Abstract
Abnormal calcium homeostasis, activation of protease calpain, generation of p25 and hyperactivation of cyclin-dependent kinase 5 (Cdk5) have all been implicated in the pathogenesis of neurogenerative diseases including Alzheimer’s disease. We have recently shown that extracellular cold-inducible RNA-binding protein (eCIRP) induces Cdk5 activation via p25. However, the precise molecular mechanism by which eCIRP regulates calcium signaling and calpain remains to be addressed. We hypothesized that eCIRP regulates p25 via Ca2+-dependent calpain activation. eCIRP increased calpain activity and decreased the endogenous calpain inhibitor calpastatin in Neuro 2a (N2a) cells. Calpain inhibition with calpeptin attenuated eCIRP-induced calpain activity and p25. eCIRP specifically upregulated cytosolic calpain 1, and calpain 1 silencing attenuated the eCIRP-induced increase in p25. eCIRP stimulation increased cytosolic free Ca2+, especially in hippocampal neuronal HT22 cells, which was attenuated by the eCIRP inhibitor Compound 23 (C23). Endoplasmic reticulum (ER) inositol 1,4,5-trisphosphate receptor (IP3R) inhibition using 2-aminoethoxy-diphenyl-borate or xestospongin-C (X-C), interleukin-6 receptor alpha (IL-6Rα)-neutralization, and phospholipase C (PLC) inhibition with U73122 attenuated eCIRP-induced Ca2+ increase, while Ca2+ influx across the plasma membrane remained unaffected by eCIRP. Finally, C23, IL-6Rα antibody, U73122 and X-C attenuated eCIRP-induced p25 in HT-22 cells. In conclusion, the current study uncovers eCIRP-triggered Ca2+ release from ER stores in an IL-6Rα/PLC/IP3-dependent manner as a novel molecular mechanism underlying eCIRP’s induction of Cdk5 activity and potential involvement in neurodegeneration.










Similar content being viewed by others
Data Availability
All data generated or analyzed during this study are included in this manuscript.
References
LaFerla FM (2002) Calcium dyshomeostasis and intracellular signalling in Alzheimer’s disease. Nat Rev Neurosci 3(11):862–872. https://doi.org/10.1038/nrn960
Marambaud P, Dreses-Werringloer U, Vingtdeux V (2009) Calcium signaling in neurodegeneration. Mol Neurodegener 4:20. https://doi.org/10.1186/1750-1326-4-20
Mahaman YAR, Huang F, Kessete Afewerky H, Maibouge TMS, Ghose B, Wang X (2019) Involvement of calpain in the neuropathogenesis of Alzheimer’s disease. Med Res Rev 39(2):608–630. https://doi.org/10.1002/med.21534
Metwally E, Zhao G, Zhang YQ (2021) The calcium-dependent protease calpain in neuronal remodeling and neurodegeneration. Trends Neurosci 44(9):741–752. https://doi.org/10.1016/j.tins.2021.07.003
Cascella R, Cecchi C (2021) Calcium dyshomeostasis in Alzheimer's disease pathogenesis. Int J Mol Sci 22(9). https://doi.org/10.3390/ijms22094914
Goll DE, Thompson VF, Li H, Wei W, Cong J (2003) The calpain system. Physiol Rev 83(3):731–801. https://doi.org/10.1152/physrev.00029.2002
Patrick GN, Zukerberg L, Nikolic M, de la Monte S, Dikkes P, Tsai LH (1999) Conversion of p35 to p25 deregulates Cdk5 activity and promotes neurodegeneration. Nature 402(6762):615–622. https://doi.org/10.1038/45159
Cruz JC, Tseng HC, Goldman JA, Shih H, Tsai LH (2003) Aberrant Cdk5 activation by p25 triggers pathological events leading to neurodegeneration and neurofibrillary tangles. Neuron 40(3):471–483. https://doi.org/10.1016/s0896-6273(03)00627-5
Cheung ZH, Ip NY (2012) Cdk5: a multifaceted kinase in neurodegenerative diseases. Trends Cell Biol 22(3):169–175. https://doi.org/10.1016/j.tcb.2011.11.003
Noble W, Olm V, Takata K, Casey E, Mary O, Meyerson J, Gaynor K, LaFrancois J et al (2003) Cdk5 is a key factor in tau aggregation and tangle formation in vivo. Neuron 38(4):555–565. https://doi.org/10.1016/s0896-6273(03)00259-9
Seo J, Kritskiy O, Watson LA, Barker SJ, Dey D, Raja WK, Lin YT, Ko T et al (2017) Inhibition of p25/Cdk5 attenuates tauopathy in mouse and iPSC models of frontotemporal dementia. J Neurosci 37(41):9917–9924. https://doi.org/10.1523/jneurosci.0621-17.2017
Xu M, Huang Y, Song P, Huang Y, Huang W, Zhang HT, Hu Y (2019) AAV9-mediated Cdk5 inhibitory peptide reduces hyperphosphorylated tau and inflammation and ameliorates behavioral changes caused by overexpression of p25 in the brain. J Alzheimers Dis 70(2):573–585. https://doi.org/10.3233/jad-190099
Ghosh A, Greenberg ME (1995) Calcium signaling in neurons: molecular mechanisms and cellular consequences. Science 268(5208):239–247. https://doi.org/10.1126/science.7716515
Daverkausen-Fischer L, Pröls F (2022) Regulation of calcium homeostasis and flux between the endoplasmic reticulum and the cytosol. J Biol Chem 298(7):102061. https://doi.org/10.1016/j.jbc.2022.102061
Bagur R, Hajnóczky G (2017) Intracellular Ca(2+) sensing: its role in calcium homeostasis and signaling. Mol Cell 66(6):780–788. https://doi.org/10.1016/j.molcel.2017.05.028
Verkhratsky A (2005) Physiology and pathophysiology of the calcium store in the endoplasmic reticulum of neurons. Physiol Rev 85(1):201–279. https://doi.org/10.1152/physrev.00004.2004
Rajayer SR, Jacob A, Yang WL, Zhou M, Chaung W, Wang P (2013) Cold-inducible RNA-binding protein is an important mediator of alcohol-induced brain inflammation. PLoS One 8(11):e79430. https://doi.org/10.1371/journal.pone.0079430
Zhou M, Yang WL, Ji Y, Qiang X, Wang P (2014) Cold-inducible RNA-binding protein mediates neuroinflammation in cerebral ischemia. Biochim Biophys Acta 1840(7):2253–2261. https://doi.org/10.1016/j.bbagen.2014.02.027
Aziz M, Brenner M, Wang P (2019) Extracellular CIRP (eCIRP) and inflammation. J Leukoc Biol 106(1):133–146. https://doi.org/10.1002/jlb.3mir1118-443r
Sharma A, Brenner M, Wang P (2020) Potential role of extracellular CIRP in alcohol-induced Alzheimer’s disease. Mol Neurobiol 57(12):5000–5010. https://doi.org/10.1007/s12035-020-02075-1
Sharma A, Brenner M, Jacob A, Marambaud P, Wang P (2021) Extracellular CIRP activates the IL-6Rα/STAT3/Cdk5 pathway in neurons. Mol Neurobiol 58(8):3628–3640. https://doi.org/10.1007/s12035-021-02368-z
Jacob A, Ma Y, Nasiri E, Ochani M, Carrion J, Peng S, Brenner M, Huerta PT et al (2019) Extracellular cold inducible RNA-binding protein mediates binge alcohol-induced brain hypoactivity and impaired cognition in mice. Mol Med 25(1):24. https://doi.org/10.1186/s10020-019-0092-3
Jacob A, Wang P (2020) Alcohol intoxication and cognition: implications on mechanisms and therapeutic strategies. Front Neurosci 14:102. https://doi.org/10.3389/fnins.2020.00102
Orellana DI, Quintanilla RA, Gonzalez-Billault C, Maccioni RB (2005) Role of the JAKs/STATs pathway in the intracellular calcium changes induced by interleukin-6 in hippocampal neurons. Neurotox Res 8(3–4):295–304. https://doi.org/10.1007/bf03033983
Quintanilla RA, Orellana DI, González-Billault C, Maccioni RB (2004) Interleukin-6 induces Alzheimer-type phosphorylation of tau protein by deregulating the cdk5/p35 pathway. Exp Cell Res 295(1):245–257. https://doi.org/10.1016/j.yexcr.2004.01.002
Suzuki T, Imai J, Yamada T, Ishigaki Y, Kaneko K, Uno K, Hasegawa Y, Ishihara H et al (2011) Interleukin-6 enhances glucose-stimulated insulin secretion from pancreatic beta-cells: potential involvement of the PLC-IP3-dependent pathway. Diabetes 60(2):537–547. https://doi.org/10.2337/db10-0796
Qiang X, Yang WL, Wu R, Zhou M, Jacob A, Dong W, Kuncewitch M, Ji Y et al (2013) Cold-inducible RNA-binding protein (CIRP) triggers inflammatory responses in hemorrhagic shock and sepsis. Nat Med 19(11):1489–1495. https://doi.org/10.1038/nm.3368
Capiralla H, Vingtdeux V, Zhao H, Sankowski R, Al-Abed Y, Davies P, Marambaud P (2012) Resveratrol mitigates lipopolysaccharide- and Aβ-mediated microglial inflammation by inhibiting the TLR4/NF-κB/STAT signaling cascade. J Neurochem 120(3):461–472. https://doi.org/10.1111/j.1471-4159.2011.07594.x
Dreses-Werringloer U, Lambert JC, Vingtdeux V, Zhao H, Vais H, Siebert A, Jain A, Koppel J et al (2008) A polymorphism in CALHM1 influences Ca2+ homeostasis, Abeta levels, and Alzheimer’s disease risk. Cell 133(7):1149–1161. https://doi.org/10.1016/j.cell.2008.05.048
Lee MS, Kwon YT, Li M, Peng J, Friedlander RM, Tsai LH (2000) Neurotoxicity induces cleavage of p35 to p25 by calpain. Nature 405(6784):360–364. https://doi.org/10.1038/35012636
Rao MV, McBrayer MK, Campbell J, Kumar A, Hashim A, Sershen H, Stavrides PH, Ohno M et al (2014) Specific calpain inhibition by calpastatin prevents tauopathy and neurodegeneration and restores normal lifespan in tau P301L mice. J Neurosci 34(28):9222–9234. https://doi.org/10.1523/jneurosci.1132-14.2014
Sato K, Minegishi S, Takano J, Plattner F, Saito T, Asada A, Kawahara H, Iwata N et al (2011) Calpastatin, an endogenous calpain-inhibitor protein, regulates the cleavage of the Cdk5 activator p35 to p25. J Neurochem 117(3):504–515. https://doi.org/10.1111/j.1471-4159.2011.07222.x
Baudry M, Bi X (2016) Calpain-1 and calpain-2: the Yin and Yang of synaptic plasticity and neurodegeneration. Trends Neurosci 39(4):235–245. https://doi.org/10.1016/j.tins.2016.01.007
Sorimachi H, Hata S, Ono Y (2011) Calpain chronicle–an enzyme family under multidisciplinary characterization. Proc Jpn Acad Ser B Phys Biol Sci 87(6):287–327. https://doi.org/10.2183/pjab.87.287
Kang Y, Tiziani S, Park G, Kaul M, Paternostro G (2014) Cellular protection using Flt3 and PI3Kα inhibitors demonstrates multiple mechanisms of oxidative glutamate toxicity. Nat Commun 5:3672. https://doi.org/10.1038/ncomms4672
Chen S, Zou Q, Guo Q, Chen Y, Kuang X, Zhang Y, Liu Y, Wu W et al (2020) SPARC knockdown reduces glutamate-induced HT22 hippocampal nerve cell damage by regulating autophagy. Front Neurosci 14:581441. https://doi.org/10.3389/fnins.2020.581441
Zhou M, Aziz M, Denning NL, Yen HT, Ma G, Wang P (2020) Extracellular CIRP induces macrophage endotoxin tolerance through IL-6R-mediated STAT3 activation. JCI Insight 5(5). https://doi.org/10.1172/jci.insight.133715
Miller DJ, Adams SE, Hallett MB, Allemann RK (2013) Calpain-1 inhibitors for selective treatment of rheumatoid arthritis: what is the future? Future Med Chem 5(17):2057–2074. https://doi.org/10.4155/fmc.13.172
Fujita Y, Yago T, Asano T, Matsumoto H, Matsuoka N, Temmoku J, Sato S, Yashiro-Furuya M et al (2021) Clinical relevance for circulating cold-inducible RNA-binding protein (CIRP) in patients with adult-onset Still’s disease. PLoS One 16(8):e0255493. https://doi.org/10.1371/journal.pone.0255493
Wei W, Fareed MU, Evenson A, Menconi MJ, Yang H, Petkova V, Hasselgren PO (2005) Sepsis stimulates calpain activity in skeletal muscle by decreasing calpastatin activity but does not activate caspase-3. Am J Physiol Regul Integr Comp Physiol 288(3):R580-590. https://doi.org/10.1152/ajpregu.00341.2004
Kurbatskaya K, Phillips EC, Croft CL, Dentoni G, Hughes MM, Wade MA, Al-Sarraj S, Troakes C et al (2016) Upregulation of calpain activity precedes tau phosphorylation and loss of synaptic proteins in Alzheimer’s disease brain. Acta Neuropathol Commun 4:34. https://doi.org/10.1186/s40478-016-0299-2
Vosler PS, Gao Y, Brennan CS, Yanagiya A, Gan Y, Cao G, Zhang F, Morley SJ et al (2011) Ischemia-induced calpain activation causes eukaryotic (translation) initiation factor 4G1 (eIF4GI) degradation, protein synthesis inhibition, and neuronal death. Proc Natl Acad Sci USA 108(44):18102–18107. https://doi.org/10.1073/pnas.1112635108
de la Fuente S, Sansa A, Hidalgo I, Vivancos N, Romero-Guevara R, Garcera A, Soler RM (2020) Calpain system is altered in survival motor neuron-reduced cells from in vitro and in vivo spinal muscular atrophy models. Cell Death Dis 11(6):487. https://doi.org/10.1038/s41419-020-2688-5
Yu CG, Bondada V, Joshi A, Reneer DV, Telling GC, Saatman KE, Geddes JW (2020) Calpastatin overexpression protects against excitotoxic hippocampal injury and traumatic spinal cord injury. J Neurotrauma 37(21):2268–2276. https://doi.org/10.1089/neu.2020.7122
Guyton MK, Das A, Samantaray S, Wallace GCt, Butler JT, Ray SK, Banik NL (2010) Calpeptin attenuated inflammation, cell death, and axonal damage in animal model of multiple sclerosis. J Neurosci Res 88(11):2398–2408. https://doi.org/10.1002/jnr.22408
Hoffmann DB, Williams SK, Bojcevski J, Müller A, Stadelmann C, Naidoo V, Bahr BA, Diem R et al (2013) Calcium influx and calpain activation mediate preclinical retinal neurodegeneration in autoimmune optic neuritis. J Neuropathol Exp Neurol 72(8):745–757. https://doi.org/10.1097/NEN.0b013e31829c7370
Dufty BM, Warner LR, Hou ST, Jiang SX, Gomez-Isla T, Leenhouts KM, Oxford JT, Feany MB et al (2007) Calpain-cleavage of alpha-synuclein: connecting proteolytic processing to disease-linked aggregation. Am J Pathol 170(5):1725–1738. https://doi.org/10.2353/ajpath.2007.061232
Rao MV, Mohan PS, Peterhoff CM, Yang DS, Schmidt SD, Stavrides PH, Campbell J, Chen Y et al (2008) Marked calpastatin (CAST) depletion in Alzheimer’s disease accelerates cytoskeleton disruption and neurodegeneration: neuroprotection by CAST overexpression. J Neurosci 28(47):12241–12254. https://doi.org/10.1523/jneurosci.4119-08.2008
Rao MV, Campbell J, Palaniappan A, Kumar A, Nixon RA (2016) Calpastatin inhibits motor neuron death and increases survival of hSOD1(G93A) mice. J Neurochem 137(2):253–265. https://doi.org/10.1111/jnc.13536
Su W, Zhou Q, Wang Y, Chishti A, Li QQ, Dayal S, Shiehzadegan S, Cheng A et al (2020) Deletion of the Capn1 gene results in alterations in signaling pathways related to Alzheimer’s disease, protein quality control and synaptic plasticity in mouse brain. Front Genet 11:334. https://doi.org/10.3389/fgene.2020.00334
Wang CY, Xie JW, Wang T, Xu Y, Cai JH, Wang X, Zhao BL, An L et al (2013) Hypoxia-triggered m-calpain activation evokes endoplasmic reticulum stress and neuropathogenesis in a transgenic mouse model of Alzheimer’s disease. CNS Neurosci Ther 19(10):820–833. https://doi.org/10.1111/cns.12151
Kritis AA, Stamoula EG, Paniskaki KA, Vavilis TD (2015) Researching glutamate - induced cytotoxicity in different cell lines: a comparative/collective analysis/study. Front Cell Neurosci 9:91. https://doi.org/10.3389/fncel.2015.00091
Yang YR, Kang DS, Lee C, Seok H, Follo MY, Cocco L, Suh PG (2016) Primary phospholipase C and brain disorders. Adv Biol Regul 61:80–85. https://doi.org/10.1016/j.jbior.2015.11.003
Acknowledgements
The authors thank all the members of the Center for Immunology and Inflammation for their support on this study.
Funding
This work was supported by the National Institutes of Health grants R01 AA028947 (PW, PM) and R35 GM118337 (PW).
Author information
Authors and Affiliations
Contributions
AS conceived and designed the experiments and wrote the manuscript; ES and AS conducted all the experiments, acquired, and analyzed the data; SP performed some immunoblots and calpain activity assays, YC performed confocal and some immunofluorescent imaging; PM provided reagents and critical input in some experimental designs; PW, MB and PM critically reviewed the manuscript, and PW supervised the research. All authors read and approved the final manuscript.
Corresponding author
Ethics declarations
Ethics Approval
Not Applicable
Consent to Participate
Not Applicable
Consent to Publish
Not Applicable
Competing Interests
All the authors declare that they have no competing interests.
Additional information
Publisher's Note
Springer Nature remains neutral with regard to jurisdictional claims in published maps and institutional affiliations.
Supplementary Information
Below is the link to the electronic supplementary

12035_2023_3273_Fig11_ESM.png
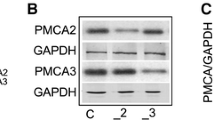
Supplementary Fig. 1. eCIRP Transiently Increases Neuronal Calpain 1 not Calpain 2. a N2a cells were treated with vehicle or 2.5 µg/ml eCIRP for 16 h. RNA was isolated from N2a cells and subjected to qPCR. Relative CT values for calpain 1 (Cal 1) (n = 7/group) and calpain 2 (Cal 2) (n = 9/group) mRNA in vehicle treated control N2a cells. Data are means ± SEM compared by Student’s t-test. * p < 0.05 vs. Cal 1. b N2a cells were treated with vehicle or eCIRP at indicated doses for 48 h. Total cell lysates were prepared and subjected to WB. Representative WB images for calpain 1 and actin and bar graphs (n = 4–6/group) from the densitometric analysis of blots are shown. The dotted lines on the WB image reflect different samples from the corresponding groups shown in the bar graph below. Data are means ± SEM compared by ANOVA/Tukey analysis and no significant differences were found. c N2a cells were treated with vehicle or eCIRP at indicated doses for 16 h. Total cell lysates were prepared and subjected to WB. Representative WB images for calpain 2 and actin and bar graphs (n = 6/group) from the densitometric analysis of blots are shown. The dotted lines on the WB image reflect different samples from the corresponding groups shown in the bar graph below. Data are means ± SEM compared by ANOVA/Tukey analysis and differences were not significant (ns) (PNG 179 kb)

12035_2023_3273_Fig12_ESM.png
Supplementary Fig. 2. eCIRP Induces Intracellular Ca2+ in HT22 Cells in a Dose-Dependent Manner. HT22 cells (n = 12/group) were stimulated with indicated doses of eCIRP or no eCIRP as control in a clear 96 well-black plate. After 3 h the medium is removed, the cells were loaded with Fluo-4 AM dye. a Fluorescence measurement for intracellular Ca2+ levels performed at 485/535 nm. Fluo-4 fluorescence units for control cells was set as 100%. Data are means ± SEM and compared by ANOVA/Tukey analysis. * p < 0.05 vs. no eCIRP and # p < 0.05 vs. eCIRP. b Representative confocal images of the Fluo-4 dye loaded HT22 cells under untreated control, and eCIRP treatment are shown. Scale bar, 100 µm. c Bar graphs from the fluorescence intensity analysis of the images with relative fluorescence units for all HT22 cells in the field are shown. Data are means ± SEM and compared by ANOVA/SNK analysis. * p < 0.05 vs. no eCIRP and # p < 0.05 vs. 0.1 µg/ml eCIRP (PNG 389 kb)

12035_2023_3273_Fig13_ESM.png
Supplementary Fig. 3. eCIRP Does not Affect Extracellular Ca2+ Influx. HT22 cells were treated with vehicle or 2.5 μg/ml eCIRP for 3 h. After 3 h the medium is removed, the cells were washed and loaded with Fluo-4 AM dye followed with Ca2+ depletion (0 mM CaCl2) and Ca2+ added back (1.4 mM CaCl2). Fluorescence measurements for intracellular Ca2+ levels were performed at 485/535 nm and data shown as a kinetic graph of relative fluorescence units (RFU) (n = 4/group) expressed as means ± SEM over time for control cells (open black circles with black lines for SEM) and eCIRP treated cells (filled red circles with red lines for SEM). No significant differences were found when compared by ANOVA/Tukey analysis (PNG 178 kb)
Rights and permissions
Springer Nature or its licensor (e.g. a society or other partner) holds exclusive rights to this article under a publishing agreement with the author(s) or other rightsholder(s); author self-archiving of the accepted manuscript version of this article is solely governed by the terms of such publishing agreement and applicable law.
About this article
Cite this article
Sharma, A., Sari, E., Lee, Y. et al. Extracellular CIRP Induces Calpain Activation in Neurons via PLC-IP3-Dependent Calcium Pathway. Mol Neurobiol 60, 3311–3328 (2023). https://doi.org/10.1007/s12035-023-03273-3
Received:
Accepted:
Published:
Issue Date:
DOI: https://doi.org/10.1007/s12035-023-03273-3