Abstract
The gut microbiome may be involved in the occurrence of dementia primarily through the molecular mechanisms of producing bioactive molecules and promoting inflammation. Epidemiological evidence linking gut microbiome molecules and inflammatory markers to dementia risk has been mixed, and the intricate interplay between these groups of biomarkers suggests that their joint investigation in the context of dementia is warranted. We aimed to simultaneously investigate the association of circulating levels of selected gut microbiome molecules and inflammatory markers with dementia risk. This case–cohort epidemiological study included 805 individuals (83 years, 66% women) free of dementia at baseline. Plasma levels of 19 selected gut microbiome molecules comprising lipopolysaccharide, short-chain fatty acids, and indole-containing tryptophan metabolites as well as four inflammatory markers measured at baseline were linked to incident all-cause (ACD) and Alzheimer’s disease dementia (AD) in binary outcomes and time-to-dementia analyses. Independent of several covariates, seven gut microbiome molecules, 5-hydroxyindole-3-acetic acid, indole-3-butyric acid, indole-3-acryloylglycine, indole-3-lactic acid, indole-3-acetic acid methyl ester, isobutyric acid, and 2-methylbutyric acid, but no inflammatory markers discriminated incident dementia cases from non-cases. Furthermore, 5-hydroxyindole-3-acetic acid (hazard ratio: 0.58; 0.36–0.94, P = 0.025) was associated with time-to-ACD. These molecules underpin gut microbiome-host interactions in the development of dementia and they may be crucial in its prevention and intervention strategies. Future larger epidemiological studies are needed to confirm our findings, specifically in exploring the repeatedly measured circulating levels of these molecules and investigating their causal relationship with dementia risk.
Similar content being viewed by others
Avoid common mistakes on your manuscript.
Introduction
Dementia is a neurodegenerative disease characterized by cognitive impairment that affects memory, cognitive abilities, and behavior, and significantly interferes with a person’s ability to perform daily activities [1]. The cognitive functional deterioration in dementia is beyond what is expected as the natural consequence of biological ageing [1]. Dementia has uncertain etiology, inherently complex pathophysiology, and heterogeneous manifestations [2]. Alzheimer’s disease dementia (AD) is the most frequent subtype, accounting for 60–80% of dementia as a whole, all-cause dementia (ACD) [3]. AD is driven by the brain accumulation of beta-amyloid plaques and tau protein tangles, but other mechanisms that include neuronal loss, synaptic dysfunction, neurodegeneration, and metabolic and inflammatory alterations might play earlier or more central role [4]. The global burden of dementia, influenced by the increasing life expectancy, demographics, and risk factors, was recently projected to increase in some countries such as the USA and Germany [5]. Indeed, a deeper insight into dementia’s well-known and emerging modifiable risk factors could have a major impact on its rising burden through targeted prevention and intervention strategies.
Interestingly, there is a growing recognition that the gut microbiome may play a role in the occurrence of dementia [6,7,8]. The major putative molecular mechanisms underlying this link are the production of gut microbiome bioactive molecules [6,7,8,9] and gut microbiome-induced systemic inflammation [6, 7, 10]. These gut microbiome bioactive molecules comprising those produced solely by the gut microbiome and those resulting from the host–gut microbiome co-metabolism are primarily bacterial endotoxins such as lipopolysaccharide (LPS), short-chain fatty acids (SCFA), and indole-containing tryptophan metabolites [6, 9, 11]. Crucially, some of these molecules are detectable in the systemic circulation [6, 9, 12] reaching concentrations up to and above those achieved by a typical drug dose [12] and they have been reported to cross the blood–brain barrier (BBB) [8, 9, 13, 14].
Remarkably, epidemiological studies have reported associations of gut microbiome molecules, specifically acetic acid (AA) and propionic acid (PA) [15], isobutyric acid and isovaleric acid [16] and indoxyl sulfate (IS) [17], LPS [18], LPS-binding protein (LBP) [19], AA [20], PA [21, 22], 2-methylbutyric acid, isovaleric acid, valeric acid, indole-3-pyruvic acid [22], and 5-hydroxyindole-3-acetic acid (5OH-IAA) [23, 24] with either ACD or AD risk but others did not observe associations with AA [16, 25], PA [16], and indole [16], LPS [22], indole-3-acetic acid (IAA) [23], indoleacrylic acid (IACR) [22], and 5OH-IAA [26]. Similarly, a few studies reported association of inflammatory markers, C-reactive protein (CRP), IL-1β, IL-6, and tumor necrosis factor-alpha (TNF-α) with either ACD or AD risk [27, 28], whereas others indicated no association with CRP [29,30,31], IL-1β [31], IL-6 [19, 31], and TNF-α [31]. These mixed findings may be partly due to the generally modest sample size of the aforementioned studies. Thus, larger studies are warranted. Furthermore, the levels of some gut microbiome molecules and systemic inflammatory markers as well as dementia risk are influenced by a myriad of factors such as body composition, smoking, alcohol consumption, and chronic diseases [2, 32,33,34]. These factors were not sufficiently accounted for in previous studies. Most important, the extensively reported association of some gut microbiome molecules and inflammatory markers [32, 33, 35,36,37,38] suggests that there is an intricate pathophysiological interplay between these molecules and inflammation. However, a joint investigation of these molecules and inflammatory markers in the context of dementia occurrence, which seems crucially important, has received limited attention.
To this end, the present epidemiological investigation sought to explore the circulating levels of selected gut microbiome molecules and inflammatory markers simultaneously and examine their association with the risk of ACD and AD while accounting for these important risk factors.
Methods
Study Population
The present study is embedded within the German study on Ageing, Cognition, and Dementia in Primary Care Patients (AgeCoDe) study. The AgeCoDe is a unique study in that it is a prospective cohort of elderly (≥75 years) general practitioner (GP) patients. Other inclusion criteria include being a native German language speaker or speaking German fluently, absence of severe hearing or vision impairments, and residency at home. The participants were recruited from six German cities, Bonn, Düsseldorf, Hamburg, Leipzig, Mannheim, and Munich. The study commenced between 2003 and 2004, and detailed clinical information that includes standardized cognitive testing was conducted. Follow-up assessments were performed every 18 months and every 10 months after follow-up seven. At follow-up three (henceforth, baseline) which commenced in 2007, participants provided blood samples at the GP’s office, from where the samples were transported to the central laboratory for storage. For the current study, we considered incident dementia, that is, dementia diagnosis between baseline and follow-up nine (henceforth, end of follow-up), which was completed in 2016. The ethical approval for the AgeCoDe study was obtained from the Ethics Commission of the University of Bonn 050/02, 258/07; the Ethics Commission of the Medical Faculty of the Heinrich Heine University Düsseldorf 2079/2002, 2999/2008; the Ethics Commission of the Medical Association Hamburg OB/08/02, 2817/2007; the Ethics Commission at the Medical Center of the University of Leipzig 143/2002, 309/2007. The ethical approval for the present biomarker analysis was obtained from the Ethics Commission of the University of Bonn 245/22. All participants gave written informed consent. Details of the recruitment of participants and assessment of dementia in the AgeCoDe have been reported previously [39].
Study Design
The eligible individuals were those free of dementia at baseline and with information on classical risk factors of dementia, namely age, sex, and body mass index (BMI) at baseline. Consequently, the total size of this current full cohort was N = 1323, of which 281 (21%) developed incident ACD. Incident dementia was defined as cases from the full cohort occurring between baseline and end. Person time (time-to-event) was calculated from the baseline date to the date of diagnosis of dementia, or the end of study, whichever occurred first. We censored individuals at the end of the study on 29 November 2016.
From these N = 1323 eligible individuals, we designed a classical case–cohort study that comprise 50% (N = 662) subcohort selected via a simple random sampling without replacement and all the ACD cases outside the subcohort. The sampling fraction and method were chosen for their reported efficiency [40]. Consequently, the case–cohort sample for ACD analyses was N = 805 (N = 143 non-subcohort cases, N = 138 subcohort cases, and N = 524 subcohort non-cases). Secondarily, we selected AD cases outside the subcohort to form an AD case–cohort sample of N = 740 (N = 78 non-subcohort cases, N = 73 subcohort cases, and N = 589 subcohort non-cases).
Measurement of Gut Microbiome Molecules and Inflammatory Markers
All biomarkers were measured from EDTA plasma collected at baseline. All laboratory analyses were blinded to the participants’ dementia status and any characteristics.
Lipopolysaccharide and Lipopolysaccharide-Binding Protein
LPS was measured by a quantitative sandwich enzyme immunoassay technique (MBS702450; MyBiosource, San Diego, CA, USA) and LBP by a solid-phase, two-site chemiluminescent immunometric assay (IMMULITE®1000, Siemens Healthcare GmbH, Erlangen, Germany). Further processing of the samples was carried out according to the specifications from the kit instructions or according to the specifications of the laboratories. For both LPS and LBP, the intra-assay coefficient of variation (CV) was <8% and inter-assay CV was <10%.
Indole-Containing Tryptophan Metabolites
Targeted metabolomics quantification of the concentrations 9 indole-containing tryptophan metabolites, IAA, indole-3-acetic acid methyl ester (IAA ME), 5OH-IAA, indole-3-propionic acid (IPA), indole-3-butyric acid (IBA), indole-3-lactic acid (ILA), indole-3-carboxaldehyde (ICARB), indole-3-acryloylglycine (IAG), IS was determined by ultra high performance liquid chromatography-electrospray ionization-triple quadrupole-mass spectrometry, as reported previously [41]. Other metabolites, which include tryptophan, methionine, tyrosine, serotonin, and N-acetyl-tryptophan, were also quantified in this targeted assay. The intra-day CV for all metabolites in the present analysis was less than 15%.
Short-Chain Fatty Acids
The measurement of the SCFA was according to previously reported targeted metabolomics analysis [42]. We measured eight SCFA namely AA, PA, isobutyric acid, butyric acid (BA), 2-methylbutyric acid, isovaleric acid, valeric acid (VA), and hexanoic acid (HA). The intra-day CV for all SCFAs was less than 20%.
Inflammatory Markers
The multiplexing analysis of IL-1β, IL-6, and TNFα was performed using the Luminex™ 200 system (Luminex, Austin, TX, USA). The intra-assay CV for all three markers was less than 10%. The inter-assay CV for IL-1β and IL-6 was less than 15% while TNF-α was less than 20%. High-sensitivity CRP was measured at the central laboratory of the University Hospital in Bonn.
Assessment of Covariates: Sociodemographic, Anthropometry, Lifestyle Factors, and Prevalent Diseases
All covariates were assessed at baseline. Standardized questionnaires were used to obtain information on age, sex, weight, height, education, last employment status, smoking status, alcohol consumption, physical activity, social status (marital status and living alone), and the presence of prevalent disease (hypertension, type 2 diabetes, coronary heart disease, stroke, depression, hearing and visual impairment, and traumatic brain injury). BMI was calculated as weight in kilograms divided by the squared height in meters. Educational level was categorized into low (inadequately completed or elementary schooling), middle (secondary), and high (tertiary). Participants whose last employment status was manual jobs, salaried jobs, civil service jobs, and self-employed were categorized as employed and others were categorized as unemployed. Smoking was assessed as the current smoking of cigarettes, a pipe, cigars, or other tobacco products. Individuals who were current non-smokers but smoked for any number of years of smoking were categorized as ex-smokers. Alcohol consumption was determined from the frequency and quantity of consumption and converted to a uniform measure of grams per day. Physically active individuals were those who had more than one per week cycling, hiking or long walks, swimming, gymnastics, and other sports such as golf. Marital status was categorized into four groups, widowed, divorced, married, and single. The Mini-Mental State Examination (MMSE) score was used to assess global cognitive function at baseline. Depression was assessed based on the 15-item version of the Geriatric Depression Scale dichotomized into <6 points (no evidence of depressive symptoms) and ≥6 points (evidence of depressive symptoms). Medication use was obtained from questionnaire. Plasma hemoglobin A1c (HbA1c) was measured using the Roche/Hitachi-ModularSystems (Roche) according to the manufacturer’s protocols. Apolipoprotein E (APOE)-ɛ4) status was determined from leucocyte DNA.
Outcomes
Dementia diagnoses were based on a validated, structured interview for the diagnosis of dementia of the Alzheimer type, multi-infarct (or vascular) dementia, and dementias of other etiology according to the Diagnostic and Statistical Manual of Mental Disorders (DSM)-III-R, DSM-IV, and ICD-10 (Structured Interview for Diagnosis of Dementia of Alzheimer type, Multi-infarct Dementia and Dementia of other etiology according to DSM-IV and ICD-10 (SIDAM) [43]), implemented by trained research assistants. The SIDAM consists of a cognitive test battery (55 items including the Mini-Mental State Examination and covering the cognitive domains of orientation, memory, abstract reasoning, verbal ability and calculation, constructional ability, aphasia and apraxia) and a section for clinical diagnostic impression and rating of psychosocial impairment with a scale for the assessment of activities of daily living. Dementia was diagnosed according to the criteria of the DSM-IV, which comprise a diagnostic algorithm in the SIDAM including cognitive impairment on the SISCO score and impairment in ADL (score of ≥2 on the SIDAM ADL Scale). The diagnosis of dementia in AD was established according to the National Institute of Neurological and Communicative Disorders and Stroke–Alzheimer’s Disease and Related Disorders Association criteria for probable AD [44]. Vascular dementia diagnosis was guided by the National Institute of Neurological Disorders and Stroke–Association Internationale pour la Recherché et l’Enseignement en Neurosciences criteria [45] (i.e., evidence of a cerebrovascular event [Hashinski-Rosen Scale and medical history] and temporal association of the cerebrovascular event with cognitive decline). Mixed dementia was diagnosed in the absence of temporal association of the cerebrovascular event with cognitive decline. For all analyses, individuals with mixed dementia and dementia in AD were combined. Dementia diagnosis in individuals who were not personally interviewed was based on the Global Deterioration Scale and the Blessed Dementia Scale subscales. A score of at least 4 on the Global Deterioration Scale represented a diagnosis of dementia. The diagnosis was established in these cases if the causal information provided was sufficient for judgment using the aforementioned criteria. All diagnoses were made in consensus conferences that included the interviewer and experienced geriatric psychiatrists or geriatricians. The primary and secondary outcomes for the present study were ACD and AD, respectively.
Statistical Analysis
Descriptive Analysis
Analysis was performed for ACD (n = 805) and AD (n = 740) case–cohorts separately. Continuous and categorical variables were summarized as median (25% and 75% percentile), and count (percentage), respectively. Difference in continuous and categorical predictors across dementia status were tested with the Kruskal–Wallis rank-sum test and either Pearson’s Chi-squared or Fisher’s exact test, respectively.
Multivariable Modeling of the Association of Gut Microbiome Molecules and Inflammatory Markers with Dementia Risk
Selection of Covariates
We identified covariates for the causal inference between gut microbiome molecules and inflammatory markers with dementia risk using a directed acyclic graph (DAG). Based on a priori knowledge and biological plausibility, we used a DAG to draw the directions of the paths between the gut microbiome molecules or inflammatory markers and covariates, between covariates and dementia, and between covariates. A minimal sufficient adjustment set of confounders was selected and used as covariates.
From the DAG, our covariates were as follows: age (years), sex (men and women: reference), BMI (kg/m2), APOE-ɛ4 (homozygous, heterozygous, absent: reference), smoking status (smokers, ex-smokers, non-smokers: reference), alcohol intake (g/day), educational level (high, middle low: reference), employment (employed and unemployed: reference), physical activity (active and inactive: reference), marital status (widowed, divorced, married, single: reference), living alone (yes and no: reference), family history of dementia (yes and no: reference), prevalent hypertension, diabetes mellitus, coronary heart disease, stroke, depression, traumatic brain injury (TBI) (yes and no: reference), hearing impairment (significant hearing loss, mild hearing loss, and no impairment: reference), visual impairment (most severe visual impairment, considerable visual impairment, difficult vision, and no impairment: reference), mediation (yes and no: reference), study center (Leipzig, Hamburg, Düsseldorf, Mannheim Munich, Bonn: reference), MMSE score, HbA1c, and habitual diet. Due to unavailability of self-reported dietary intake data in this study and since plasma concentrations of tryptophan, methionine, and tyrosine have been reported to differentiate habitual diet groups, fish-eaters and vegetarians, meat-eaters, and vegans [46], we used them as proxies for habitual diet. We additionally adjusted for serotonin and N-acetyl-tryptophan. The 23 primary predictors (molecules and inflammatory markers) were LPS (pg/ml), LBP (μg/ml), IAA, IAA ME, 5OH-IAA, IPA, IBA, ILA, ICARB, IAG, IS, AA, PA, isobutyric acid, BA, 2-methylbutyric acid, isovaleric acid, VA, and HA (μM), CRP (mg/ml), and IL-1β, IL-6, and TNF-α (pg/ml). We checked the bivariate association between the primary predictors and covariates using the Spearman correlation and Kruskal–Wallis rank-sum test.
Handling of Missingness
We examined the proportion of missingness across the variables. Globally, we evaluated the missing completely at random (MCAR) assumption with Little’s MCAR test. Afterwards, we tested the missing data mechanism of each variable with a regression-based approach. We imputed the missing values when MCAR or missing at random (MAR) assumption is reasonable.
Statistical Power Analysis
There is no well-established power calculation for case–cohort studies with continuous predictors and non-rare events. Therefore, we used the standard power method for case–control studies. For this method, we used type I error rate of 0.05 and the values of three predictors of AD risk of André et al. [19]. Since the variables were standardized beforehand, we assumed them to be normally distributed with 0 mean and a standard deviation of 1. The dementia-associated adjusted odds ratio of the main predictor was 1.3 and the two covariates were 1.09 and 0.98. We independently included sample size and proportion of events for the ACD and AD. The power of the n = 805 ACD case–cohort was 91% and for the n = 740 AD case–cohort was 76%. Indeed, a sample size of n = 577 and n = 809 would produce the conventionally acceptable power (≥ 80%) for the ACD and AD case–cohorts, respectively. Considering that this standard power method has been shown to produce conservative estimates for case–cohort studies with non-rare events and binary predictors [47], it is likely that the actual power of our study samples would be higher.
Multivariable Regression Analysis
Continuous and categorical predictors were standardized and dummy coded, respectively. To estimate the association of the primary predictors (gut microbiome molecules and inflammatory markers) adjusted for covariates with ACD and AD risk, we adopted one of the recommended multivariable statistical approaches for analyzing case–cohort data, which comprises an initial variable selection step in binary outcome analysis with logistic regression followed by time-to-event analysis with weighted Cox proportional hazards (Cox PH) regression [48]. In the current variable selection step, we used three methods, the parametric adaptive Least Absolute Shrinkage and Selection Operator (aLASSO) logistic regression with 10-fold cross-validation, the random forest–based Boruta algorithm (RF-Boruta), and the recursive feature elimination implemented using Naïve Bayes algorithm (RFE-NB) with 10-fold cross-validation. These methods help to capture all (linear, non-linear, and interactions) complex inter-relationships among the predictors so that those that robustly discriminate dementia cases from non-cases are recovered. It also reduces potentially exaggerating the strength of associations of the multiple primary predictors with dementia risk and over-adjustment for covariates in the time-to-dementia models. Predictors with non-zero coefficients from the aLASSO logistic regression, predictors confirmed as important from the RF-Boruta, and optimal features from the RFE-NB were considered as the true relevant predictors of dementia. These true relevant predictors were used to estimate time-to-ACD and time-to-AD. We fitted Self-Prentice weighted Cox PH and checked for the PH assumption. The continuous predictors that violated the PH assumption were included with their time-varying form, while categorical predictors were handled by stratification of their baseline hazard function leading to no estimates for them. In addition, we fitted the accelerated failure time (AFT) models with weighted least-squares approach.
Bias Analysis
If any main predictor is significantly associated with time-to-dementia in the Cox PH, we estimated the strength of association (E-value) [49] on the risk ratio scale that unmeasured confounder(s) would need to have with both the predictor and dementia risk to completely explain away the predictor–dementia risk association, conditional on the measured covariates. Furthermore, by excluding early (first year of follow-up) incident cases, we addressed reverse causality in which the long prodromal phase and premorbid (subclinical) dementia might have directly altered the levels of these biomarkers rather than the reverse.
All probabilities were two-sided and significant level was set at P < 0.05. Statistical analyses were performed using R version 4.2.1.
Results
Descriptive Analysis
Tables 1 and 2 summarize the baseline characteristics of the n = 805 ACD and n = 740 AD study populations with 281 (35%) cases and 151 (20%) cases, respectively. About two-thirds were women with median age and BMI of 83 years and 25 kg/m2, respectively. Around 77% were physically active, about 5% were current smokers, mild alcohol consumers, and had normal MMSE score. Cases for both dementia outcomes were more likely to be women, older, more likely to be APOE-ɛ4 carriers, less physically active, less likely to be married, more likely to live alone, and had lower MMSE score. AD cases also had lower BMI. In addition, cases had higher IBA and lower 5OH-IAA (Table 3).
Multivariable Modeling of the Association of Gut Microbiome Molecules and Inflammatory Markers with Dementia Risk
Some primary predictors are intercorrelated, highest between IAG and IPA, and between 2-methylbutyric acid with isobutyric acid and isovaleric acid (Table A.1). Furthermore, at least one primary predictor was associated with a covariate, with the largest proportion of the primary predictors associated with tryptophan and study center (Table A.1 and Table A.2).
Handling of Missingness
The proportion of missingness was low to moderate, between 0.1 and 6.8% in the ACD case–cohort and between 0.1 and 7.2% in the AD casecohort (Table A.3). For the ACD case–cohort, VA, PA, BA, HA, marital status, and smoking status were MAR, while other variables were MCAR. For the AD case–cohort, VA, BA, marital status, and smoking status were MAR, while other variables were MCAR (Table A.3). Although the global MCAR assumption was not significant for both datasets (P = <0.001), the fact that the predictors were a mix of MCAR and MAR suggests that the MAR assumption is optimally appropriate for both datasets. Hence, missing values were imputed using the non-parametric multivariate imputation by the chained random forest weighted by the number of non-missing values per observation.
Multivariable Regression Analysis
All-Cause Dementia
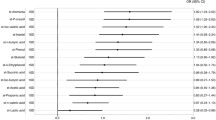
The 13 (eight positive and five negative) non-zero predictors from the aLASSO logistic regression were age, sex, heterozygous APOE-ɛ4 vs. none, homozygous APOE-ɛ4 vs none, MMSE score, family history of dementia, physically active vs. inactive, prevalent visual impairment, prevalent stroke, TBI, medication use, serotonin, and study center Düsseldorf vs. Bonn (Fig. 1A). The RF-Boruta confirmed eight important predictors, 5OH-IAA, IBA, 2-methylbutyric acid, age, sex, MMSE, heterozygous APOE-ɛ4 vs. none, and serotonin (Fig. 1B). The RFE-NB showed that a four-predictor model with age, sex, MMSE score, and 5OH-IAA optimally discriminates ACD cases from non-cases (Fig. 1C). Overall, 16 true relevant predictors discriminated ACD cases from non-cases. These were three gut microbiome molecules (5OH-IAA, IBA, 2-methylbutyric acid) and 13 covariates (age, sex, homozygous APOE-ɛ4 vs none, heterozygous APOE-ɛ4 vs. none, MMSE score, family history of dementia, physical active vs. inactive, prevalent visual impairment, prevalent stroke, history of TBI, medication, serotonin, and study center Düsseldorf vs. Bonn).
The true relevant predictors of all-cause dementia risk obtained from adaptive Least Absolute Shrinkage and Selection Operator logistic regression (green: positively associated predictors, red: negatively associated predictors) (A), random forest–based Boruta algorithm (Importance = median, minimum, and maximum z-scores of importance computed over multiple iterations) (B), and recursive feature elimination implemented using Naïve Bayes algorithm (Importance = area under the ROC curve (AUC) score importance) (C)
The Cox PH model with the aforementioned true relevant predictors showed that the whole model (P = <0.001), homozygous APOE-ɛ4 vs none (P = <0.001), MMSE score (P = <0.001), and serotonin (P = 0.02) violated the PH assumption. Consequently, we fitted the Cox PH model comprising the original predictors, the time-dependent MMSE score and serotonin, and stratification of the baseline hazard function for homozygous APOE-ɛ4 vs none. The result showed that over time, a one-SD increase in 5OH-IAA is significantly associated with a constant 42% decrease ACD risk (adjusted hazard ratio (HR) 0.58; 95% confidence interval (CI): 0.36 to 0.94, P = 0.025) (Fig. 2A). In line with the Cox PH model, the AFT model with the true relevant predictors showed that for each one-SD increase in 5OH-IAA, the logarithm of ACD survival time significantly increases by 0.21 (adjusted coefficient 0.21; 95% CI 0.02 to 0.40, P = 0.03) years (Fig. 2B). Other significant predictors of time-to-ACD were age, sex, homozygous APOE-ɛ4 vs none, heterozygous APOE-ɛ4 vs. none, MMSE score, physical active vs. inactive, TBI, and serotonin.
Bias Analysis
The E-values for 5OH-IAA were 2.27 and 1.27 for its adjusted HR of 0.58 (risk ratio, RR of 0.69) and upper CI of 0.94 (RR of 0.95), respectively. The observed adjusted HR of 0.58 could be explained away by an unmeasured confounder that is associated with both 5OH-IAA and time-to-ACD risk by a RR of 2.27-fold each, beyond the measured confounders, but weaker confounding could not do so. Furthermore, the upper CI could be moved to include one by an unmeasured confounder that was associated with both 5OH-IAA and time-to-ACD risk by a RR of 1.27-fold each, above and beyond the measured confounders, but weaker confounding could not do so. In addition, the association between 5OH-IAA and time-to-ACD risk was robust to the exclusion of cases within the first 1 year of follow-up, making it unlikely that the result is explained by reverse causality (Table A.4).
Alzheimer’s Disease Dementia
The 12 (six positive and six negative) non-zero predictors from aLASSO logistic regression were IAG, age, sex, MMSE score, homozygous APOE-ɛ4 vs none, heterozygous APOE-ɛ4 vs. none, married vs single, widowed vs. single, prevalent stroke vs. not, physical active vs. inactive, Düsseldorf vs. Bonn, and Munich vs. Bonn (Fig. 3A). The RF-Boruta confirmed 10 important predictors, ILA, IAA ME, isobutyric acid, 2-methylbutyric acid, age, MMSE score, homozygous APOE-ɛ4 vs none, widowed vs. single, serotonin, and tryptophan, as discriminating AD cases from non-cases (Fig. 3B). The RFE-NB showed that a four-predictor model with age, MMSE score, married vs single, widowed vs. single optimally discriminates AD cases from non-cases (Fig. 3C). Overall, 18 true relevant predictors discriminated AD cases from non-cases. This included five gut microbiome molecules (IAG, ILA, IAA ME, isobutyric acid, 2-methylbutyric acid) and 13 covariates (age, sex, MMSE score, homozygous APOE-ɛ4 vs none, heterozygous APOE-ɛ4 vs. none, married vs single, widowed vs. single, serotonin, tryptophan, prevalent stroke vs. not, physical active vs. inactive, study center Düsseldorf vs. Bonn, and study center Munich vs. Bonn). However, none of the four inflammatory markers discriminated AD cases from non-cases.
The true relevant predictors of Alzheimer’s disease dementia risk obtained from adaptive Least Absolute Shrinkage and Selection Operator logistic regression (green: positively associated predictors, red: negatively associated predictors) (A), random forest–based Boruta algorithm (Importance = median, minimum, and maximum z-scores of importance computed over multiple iterations) (B), and recursive feature elimination implemented using Naïve Bayes algorithm (Importance = area under the ROC curve (AUC) score importance) (C)
The Cox PH model with the aforementioned true relevant predictors showed that the whole model (global test, P = <0.001), IAG (P = <0.001), and homozygous APOE-ɛ4 vs none (P = <0.001) violated the PH assumption. Consequently, we fitted the Cox PH model comprising the original predictors, time-dependent IAG, and stratification of the baseline hazard function for homozygous APOE-ɛ4 vs none. We observed that none of the primary predictors was associated with time-to-AD in the Cox PH (Fig. 4A) and AFT models (Fig. 4B). Consequently, no bias analysis was performed for AD. The significant predictors of time-to-AD were age, homozygous APOE-ɛ4 vs none, heterozygous APOE-ɛ4 vs. none, MMSE score, physical active vs. inactive, and study center Düsseldorf vs. Bonn.
Discussion
The present epidemiological study leveraging a unique multicenter German cohort explored the relationship between the plasma levels of 19 gut microbiome molecules and four inflammatory markers and the risk of incident dementia. There were three observations. Firstly, seven (three ACD-related: 5OH-IAA, IBA, and 2-methylbutyric acid and five AD-related: IAG, ILA, IAA ME, isobutyric acid, and 2-methylbutyric acid) gut microbiome molecules discriminated incident dementia cases from non-cases. Secondly, decreased 5OH-IAA level was associated with elevated time-to-ACD. Thirdly, there was no association between inflammatory markers and the risk of either ACD or AD.
The relationship between IBA, IAG, ILA, and IAA ME and either ACD or AD risk has not been reported previously. Hence, the current study adds to the body of literature. Our observed relationship between 2-methylbutyric acid and AD risk is in consort with Wu et al. where fecal 2-methylbutyric acid was associated with AD risk in 55 individuals [22]. 2-Methylbutyric acid is a branched SCFA produced by microbial fermentation of isoleucine [50]. Another AD-related branched SCFA, isobutyric acid is produced by microbial fermentation of valine [50]. Isobutyric acid was previously associated with ACD [16]. Bacteroides, Propionibacterium, Bacillus, Lactobacillus, Clostridium, and Escherichia coli produce isobutyric acid and 2-methylbutyric acid [50]. The potential explanation for their relationship with dementia is that SCFAs modulate microglial activation, although the exact signaling pathways are not fully understood [51]. SCFAs also stimulate the expression of aryl hydrocarbon receptor (AhR) factors [52].
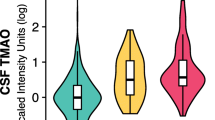
The first indole-containing tryptophan metabolite, ILA is secreted by Bifidobacterium infantis [53] and Lactilactobacillus species [54], functioning as a potent activator of human AhR signaling [52]. The second, IBA is a precursor of IAA [55] produced by Bifidobacterium, Lactilactobacillus, Clostridium, and Bacteroides [54]. Furthermore, IAA ME is a metabolite of IAA produced by Pseudomonas amygdali [56] and IAG is synthesized from microbial tryptophan metabolism and host glycine conjugation [57]. The last, 5OH-IAA is the most compelling finding, as it was associated with time-to-ACD independent of several covariates and robust against bias. 5OH-IAA was previously associated with AD [23, 24]. Possible explanation for 5OH-IAA is that it is an agonist for AhR signaling [52, 58,59,60] and prevents the formation of amyloid beta plaques [61]. Thus, its low circulating levels suggest a reduction in these dementia-preventing properties. 5OH-IAA is synthesized mainly in the kidney and liver as the final serotonin catabolite in a two-step reaction, involving monoamine oxidase and aldehyde dehydrogenase [62]. Besides, it functions in the indole pathway [63]. Some gut bacteria such as Pseudomonas [64, 65] also directly synthesize its serotonin precursor. It is therefore unsurprising that 5OH-IAA is highly associated with the gut microbiome [66] and an emerging gut microbiome molecule [58,59,60, 67]. Interestingly, alteration in this host–gut microbiome co-molecule is implicated in neuropsychiatric conditions such as depression [67], epilepsy [68], and schizophrenia [69]. This suggests that the comorbidity of these conditions with dementia [70] may be partly underlined by the gut microbiome and 5OH-IAA.
Surprisingly, the gut microbiome de novo synthesized LPS and a measure of its long-term exposure (LBP) was not related to either ACD or AD. This is in contrast to the association of plasma LPS in 36 individuals [18] and plasma LBP in 636 individuals [19] with AD as well as the independent association of plasma LPS with cognitive decline in 127 individuals [71]. Moreover, other previously reported ACD-related gut microbiome molecules were saliva AA and PA in 51 individuals [15], fecal isovaleric acid in 107 individuals [16], and plasma IS in 24 individuals [17]. While Zhang et al. [18] was independent of age, André et al. [19] and Figueira et al. [15] were independent of a few covariates, Saji et al. [16] was not significant after adjusting for covariates, and Teruya et al. [17] was unadjusted for covariates. In addition, PA [21, 22] and 5OH-IAA [23, 24] have been consistently associated with AD, independent of age and sex. Yilmaz et al. observed the association in the saliva of 21 individuals [21], Wu et al. in the feces of 55 individuals [22]. Whiley et al. in the urine of 556 individuals [23], and Baker et al. in the brain of 25 individuals [24]. The fact most of the aforementioned molecules were not related to either ACD or AD suggests that the discrepancy between our findings and others is likely attributable to underlying differences in the study populations and methodologies. Moreover, the absence of association of any molecule with time-to-AD is unlikely due to statistical power since time-to-event analysis has greater statistical power than binary outcome analysis [72].
Unexpectedly, inflammatory markers, CRP, IL-1β, IL-6, and TNF-α did not discriminate dementia cases from non-cases. The absence of their association with dementia risk is unlikely to be due to intercorrelation of the markers, which is low, or covariate adjustment, since none was associated with dementia in the unadjusted analysis. This finding is in consort with recent reports [19, 29,30,31]. Two studies like ours investigated both ACD and AD [27, 29]. While the meta-analysis showed that CRP and IL-6 are associated with ACD and CRP with AD [27], the more recent study [29] did not observe an association of CRP with either ACD or AD. Considering that most recent studies [19, 30, 31] did not observe an association with other inflammatory markers casts doubt on the independent association between the circulating levels of this set of inflammatory markers and dementia risk. Nevertheless, this does not preclude the potential role of other inflammatory markers since systemic inflammation is the primary cause of BBB damage and often precedes dementia pathologies [73].
It is noteworthy that we confirmed previously reported determinants of dementia such as age [74], sex [16, 74], APOE-ɛ4 [16, 74, 75], MMSE [16, 22], and physical inactivity [2, 75]. In fact, we observed that age, sex, APOE-ɛ4, and MMSE were independent predictors of time-to-dementia risk. Additionally, our objectively measured habitual diet proxies that were negligible predictors of dementia agree with recent inconclusive evidence linking diet to dementia risk [76,77,78]. Furthermore, there are indications that the association between diet and dementia risk is driven by cardiovascular risk factors [2]. Since we adjusted for cardiovascular risk factors, it is likely that residual confounding by diet would be trivially small, despite SCFA and indole-containing tryptophan metabolites being diet-dependent. Furthermore, APOE-ɛ4 is a strong determinant of dementia and interacts with other risk factors [74]. Adjusting for APOE-ɛ4 status as a three-group variable ensures that its influence and related factors are properly accounted for.
There are several strengths of this study. It is a multicenter study; as such, these findings are generalizable to the broader German population. It is also one of the largest studies linking this set of biomarkers to dementia risk. Our analyses are sufficiently powered to produce valid and reliable results. Standardization of all continuous predictors reduces the impact of variation in the molecules and inflammatory markers thereby facilitating their comparison. Furthermore, our multivariable analysis ensured that we accounted for most of the inter-relationships among the molecules and inflammatory markers, covariates, and dementia risk. Our reporting of the effect estimates of primary predictors and covariates will improve the statistical power estimation of future studies. Finally, the case–cohort design affords the use of the subcohort for other health conditions since it is not case-matched. While this study is hypothesis-driven and yielded scientifically interesting and biologically plausible findings, it is important to acknowledge its limitations. This is an observational study; thus, it does not prove causal relationship between these molecules and dementia risk. Indeed, the potential causal relationship of 5OH-IAA with ACD risk may be explored by linking genetically predicted levels of 5OH-IAA with ACD risk in Mendelian randomization analysis. Besides, our finding may be different in other biospecimen. However, this seems unlikely for 5OH-IAA since there is a good agreement of its plasma, serum, and urine levels [60]. Moreover, we reported the impact of reverse causality and the strength of unmeasured confounders that are likely to explain away our findings. Despite these bias analyses and extensive adjustment for covariates, our results could still be biased due to measurement error and the use of two categories for some covariates. Our limited sample size precludes an intermediate step of internally validating and assessing the potential clinical utility of the true relevant predictors in a holdout dataset. Our findings should be confirmed in other studies, particularly in larger well-characterized and harmonized multicenter studies with broader microbiome metabolomics and a larger set of inflammatory markers. Since the levels of some of these dementia-related molecules are time-dependent [33], the relationship between their repeatedly measured levels and dementia risk should be investigated. Indeed, the AD-related molecules are interesting candidates to thoroughly elucidate in future biomarker-based research.
Conclusion
In a relatively large cohort of older Germans, we observed that circulating concentrations of seven gut microbiome molecules are related to dementia risk, of which 5OH-IAA is associated with long-term ACD risk. These molecules underpin gut microbiome-host interactions in dementia occurrence. The modulation of these molecules such as through direct supplemental intake and probiotic consumption of their synthesizing bacteria may be crucially relevant in dementia’s multifactorial risk prevention and intervention strategies.
Data Availability
The datasets generated during and/or analyzed during the current study are available from the corresponding author on reasonable request and subsequent approval of the principal coordinators of the AgeCoDe study.
Abbreviations
- AD:
-
Alzheimer’s disease dementia
- ACD:
-
all-cause dementia
- HbA1c:
-
hemoglobin A1c
- LPS:
-
lipopolysaccharide
- SCFA:
-
short-chain fatty acids
- BBB:
-
blood-brain barrier
- AA:
-
acetic acid
- PA:
-
propionic acid
- BA:
-
butyric acid
- HA:
-
hexanoic acid
- IS:
-
indoxyl sulfate
- LBP:
-
LPS-binding protein
- 5OH-IAA:
-
5-hydroxyindole-3-acetic acid
- IAA:
-
indole-3-acetic acid
- IACR:
-
indoleacrylic acid
- CRP:
-
C-reactive protein
- IL:
-
interleukin
- TNF-α:
-
tumor necrosis factor-alpha
- AgeCoDe:
-
German study on Ageing, Cognition, and Dementia in Primary Care Patients
- BMI:
-
body mass index
- CV:
-
coefficient of variation
- IAA ME:
-
indole-3-acetic acid methyl ester
- IPA:
-
indole-3-propionic acid
- IBA:
-
indole-3-butyric acid
- ILA:
-
indole-3-lactic acid
- ICARB:
-
indole-3-carboxaldehyde
- IAG:
-
indole-3-acryloylglycine
- DSM:
-
Diagnostic and Statistical Manual of Mental Disorders
- SIDAM:
-
Structured Interview for Diagnosis of Dementia of Alzheimer type, Multi-infarct Dementia and Dementia of other etiology according to DSM-IV and ICD-10
- DAG:
-
directed acyclic graph
- MMSE:
-
Mini-Mental State Examination
- APOE:
-
apolipoprotein E
- TBI:
-
traumatic brain injury
- MCAR:
-
missing completely at random
- MAR:
-
missing at random
- Cox PH:
-
cox proportional hazards
- aLASSO:
-
adaptive Least Absolute Shrinkage and Selection Operator
- RF-Boruta:
-
random forest–based Boruta algorithm
- RFE-NB:
-
recursive feature elimination implemented using Naïve Bayes algorithm
- AFT:
-
accelerated failure time
- SD:
-
standard deviation
- HR:
-
hazard ratio
- CI:
-
confidence interval
- RR:
-
risk ratio
References
WHO (2017) Global action plan on the public health response to dementia 2017–2025. World Health Organization, Geneva
Livingston G, Huntley J, Sommerlad A, Ames D, Ballard C, Banerjee S et al (2020) Dementia prevention, intervention, and care: 2020 report of the lancet commission. Lancet 396(10248):413–446
Alzheimer’s Association (2020) Alzheimer’s disease facts and figures. Alzheimers Dement 16:391–460
Sperling RA, Aisen PS, Beckett LA, Bennett DA, Craft S, Fagan AM et al (2011) Toward defining the preclinical stages of Alzheimer's disease: recommendations from the National Institute on Aging-Alzheimer's Association workgroups on diagnostic guide guidelines for Alzheimer's disease. Alzheimer's & Dementia: the journal of the Alzheimer's Association 7(3):280–292
Nichols E, Steinmetz JD, Vollset SE, Fukutaki K, Chalek J, Abd-Allah F et al (2022) Estimation of the global prevalence of dementia in 2019 and forecasted prevalence in 2050: an analysis for the global burden of disease study 2019. Lancet Public Health 7(2):e105–ee25
Needham BD, Kaddurah-Daouk R, Mazmanian SK (2020) Gut microbial molecules in behavioural and neurodegenerative conditions. Nat Rev Neurosci 21(12):717–731
Wu S, Liu X, Jiang R, Yan X, Ling Z (2021) Roles and mechanisms of gut microbiota in patients with Alzheimer’s disease. Front Aging Neurosci 13. https://doi.org/10.3389/fnagi.2021.650047
Pappolla MA, Perry G, Fang X, Zagorski M, Sambamurti K, Poeggeler B (2021) Indoles as essential mediators in the gut-brain axis. Their role in Alzheimer's disease. Neurobiol Dis 156:105403
Connell E, Le Gall G, Pontifex MG, Sami S, Cryan JF, Clarke G et al (2022) Microbial-derived metabolites as a risk factor of age-related cognitive decline and dementia. Mol Neurodegener 17(1):43
Mou Y, Du Y, Zhou L, Yue J, Hu X, Liu Y et al (2022) Gut microbiota interact with the brain through systemic chronic inflammation: implications on neuroinflammation, neurodegeneration, and aging. Front Immunol 13(796288). https://doi.org/10.3389/fimmu.2022.796288
Kumar P, Lee J-H, Lee J (2021) Diverse roles of microbial indole compounds in eukaryotic systems. Biol Rev 96(6):2522–2545
Dodd D, Spitzer MH, Van Treuren W, Merrill BD, Hryckowian AJ, Higginbottom SK et al (2017) A gut bacterial pathway metabolizes aromatic amino acids into nine circulating metabolites. Nature 551(7682):648–652
Wekerle H (2017) Brain autoimmunity and intestinal microbiota: 100 trillion game changers. Trends Immunol 38(7):483–497
Silva YP, Bernardi A, Frozza RL (2020) The role of short-chain fatty acids from gut microbiota in gut-brain communication. Front Endocrinol 11. https://doi.org/10.3389/fendo.2020.00025
Figueira J, Jonsson P, Nordin Adolfsson A, Adolfsson R, Nyberg L, Öhman A (2016) NMR analysis of the human saliva metabolome distinguishes dementia patients from matched controls. Mol BioSyst 12(8):2562–2571
Saji N, Murotani K, Hisada T, Kunihiro T, Tsuduki T, Sugimoto T et al (2020) Relationship between dementia and gut microbiome-associated metabolites: a cross-sectional study in Japan. Sci Rep 10(1):8088
Teruya T, Chen Y-J, Kondoh H, Fukuji Y, Yanagida M (2021) Whole-blood metabolomics of dementia patients reveal classes of disease-linked metabolites. Proc Natl Acad Sci 118(37):e2022857118
Zhang R, Miller RG, Gascon R, Champion S, Katz J, Lancero M et al (2009) Circulating endotoxin and systemic immune activation in sporadic amyotrophic lateral sclerosis (sALS). J Neuroimmunol 206(1–2):121–124
André P, Samieri C, Buisson C, Dartigues JF, Helmer C, Laugerette F et al (2019) Lipopolysaccharide-binding protein, soluble CD14, and the long-term risk of Alzheimer's disease: a nested case-control pilot study of older community dwellers from the Three-City cohort. Journal of Alzheimer's disease: JAD 71(3):751–761
Botosoa EP, Zhu M, Marbeuf-Gueye C, Tribaa MN, Dutheil F, Duyckäerts C et al (2012) NMR metabolomic of frontal cortex extracts: first study comparing two neurodegenerative diseases, Alzheimer disease and amyotrophic lateral sclerosis. IRBM 33:281–286
Yilmaz A, Geddes T, Han B, Bahado-Singh RO, Wilson GD, Imam K et al (2017) Diagnostic biomarkers of Alzheimer's disease as identified in saliva using 1H NMR-based metabolomics. Journal of Alzheimer's disease: JAD 58(2):355–359
Wu L, Han Y, Zheng Z, Peng G, Liu P, Yue S et al (2021) Altered gut microbial metabolites in amnestic mild cognitive impairment and Alzheimer's disease: signals in host-microbe interplay. Nutrients 13(1). https://doi.org/10.3390/nu13010228
Whiley L, Chappell KE, D’Hondt E, Lewis MR, Jiménez B, Snowden SG et al (2021) Metabolic phenotyping reveals a reduction in the bioavailability of serotonin and kynurenine pathway metabolites in both the urine and serum of individuals living with Alzheimer’s disease. Alzheimers Res Ther 13(1):20
Baker GB, Reynolds GP (1989) Biogenic amines and their metabolites in Alzheimer's disease: noradrenaline, 5-hydroxytryptamine and 5-hydroxyindole-3-acetic acid depleted in hippocampus but not in substantia innominata. Neurosci Lett 100(1):335–339
Laakso MP, Jukarainen NM, Vepsalainen J (2015) Diagnosis of dementias by high-field H-1 MRS of cerebrospinal fluid. J Neurol Neurosur Psychiatry 86:1286–1290
Tohgi H, Abe T, Takahashi S, Kimura M, Takahashi J, Kikuchi T (1992) Concentrations of serotonin and its related substances in the cerebrospinal fluid in patients with Alzheimer type dementia. Neurosci Lett 141(1):9–12
Koyama A, O'Brien J, Weuve J, Blacker D, Metti AL, Yaffe K (2013) The role of peripheral inflammatory markers in dementia and Alzheimer's disease: a meta-analysis. J Gerontol A Biol Sci Med Sci 68(4):433–440
Zheng C, Zhou X-W, Wang J-Z (2016) The dual roles of cytokines in Alzheimer’s disease: update on interleukins, TNF-α, TGF-β and IFN-γ. Transl Neurodegener 5(1):7
van Himbergen TM, Beiser AS, Ai M, Seshadri S, Otokozawa S, Au R et al (2012) Biomarkers for insulin resistance and inflammation and the risk for all-cause dementia and Alzheimer disease: results from the Framingham heart study. Arch Neurol 69(5):594–600
Gong C, Wei D, Wang Y, Ma J, Yuan C, Zhang W et al (2016) A meta-analysis of C-reactive protein in patients with Alzheimer's disease. Am J Alzheimers Dis Other Dement 31(3):194–200
Ng A, Tam WW, Zhang MW, Ho CS, Husain SF, McIntyre RS et al (2018) IL-1β, IL-6, TNF- α and CRP in elderly patients with depression or Alzheimer's disease: systematic review and meta-analysis. Sci Rep 8(1):12050
Cussotto S, Delgado I, Anesi A, Dexpert S, Aubert A, Beau C et al (2020) Tryptophan metabolic pathways are altered in obesity and are associated with systemic inflammation. Front Immunol 11:557
Oluwagbemigun K, Anesi A, Ulaszewska M, Clarke G, Alexy U, Schmid M et al (2020) Longitudinal relationship of amino acids and indole metabolites with long-term body mass index and cardiometabolic risk markers in young individuals. Sci Rep 10(1):6399
Lin R, Zhang Y, Chen L, Qi Y, He J, Hu M et al (2020) The effects of cigarettes and alcohol on intestinal microbiota in healthy men. J Microbiol 58(11):926–937
Hakoupian M, Ferino E, Jickling GC, Amini H, Stamova B, Ander BP et al (2021) Bacterial lipopolysaccharide is associated with stroke. Sci Rep 11(1):6570
Gaïni S, Koldkjær OG, Pedersen C, Pedersen SS (2006) Procalcitonin, lipopolysaccharide-binding protein, interleukin-6 and C-reactive protein in community-acquired infections and sepsis: a prospective study. Crit Care 10(2):R53
Morris G, Berk M, Carvalho A, Caso JR, Sanz Y, Walder K et al (2017) The role of the microbial metabolites including tryptophan catabolites and short chain fatty acids in the pathophysiology of immune-inflammatory and neuroimmune disease. Mol Neurobiol 54(6):4432–4451
Aust A-C, Benesova E, Vidova V, Coufalikova K, Smetanova S, Borek I et al (2021) Profiling tryptophan catabolites of human gut microbiota and acute-phase protein levels in neonatal dried blood specimens. Front Microbiol 12(665743). https://doi.org/10.3389/fmicb.2021.665743
Ramirez A, Wolfsgruber S, Lange C, Kaduszkiewicz H, Weyerer S, Werle J et al (2015) Elevated HbA1c is associated with increased risk of incident dementia in primary care patients. J Alzheimers Dis 44:1203–1212
Cologne J, Preston DL, Imai K, Misumi M, Yoshida K, Hayashi T et al (2012) Conventional case–cohort design and analysis for studies of interaction. Int J Epidemiol 41(4):1174–1186
Anesi A, Rubert J, Oluwagbemigun K, Orozco-Ruiz X, Nöthlings U, Breteler MMB et al (2019) Metabolic profiling of human plasma and urine, targeting tryptophan, tyrosine and branched chain amino acid pathways. Metabolites 9(11):261
Lotti C, Rubert J, Fava F, Tuohy K, Mattivi F, Vrhovsek U (2017) Development of a fast and cost-effective gas chromatography–mass spectrometry method for the quantification of short-chain and medium-chain fatty acids in human biofluids. Anal Bioanal Chem 409(23):5555–5567
Zaudig M, Hiller W (1996) SIDAM – a structured interview for the diagnosis of dementia of the Alzheimer type, multi-infarct (or vascular) dementia and dementias of other aetiology according to DSM-III-R, DSM-IV and ICD-10 (SIDAM-manual) [in German]. Huber, Bern
McKhann G, Drachman D, Folstein M, Katzman R, Price D, Stadlan EM (1984) Clinical diagnosis of Alzheimer's disease: report of the NINCDS-ADRDA work group under the auspices of Department of Health and Human Services Task Force on Alzheimer's disease. Neurology. 34(7):939–944
Román GC, Tatemichi TK, Erkinjuntti T, Cummings JL, Masdeu JC, Garcia JH et al (1993) Vascular dementia: diagnostic criteria for research studies. Report of the NINDS-AIREN international workshop. Neurology 43(2):250–260
Schmidt JA, Rinaldi S, Scalbert A, Ferrari P, Achaintre D, Gunter MJ et al (2016) Plasma concentrations and intakes of amino acids in male meat-eaters, fish-eaters, vegetarians and vegans: a cross-sectional analysis in the EPIC-Oxford cohort. Eur J Clin Nutr 70(3):306–312
Kim MY, Xue X, Du Y (2006) Approaches for calculating power for case–cohort studies. Biometrics 62(3):929–933
Staley JR, Jones E, Kaptoge S, Butterworth AS, Sweeting MJ, Wood AM et al (2017) A comparison of cox and logistic regression for use in genome-wide association studies of cohort and case–cohort design. Eur J Hum Genet 25(7):854–862
VanderWeele TJ, Ding P (2017) Sensitivity analysis in observational research: introducing the E-value. Ann Intern Med 167(4):268–274
Salazar N, González S, de los Reyes Gavilan CG, Rios-Covian D, (2022) Branched short-chain fatty acids as biological indicators of microbiota health and links with anthropometry. In: Patel VB, Preedy VR (eds) Biomarkers in nutrition. Springer International Publishing, Cham, pp 1–17
Xie J, Van Hoecke L, Vandenbroucke RE (2022) The impact of systemic inflammation on Alzheimer’s disease pathology. Front Immunol 1212(796867). https://doi.org/10.3389/fimmu.2021.796867
Salminen A (2023) Activation of aryl hydrocarbon receptor (AhR) in Alzheimer's disease: role of tryptophan metabolites generated by gut host-microbiota. J Mol Med (Berlin, Germany) 101(3):201–222
Evidente A, Iacobellis NS, Sisto A (1993) Isolation of indole-3-acetic acid methyl ester, a metabolite of indole-3-acetic acid from pseudomonas amygdali. Experientia 49(2):182–183
Zhou Q, Xie Z, Wu D, Liu L, Shi Y, Li P et al (2022) The effect of indole-3-lactic acid from Lactiplantibacillus plantarum ZJ316 on human intestinal microbiota in vitro. Foods 11(20):3302
Agus A, Planchais J, Sokol H (2018) Gut microbiota regulation of tryptophan metabolism in health and disease. Cell Host Microbe 23(6):716–724
Meng D, Sommella E, Salviati E, Campiglia P, Ganguli K, Djebali K et al (2020) Indole-3-lactic acid, a metabolite of tryptophan, secreted by Bifidobacterium longum subspecies infantis is anti-inflammatory in the immature intestine. Pediatr Res 88(2):209–217
Hsiao EY, McBride SW, Hsien S, Sharon G, Hyde ER, McCue T et al (2013) Microbiota modulate behavioral and physiological abnormalities associated with neurodevelopmental disorders. Cell 155(7):1451–1463
Dong F, Hao F, Murray IA, Smith PB, Koo I, Tindall AM et al (2020) Intestinal microbiota-derived tryptophan metabolites are predictive of ah receptor activity. Gut Microbes 12(1):1–24
Swer NM, Venkidesh BS, Murali TS, Mumbrekar KD (2023) Gut microbiota-derived metabolites and their importance in neurological disorders. Mol Biol Rep 50(2):1663–1675
Rosser EC, Piper CJM, Matei DE, Blair PA, Rendeiro AF, Orford M et al (2020) Microbiota-derived metabolites suppress arthritis by amplifying aryl-hydrocarbon receptor activation in regulatory B cells. Cell Metab 31(4):837–51.e10
Dang G, Wen X, Zhong R, Wu W, Tang S, Li C et al (2023) Pectin modulates intestinal immunity in a pig model via regulating the gut microbiota-derived tryptophan metabolite-AhR-IL22 pathway. J Anim Sci Biotechnol 14(1):38
Ewang-Emukowhate M, Nair D, Caplin M (2019) The role of 5-hydroxyindoleacetic acid in neuroendocrine tumors: the journey so far. International journal of endocrine. Oncology 6(2):IJE17
Petersen A, Jokinen M, Plichta DR, Liebisch G, Gronwald W, Dettmer K et al (2021) Cytokine-specific autoantibodies shape the gut microbiome in autoimmune polyendocrine syndrome type 1. J Allergy Clin Immunol 148(3):876–888
Everett BA, Tran P, Prindle A (2022) Toward manipulating serotonin signaling via the microbiota–gut–brain axis. Curr Opin Biotechnol 78:102826
Kaur H, Bose C, Mande SS (2019) Tryptophan metabolism by gut microbiome and gut-brain-axis: an in silico analysis. Front Neurosci 13. https://doi.org/10.3389/fnins.2019.01365
Yu JS, Youn GS, Choi J, Kim C-H, Kim BY, Yang S-J et al (2021) Lactobacillus lactis and Pediococcus pentosaceus-driven reprogramming of gut microbiome and metabolome ameliorates the progression of nonalcoholic fatty liver disease. Clin Transl Med 11(12):e634
Liu L, Wang H, Chen X, Zhang Y, Zhang H, Xie P (2023) Gut microbiota and its metabolites in depression: from pathogenesis to treatment. EBioMedicine 90(104527). https://doi.org/10.1016/j.ebiom.2023.104527
Petrucci AN, Joyal KG, Purnell BS, Buchanan GF (2020) Serotonin and sudden unexpected death in epilepsy. Exp Neurol 325:113145
Ohuoha DC, Hyde TM, Kleinman JE (1993) The role of serotonin in schizophrenia: an overview of the nomenclature, distribution and alterations of serotonin receptors in the central nervous system. Psychopharmacology 112(1 Suppl):S5–S15
Hesdorffer DC (2016) Comorbidity between neurological illness and psychiatric disorders. CNS Spectrums 21(3):230–238
Saji N, Saito Y, Yamashita T, Murotani K, Tsuduki T, Hisada T et al (2022) Relationship between plasma lipopolysaccharides, gut microbiota, and dementia: a cross-sectional study. Journal of Alzheimer's Disease: JAD 86(4):1947–1957
George B, Seals S, Aban I (2014) Survival analysis and regression models. Journal of nuclear cardiology: official publication of the American Society of Nuclear Cardiology 21(4):686–694
Kinney JW, Bemiller SM, Murtishaw AS, Leisgang AM, Salazar AM, Lamb BT (2018) Inflammation as a central mechanism in Alzheimer's disease. Alzheimer's & Dementia (New York, N Y) 4:575–590
van der Flier WM, Scheltens P (2005) Epidemiology and risk factors of dementia. J Neurol Neurosurg Psychiatry 76(suppl 5):v2–v7
Luck T, Riedel-Heller SG, Luppa M, Wiese B, Köhler M, Jessen F et al (2014) Apolipoprotein E epsilon 4 genotype and a physically active lifestyle in late life: analysis of gene-environment interaction for the risk of dementia and Alzheimer's disease dementia. Psychol Med 44(6):1319–1329
Shannon OM, Ranson JM, Gregory S, Macpherson H, Milte C, Lentjes M et al (2023) Mediterranean diet adherence is associated with lower dementia risk, independent of genetic predisposition: findings from the UK biobank prospective cohort study. BMC Med 21(1):81
Townsend RF, Logan D, O’Neill RF, Prinelli F, Woodside JV, McEvoy CT (2023) Whole dietary patterns, cognitive decline and cognitive disorders: a systematic review of prospective and intervention studies. Nutrients 15(2):333
Glans I, Sonestedt E, Nägga K, Gustavsson A-M, González-Padilla E, Borne Y et al (2023) Association between dietary habits in midlife with dementia incidence over a 20-year period. Neurology 100(1):e28–e37
Acknowledgements
The authors would like to appreciate Dimitrios Moutopoulos and Michaela Thoenes and their colleagues involved in sample retrieval and processing and data management, Prof. Dr. Sabine Ellinger for laboratory infrastructural support, Petra Pickert for the enormous work of aliquoting and further processing of samples, Stefan Benda for formatting of the figures, and Dr. Kathrin Heser for the additional comments. A very special thanks to the wonderful Oreoluwa Hans Oluwagbemigun for his amazing support. We also sincerely thank all participating patients and their general practitioners for their invaluable contribution to the AgeCoDe study.
Funding
Open Access funding enabled and organized by Projekt DEAL. This study is part of the German Research Network on Dementia (KND), the German Research Network on Degenerative Dementia (KNDD; German Study on Ageing, Cognition and Dementia in Primary Care Patients; AgeCoDe), and the Health Service Research Initiative (Study on Needs, health service use, costs and health-related quality of life in a large sample of oldest-old primary care patients (85+; AgeQualiDe)) and was funded by the German Federal Ministry of Education and Research (grants KND: 01GI0102, 01GI0420, 01GI0422, 01GI0423, 01GI0429, 01GI0431, 01GI0433, 01GI0434; grants KNDD: 01GI0710, 01GI0711, 01GI0712, 01GI0713, 01GI0714, 01GI0715, 01GI0716; grants Health Service Research Initiative: 01GY1322A, 01GY1322B, 01GY1322C, 01GY1322D, 01GY1322E, 01GY1322F, 01GY1322G). The measurement of the current sets of biomakers and K.O are supported by the German Research Foundation (Deutsche Forschungsgemeinschaft, DFG) under the grant number 460591722.
Author information
Authors and Affiliations
Contributions
Kolade Oluwagbemigun designed the study, performed all statistical analyses, and wrote the first draft of the manuscript. Michael Pentzek, Martin Scherer, Steffi G. Riedel-Heller, Siegfried Weyerer, Horst Bickel, Birgitt Wiese, Alfredo Ramirez, and Michael Wagner are the principal investigators of the AgeCoDe study responsible for the study participants’ recruitment and data and biosample collection and storage. Pamela Martino Adami extracted and provided the raw baseline data for the present study sample. Ute Nöthlings, Alfredo Ramirez, and Michael Wagner supervised and provided input on the study. Andrea Anesi, Urska Vrhovsek, and Fulvio Mattivi performed the measurement of the SCFA and indole-containing tryptophan metabolites. Matthias Schmid provided statistical support. John F. Cryan supported the research idea. All authors commented on previous versions of the manuscript. All authors read and approved the final manuscript.
Corresponding author
Ethics declarations
Ethics Approval
This study was performed in line with the principles of the Declaration of Helsinki. Approval was granted by the Ethics Commission of the University of Bonn 050/02, 258/07; the Ethics Commission of the Medical Faculty of the Heinrich Heine University Düsseldorf 2079/2002, 2999/2008; the Ethics Commission of the Medical Association Hamburg OB/08/02, 2817/2007; and the Ethics Commission at the Medical Center of the University of Leipzig 143/2002, 309/2007. The ethical approval for the present biomarker analysis was obtained from the Ethics Commission of the University of Bonn 245/22.
Consent to Participate
Informed consent was obtained from all individuals included in the study.
Consent for Publication
Not applicable.
Competing Interests
The authors have no competing interests to declare that are relevant to the content of this article.
Additional information
Publisher’s Note
Springer Nature remains neutral with regard to jurisdictional claims in published maps and institutional affiliations.
Supplementary information
ESM 1
(XLSX 87 kb)
Rights and permissions
Open Access This article is licensed under a Creative Commons Attribution 4.0 International License, which permits use, sharing, adaptation, distribution and reproduction in any medium or format, as long as you give appropriate credit to the original author(s) and the source, provide a link to the Creative Commons licence, and indicate if changes were made. The images or other third party material in this article are included in the article's Creative Commons licence, unless indicated otherwise in a credit line to the material. If material is not included in the article's Creative Commons licence and your intended use is not permitted by statutory regulation or exceeds the permitted use, you will need to obtain permission directly from the copyright holder. To view a copy of this licence, visit http://creativecommons.org/licenses/by/4.0/.
About this article
Cite this article
Oluwagbemigun, K., Anesi, A., Vrhovsek, U. et al. An Investigation into the Relationship of Circulating Gut Microbiome Molecules and Inflammatory Markers with the Risk of Incident Dementia in Later Life. Mol Neurobiol (2023). https://doi.org/10.1007/s12035-023-03513-6
Received:
Accepted:
Published:
DOI: https://doi.org/10.1007/s12035-023-03513-6