strength with age, resulting in reduced muscle physiology [56]. Approximately 10–40% of people over the age of 60 years suffer from sarcopenia [57]. Sarcopenia may lead to adverse clinical outcomes, decreased self-care ability, and mortality [58]. The current literature indicates a strong correlation between sarcopenia and neurodegeneration [59], such as AD [60] and brain atrophy [61]. Moreover, POD is associated with muscular atrophy caused by sarcopenia [12].
A kind of neurotrophic factor, BDNF, promotes neurogenesis and regulates synaptic plasticity [62]. Specifically, BDNF performs multiple functions by binding to its tropomyosin receptor kinase B (TrkB); these functions include supporting neuronal survival and growth, affecting synaptic transmission, enhancing neurogenesis, and altering synaptic plasticity [63]. Skeletal muscle has been found to be a secretory organ that is a major source of BDNF [59]. Furthermore, exercise increases the level of BDNF according to previous studies [64], and BDNF functions with exercise to promote hippocampal neurogenesis and improve cognitive decline in mice [65]. Treatment with TrkB inhibitors blocked exercise’s beneficial effects in Parkinson’s disease (PD) rats [66]. However, it is unclear how muscle-derived BDNF crosses the BBB to affect the brain. FNDC5 is a muscle protein induced by exercise that can be cleaved and converted into iridin [67]; interestingly, the expression of BDNF increases when irisin is upregulated in primary cortical neurons, whereas it is reduced when FNDC5 is knocked down with RNAi [68]. Furthermore, hippocampal BDNF and other neuroprotective genes were increased due to the elevated expression of FNDC5 and irisin in peripheral blood [68]. In addition, exercise induces an increase in myokine and cathepsin B, which can be released into the peripheral blood and cross the BBB to increase protein and mRNA expression of BNDF in the hippocampus [69].
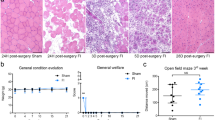
Resistance exercise prevents the decline in BDNF and improves POCD in aged mice undergoing anesthesia and surgery, indicating that BDNF is important in regulating the beneficial effects of exercise on POCD [20]. Nemoto et al. reported a low skeletal muscle mass animal model by suspending the rats’ tail for 2 weeks without allowing the hind limbs to touch the ground [21]. The analysis excluded rats who tried climbing their own tails due to insufficient muscle atrophy. In this experiment, the MWM and fear conditioning test results demonstrated that rats with low skeletal muscle mass undergoing anesthesia and surgery showed cognitive decline. Additionally, inhibition of the proliferation of immature nerves in the hippocampal dentate gyrus and a reduction in BDNF were also revealed. Thus, maintaining optimal muscle strength and mass through preoperative exercises is important to prevent the occurrence of PNDs.
Mitochondria
Mitochondria increase in number through biogenesis and fusion processes, thereby increasing their capacity for energy supply and Ca2+ handling [70]. However, fission and mitophagy occur when mitochondria are excessive or dysfunctional to maintain cellular metabolic homeostasis and mitochondrial health [71]. Mitofusin-1/2 (Mfn1/2) and optical atrophy protein 1/2 (Opa1/2) are core proteins in the mitochondrial fusion mechanism; they can promote the fusion of the outer and inner mitochondrial membranes, respectively [72]. Proteins, dynamin-related protein 1 (Drp1), and fission protein 1 (Fis1) combine to complete mitochondrial fission, ultimately leading to contraction and cleavage of mitochondrial segments for clearance [73]. Mitophagy, which is more efficient when fission occurs [74], mediates the removal of damaged mitochondria through autophagy and lysosomal degradation, thus ensuring intracellular mitochondrial quality.
Increased release of reactive oxygen species (ROS) and cell death–related factors caused by impaired mitophagy mechanism play an important role in neurodegenerative diseases [75]. Increased ROS resulting from mitochondrial dysfunction can over-activate microglia to cause neuroinflammation and apoptosis [76]. Cognitive dysfunction induced by chronic cerebral underperfusion in rats is mainly attributed to increased ROS and neuroinflammation due to mitochondrial dysfunction, and this pathological process was reversed by stabilizing mitochondrial function and promoting mitochondrial biogenesis [77]. Anesthesia and surgery promote ROS accumulation and inhibit energy metabolism in the brain of aging mice, primarily by disrupting the balance of mitochondrial dynamics and altering mitochondrial ultrastructure [78]. Similarly, the activation of mitochondrial fission caused by anesthesia and surgery resulted in increased mitochondrial fragmentation in the hippocampus of aged mice [42].
Several studies have shown that exercise may increase the number of mitochondria and improve oxidative phosphorylation and respiratory capacity [79, 80]. Mice receiving swim training showed improved cognitive function, inhibited oxidative stress, and increased expression of Mfn1/2 and Drp1 compared to untrained mice [81]. In another study, 12 weeks of treadmill exercise increased mitochondrial fusion proteins and mitochondrial autophagy proteins and inhibited fission-related proteins, resulting in improved mitochondrial respiratory activity and reduced apoptotic signaling in the cerebral cortex and cerebellum [82]. Transplantation of plasma from long-term exercised mice into AD mice improves spatial memory and learning performance by improving mitochondrial function and inhibiting apoptosis in the brain, which appeared to correlate with high levels of BDNF in the plasma of exercised mice [83]. In summary, all the above results indicate that exercise can maintain brain health by improving mitochondrial dynamics.
Four weeks of preoperative resistance exercise in mice improved cognitive dysfunction induced by laparotomy [20]. Moreover, preoperative resistance exercise reversed the hippocampal mitochondrial defects induced by laparotomy in aged mice. Furthermore, anesthesia and surgery can increase Mfn-2 levels in the hippocampus, which can be prevented by resistance exercise, suggesting that resistance exercise also ameliorates post-operative cognitive impairment in aged mice by moderating mitochondrial dynamics [20].
Synapse
The synapse is where neurons transmit information to each other, which is primarily mediated by neurotransmitters [84]. Dendritic spines protrude from the dendritic shaft, the main site of synaptic plasticity [85]. Synaptic plasticity involves the formation of new spines, elimination of spines, and modifications to the shape of spines [86]. Changes caused by synaptic plasticity may also affect the number of neurotransmitter receptors, thereby altering the strength of signaling to neurotransmitters [87]. Dendritic arborization and spine density form the morphological and structural basis of synaptic plasticity, which is closely correlated to cognitive function [88]. Therefore, the disruption of synaptic plasticity and abnormal spine morphology is often observed in various neurocognitive disorders [89]. Long-term potentiation (LTP), widely considered a biological mechanism of learning and memory, generally refers to the strengthening of synapses [90]. Extensive research proved that long-term depression (LTD) is closely associated with multiple neurodegenerations. Dysregulation of physiological mechanisms between LTD and LTP may lead to cognitive decline, particularly learning and memory deficits. Nevertheless, basal levels of LTD in the hippocampus remain essential for normal cognitive function [91].
N-Methyl-D-aspartate receptor (NMDAR) plays a crucial role in synaptic plasticity and cognitive function [92]. For instance, long-term memory is formed by NMDAR-dependent LTP in the hippocampus. As a general rule, NMDAR is present in the presynaptic and postsynaptic sites of dendritic spines, where they are closely associated with regulating glutamate release, LTP, and synaptic plasticity [93, 94]. Extrasynaptic NMDAR is detected on the spine neck, dendritic shaft, or close to the mitochondria. The activation of the extrasynaptic NMDAR causes loss of mitochondrial membrane potential and induces Ca2+ neurotoxicity, ultimately resulting in LTD, spinal atrophy, synaptic loss, and apoptosis [93, 95]. Surgical incision–induced pain stimulation appears to have effects on learning and memory functions via NMDA receptor 2B. Painful stimuli induced by surgical trauma decreased the level of cortical NMDA receptor 2B in mice and improved POCD due to painful stimuli by increasing the level of this receptor [42]. This seems to point out that different subtypes of NMDA receptors are performing different roles in cognitive functions.
Increasing evidence suggests that physical exercise improves synaptic plasticity and learning memory impairment in AD models through different pathways [96, 97]. It has been shown that long-term voluntary exercise effectively raises the number of dendritic spines and the level of PSD-95 protein in the hippocampus of mice with AD by inhibiting the abnormal phagocytosis of synapses induced by microglia activation [98]. Interestingly, low-intensity continuous treadmill exercise induced the expression of NMDA receptor 2B in the rat hippocampus, which was suppressed in the high-intensity continuous treadmill exercise group [99]. Resistance exercise prevents the decline of dendritic process complexity and spine density in the hippocampus in POCD animal models, resulting in improved synaptic plasticity and cognitive function in mice [20]. Furthermore, resistance exercise also prevents surgery-induced NMDAR activation [20].In a separate study, appropriate treadmill exercise also reversed the decrease in dendritic branches and spine density in mice undergoing anesthesia and surgery and thus improved post-operative cognitive dysfunction [19].
The benefits of exercise are not only confined to the skeletal muscle but involve the modulation of the gut microbiota, stimulation of neurotrophic factors, maintenance of mitochondrial homeostasis alleviation of neuroinflammation, and improvement in neuroplasticity as well, causing changes in the CNS at the anatomical, cellular, and molecular levels (Fig. 1).
Molecular mechanisms through which exercise may affect cognitive function. Surgical procedures can activate damage-associated molecular patterns (DAMPs), further activating macrophages. Activated macrophages can secrete cytokines through the damaged BBB, further leading to microglia activation in the hippocampus. After being activated, microglia can be divided into M1 and M2 phenotypes. M1-type microglia produce pro-inflammatory cytokines to damage neurons. M2-type microglia secrete anti-inflammatory cytokines participating in tissue repair and extracellular matrix reconstruction. Surgical trauma makes microglia develop M1 polarization, leading to a vicious circle of neuroinflammation progression. Exercise can promote microglia development in M2 polarization and inhibit the level of pro-inflammatory cytokines to promote neuronal recovery. Exercise can inhibit the production of valeric acid by altering the diversity of gut microbiota. Valeric acid produced by gut microbiota inhibited neurogenesis, reduced the dendritic branches and spine density, and increased the production of pro-inflammatory cytokines in the hippocampus. At the same time, exercise can also increase skeletal muscle mass, secrete the muscle factor irisin, and release it into the peripheral blood. Irisin crosses the BBB to promote the production of BDNF and thus induce neurogenesis. Furthermore, exercise regulates mitochondrial dynamics in the hippocampus, thus ensuring mitochondrial quality and reducing mitochondrial abnormalities. Finally, exercise modulates synaptic plasticity by acting on NMDA receptors at the synapse
Appropriate Exercise in the Perioperative Period
Poor physical performance increases mortality and post-operative complications and delays in recovery after surgery [100]. Several clinical studies have shown the beneficial effect of preoperative exercise on post-operative outcomes, including hospital stay, mortality, and complications. Considerable evidence exists which demonstrates improved preoperative physical performance through preoperative exercise, resulting in reduced mortality and complications after major cardiovascular and thoracic surgery [101]. In contrast, Carli et al. reported that patients who completed a more intense exercise program before surgery had worse outcomes [100].
Different types of exercise performed by individuals may have different cognitive outcomes. Exercise includes aerobic training and resistance training. Aerobic training can enhance cardiopulmonary function, while resistance exercise can improve skeletal muscle quality. However, both aerobic and resistance training can improve cognition and enhance brain function in older adults [102, 103]. Six months of moderate-intensity aerobic exercise significantly reduced the Alzheimer’s disease Assessment Scale—Cognition (ADAS-Cog) growth score in older adults [104]. In human studies, the effect of aerobic exercise on BDNF is contradictory. Some studies reported that aerobic exercise promoted the expression of BDNF, while others found no changes in BDNF [105]. This appears to be related to the measurement time between BDNF and aerobic exercise, exercise frequency, exercise intensity, age, and gender. Training with adjustable resistance equipment for 12 weeks along with regular exercise improves general learning and memory in older adults with subjective cognitive impairment [106]. The molecular and biological mechanisms of resistance training that help to enhance cognitive function may be different from those of aerobic training. Both aerobic training and resistance exercise improved learning and memory in adult male rats. However, aerobic training preferentially increases BDNF, while resistance training preferentially increases insulin-like growth factor-1 (IGF-1) in the hippocampus [107]. In human studies, hippocampal volume showed a significant increase after aerobic training in older women suffering from probable MCI, whereas resistance exercise failed to do so [108]. Multicomponent exercise might be an effective strategy for preventing cognitive decline and executive dysfunction [109]. In recent literature, a non-linear dose–response relationship exists between overall exercise and cognition, and many types of movement may have clinically important effects at lower doses [110]. A randomized controlled trial has shown that among older adult patients undergoing anesthesia for unilateral total hip replacement, post-operative cognitive therapy combined with rehabilitation exercise has a protective impact on cognitive function compared with the control group [111]. Notably, some types of exercise do not affect cognition, such as cycling and resistance and balance exercise [110]. Although exercise is not suitable for all patients, particularly those with fractures or movement limitations, there are still benefits to be obtained by exercising at the earliest possible time. In summary, both aerobic and resistance exercises have shown great potential in enhancing cognition and improving brain function (Fig. 2).
Impact of different types of exercise on the brain. In animal studies, swimming and running have been shown to reduce pro-inflammatory cytokines and regulate gut microbiota, thereby improving post-operative cognitive function. In human studies, walking, multicomponent exercise, and resistance exercise can prevent cognitive decline. Rehabilitation exercise has a protective effect on post-operative cognitive function in elderly patients
Conclusion
This review summarized current clinical evidence of perioperative exercise in improving PNDs and the potential mechanisms by which exercise may influence PNDs. Exercise has been proven to be good for overall health, and each part of the body benefits from different types of exercise, such as aerobic or resistance exercise. Increasing evidence shows that exercise has a beneficial effect on cognitive improvement and brain health [112, 113]. Physical exercise can also reduce anxiety [114] and depression [115]. Moreover, not only does physical exercise reduce the risk of dementia [109], but it also appears to be important in treating the disease [116]. In a separate study, the cognitive decline with age in healthy individuals and those with neurodegenerative diseases was suppressed by regular exercise [117]. Thus, much study-based evidence shows that exercise has a sustained and specific neuroprotective effect.
These studies used animal models to explain the potential benefits of exercise on PNDs. Animal models have contributed to elucidating neuroprotective molecular pathways activated through exercise, suggesting neuroinflammation, synaptic plasticity, and BDNF as key pathways capable of attenuating the phenotypes of neurodegenerative diseases. Nevertheless, only a clearer understanding of the mechanisms by which exercise interventions mediate neuroprotection will allow the design of strategies to prevent PNDs.
Not all levels and type of exercise are beneficial, although exercise can increase the physiological capacity of the heart and skeletal muscle and may improve post-operative complications in older patients as well as the quality of life in patients with PNDs owing to the difference in everyone’s exercise capacity; thus, an individualized exercise program is necessary to maximize the benefits of exercise. In the future, designing reasonable clinical trials, particularly multicenter prospective randomized controlled trials with large samples, is necessary to verify the role of different perioperative exercise in PNDs and its potential benefits on post-operative recovery of older adult patients, which will help to develop more reasonable perioperative exercise strategies.
Data Availability
Not applicable
References
Evered L, Silbert B, Knopman DS, Scott DA, DeKosky ST, Rasmussen LS, Oh ES, Crosby G et al (2018) Nomenclature consensus working, recommendations for the nomenclature of cognitive change associated with anaesthesia and surgery-2018. Br J Anaesth 121(5):1005–1012. https://doi.org/10.1016/j.bja.2017.11.087
Eckenhoff RG, Maze M, Xie Z, Culley DJ, Goodlin SJ, Zuo Z, Wei H, Whittington RA et al (2020) Perioperative neurocognitive disorder: state of the preclinical science. Anesthesiology 132(1):55–68. https://doi.org/10.1097/ALN.0000000000002956
Gill SS (2022) In older adults having hip fracture surgery, regional vs. general anesthesia did not reduce postoperative delirium. Ann Intern Med 175(5):JC53. https://doi.org/10.7326/J22-0027
Evered LA, Chan MTV, Han R, Chu MHM, Cheng BP, Scott DA, Pryor KO, Sessler DI et al (2021) anaesthetic depth and delirium after major surgery: a randomised clinical trial. Br J Anaesth 127(5):704–712. https://doi.org/10.1016/j.bja.2021.07.021
Aoki Y, Kurita T, Nakajima M, Imai R, Suzuki Y, Makino H, Kinoshita H, Doi M et al (2023) Association between remimazolam and postoperative delirium in older adults undergoing elective cardiovascular surgery: a prospective cohort study. J Anesth 37(1):13–22. https://doi.org/10.1007/s00540-022-03119-7
Moller JT, Cluitmans P, Rasmussen LS, Houx P, Rasmussen H, Canet J, Rabbitt P, Jolles J et al (1998) Long-term postoperative cognitive dysfunction in the elderly ISPOCD1 study. ISPOCD investigators. International Study of Post-Operative Cognitive Dysfunction. Lancet 351(9106):857–861. https://doi.org/10.1016/s0140-6736(97)07382-0
Monk TG, Weldon BC, Garvan CW, Dede DE, van der Aa MT, Heilman KM, Gravenstein JS (2008) Predictors of cognitive dysfunction after major noncardiac surgery. Anesthesiology 108(1):18–30. https://doi.org/10.1097/01.anes.0000296071.19434.1e
Jin Z, Hu J, Ma D (2020) Postoperative delirium: perioperative assessment, risk reduction, and management. Br J Anaesth 125(4):492–504. https://doi.org/10.1016/j.bja.2020.06.063
Rossi PG, Carnavale BF, Farche ACS, Ansai JH, de Andrade LP, Takahashi ACM (2021) Effects of physical exercise on the cognition of older adults with frailty syndrome: a systematic review and meta-analysis of randomized trials. Arch Gerontol Geriatr 93:104322. https://doi.org/10.1016/j.archger.2020.104322
Ogawa M, Izawa KP, Satomi-Kobayashi S, Kitamura A, Tsuboi Y, Komaki K, Ono R, Sakai Y et al (2018) Preoperative exercise capacity is associated with the prevalence of postoperative delirium in elective cardiac surgery. Aging Clin Exp Res 30(1):27–34. https://doi.org/10.1007/s40520-017-0736-5
Yanagisawa T, Tatematsu N, Horiuchi M, Migitaka S, Yasuda S, Itatsu K, Kubota T, Sugiura H (2022) Preoperative low physical activity is a predictor of postoperative delirium in patients with gastrointestinal cancer: a retrospective study. Asian Pac J Cancer Prev 23(5):1753–1759. https://doi.org/10.31557/APJCP.2022.23.5.1753
Mosk CA, van Vugt JLA, de Jonge H, Witjes CD, Buettner S, Ijzermans JN, van der Laan L (2018) Low skeletal muscle mass as a risk factor for postoperative delirium in elderly patients undergoing colorectal cancer surgery. Clin Interv Aging 13:2097–2106. https://doi.org/10.2147/CIA.S175945
Xu J, Yang Y, Hu D (2023) Predictors of cognitive impairment in patients undergoing ileostomy for colorectal cancer: a retrospective analysis. PeerJ 11:e15405. https://doi.org/10.7717/peerj.15405
van Vugt JL, Levolger S, Gharbharan A, Koek M, Niessen WJ, Burger JW, Willemsen SP, de Bruin RW et al (2017) A comparative study of software programmes for cross-sectional skeletal muscle and adipose tissue measurements on abdominal computed tomography scans of rectal cancer patients. J Cachexia Sarcopenia Muscle 8(2):285–297. https://doi.org/10.1002/jcsm.12158
Hirase T, Haghshenas V, Bratescu R, Dong D, Kuo PH, Rashid A, Kavuri V, Hanson DS et al (2021) Sarcopenia predicts perioperative adverse events following complex revision surgery for the thoracolumbar spine. Spine J 21(6):1001–1009. https://doi.org/10.1016/j.spinee.2021.02.001
Makiguchi T, Yamaguchi T, Nakamura H, Ogawa M, Harimoto N, Shirabe K, Yokoo S (2020) Impact of skeletal muscle mass on postoperative delirium in patients undergoing free flap repair after oral cancer resection. J Plast Surg Hand Surg 54(3):161–166. https://doi.org/10.1080/2000656X.2020.1724545
Lee SS, Lo Y, Verghese J (2019) Physical activity and risk of postoperative delirium. J Am Geriatr Soc 67(11):2260–2266. https://doi.org/10.1111/jgs.16083
Feng X, Uchida Y, Koch L, Britton S, Hu J, Lutrin D, Maze M (2017) exercise prevents enhanced postoperative neuroinflammation and cognitive decline and rectifies the gut microbiome in a rat model of metabolic syndrome. Front Immunol 8:1768. https://doi.org/10.3389/fimmu.2017.01768
Lai Z, Shan W, Li J, Min J, Zeng X, Zuo Z (2021) Appropriate exercise level attenuates gut dysbiosis and valeric acid increase to improve neuroplasticity and cognitive function after surgery in mice. Mol Psychiatry 26(12):7167–7187. https://doi.org/10.1038/s41380-021-01291-y
Liu Y, Chu JMT, Ran Y, Zhang Y, Chang RCC, Wong GTC (2022) Prehabilitative resistance exercise reduces neuroinflammation and improves mitochondrial health in aged mice with perioperative neurocognitive disorders. J Neuroinflammation 19(1):150. https://doi.org/10.1186/s12974-022-02483-1
Nemoto A, Goyagi T, Nemoto W, Nakagawasai O, Tan-No K, Niiyama Y (2022) Low skeletal muscle mass is associated with perioperative neurocognitive disorder due to decreased neurogenesis in rats. Anesth Analg 134(1):194–203. https://doi.org/10.1213/ANE.0000000000005681
Dheen ST, Kaur C, Ling EA (2007) Microglial activation and its implications in the brain diseases. Curr Med Chem 14(11):1189–1197. https://doi.org/10.2174/092986707780597961
Block ML, Zecca L, Hong JS (2007) Microglia-mediated neurotoxicity: uncovering the molecular mechanisms. Nat Rev Neurosci 8(1):57–69. https://doi.org/10.1038/nrn2038
Frank-Cannon TC, Alto LT, McAlpine FE, Tansey MG (2009) Does neuroinflammation fan the flame in neurodegenerative diseases? Mol Neurodegener 4:47. https://doi.org/10.1186/1750-1326-4-47
Terrando N, Eriksson LI, Ryu JK, Yang T, Monaco C, Feldmann M, Jonsson Fagerlund M, Charo IF et al (2011) Resolving postoperative neuroinflammation and cognitive decline. Ann Neurol 70(6):986–995. https://doi.org/10.1002/ana.22664
Tang Y, Le W (2016) Differential roles of M1 and M2 microglia in neurodegenerative diseases. Mol Neurobiol 53(2):1181–1194. https://doi.org/10.1007/s12035-014-9070-5
Teleanu DM, Niculescu AG, Lungu CI II, Radu O, Vladacenco E, Roza B, Costachescu AM, Grumezescu RIT (2022) An overview of oxidative stress, neuroinflammation, and neurodegenerative diseases. Int J Mol Sci 23(11). https://doi.org/10.3390/ijms23115938
Masdeu JC, Pascual B, Fujita M (2022) Imaging neuroinflammation in neurodegenerative disorders. J Nucl Med 63(Suppl 1):45S–52S. https://doi.org/10.2967/jnumed.121.263200
Mangalmurti A, Lukens JR (2022) How neurons die in Alzheimer’s disease: implications for neuroinflammation. Curr Opin Neurobiol 75:102575. https://doi.org/10.1016/j.conb.2022.102575
Liu Y, Yin Y (2018) Emerging roles of immune cells in postoperative cognitive dysfunction. Mediators Inflamm 2018:6215350. https://doi.org/10.1155/2018/6215350
Taylor J, Parker M, Casey CP, Tanabe S, Kunkel D, Rivera C, Zetterberg H, Blennow K et al (2022) Postoperative delirium and changes in the blood-brain barrier, neuroinflammation, and cerebrospinal fluid lactate: a prospective cohort study. Br J Anaesth 129(2):219–230. https://doi.org/10.1016/j.bja.2022.01.005
Ruhnau J, Muller J, Nowak S, Strack S, Sperlich D, Pohl A, Dilz J, Saar A et al (2023) Serum biomarkers of a pro-neuroinflammatory state may define the pre-operative risk for postoperative delirium in spine surgery. Int J Mol Sci 24(12). https://doi.org/10.3390/ijms241210335
Lai Z, Min J, Li J, Shan W, Yu W, Zuo Z (2021) Surgery trauma severity but not anesthesia length contributes to postoperative cognitive dysfunction in mice. J Alzheimers Dis 80(1):245–257. https://doi.org/10.3233/JAD-201232
Zhang ZJ, Zheng XX, Zhang XY, Zhang Y, Huang BY, Luo T (2020) Aging alters Hv1-mediated microglial polarization and enhances neuroinflammation after peripheral surgery. CNS Neurosci Ther 26(3):374–384. https://doi.org/10.1111/cns.13271
Luo G, Wang X, Cui Y, Cao Y, Zhao Z, Zhang J (2021) Metabolic reprogramming mediates hippocampal microglial M1 polarization in response to surgical trauma causing perioperative neurocognitive disorders. J Neuroinflammation 18(1):267. https://doi.org/10.1186/s12974-021-02318-5
Yang T, Velagapudi R, Kong C, Ko U, Kumar V, Brown P, Franklin NO, Zhang X et al (2023) Protective effects of omega-3 fatty acids in a blood-brain barrier-on-chip model and on postoperative delirium-like behaviour in mice. Br J Anaesth 130(2):e370–e380. https://doi.org/10.1016/j.bja.2022.05.025
Liaquat Z, Xu X, Zilundu PLM, Fu R, Zhou L (2021) The current role of dexmedetomidine as neuroprotective agent: an updated review. Brain Sci 11(7). https://doi.org/10.3390/brainsci11070846
Gonzalo-Encabo P, Maldonado G, Valades D, Ferragut C, Perez-Lopez A (2021) The role of exercise training on low-grade systemic inflammation in adults with overweight and obesity: a systematic review. Int J Environ Res Public Health 18(24). https://doi.org/10.3390/ijerph182413258
Connolly MG, Bruce SR, Kohman RA (2022) Exercise duration differentially effects age-related neuroinflammation and hippocampal neurogenesis. Neuroscience 490:275–286. https://doi.org/10.1016/j.neuroscience.2022.03.022
Liu Y, Chu JMT, Yan T, Zhang Y, Chen Y, Chang RCC, Wong GTC (2020) Short-term resistance exercise inhibits neuroinflammation and attenuates neuropathological changes in 3xTg Alzheimer’s disease mice. J Neuroinflammation 17(1):4. https://doi.org/10.1186/s12974-019-1653-7
Zhang X, He Q, Huang T, Zhao N, Liang F, Xu B, Chen X, Li T et al (2019) Treadmill exercise decreases abeta deposition and counteracts cognitive decline in APP/PS1 mice, possibly via hippocampal microglia modifications. Front Aging Neurosci 11:78. https://doi.org/10.3389/fnagi.2019.00078
Yang Y, Liu Y, Zhu J, Song S, Huang Y, Zhang W, Sun Y, Hao J et al (2022) Neuroinflammation-mediated mitochondrial dysregulation involved in postoperative cognitive dysfunction. Free Radic Biol Med 178:134–146. https://doi.org/10.1016/j.freeradbiomed.2021.12.004
Adak A, Khan MR (2019) An insight into gut microbiota and its functionalities. Cell Mol Life Sci 76(3):473–493. https://doi.org/10.1007/s00018-018-2943-4
Socala K, Doboszewska U, Szopa A, Serefko A, Wlodarczyk M, Zielinska A, Poleszak E, Fichna J et al (2021) The role of microbiota-gut-brain axis in neuropsychiatric and neurological disorders. Pharmacol Res 172:105840. https://doi.org/10.1016/j.phrs.2021.105840
Prager O, Friedman A, Nebenzahl YM (2017) Role of neural barriers in the pathogenesis and outcome of Streptococcus pneumoniae meningitis. Exp Ther Med 13(3):799–809. https://doi.org/10.3892/etm.2017.4082
Wang X, Wang Z, Cao J, Dong Y, Chen Y (2023) Gut microbiota-derived metabolites mediate the neuroprotective effect of melatonin in cognitive impairment induced by sleep deprivation. Microbiome 11(1):17. https://doi.org/10.1186/s40168-022-01452-3
Barichella M, Severgnini M, Cilia R, Cassani E, Bolliri C, Caronni S, Ferri V, Cancello R et al (2019) Unraveling gut microbiota in Parkinson’s disease and atypical parkinsonism. Mov Disord 34(3):396–405. https://doi.org/10.1002/mds.27581
Liufu N, Liu L, Shen S, Jiang Z, Dong Y, Wang Y, Culley D, Crosby G et al (2020) Anesthesia and surgery induce age-dependent changes in behaviors and microbiota. Aging (Albany NY) 12(2):1965–1986. https://doi.org/10.18632/aging.102736
Liu M, Song S, Chen Q, Sun J, Chu W, Zhang Y, Ji F (2021) Gut microbiota mediates cognitive impairment in young mice after multiple neonatal exposures to sevoflurane. Aging (Albany NY) 13(12):16733–16748. https://doi.org/10.18632/aging.203193
Zhang Y, Baldyga K, Dong Y, Song W, Villanueva M, Deng H, Mueller A, Houle TT et al (2023) The association between gut microbiota and postoperative delirium in patients. Transl Psychiatry 13(1):156. https://doi.org/10.1038/s41398-023-02450-1
Li R, Liu R, Chen L, Wang G, Qin L, Yu Z, Wan Z (2023) Microbiota from exercise mice counteracts high-fat high-cholesterol diet-induced cognitive impairment in C57BL/6 mice. Oxid Med Cell Longev 2023:2766250. https://doi.org/10.1155/2023/2766250
Yuan S, Yang J, Jian Y, Lei Y, Yao S, Hu Z, Liu X, Tang C et al (2022) Treadmill exercise modulates intestinal microbes and suppresses LPS displacement to alleviate neuroinflammation in the brains of APP/PS1 mice. Nutrients 14(19). https://doi.org/10.3390/nu14194134
Wang R, Cai Y, Lu W, Zhang R, Shao R, Yau SY, Stubbs B, McIntyre RS et al (2023) Exercise effect on the gut microbiota in young adolescents with subthreshold depression: a randomized psychoeducation-controlled Trial. Psychiatry Res 319:115005. https://doi.org/10.1016/j.psychres.2022.115005
Yang W, Yu T, Huang X, Bilotta AJ, Xu L, Lu Y, Sun J, Pan F et al (2020) Intestinal microbiota-derived short-chain fatty acids regulation of immune cell IL-22 production and gut immunity. Nat Commun 11(1):4457. https://doi.org/10.1038/s41467-020-18262-6
Fan D, Li J, Zheng B, Hua L, Zuo Z (2016) Enriched environment attenuates surgery-induced impairment of learning, memory, and neurogenesis possibly by preserving BDNF expression. Mol Neurobiol 53(1):344–354. https://doi.org/10.1007/s12035-014-9013-1
Shimada H, Tsutsumimoto K, Doi T, Lee S, Bae S, Nakakubo S, Makino K, Arai H (2021) Effect of sarcopenia status on disability incidence among Japanese older adults. J Am Med Dir Assoc 22(4):846–852. https://doi.org/10.1016/j.jamda.2020.10.036
Bahat G, Tufan A, Kilic C, Karan MA, Cruz-Jentoft AJ (2020) Prevalence of sarcopenia and its components in community-dwelling outpatient older adults and their relation with functionality. Aging Male 23(5):424–430. https://doi.org/10.1080/13685538.2018.1511976
Yang R, Zhang Y, Shen X, Yan S (2016) Sarcopenia associated with renal function in the patients with type 2 diabetes. Diabetes Res Clin Pract 118:121–129. https://doi.org/10.1016/j.diabres.2016.06.023
Sui SX, Williams LJ, Holloway-Kew KL, Hyde NK, Pasco JA (2020) Skeletal muscle health and cognitive function: a narrative review. Int J Mol Sci 22(1). https://doi.org/10.3390/ijms22010255
Ogawa Y, Kaneko Y, Sato T, Shimizu S, Kanetaka H, Hanyu H (2018) Sarcopenia and muscle functions at various stages of Alzheimer disease. Front Neurol 9:710. https://doi.org/10.3389/fneur.2018.00710
Tanabe C, Reed MJ, Pham TN, Penn K, Bentov I, Kaplan SJ (2019) Association of brain atrophy and masseter sarcopenia with 1-year mortality in older trauma patients. JAMA Surg 154(8):716–723. https://doi.org/10.1001/jamasurg.2019.0988
Park H, Poo MM (2013) Neurotrophin regulation of neural circuit development and function. Nat Rev Neurosci 14(1):7–23. https://doi.org/10.1038/nrn3379
Colucci-D'Amato L, Speranza L, Volpicelli F (2020) Neurotrophic Factor BDNF, Physiological functions and therapeutic potential in depression, neurodegeneration and brain cancer. Int J Mol Sci 21(20). https://doi.org/10.3390/ijms21207777
Etnier JL, Wideman L, Labban JD, Piepmeier AT, Pendleton DM, Dvorak KK, Becofsky K (2016) The effects of acute exercise on memory and brain-derived neurotrophic factor (BDNF). J Sport Exerc Psychol 38(4):331–340. https://doi.org/10.1123/jsep.2015-0335
El Hayek L, Khalifeh M, Zibara V, Abi Assaad R, Emmanuel N, Karnib N, El-Ghandour R, Nasrallah P et al (2019) Lactate mediates the effects of exercise on learning and memory through SIRT1-dependent activation of hippocampal brain-derived neurotrophic factor (BDNF). J Neurosci 39(13):2369–2382. https://doi.org/10.1523/JNEUROSCI.1661-18.2019
Real CC, Ferreira AF, Chaves-Kirsten GP, Torrao AS, Pires RS, Britto LR (2013) BDNF receptor blockade hinders the beneficial effects of exercise in a rat model of Parkinson’s disease. Neuroscience 237:118–129. https://doi.org/10.1016/j.neuroscience.2013.01.060
Dun SL, Lyu RM, Chen YH, Chang JK, Luo JJ, Dun NJ (2013) Irisin-immunoreactivity in neural and non-neural cells of the rodent. Neuroscience 240:155–162. https://doi.org/10.1016/j.neuroscience.2013.02.050
Wrann CD, White JP, Salogiannnis J, Laznik-Bogoslavski D, Wu J, Ma D, Lin JD, Greenberg ME et al (2013) Exercise induces hippocampal BDNF through a PGC-1alpha/FNDC5 pathway. Cell Metab 18(5):649–659. https://doi.org/10.1016/j.cmet.2013.09.008
Moon HY, Becke A, Berron D, Becker B, Sah N, Benoni G, Janke E, Lubejko ST et al (2016) Running-induced systemic cathepsin B secretion is associated with memory function. Cell Metab 24(2):332–340. https://doi.org/10.1016/j.cmet.2016.05.025
Spinelli JB, Haigis MC (2018) The multifaceted contributions of mitochondria to cellular metabolism. Nat Cell Biol 20(7):745–754. https://doi.org/10.1038/s41556-018-0124-1
Hood DA, Memme JM, Oliveira AN, Triolo M (2019) Maintenance of skeletal muscle mitochondria in health, exercise, and aging. Annu Rev Physiol 81:19–41. https://doi.org/10.1146/annurev-physiol-020518-114310
Mishra P, Chan DC (2016) Metabolic regulation of mitochondrial dynamics. J Cell Biol 212(4):379–387. https://doi.org/10.1083/jcb.201511036
Toyama EQ, Herzig S, Courchet J, Lewis TL Jr, Loson OC, Hellberg K, Young NP, Chen H et al (2016) AMP-activated protein kinase mediates mitochondrial fission in response to energy stress. Science 351(6270):275–281. https://doi.org/10.1126/science.aab4138
Pickles S, Vigie P, Youle RJ (2018) Mitophagy and quality control mechanisms in mitochondrial maintenance. Curr Biol 28(4):R170–R185. https://doi.org/10.1016/j.cub.2018.01.004
Fang EF, Hou Y, Palikaras K, Adriaanse BA, Kerr JS, Yang B, Lautrup S, Hasan-Olive MM et al (2019) Mitophagy inhibits amyloid-beta and tau pathology and reverses cognitive deficits in models of Alzheimer’s disease. Nat Neurosci 22(3):401–412. https://doi.org/10.1038/s41593-018-0332-9
Agrawal I, Jha S (2020) Mitochondrial dysfunction and Alzheimer’s disease: role of microglia. Front Aging Neurosci 12:252. https://doi.org/10.3389/fnagi.2020.00252
Zhao Y, Zhang J, Zheng Y, Zhang Y, Zhang XJ, Wang H, Du Y, Guan J et al (2021) NAD(+) improves cognitive function and reduces neuroinflammation by ameliorating mitochondrial damage and decreasing ROS production in chronic cerebral hypoperfusion models through Sirt1/PGC-1alpha pathway. J Neuroinflammation 18(1):207. https://doi.org/10.1186/s12974-021-02250-8
Lu Y, Chen L, Ye J, Chen C, Zhou Y, Li K, Zhang Z, Peng M (2020) Surgery/anesthesia disturbs mitochondrial fission/fusion dynamics in the brain of aged mice with postoperative delirium. Aging (Albany NY) 12(1):844–865. https://doi.org/10.18632/aging.102659
Porter C, Reidy PT, Bhattarai N, Sidossis LS, Rasmussen BB (2015) Resistance exercise training alters mitochondrial function in human skeletal muscle. Med Sci Sports Exerc 47(9):1922–1931. https://doi.org/10.1249/MSS.0000000000000605
Arribat Y, Broskey NT, Greggio C, Boutant M, Conde Alonso S, Kulkarni SS, Lagarrigue S, Carnero EA et al (2019) Distinct patterns of skeletal muscle mitochondria fusion, fission and mitophagy upon duration of exercise training. Acta Physiol (Oxf) 225(2):e13179. https://doi.org/10.1111/apha.13179
Luo L, Dai JR, Guo SS, Lu AM, Gao XF, Gu YR, Zhang XF, Xu HD et al (2017) Lysosomal proteolysis is associated with exercise-induced improvement of mitochondrial quality control in aged hippocampus. J Gerontol A Biol Sci Med Sci 72(10):1342–1351. https://doi.org/10.1093/gerona/glw242
Marques-Aleixo I, Santos-Alves E, Balca MM, Rizo-Roca D, Moreira PI, Oliveira PJ, Magalhaes J, Ascensao A (2015) Physical exercise improves brain cortex and cerebellum mitochondrial bioenergetics and alters apoptotic, dynamic and auto(mito)phagy markers. Neuroscience 301:480–495. https://doi.org/10.1016/j.neuroscience.2015.06.027
Kim TW, Park SS, Park JY, Park HS (2020) Infusion of plasma from exercised mice ameliorates cognitive dysfunction by increasing hippocampal neuroplasticity and mitochondrial functions in 3xTg-AD mice. Int J Mol Sci 21(9):10.3390/ijms21093291
Bellot A, Guivernau B, Tajes M, Bosch-Morato M, Valls-Comamala V, Munoz FJ (2014) The structure and function of actin cytoskeleton in mature glutamatergic dendritic spines. Brain Res 1573:1–16. https://doi.org/10.1016/j.brainres.2014.05.024
Maiti P, Manna J, Ilavazhagan G, Rossignol J, Dunbar GL (2015) Molecular regulation of dendritic spine dynamics and their potential impact on synaptic plasticity and neurological diseases. Neurosci Biobehav Rev 59:208–237. https://doi.org/10.1016/j.neubiorev.2015.09.020
Nicoll RA, Schmitz D (2005) Synaptic plasticity at hippocampal mossy fibre synapses. Nat Rev Neurosci 6(11):863–876. https://doi.org/10.1038/nrn1786
Hering H, Sheng M (2001) Dendritic spines: structure, dynamics and regulation. Nat Rev Neurosci 2(12):880–888. https://doi.org/10.1038/35104061
Buffington SA, Huang W, Costa-Mattioli M (2014) Translational control in synaptic plasticity and cognitive dysfunction. Annu Rev Neurosci 37:17–38. https://doi.org/10.1146/annurev-neuro-071013-014100
van Spronsen M, Hoogenraad CC (2010) Synapse pathology in psychiatric and neurologic disease. Curr Neurol Neurosci Rep 10(3):207–214. https://doi.org/10.1007/s11910-010-0104-8
Hayashi Y (2022) Molecular mechanism of hippocampal long-term potentiation - towards multiscale understanding of learning and memory. Neurosci Res 175:3–15. https://doi.org/10.1016/j.neures.2021.08.001
Pinar C, Fontaine CJ, Trivino-Paredes J, Lottenberg CP, Gil-Mohapel J, Christie BR (2017) Revisiting the flip side: long-term depression of synaptic efficacy in the hippocampus. Neurosci Biobehav Rev 80:394–413. https://doi.org/10.1016/j.neubiorev.2017.06.001
Watanabe Y, Muller MK, von Engelhardt J, Sprengel R, Seeburg PH, Monyer H (2015) Age-dependent degeneration of mature dentate gyrus granule cells following NMDA receptor ablation. Front Mol Neurosci 8:87. https://doi.org/10.3389/fnmol.2015.00087
Hardingham GE, Bading H (2010) Synaptic versus extrasynaptic NMDA receptor signalling: implications for neurodegenerative disorders. Nat Rev Neurosci 11(10):682–696. https://doi.org/10.1038/nrn2911
Dore K, Stein IS, Brock JA, Castillo PE, Zito K, Sjostrom PJ (2017) Unconventional NMDA receptor signaling. J Neurosci 37(45):10800–10807. https://doi.org/10.1523/JNEUROSCI.1825-17.2017
Kullmann DM, Lamsa KP (2007) Long-term synaptic plasticity in hippocampal interneurons. Nat Rev Neurosci 8(9):687–699. https://doi.org/10.1038/nrn2207
Azimi M, Gharakhanlou R, Naghdi N, Khodadadi D, Heysieattalab S (2018) Moderate treadmill exercise ameliorates amyloid-beta-induced learning and memory impairment, possibly via increasing AMPK activity and up-regulation of the PGC-1alpha/FNDC5/BDNF pathway. Peptides 102:78–88. https://doi.org/10.1016/j.peptides.2017.12.027
Lourenco MV, Frozza RL, de Freitas GB, Zhang H, Kincheski GC, Ribeiro FC, Goncalves RA, Clarke JR et al (2019) Exercise-linked FNDC5/irisin rescues synaptic plasticity and memory defects in Alzheimer’s models. Nat Med 25(1):165–175. https://doi.org/10.1038/s41591-018-0275-4
Wang YY, Zhou YN, Jiang L, Wang S, Zhu L, Zhang SS, Yang H, He Q et al (2023) Long-term voluntary exercise inhibited AGE/RAGE and microglial activation and reduced the loss of dendritic spines in the hippocampi of APP/PS1 transgenic mice. Exp Neurol 363:114371. https://doi.org/10.1016/j.expneurol.2023.114371
Wu Y, Deng F, Wang J, Liu Y, Zhou W, Qu L, Cheng M (2020) Intensity-dependent effects of consecutive treadmill exercise on spatial learning and memory through the p-CREB/BDNF/NMDAR signaling in hippocampus. Behav Brain Res 386:112599. https://doi.org/10.1016/j.bbr.2020.112599
Wilson RJ, Davies S, Yates D, Redman J, Stone M (2010) Impaired functional capacity is associated with all-cause mortality after major elective intra-abdominal surgery. Br J Anaesth 105(3):297–303. https://doi.org/10.1093/bja/aeq128
Valkenet K, van de Port IG, Dronkers JJ, de Vries WR, Lindeman E, Backx FJ (2011) The effects of preoperative exercise therapy on postoperative outcome: a systematic review. Clin Rehabil 25(2):99–111. https://doi.org/10.1177/0269215510380830
Cassilhas RC, Viana VA, Grassmann V, Santos RT, Santos RF, Tufik S, Mello MT (2007) The impact of resistance exercise on the cognitive function of the elderly. Med Sci Sports Exerc 39(8):1401–1407. https://doi.org/10.1249/mss.0b013e318060111f
Nagamatsu LS, Handy TC, Hsu CL, Voss M, Liu-Ambrose T (2012) Resistance training promotes cognitive and functional brain plasticity in seniors with probable mild cognitive impairment. Arch Intern Med 172(8):666–668. https://doi.org/10.1001/archinternmed.2012.379
Yu F, Vock DM, Zhang L, Salisbury D, Nelson NW, Chow LS, Smith G, Barclay TR et al (2021) Cognitive effects of aerobic exercise in Alzheimer’s disease: a pilot randomized controlled trial. J Alzheimers Dis 80(1):233–244. https://doi.org/10.3233/JAD-201100
Szuhany KL, Bugatti M, Otto MW (2015) A meta-analytic review of the effects of exercise on brain-derived neurotrophic factor. J Psychiatr Res 60:56–64. https://doi.org/10.1016/j.jpsychires.2014.10.003
Cavalcante BR, de Souza MF, Falck RS, Liu-Ambrose T, Behm DG, Pitangui ACR, de Araujo RC (2020) Effects of resistance exercise with instability on cognitive function (REI study): a proof-of-concept randomized controlled trial in older adults with cognitive complaints. J Alzheimers Dis 77(1):227–239. https://doi.org/10.3233/JAD-200349
Cassilhas RC, Lee KS, Fernandes J, Oliveira MG, Tufik S, Meeusen R, de Mello MT (2012) Spatial memory is improved by aerobic and resistance exercise through divergent molecular mechanisms. Neuroscience 202:309–317. https://doi.org/10.1016/j.neuroscience.2011.11.029
ten Brinke LF, Bolandzadeh N, Nagamatsu LS, Hsu CL, Davis JC, Miran-Khan K, Liu-Ambrose T (2015) Aerobic exercise increases hippocampal volume in older women with probable mild cognitive impairment: a 6-month randomised controlled trial. Br J Sports Med 49(4):248–254. https://doi.org/10.1136/bjsports-2013-093184
Huang X, Zhao X, Li B, Cai Y, Zhang S, Wan Q, Yu F (2022) Comparative efficacy of various exercise interventions on cognitive function in patients with mild cognitive impairment or dementia: a systematic review and network meta-analysis. J Sport Health Sci 11(2):212–223. https://doi.org/10.1016/j.jshs.2021.05.003
Gallardo-Gomez D, Del Pozo-Cruz J, Noetel M, Alvarez-Barbosa F, Alfonso-Rosa RM, Del Pozo Cruz B (2022) Optimal dose and type of exercise to improve cognitive function in older adults: a systematic review and bayesian model-based network meta-analysis of RCTs. Ageing Res Rev 76:101591. https://doi.org/10.1016/j.arr.2022.101591
Duan S, Liao Y, Tang Y, Zhang B, Peng M, Tong J, Ouyang W, Le Y (2022) Short-term perioperative cognitive therapy combined with rehabilitation exercise reduces the incidence of neurocognitive disorder in elderly patients: a randomized controlled trial. Minerva Anestesiol 88(3). https://doi.org/10.23736/s0375-9393.21.15877-8
Cotman CW, Berchtold NC, Christie LA (2007) Exercise builds brain health: key roles of growth factor cascades and inflammation. Trends Neurosci 30(9):464–472. https://doi.org/10.1016/j.tins.2007.06.011
Mattson MP (2012) Energy intake and exercise as determinants of brain health and vulnerability to injury and disease. Cell Metab 16(6):706–722. https://doi.org/10.1016/j.cmet.2012.08.012
LeBouthillier DM, Asmundson GJG (2017) The efficacy of aerobic exercise and resistance training as transdiagnostic interventions for anxiety-related disorders and constructs: a randomized controlled trial. J Anxiety Disord 52:43–52. https://doi.org/10.1016/j.janxdis.2017.09.005
Philippot A, Dubois V, Lambrechts K, Grogna D, Robert A, Jonckheer U, Chakib W, Beine A et al (2022) Impact of physical exercise on depression and anxiety in adolescent inpatients: a randomized controlled trial. J Affect Disord 301:145–153. https://doi.org/10.1016/j.jad.2022.01.011
Pedersen BK, Saltin B (2015) Exercise as medicine - evidence for prescribing exercise as therapy in 26 different chronic diseases. Scand J Med Sci Sports 25(Suppl 3):1–72. https://doi.org/10.1111/sms.12581
Voss MW, Nagamatsu LS, Liu-Ambrose T, Kramer AF (2011) Exercise, brain, and cognition across the life span. J Appl Physiol (1985) 111(5):1505–1513. https://doi.org/10.1152/japplphysiol.00210.2011
Acknowledgements
Not applicable
Funding
The work is funded by the National Natural Science Foundation of China (82101255), Natural Science Foundation of Shandong Province (ZR2020QH291), Qingdao Key Health Discipline Development Fund (QDZDZK-2022094), Qingdao Outstanding Health Professional Development Fund (2022), and the Scientific Research Foundation of Qilu Hospital of Shandong University (Qingdao) (QDKY2022QN03).
Author information
Authors and Affiliations
Contributions
HF, PW, and JL were involved in the review concept and acquired the funding. HF conducted the literature review and wrote the original draft. HF and PW made the figures. ZZ, WL, XK, JL, HZ, and PW contributed to the revision of the manuscript. All authors approved the final submitted version.
Corresponding authors
Ethics declarations
Ethics Approval
Not applicable
Consent to Participate
Not applicable
Consent for Publication
Not applicable
Competing Interests
The authors declare no competing interests.
Additional information
Publisher’s Note
Springer Nature remains neutral with regard to jurisdictional claims in published maps and institutional affiliations.
Rights and permissions
Open Access This article is licensed under a Creative Commons Attribution 4.0 International License, which permits use, sharing, adaptation, distribution and reproduction in any medium or format, as long as you give appropriate credit to the original author(s) and the source, provide a link to the Creative Commons licence, and indicate if changes were made. The images or other third party material in this article are included in the article's Creative Commons licence, unless indicated otherwise in a credit line to the material. If material is not included in the article's Creative Commons licence and your intended use is not permitted by statutory regulation or exceeds the permitted use, you will need to obtain permission directly from the copyright holder. To view a copy of this licence, visit http://creativecommons.org/licenses/by/4.0/.
About this article
Cite this article
Feng, H., Zhang, Z., Lyu, W. et al. The Effects of Appropriate Perioperative Exercise on Perioperative Neurocognitive Disorders: a Narrative Review. Mol Neurobiol 61, 4663–4676 (2024). https://doi.org/10.1007/s12035-023-03864-0
Received:
Accepted:
Published:
Issue Date:
DOI: https://doi.org/10.1007/s12035-023-03864-0