Abstract
Malaria is one of the severe infectious diseases that has victimized about half a civilization billion people each year worldwide. The application of long-lasting insecticides is the main strategy to control malaria; however, a surge in antimalarial drug development is also taking a leading role to break off the infections. Although, recurring drug resistance can compromise the efficiency of both conventional and novel antimalarial medicines. The eradication of malaria is significantly contingent on discovering novel potent agents that are low cost and easy to administer. In this context, plant metabolites inhibit malaria infection progression and might potentially be utilized as an alternative treatment for malaria, such as artemisinin. Advances in genetic engineering technology, especially the advent of molecular farming, have made plants more versatile in producing protein drugs (PDs) to treat infectious diseases, including malaria. These recent developments in genetic modifications have enabled the production of native pharmaceutically active compounds and the accumulation of diverse heterologous proteins such as human antibodies, booster vaccines, and many PDs to treat infectious diseases and genetic disorders. This review will discuss the pivotal role of a plant-based production system that expresses natural antimalarial agents or host protein drugs to cure malaria infections. The potential of these natural and induced compounds will support modern healthcare systems in treating malaria infections, especially in developing countries to mitigate human fatalities.
Similar content being viewed by others
Avoid common mistakes on your manuscript.
Introduction
Malaria is among the deadliest infectious diseases caused by Plasmodium parasites. Malarial infections are transmitted within the population through infected female Anopheles mosquitoes. Five parasite species including P. knowlesi, P. ovale, P. malariae, P. vivax, and P. falciparum are known sources of malaria in humans, and the two last species pose the greatest threat [1] as P. vivax causes the most morbidity and P. falciparum causes most mortality, mainly in children under five [2]. Malaria has affected around half of the modern civilization and is endemic in more than hundred countries [3]. The malaria-related mortalities are disproportionately high in developing countries compared to technologically advanced countries due to several reasons. Unfortunately, the socioeconomic status of the population in developing countries has limited their access to antimalaria therapies. According to the world malaria report released in December 2019, approximately 228 million malaria cases have occurred worldwide, of which 435,000 malaria-related deaths have occurred in African regions where 85% of global malaria cases and 94% of deaths were reported [4]. Considering this, current predictions suggest that nearly half of the world’s inhabitants are at high risk of malaria infections. In addition to increasing deaths, malaria infections can account for massive economic losses, with an estimated US$2.7 billion in healthcare-related expenditures in 2018 [4], subsequently contributing to economic deterioration in resource-poor countries.
The current pandemic of SARS-CoV-2, known as COVID-19, can potentially trigger malaria crises in the region because of the vulnerability of health and economic systems, along with the high burden of malaria [5]. Moreover, the potential impact of the spread of COVID-19 on Plasmodium falciparum malaria morbidity and mortality has been reported [6], and World Health Organization (WHO) has strongly highlighted the importance of continuing malaria diagnostic, prevention, and case management activities [7]. Keeping in view the urgency of novel therapeutics, plants can offer natural and recombinant medication to combat widespread malaria infections. Since malaria is commonly associated with poverty, inexpensive large-scale production of antimalaria drugs under the current infrastructure in the remote area is an urgent need for its eradication. This goal can be achieved efficiently in a cost-effective manner by bulk production of antimalaria drugs using a plant expression system by avoiding the obligatory cold chain conditions for its storage and distribution. Hence, this review also elaborates on the capacity of herbal medicine and plant molecular farming to treat malaria infections keeping the developing world in focus.
Malaria Life Cycle
The life cycle of the malarial parasite included multiple stages that involve two hosts, i.e., the human and the mosquito. The life cycle initiates with a single bite of infected female Anopheles mosquitoes and inoculation of uninucleated sporozoites into the bloodstream. Sporozoites subsequently migrate from blood to liver tissue in less than a minute and soon after five days, sporozoites develop into uninucleated merozoites with a range of 10,000–40,000 that further can invade a normal erythrocyte [8]. After maturation in the liver, merozoites can be released, and the cycle of intraerythrocytic-stage development, rupture, and reinvasion can be continued and/or can also be developed into sexual-stage parasites, gametocytes. In the mosquito’s gut, gametocytes separate from erythrocytes and produce gametes to complete the life cycle by fusing to form a zygote (ookinetes) which subsequently transform into an oocyst in which new sporozoites are formed. Finally, the newly produced sporozoites migrate to the salivary glands and eventually become infectious to humans when the mosquito feeds [9].
Currently Available Antimalarial Drugs
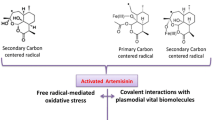
Malaria control and eradication are complicated where different factors affect the treatment process, such as drug resistance, socioeconomic status, cost of production, and drugs quality. Antimalarial therapy is currently based on four major drug classes, including quinolone derivatives, antifolates, artemisinin derivatives, and antimicrobial [10]. The most available drugs target the asexual phase (erythrocytic stage) of the malaria parasite generating symptomatic illness [11]. Despite intensive efforts in malaria research, currently, there is no report on identifying a single drug, which can wipe out all strains of malaria and appear in the global market. Moreover, single drugs utilization is limited to a certain period until the emergence of drug resistance. For example, malaria resistance to artemisinin derivatives was identified in Myanmar, Thailand, Cambodia, and Vietnam [12]. Hence, a combination of drugs has been suggested as an alternative to combat malaria infections. Changing the combination of drugs may decrease the risk of resistance development as well as treatment failure. In this context, depending on the severity of the disease, the geographic location of the infection and the species of parasites, antimalarial dosing therapies are prescribed accordingly [11].
In the case of artemisinin-resistant malaria, WHO recommends artemisinin-based combination therapy (ACT) as a reliable and genuine therapeutic antimalarial drug. However, the drug resistance was reported to multiple ACTs in Cambodia Pailin province; therefore, a combination without artemisinin (atovaquone plus proguanil) was suggested by WHO in 2013 [13]. In addition, arterolane is an antimalarial compound reported in the early 2000s marketed in India and African countries in fixed dose combination with piperaquine. However, the dose combination was not approved to date by WHO for general use [12]. In addition, comprehensive reviews of drug resistance and efficiency have been documented [14,15,16]. The general guidelines for the control and treatment of malaria by WHO were also provided [17]. The wealth of data is available where antimalarial drugs and potential drug candidates are reviewed [10, 18,19,20,21].
Herbal Medicine Against Malaria
Medicinal plants may play a critical role in synthesizing novel and potent antimalarial agents. Pharmacological studies have been performed on plant extracts, and purified metabolites for antimalarial activity have indicated the efficacy of most plants in the treatment of malaria. More importantly, there is no evidence of resistance because of the plant’s synergistic action of several constituents representing the great potential of plant extract against malaria resistance. Herbal medicine may also contribute to reduce the risks of disease without removing the continued exposure to infection necessary to retain immunity, which is critical in the management and eradication of malaria particularly in Africa [22]. Antimalaria compounds, including natural products and plant extracts have been reported in several review articles which are summarized in the following paragraphs.
The review by [23] evaluated the antimalarial activity of 124 medicinal plant species that belong to 55 families and 99 genera during 1991–2016 in Ethiopia. This review also assessed the antiplasmodial activity of 25 plant extracts with their structures and 28 medicinal plant species from 24 families commonly used for malarial treatment. Allium sativum L., Croton macrostachyus Del., Carica papaya L., Lepidium sativum L., and Vernonia amygdalina Del. were reported plant species based on ethnomedicinal survey performed in this review and A. sativum L., and C., papaya L., are reported based on traditional healers for treatment of malaria. Plant leaves are reported as most frequently used plant part, while alkaloids and terpenoids are reported as chemical classes most frequently identified for their antiplasmodial activity.
In another study, a total of 356 active chemical constituents from antimalarial plants are summarized by [24]. This review examined 26 active components with their chemical structures. The compounds listed in this review belong to the class of alkaloids, flavonoids, terpenoids, saponins, tannins, essential oils, sesquiterpene lactones, xanthanoids, polyphenol, iridoid glycosides, coumarins, anthraquinones, limonoids, tetranortriterpenoids, triketones, cembranolides, tetrahydropyrone derivatives, triterpene hydrocarbon derivatives, cucurbitacin glycosides, poliothrysoside, benzophenones, chalcones, and phloroglucinols.
A large number of 2,000 plant extracts from 50 families against P. falciparum were studied and dozens of plants with antimalarial activity were discovered which cover a total of 175 antiplasmodial compounds extracted from plants from 2001 to the end of 2017. Twenty-five out of these 175 antiplasmodial compounds belong to marine plants. All these compounds are organized according to their plant family of origin. After screening of 175 antiplasmodial compounds, only 8 compounds, including trichothecene roridin E from Rhaphidophora decursiva (Araceae), Verrucarin L., acetate from Ficus fistulosa (Moraceae family), phenanthroindolizine alkaloids dehydroantofine and tylophoridicine D from Ficus septica (Moraceae), fortunilide A., and fortunilide E., sarglabolide J., from Chloranthus fortunei, and chlorajaponilide C., from Chloranthus multisachs (Chloranthaceae) showed a range of nanomolar activity, considered for further analysis for their antimalarial activity. The structure of all compounds has also been elucidated.
Numerous studies on antimalarial and antiplasmodial activities from January 2009 to November 2010 were performed and a total of 30 antiplasmodial natural products including terpenes, flavonoids, alkaloids, peptides, polyketides, macrolides, and miscellaneous compounds along with their structures were summarized by [25]. The review highlights a wide range of novel natural products on which to base the identification and establishment of antimalarial drugs. The most potent antiplasmodial natural products have been categorized in detail. Majority of the reviewed compounds were based on in vitro assays; however, fewer were analyzed for cytotoxicity. Also, the less active compounds have been evaluated based on in vivo analysis.
Memvanga and his colleagues evaluated [26] the antimalarial compound in 100 species from Congolese antimalarial plants during the period of 1999–2001, based on in vitro and in vivo analyses. The antimalarial plant data of bio-guided fractionation, isolation, and structure elucidation have been summarized in this review. In vitro antiplasmodial activity and cytotoxicity of plant-derived components have been reported. The review highlights clinical studies to evaluate safety and the efficacy of quantified extract and commercialized plant-derived products extract. A phase I, IIA, and IIB clinical trial of crude extract from Nauclea pobeguinii indicated promising results in terms of safety and efficacy as well as fewer side effects. However, these clinical studies did not cover nonimmune patients (e.g., children) which are noticeably more suffered by the malaria disease. This review also presents performed clinical trials of A., annua extract on the treatment of malaria in Congo and demonstrates the efficacy of A., annua extract to remove malaria symptoms. To potentiate long-term protection of A. annua and decrease high rate of recrudescence, combination with Curcuma longa extracts was proposed. This review presents two commercialized antimalarial products Manalaria® (Gotu Kola) and Nsansiphos® (Cephalanthus occidentalis and N., latifolia) that received regulatory approval in Congo.
From 1994 to 2013, 278 plant compounds including alkaloids, flavonoids, terpenoids, phenolics, coumarines, polyacetylenes, xanthones, quinones, steroids, and lignans extracted from African flora have been reviewed [27, 28]. The activities of 171 compounds belonging to the alkaloid and terpenoid classes have been reviewed in the first and second sections, respectively. In vitro and in vivo assays of some derived phytochemicals also have been discussed. The cheminformatic analysis of > 500 natural products extracted from African medicinal plants is reviewed in the last section, with weak to robust in vitro antimalarial activities.
In another study, 99 species in 81 genera and 45 families from Kenya were summarized and investigated for in vitro antiplasmodial activity [29]. The review concludes that about 24.2% species presented antiplasmodial efficacy of IC50 ≤ 5 µg/ml and MeOH root bark extract of Maytenus obtusifolia ((IC50 < 1.9 µg/ml) was considered to have potential for isolation of antimalarial compounds.
A comprehensive literature search retrieved 286 antimalarial plant species distributed among 75 families and 192 genera in Kenya [30]. The most frequently used plant families were Asteraceae, Fabaceae, Lamiaceae, Euphorbiaceae, Rutaceae, and Rubiaceae. Toddalia asiatica (L.) Lam, Aloe secundiflora Engl., Azadirachta indica A. Juss, Carissa edulis (Forsk.) Vahl., and Harrisonia abyssinica Olive. Additionally, side effect of 13 medicinal plant species with antimalaria activity were reviewed, including vomiting, diarrhea, and bile release. Of 286 antimalarial plant species, 139 have been evaluated for antiplasmodial (n = 25, 18%) or antimalarial activities (n = 135, 97.1%; IC50 ug/ml), bioactive compound, and toxicity.
Combined survey of traditional healers and literature search about herbal medicines traditionally used for malaria treatment in Democratic Republic of Congo (DRC) region were reviewed in [31]. Direct interview of 32 traditional healers characterized 45 plant species among 21 botanical families and 41 genera. Artemisia annua L., (Asteraceae) and Carica papaya L., (Caricaceae) were the most frequently claimed. The diverse remedy preparation methods include decoction, infusion, maceration, sap extraction, juice extraction, powder, ash, and ovule. Combinatory use of these remedies generated 25 multi-herbal and 27 mono-herbal recipes by traditional healers. The study also retrieved 194 plant species belonging to 69 families and 164 genera that were previously documented for malaria treatment in DRC region and compared them with those identified by traditional healers. Only 38% of surveyed medicinal plant species were cited previously by other studies.
The review by [32] was obtained from African Compound Libraries from 2013 to 2019, which is constantly updated. The bulk of 187 natural compounds from plants which demonstrated variety of antimalarial/antiplasmodial activity mainly consisted of terpenoids, flavonoids, alkaloids, and quinones with percentage more than 5% in the entire compound collection. Also, most antimalarial/antiplasmodial compounds were derived from plant species family Rubiaceae. The most active compounds belonged to the same classes from which the natural origins of current antimalaria drugs are derived, such as quinine from alkaloid and artemisinin from terpenoid.
Novel Antimalarial Natural Products Discovery
The discovery and isolation of novel therapeutic candidates in numerous medicinal plant resources are foundation of developing antimalarial drugs or phytomedicines. In this case, basic methodologies have been applied in the selection of medicinal plants for further analysis in drug discovery and development. They included mass screening of plants, ethnomedicinal uses, available databases, and chemotaxonomic approaches [33, 34]. The selection of the ideal leads with the high efficacy and safety properties as antimalarial drug is the most complicated part in development of new antimalarial drug from medicinal plants. Safety of natural products in terms of contradictions, side effects, toxicity, and treatment time are critical issues, which should be carefully considered [35]. The medicinal plant’s safety is of paramount importance for registration/authorization purposes. The potential candidate should pass at least in vitro and in vivo genotoxicity analyses, carcinogenicity, reproductive and developmental toxicity assays, and studies of the effects on drug-metabolizing enzymes [36].
To determine plants potential with high antiplasmodial activity, pharmacological investigations emphasized crude extracts and fractions. Based on published guidelines from WHO and basic criteria for antiplasmodial drug discovery [37, 38], plant extracts can be categorized into three levels based on their antiplasmodial activity as follows: high or pronounced activity (IC50 ≤ 5 μg/ml), good or promising activity (5 μg/ml < IC50 ≤ 15 μg/ml), moderate activity (15 μg/ml < IC50 ≤ 50 μg/ml), and weak activity (50 mg/ml < IC50 < 100 μg/ml). A pure substance is determined as highly active when its IC50 ≤ 1 μg/ml. Also, extracts that exhibit 50% of P. falciparum schizonts maturation at concentrations < 5 mg/ml were considered significant antimalarial leads [26]. Next, the cytotoxicity of plant-derived compounds on human cells should also be considered for the antiplasmodial activity. To evaluate the plant extract or isolated compounds for their efficacy against the P. falciparum parasite compared to its cytotoxicity for mammalian cells, their selectivity index (SI) has been defined. The cytotoxic CC50 value ratio on a cell line to the antiparasitic IC50 value on a P. falciparum strain is calculated as SI. According to Camacho analysis [39] the extracts or fractions are selective against the Plasmodium parasite if IS value is greater than 1.0. In contrast, extracts or fractions with SI lower than 1.0 are selective against the cell line used. Therefore, plant-derived antimalarial compounds with SI greater than 1.0 can be considered for further investigations. However, SI values for lead compounds must be greater than 10–100 [37, 38].
In the classic discovery for natural products, the compounds are commonly investigated in vivo only after in vitro characterization. Nevertheless, screening of drug (compound isolation, structure elucidation, structure–activity relationship, lead optimization, clinical trials, and authorization for product launch) by this method is prolonged, inefficient, and expensive. The journey of product development is time consuming (10–15 years) from the concept to clinical trials and also requires a whopping investment of US $ 1 to 1.5 billion [40]. Additionally, product development cost ends up with a high price that often results in its unavailability and unaffordability in developing countries. Furthermore, the pharmaceutical industries are searching beyond classical drug discovery and development concepts that accelerate the process and guarantee that efficient and safe drugs could be released faster and sustained reverse pharmacology, also known as bedside to bench, is a multidisciplinary procedure emphasing on conventional knowledge, experimental observation, and clinical experience [43]. Reverse pharmacology is associated with reversing the routing ‘laboratory to clinical discovery’ to ‘clinical to laboratory practice’ [41]. This approach can add balance to current approaches, such as when first-line treatment is not available and can be employed to decline the progress of resistance to existing standard drugs. Reverse pharmacology has been successfully used to develop antimalarial phytomedicine derived from Argemone mexicana decoction [42]. Argemone mexicana has been investigated for reverse pharmacology process in Mali and categorized into 4 stages, including selection of the remedy, dose-escalating clinical trials, randomized control, and isolation of tested compounds [42]. This example of reverse pharmacology demonstrates that a standardized phytomedicine development is faster and cost effective in comparison to conventional drugs and that can be an efficient alternative approach for the development of a validated phytomedicine [43]. Several antimalaria phytomedicines have been successfully developed and have received government authorization in Ghana (Cryptolepis sanguinolenta root infusion), in Burkina Faso (Cochlospermum planchonii root decoction) [22], and the Democratic Republic of Congo (A. annua Anamed leaf infusion) [44]. The examples are reported as safe and effective in pre-clinical trials; however, further investigations are required to investigate their effectiveness in public health strategies to manage and eradicate malaria. Moreover, inexpensive and reliable tests are needed to perform quality control and optimization of plant materials. Besides efficacy, the drug dosage is equally important for standardizing medicinal plant formulations. In the context of standardization, there are several key factors to consider, such as drug quality, physical, chemical, phytochemical, and standardization, as well as in vitro and in vivo parameters which are equally important. Optimization is complex because plant’s genetic and environmental factors are critical contributors for variability in herbal preparation. Also, the raw material is supplied in batches that can vary in active compounds. Therefore uniform optimization regarding quality among different batches are hard to control and ascertain [45]. Furthermore, the absence of regulatory standards regarding herbal medicine preparation and clinical evaluation makes product development complicated and difficult.
Whole Plant or Its Isolated Natural Products Against Malaria
A major complexity in discovering single-active constituent as new drug from plants stems is the efficacy of most plant natural products associated synergistically with diverse components rather than a single compound [46, 47]. This complexity hinders the development for discovery of novel natural product for antimalarial agents. Natural medicines’ synergistic actions come from evolutionary responses toward invaders [48]. As a self-defense mechanism, plants synthesized and secreted antimicrobials to fight against pathogens and, in the response, pathogens developed their resistant systems for survival. In the next step, plants were induced to develop resistant inhibitors [49]. A crude extract can then contain both resistant inhibitors and their potentiators [50]. Synergistic interactions are the body of the pharmacodynamic augmentation, where different constituents in the crude extract provide a combined effect. In this context, the in -vitro antiplasmodial activity of 14 medicinal plants indicated that berberine was the single most active antimalarial compound [51]. However, extracted flavonoids from the same plant have been demonstrated to remove resistance toward berberine in microbes. Thus, while berberine may be the most important antimicrobial, eliminating flavonoids could lead to the development of microbial resistance to berberine and may account for its failure as an antimicrobial [52].
The principal synergistic combination of antimalarials were addressed with Malarone® (atovaquone–proguanil) [53] and Quinimax® (quinine–quinidine–cinchonine) [54, 55]. The product Malarone® as an antimalarial is demonstrated for prophylaxis of P. falciparum, including in areas where chloroquine resistance has been reported. Synergistic combination has been documented not only for reversal resistance but also for other positive interaction, including complementary mechanisms of action (improving bioavailability or decreasing metabolism and excretion and immunomodulation) and modulation of side effects. The synergistic combination can occur among different plants or phytochemical and a synthetic drug. Table 1 summarizes example of synergistic combination of natural plant products in treatment of malaria.
The positive effects of synergistic combination indicated that crude plant extracts or a mixture of plants that could generally have greater in vitro/in vivo antiplasmodial activity than a single compound at an equivalent dose [56]. Moreover, it has also been demonstrated that the combination strategy can decrease the toxicity of single-active compounds to the microorganism. In this case, Quinimax is an example of standardized mixture of cinchona alkaloids that exhibits less cinchonism and prolongation of the QTc interval than quinine and quinidine alone, respectively [54, 55]. Additionally, combination of plants mixtures has been successfully reported to treat numerous diseases and dysfunctions related to malaria infection, such as coated tongue and replacing blood cells during malaria infection [57] (Table 2).
Compared to whole-plant extracts, Wells and colleagues [58] demonstrated the active ingredient’s identification and its utilization in medicinal chemistry. The findings paved the foundation for the development of more potent and long-lasting medicines in malaria chemotherapy. They exemplified the adverse effects of self-administering cinchona bark extract to support this idea, which led to malaria-like symptoms of palpitations, drowsiness, vomiting, and feeling cold. However, in many cases, the whole-plant extracts were not toxic and showed safety at therapeutic doses, as demonstrated for A. annua and Argemone Mexicana [56]. Additionally, although pure drugs isolated from plants can be considered potent candidates due to their higher activity against malaria, however, the expensive separation methods and distribution process of pure compounds are costly enough to make it unaffordable to resource-limited settings. In contrast, intact plants can often be grown and harvested locally, at a much cheaper cost to those who need them [59]. However, further clinical research is required on pharmacodynamic synergy and safety of combination of plant-derived compounds and/or medicinal plant extracts to boost the activity of existing pharmaceutical preparations and the efficacy of herbal remedies for use in poor region where modern drugs are inaccessible and unaffordable.
Production of Malaria Therapeutics in Plants
Lower concentration of active molecules in source plants is one of the major concerns related to natural producers. The location and environmental condition which account for slower growth may negatively affect the production and recovery of natural products. Subsequently, larger quantities of biomass are required to fulfill the demands of commercial production of active molecules [60, 61]. Considering that active drugs should be produced inexpensively in much more significant quantities than currently available ones, genetic engineering plays a pivotal role to expand available metabolic repertoire or to express the entire biosynthesis pathways into host plants for its production with proper functionality [62, 63]. Artemisinin is an antimalarial compound and is naturally produced in A. annua in low level [64, 65], which led to relatively high costs for isolation and purification. Although, in the last decade the amount of artemisins has been increased by 36-fold [66], an efficient prophylactic approach could be in great demand in the endemic countries. The worldwide demand each year for artemisinis is around 119 metric tons (MT), while the amount of A. annua in its aerial parts is 0.01–1.2% which is not enough to meet growing demands [67]. Moreover, chemical synthesis of artemisinin makes the price unaffordable to most patients in remote areas.
Different approaches by metabolic engineering have been applied to enhance artemisinin production by overexpressing of genes involved in the biosynthetic pathway of artemisinin. [68]. Artemisinin synthesis can be considerably improved by overexpressing HMGR and ADS in A. annua [69] and also, artemisinin production has been increased by expressing HMGR and FPS together in A. annua [70]. Overexpression of FPS in A. annua leads to the accumulation of the increased amount of artemisinin through conversion of IPP and DMADP into FDP. Recent attempts have been made to induce the expression of a novel biosynthetic pathway of artemisinin in transgenic tobacco plants [71,72,73,74,75]. The best strategy to obtain high content of artemisinin in transgenic plant was established via the expression of artemisinin pathway genes in chloroplast [73]. The transgenic plants showed a threefold enhancement of isopentenyl pyrophosphate, and targeting AACPR, DBR2, and CYP71AV1 to chloroplasts resulted in higher expression and an efficient photo-oxidation of dihydroartemisinic acid to artemisinin. This strategy successfully enhanced artemisinin production with capacity of 0.8 mg/g (DW) tobacco leaves [73], which is the highest level of artemisinin produced in transgenic plant reported to date.
Besides tobacco plants, mosses Physcomitrella patens has been utilized as a production host for artemisinin. Recently, integrating the biosynthetic pathway of artemisinin by incorporating five-related genes into the moss genome was successfully performed. These genes were ADS, amorphadiene synthase; CYP71AV1, amorphadiene oxidase; ADH1, alcohol dehydrogenase-1; DBR2, artemisinic aldehyde double-bond reductase; ALDH1, aldehyde dehydrogenase-1 that resulted in a high initial production of 0.21 mg/g dry weight artemisinin after 3 days of cultivation [76].
Plant cell cultures are utilized as alternative production system for antimalarial-active molecules [77,78,79,80] at a scale of ~ 1000 L or higher [81]. Although, the production cost is relatively higher because of the requirement for fermentation equipment, growth media as well as sterile handling during upstream process, but cell cultures are preferred as suspension obtained from native or relative species. This is advantageous because intrinsic metabolic capability can be boosted by genetic engineering, hairy root cultures, precursor feeding, elicitation, permeabilization, and growth regulators to increase yields [82,83,84,85,86]. Such strategy was implemented by different research groups to enhance the yield of artemisinin [77, 87,88,89] (Fig. 1).
The evolutionary architecture of pharmacopeia during the time. Based on ancient’s records, the evolution of human clinical trials used plants to find out how they can help us treat. The historic evidence of humans using oral delivery of plants as therapeutics by the preparation of crude extracts or extraction of active compounds can be considered a great advantage, principally by providing a safe and inexpensive system to treat disease. The field of natural products moved to the chemical synthesis of natural product analogs via modifications of its functional groups aimed to elucidate the mode of action. Finally, plant biotechnology and plant molecular farming have emerged as relevant and sustainable systems to synthesize molecules (chemically) and other microbial and mammalian cell bioreactors
Plant-based antimalarial products’ success is significantly contingent to bulk production system, which provide large production of high‐quality drugs for formulation and characterization. In this context, molecular biopharming is a useful tool to overexpress potential contents of plant-derived antimalarial drugs and facilitate the large-scale production of drugs (Fig. 2). Considering the plant expression system, tobacco and N. benthamiana are currently utilized as standard systems for stable and transient foreign proteins production, respectively [90]. Transgenic tobacco plant is an efficient and sustainable platform for producing heterologous proteins because crop can be grown in sterile conditions without antibiotics and large leaves biomass account for large production and can be harvested several times a year. Moreover, each tobacco plant can produce nearly a million seeds per season [91] and high biomass yield of 91,000 tons a−1 km−2 in the case of using vertical farming units (VFUs), allowing production of pharmaceuticals in multiple tons with low cost enough to fulfill high-demand markets [92]. N. benthamiana also is ideal system foreign proteins because of its hefty biomass production ranged from 3500 to 7000 kg per week as reported by the Caliber Biotherapeutics facility 89. Moreover, ease of transformation with well-optimized protocol available, subsequent selection and development of target recombinant protein, ability to process glycosylated proteins, and cost-effective upscale production of 150 kg/year of purified product are substantial technical advantages of plant platforms over mammalian cells or cellular-based systems [93].
Development of plant-made malarial drugs: A. DNA sequences correspond to the gene of protein drugs against malaria. B. Construction of plasmid that includes the gene of interest, regulatory sequences, promoter sequences, and marker genes for transformation into the plant. C. The transformation of the plasmid into agrobacterium for infecting plants for transient expression of protein drug. D. Transient plant producing antimalarial drug in weeks after agroinfiltration. E. The confirmation of transgene integration and recombinant protein production with PCR, Western blots, and its quantitation with ELISA. F. The chromatographic purification of recombinant antimalarial drug with appropriate purification tag. G. The final antimalarial drug after characterization and quality control for commercialization
Plant-Derived Vaccine Against Malaria
The vaccine development approach stems from the fact that recurring drug resistance can compromise the efficiency of both old (use of insecticide-treated bed nets and indoor residual spraying) and new antimalarial medicines [17]. Albeit intensive research on vaccine development against malaria, there is still no vaccine available that can provide sustained immunity. The vaccine could be considered a promising alternative tool for controlling and preventing malaria, proven as an efficient and cost-effective tool for control and management of other infectious diseases. To develop an effective malaria vaccine, attempts have been made to understand the parasite life cycle classified into liver, blood, and mosquito stages. All these stages have a great potential for the development of malaria vaccine in order to elicit immune response [94]. Several aspects have been investigated to produce potential malaria vaccine candidate antigens, domains, and epitopes, and several have been advanced into pre-clinical and advanced clinical trials [95]. Plasmodium falciparum circumsporozoite protein (CSP)-based Mosquirix (RTS, S) developed by GSK is the most advanced malaria vaccine that could enter the market [96]. Like all other drugs development, the process of plant-made product development may take several years to secure regulatory approval (Fig. 3), and currently the regulations in Europe and the USA are tight to move forward any plant-made products. However, recently Covid-19 pandemic has made the regulators look for alternative method of production such as plant for scalable and cost-effective methods to mitigate the infections.
Schematic representation of the R & D process: The process of drug research and development takes 12–15 years on average for an experimental drug to journey from laboratory research, safety, and efficacy evaluation using animal models and conducting clinical trials on diverse populations to FDA approval
Although there is no report on the production of efficient vaccine which provides immunity against malaria, several candidate antigens against different stages of the parasite life cycle have been expressed using transient expression or stably transformed plants [97]. Upon oral delivery for immunization, production of neutralizing antibodies is reported in plant-made vaccine candidates. Those also enhanced immunogenicity with long-lasting TBA resulted in protective immune response in animal model [96, 97]. Subcellular targeting of malaria recombinant vaccine in reticulum endoplasmic (RE) showed that N-glycosylation was limited to high-mannose glycoforms [98], which do not contain potentially allergenic plant-specific glycan modifications [98, 99]. This concept has been recently used for high-level production of PfAMA1 (> 510 µg/g fresh leaf weight) in RE of N. benthamiana plants and it was indicated that non-glycosylated antigen could adopt a native conformation and elicit strong growth inhibitory antibody responses in rabbits [100].
Transient Expression Systems as Malaria Therapies
Transient expression systems for recombinant protein production are favored because it allows large-scale production in weeks in cost-effective manner without genomic alterations. Compared to conventional cell culture-based and transgenic plants-based approaches that require long-developmental cycles, transient expression systems are promising alternatives for producing antimalarial vaccine in a relatively shorter time. The transient expression can be obtained systematically by infection of plant with replicating virus containing the sequence of a desired recombinant protein [101]. The transient expression can also be obtained by infiltration of tobacco or by its closed relative N. benthamiana with Agrobacterium tumefaciens carrying vector with desired gene sequence. In this context, desired gene can be transferred to the plant via T-DNA plasmid, which is part of a binary vector system in agrobacterium. Provided that expression vector remains an episomal DNA molecule, the gene expression is not altered by position effects. Moreover, due to genome integration-independent strategy, those of concerns related to spread of transgenic plants could be avoided. Additionally, by this system the expression of transgene can be determined within 3 h after transformation and after 18–48 h reaches the expression plateau and remains transcriptionally active for ~ 10 days [84, 101].
In the early phase of molecular farming, systemic and agro-infection were considered separate and competing strategies to produce recombinant proteins. However, during last decades, evidence indicated that agro-infection is more effective method for replicating viruses containing gene of interest. The latest landmark advancement in molecular farming and the emergence of deconstructed vectors rely on available plant viruses [102, 103]. In this new generation of vectors, unwanted viral genome components have been eliminated, leading to the assembly larger transgene while maintaining viral replication and transcription. Moreover, agroinoculation can remove limitations related to mechanically inoculation of nucleic acid into plants by virus vector and deliver targeted genes into plant cells [103]. MagnICON system as a deconstructed viral vector has been demonstrated for rapid, high‐level accumulation of numerous pharmaceuticals, up to 1 mg/g (FW) in shorter duration (7–10 days after agroinfiltration), [104,105,106,107], some of which are recently undergoing clinical evaluation [103]. The utilization of this system also has been reported for high production of malaria asexual blood-stage subunit vaccine, PyMSP4/5 (1–2 mg/g /Fwt) and MSP119 (3–4 mg/g Fwt) in N.benthamiana, and immunogenicity of both plant-made proteins was approved [108]. However, one of the challenges in transient expression system is the yield deviation among batches [109], which points out the process reproducibility concerns [110]. To ensure consistency, improvement of process parameter controls such as incubation time and temperature using VFUs facility could overcome such challenge [111]. Comprehensive information related to VFUs has been reviewed by Fischer and colleagues [110]. This approach has been successfully implemented for transient expression of recombinant proteins involved in influenza pandemic [112] and received governmental endorsement in the USA (Paul, et al. 2013). Spiegel and colleagues investigated the scalable transient expression platform for vaccine development against malaria [113]. Large quantity of targets comprising various stages of Plasmodium falciparum life cycle were investigated as potential vaccine candidate. In their research the results have demonstrated that transient expression is essential for developing multi-domain vaccine candidates against malaria that also offers scalability with convenience.
Leafy Plants as Promising Strategy for Oral Delivery of Malaria Vaccines
The global malaria vaccines market has grown significantly in the last few years, with market value of US$ 8.5 million in 2018. The market value is expected to reach approx. at a CAGR of 102.8% by 2024 as published by Coherent Market Insights. The growing demand for vaccine provokes the scientific community to discover alternative methods for its production at larger scale to meet future demands, worldwide. Malaria Vaccine Decision-Making framework estimated the cost of US$7 per dose, plus a $5 delivery cost for a vaccine targeting P. falciparum. However, drug availability at these huge costs make it unaffordable to most of the global population, as one-third earns less than $2 per day [114]. The large-scale production of PDs and its delivery are major factors that contribute to vaccine cost. These limits should be addressed by developing new strategies to reduce costs related to production and delivery of vaccine. An affordable malaria vaccine should be cost effective, efficient, and heat stable, requiring no skilled medical worker for its administration. Using genetic engineering in edible leafy plants for production of malaria vaccine and further oral administration of produced proteins can significantly overcome those hurdles related to downstream process.
In the past decades, significant efforts have been made to produce therapeutics proteins in transplastomic plants and the first report on production of recombinant protein and vaccine in transplastomic tobacco [114] opened new window in molecular farming. Compared to nuclear transformation system, integration of foreign gene into chloroplast genome occurs by homologous recombination, eliminating gene silencing and positional effects as well as pleiotropic effects involved in gene expression variation. Owing to the polyploidy of the chloroplast system with the presence of thousands of genomes per cell, astounding high level of protein production up to 72% of the total soluble protein was achieved [114]. Moreover, the incidence of horizontal gene transfer could be minimized due to maternal inheritance of chloroplast genome, offering transgene containment compared to pollenation. Orally delivered CTB-fused malaria proteins, AMA1 and MSP1 bioencapsulated in tobacco chloroplast elicited antibodies in mice and completely inhibited proliferation of the malarial parasite and cross-reacted with the native parasite proteins [115]. This strategy has also been used for production of CTB-Pfs25 of Ch. reinhardtii cells and oral delivery of freeze-dried whole cells elicited CTB-specific IgG antibodies and secretory IgA antibodies to both CTB and Pfs25 [116, 117].
Conclusion
The incidence of malaria infection is likely to increase because of socioeconomic conditions along with climate change and migration, the lack of coherent policy by health authorities for curbing the disease spread, and resistance to antimalarial drugs particularly single-drug administration in developing countries. The escalating population in the developing world with mushrooming malaria infections will increase demand for antimalaria agents. Regardless of advancement in biotechnological processes to provide enough supply for such agents, the production system of those are based on microbes or mammalian cells cultures limited in capacity which are unlikely to meet hiking future market demands. Therefore, as promising alternative, plants have natural ability to produce agents with antimalaria function such as quinine, lapinone, and artemisinin as well as the capacity to meet the challenge of producing effective and affordable protein drugs. The recent regulatory approval of orally delivered Palforzia by FDA will encourage the scientific community to bring more of their product to clinical trials following same regulatory pathway. In addition, advancement in stable, transient-based technologies is required to manufacture malaria related compounds those are capable to reduce price tag, eliminate the cold chain requirement, avoid downstream processing by oral delivery, increase the bioavailability by passing degradation. Also, scalability of these transient production system is critical and require further research to meet future needs and save millions of lives worldwide.
Data Availability
Not applicable.
Code Availability
Not applicable.
References
Lopez, G. R., Hernan, C., Moreno, L., Fernandez, E. V., Munoz, M. F., Delgado, A., Polo, M. J., & Andres, I. (2014). Malaria in developing countries. Journal of Infection in Developing Countries, 8, 1–4.
Gamo, F.-J., Sanz, L. M., Vidal, J., de Cozar, C., Alvarez, E., Lavandera, J.-L., Vanderwall, D. E., Green, D. V., Kumar, V., & Hasan, S. (2010). Thousands of chemical starting points for antimalarial lead identification. Nature, 465, 305.
Qayum, A., Arya, R., & Lynn, A. M. (2016). Ethnobotanical perspective of antimalarial plants: Traditional knowledge-based study. BMC Research Notes, 9, 67.
WHO (2019) World malaria report: World Health Organization. licence (CC BY-NC-SA 3.0 IGO; https://creativecommons.org/ licenses/by-nc-sa/3.0/igo).
Amimo, F., Lambert, B., & Magit, A. (2020). What does the COVID-19 pandemic mean for HIV, tuberculosis, and malaria control? Tropical Medical Health, 48, 32–32.
Sherrard-Smith, E., Hogan, A. B., Hamlet, A., Watson, O. J., Whittaker, C., Winskill, P., Ali, F., Mohammad, A. B., Uhomoibhi, P., Maikore, I., Ogbulafor, N., Nikau, J., Kont, M. D., Challenger, J. D., Verity, R., Lambert, B., Cairns, M., Rao, B., Baguelin, M., … Churcher, T. S. (2020). The potential public health consequences of COVID-19 on malaria in Africa. Nature Medicine, 26, 1411–1416.
WHO (2020) Global Malaria Programme: Tailoring Malaria Interventions in the COVID-19 Response. Retrieved from https://www.whoint/publications/m/item/tailoring-malaria-interventions-in-the-covid-19-response
Hoffman, S. L., Vekemans, J., Richie, T. L., & Duffy, P. E. (2015). The march toward malaria vaccines. Vaccine, 33, D13–D23.
Cox, F. E. (2010). History of the discovery of the malaria parasites and their vectors. Parasites & Vectors, 3(5), 2014.
Gaillard, T., Madamet, M., Tsombeng, F. F., Dormoi, J., & Pradines, B. (2016). Antibiotics in malaria therapy: Which antibiotics except tetracyclines and macrolides may be used against malaria? Malaria Journal, 15, 556–556.
Mishra, M., Mishra, V. K., Kashaw, V., Iyer, A. K., & Kashaw, S. K. (2017). Comprehensive review on various strategies for antimalarial drug discovery. European Journal of Medicinal Chemistry, 125, 1300–1320.
Gorobets, N. Y., Sedash, Y. V., Singh, B. K., & Rathi, B. (2017). An overview of currently available antimalarials. Current Topics in Medicinal Chemistry, 17, 2143–2157.
WHO (2013), Stuff, World malaria report.
Haldar, K., Bhattacharjee, S., & Safeukui, I. (2018). Drug resistance in Plasmodium. Nature Reviews Microbiology, 16, 156.
Nsanzabana, C., Djalle, D., Guérin, P. J., Ménard, D., & González, I. J. (2018). Tools for surveillance of anti-malarial drug resistance: An assessment of the current landscape. Malaria Journal, 17, 75.
WHO (2010). Global report on antimalarial drug efficacy and drug resistance, 2000–2010.
Organization, WH. (2015). Guidelines for the treatment of malaria. World Health Organization.
Ashley, E. A., & Phyo, A. P. (2018). Drugs in development for malaria. Drugs, 78, 861–879.
Okombo, J., & Chibale, K. (2018). Recent updates in the discovery and development of novel antimalarial drug candidates. Medical Chemistry Communication, 9, 437–453.
Ramakrishnan, G., Chandra, N., & Srinivasan, N. (2017). Exploring anti-malarial potential of FDA approved drugs: An in silico approach. Malaria Journal., 16, 290–290.
Travassos, M., Laufer, M (2017). Antimalarial drugs: An overview. UpToDate Waltham MA: Topic 468 Version 28.0
Willcox, M. L., & Bodeker, G. (2004). Traditional herbal medicines for malaria. British Medical Journal, 329, 1156.
Suleman, S., Beyene, T. T., Kebebe, D., Belew, S., Mekonnen, Y., Gashe, F., Mussa, S., Wynendaele, E., Duchateau, L., & De Spiegeleer, B. (2018). Treatment of malaria and related symptoms using traditional herbal medicine in Ethiopia. Journal Ethnopharmacol, 213, 262–279.
Kaur, R., & Kaur, H. (2017). Plant derived antimalarial agents. Journal of Medicinal Plants, 5, 346–363.
Nogueira, C. R., & Lopes, L. M. (2011). Antiplasmodial natural products. Molecules, 16, 2146–2190.
Memvanga, P. B., Tona, G. L., Mesia, G. K., Lusakibanza, M. M., & Cimanga, R. K. (2015). Antimalarial activity of medicinal plants from the Democratic Republic of Congo: A review. Journal of Ethnopharmacology, 169, 76–98.
Amoa Onguéné, P., Ntie-Kang, F., Lifongo, L. L., Ndom, J. C., Sippl, W., & Mbaze, LMa,. (2013). The potential of anti-malarial compounds derived from African medicinal plants. Part I: A pharmacological evaluation of alkaloids and terpenoids. Malaria Journal, 12, 449.
Ntie-Kang, F., Onguéné, P. A., Lifongo, L. L., Ndom, J. C., Sippl, W., & Mbaze, LMa,. (2014). The potential of anti-malarial compounds derived from African medicinal plants, part II: A pharmacological evaluation of non-alkaloids and non-terpenoids. Malaria Journal, 13, 81.
Muthaura, C., Keriko, J., Mutai, C., Yenesew, A., Gathirwa, J., Irungu, B., Nyangacha, R., Mungai, G., & Derese, S. (2015). Antiplasmodial potential of traditional phytotherapy of some remedies used in treatment of malaria in Meru-Tharaka Nithi County of Kenya. Journal of Ethnopharmacology, 175, 315–323.
Omara, T. (2020). Antimalarial plants used across Kenyan communities. Evidence-Based Complement Alternative Medicine, 12, 4538602.
Manya, M. H., Keymeulen, F., Ngezahayo, J., Bakari, A. S., Kalonda, M. E., Kahumba, B. J., Duez, P., Stévigny, C., & Lumbu, S. J. (2020). Antimalarial herbal remedies of Bukavu and Uvira areas in DR Congo: An ethnobotanical survey. Journal Ethnopharmacol, 249, 112422.
Bekono, B. D., Ntie-Kang, F., Onguéné, P. A., Lifongo, L. L., Sippl, W., Fester, K., & Owono, L. C. O. (2020). The potential of anti-malarial compounds derived from African medicinal plants: a review of pharmacological evaluations from 2013 to 2019. Malaria Journal, 19(1), 183.
Atanasov, A. G., Waltenberger, B., Pferschy-Wenzig, E.-M., Linder, T., Wawrosch, C., Uhrin, P., Temml, V., Wang, L., Schwaiger, S., & Heiss, E. H. (2015). Discovery and resupply of pharmacologically active plant-derived natural products: A review. Biotechnology Advances, 33, 1582–1614.
Singh, R. (2016). Chemotaxonomy: A tool for plant classification. Journal of Medicinal Plants, 4, 90–93.
Gra, z B., Falquet, J., Elisabetsky, E. (2010). Ethnopharmacology, sustainable development and cooperation: The importance of gathering clinical data during field surveys. Journal Ethnopharmacol, 130, 635–638.
Moreira, Dd. L., Teixeira, S. S., Monteiro, M. H. D., De-Oliveira, A. C. A. X., & Paumgartten, F. J. R. (2014). Traditional use and safety of herbal medicines. Revista Brasileira de Farmacognosia, 24, 248–257.
Pink, R., Hudson, A., Mouriès, M.-A., & Bendig, M. (2005). Opportunities and challenges in antiparasitic drug discovery. Nature reviews Drug discovery, 4, 727.
Rasoanaivo, P., Deharo, E., Ratsimamanga-Urveg, S., Frappier F. (2004). Guidelines for the nonclinical evaluation of the efficacy of traditional antimalarials. CRC Press, 256–268.
Camacho, M., Phillipson, J., Croft, S., Solis, P., Marshall, S., & Ghazanfar, S. (2003). Screening of plant extracts for antiprotozoal and cytotoxic activities. Journal of Ethnopharmacology, 89, 185–191.
Patwardhan, B., & Vaidya, A. D. (2010). Natural products drug discovery: Accelerating the clinical candidate development using reverse pharmacology approaches. Indian Journal of Experimental Biology, 3, 220–227.
Vaidya, A. D. (2006). Reverse pharmacological correlates of ayurvedic drug actions. Indian Journal of Pharmacology, 38, 311.
Willcox, M. L., Graz, B., Falquet, J., Diakite, C., Giani, S., & Diallo, D. (2011). A “reverse pharmacology” approach for developing an anti-malarial phytomedicine. Malaria Journal, 10, S8.
Simoes-Pires, C., Hostettmann, K., Haouala, A., Cuendet, M., Falquet, J., Graz, B., & Christen, P. (2014). Reverse pharmacology for developing an anti-malarial phytomedicine. The example of Argemone mexicana. International Journal for Parasitology: Drugs and Drug Resistance, 4, 338–346.
Ntamabyaliro, N. Y., Burri, C., Nzolo, D. B., Engo, A. B., Lula, Y. N., et al. (2018). Drug use in the management of uncomplicated malaria in public health facilities in the Democratic Republic of the Congo. Malaria Journal, 17, 189.
Folashade, O., Omoregie, H., & Ochogu, P. (2012). Standardization of herbal medicines-A review. International Journal of Biodiversity and Conservation, 4, 101–112.
Houghton, P., Howes, M.-J., Lee, C., & Steventon, G. (2007). Uses and abuses of in vitro tests in ethnopharmacology: Visualizing an elephant. Journal of Ethnopharmacology, 110, 391–400.
Williamsonm, E. M. (2001). Synergy and other interactions in phytomedicines. Phytomedicine, 8, 401–409.
Ma, X., Zheng, C., Han, L., Xie, B., Jia, J., Cao, Z., Li, Y., & Chen, Y. (2009). Synergistic therapeutic actions of herbal ingredients and their mechanisms from molecular interaction and network perspectives. Drug Discovery Today, 14, 579–588.
Tegos, G., Stermitz, F. R., Lomovskaya, O., & Lewis, K. (2002). Multidrug pump inhibitors uncover remarkable activity of plant antimicrobials. Antimicrobial Agents and Chemotherapy, 46, 3133–3141.
Jia, J., Zhu, F., Ma, X., Cao, Z. W., Li, Y. X., & Chen, Y. Z. (2009). Mechanisms of drug combinations: Interaction and network perspectives. Nature Rreviews Drug Discovery, 8, 111.
Tran, Q. L., Tezuka, Y., Ueda, J. Y., Nguyen, N. T., Maruyama, Y., et al. (2003). In vitro antiplasmodial activity of antimalarial medicinal plants used in Vietnamese traditional medicine. Journal Ethnopharmacol, 86, 249–252.
Yarnell, E. (2015). Synergy in herbal medicines: Part 1. Journal of Restorative Medicine, 4, 60–73.
Fivelman, Q. L., Adagu, I. S., & Warhurst, D. C. (2004). Modified fixed-ratio isobologram method for studying in vitro interactions between atovaquone and proguanil or dihydroartemisinin against drug-resistant strains of Plasmodium falciparum. Antimicrobial Agents Chemotherapy, 48, 4097–410267.
Bunnag, D., Harinasuta, T., Looareesuwan, S., Chittamas, S., Pannavut, W., Berthe, J., & Mondesir, J. M. (1989). A combination of quinine, quinidine and cinchonine (LA 40221) in the treatment of chloroquine resistant falciparum malaria in Thailand: Two double-blind trials. Transactions of the Royal Society of Tropical Medicine and Hygiene, 83, 66.
Sowunmi, A., Salako, L. A., Laoye, O. J., & Aderounmu, A. F. (1990). Combination of quinine, quinidine and cinchonine for the treatment of acute falciparum malaria: Correlation with the susceptibility of Plasmodium falciparum to the cinchona alkaloids in vitro. Transactions of the Royal Society of Tropical Medicine and Hygiene, 84, 626–629.
Rasoanaivo, P., Wright, C. W., Willcox, M. L., & Gilbert, B. (2011). Whole-plant extracts versus single compounds for the treatment of malaria: Synergy and positive interactions. Malaria journal., 10, S4–S4.
Odugbemi, T. O., Akinsulire, O. R., Aibinu, I. E., & Fabeku, P. O. (2007). Medicinal plants useful for malaria therapy in Okeigbo, Ondo State, Southwest Nigeria. African Journal of Traditional, Complementary, and Alternative Medicines, 4, 191–198.
Wells, T. N. C. (2011). Natural products as starting points for future anti-malarial therapies: Going back to our roots? Malaria Journal, 10, S3–S3.
Hirt, H., & M’Pia, B. (2008). Natural medicine in the tropics I: Foundation text (p. 2008). Winnenden, Germany: Anamed.
Habibi, P., Daniell, H., Soccol, C. R., & Grossi-de-Sa, M. F. (2019). The potential of plant systems to break the HIV-TB link. Plant Biotechnology Journal, 17(10), 1868–1891. https://doi.org/10.1128/AEM.00714-13
Habibi, P., Prado, G.S., Pelegrini, P.B., Hefferon, K.L., Soccol, C.R. and Grossi-de-Sa, M.F., 2017. Optimization of inside and outside factors to improve recombinant protein yield in plant. Plant Cell, Tissue and Organ Culture (PCTOC), 130(3), 449–467. https://doi.org/10.1007/s11240-017-1240-5
Farré, G., Blancquaert, D., Capell, T., Van, D., Straeten, D., Christou, P., & Zhu, C. (2014). Engineering complex metabolic pathways in plants. Annual Review of Plant Biology, 65, 187–223.
Staniek, A., Bouwmeester, H., Fraser, P. D., Kayser, O., et al. (2013). Natural products–modifying metabolite pathways in plants. Biotechnology Journal, 8, 1159–1171.
WHO (2014). Status Report on Artemisinin Resistance: September 2014. Geneva: World Health Organisation; http://www.who.int/malaria/publications/atoz/status-rep-artemisinin-resistance-sep2014.pdf.
Zeng, Q., Qiu, F., & Yuan, L. (2008). Production of artemisinin by genetically-modified microbes. Biotechnology Letters, 30, 581–592.
WHO (2014) World Malaria Report. Geneva: World Health Organisation; http://www.who.int/malaria/publications/world_malaria_report_2014/en/
Nair, P., Misra, A., Singh, A., Shukla, A. K., Gupta, M. M., Gupta, A. K., Gupta, V., Khanuja, S. P., & Shasany, A. K. (2013). Differentially expressed genes during contrasting growth stages of Artemisia annua for artemisinin content. PLoS ONE, 8, e60375.
Tang, K., Shen, Q., Yan, T., & Fu, X. (2014). Transgenic approach to increase artemisinin content in Artemisia annua L. Plant Cell Reproduction, 33, 605–615.
Alam, P., & Abdin, M. Z. (2011). Over-expression of HMG-CoA reductase and amorpha-4,11-diene synthase genes in Artemisia annua L. and its influence on artemisinin content. Plant Cell Reproduction, 10, 1919–1928.
Wang, Y., Fuyuan, J., Shuoye, Yu., Yunfei, C., et al. (2011). Co-overexpression Co-overexpression of the HMGR and FPS genes enhances artemisinin content in Artemisia annua L. Journal of Medicinal Plants Research, 15, 3396–3403.
Farhim, M., Marhevkam, E., Ben-Arim, J., Algamas-Dimantovm, A., et al. (2011). Generation of the potent anti-malarial drug artemisinin in tobacco. Nature Biotechnology, 29, 1072–1074.
Fuentes, P., Zhou, F., Erban, A., Karcher, D., Kopka, J., Bock, R. (2016). A new synthetic biology approach allows transfer of an entire metabolic pathway from a medicinal plant to a biomass crop. eLife, 5.
Malhotra, K., Subramaniyan, M., Rawat, K., et al. (2016). Compartmentalized metabolic engineering for artemisinin biosynthesis and effective malaria treatment by oral delivery of plant cells. Molecular Plant, 9, 1464–1477.
Saxena, B., Subramaniyan, M., Malhotra, K., Bhavesh, N. S., Potlakayala, S. D., & Kumar, S. (2014). Metabolic engineering of chloroplasts for artemisinic acid biosynthesis and impact on plant growth. Journal of Biosciences, 39, 33–41.
Zhang, Y., Nowak, G., Reed, D. W., & Covello, P. S. (2011). The production of artemisinin precursors in tobacco. Plant Biotechnol Journal, 9, 445–454.
Khairul, N. K. B., Beyraghdar, A., Peramuna, A. V., Krol, A. R., Bouwmeester, H., & Simonsen, H. T. (2017). Stable production of the antimalarial drug artemisinin in the moss physcomitrella patens. Frontiers in Bioengineering and Biotechnology, 5, 47–47.
Ahlawat, S., Saxena, P., Alam, P., Wajid, S., & Abdin, M. (2014). Modulation of artemisinin biosynthesis by elicitors, inhibitor, and precursor in hairy root cultures of Artemisia annua L. Journal of Plant Interactions, 9, 811–824.
Baldi, A., & Dixit, V. (2008). Yield enhancement strategies for artemisinin production by suspension cultures of Artemisia annua. Bioresource Technology, 99, 4609–4614.
Caretto, S., Quarta, A., Durante, M., Nisi, R., De Paolis, A., Blando, F., & Mita, G. (2011). Methyl jasmonate and miconazole differently affect arteminisin production and gene expression in Artemisia annua suspension cultures. Plant Biology, 13, 51–58.
Liu, C.-Z., Wang, Y.-C., Guo, C., Ouyang, F., Ye, H.-C., & Li, G.-F. (1998). Production of artemisinin by shoot cultures of Artemisia annua L. in a modified inner-loop mist bioreactor. Plant Science, 135, 211–217.
Georgiev, M. I., & Weber, J. (2014). Bioreactors for plant cells: Hardware configuration and internal environment optimization as tools for wider commercialization. Biotechnology Letters, 36, 1359–1367.
Ahmadi, Y., Piri, K., Bahramnejad, B., & Habibi, P. (2013). Methyl Jasmonate and Salicylic acid effects on the dopamine production in hairy cultures of Portulaca oleracea (purslan). Environmental Pharmacolology Life Science, 2, 6.
Habibi, P., & de, MFG, da Silva, ALL., Makhzoum, A., da Luz Costa, J., Borghetti, IA., Soccol, CR. (2016). Efficient genetic transformation and regeneration system from hairy root of Origanum vulgare. Physiology and Molecular Biology of Plants, 22, 271–277.
Habibi, P., De Sa, M. F. G., Makhzoum, A., Malik, S., da Silva, A. L. L., Hefferon, K., & Soccol, C. R. (2017). Bioengineering hairy roots: Phytoremediation, secondary metabolism, molecular pharming, plant-plant interactions and biofuels. In E. Lichtfouse (Ed.), Sustainable agriculture reviews (pp. 213–251). Cham: Springer International Publishing.
Habibi, P., Piri, K., Deljo, A., Moghadam, Y. A., & Ghiasvand, T. (2015). Increasing Scopolamine content in hairy roots of atropa belladonna using bioreactor. Brazilian Archives of Biology and Technology, 58, 166–174.
Habibi, P., Soccol, CR., Grossi-de-Sa, MF. (2018). Hairy root-mediated biotransformation: Recent advances and exciting prospects. In Book: Hairy roots-an effective tool of plant biotechnology: Genesis to application publisher. Springer Nature: Singapore.
Ali, M., Abbasi, B. H., Ahmad, N., Khan, H., & Ali, G. S. (2017). Strategies to enhance biologically active-secondary metabolites in cell cultures of Artemisia–current trends. Critical Reviews in Biotechnology, 37, 833–851.
Liu, C.-Z., Guo, C., Wang, Y., & Ouyang, F. (2003). Factors influencing artemisinin production from shoot cultures of Artemisia annua L. World Journal of Microbiology and Biotechnology, 19, 535–538.
Patra, N., & Srivastava, A. K. (2015). Use of model-based nutrient feeding for improved production of artemisinin by hairy roots of Artemisia annua in a modified stirred tank bioreactor. Applied Biochemistry and Biotechnology, 177, 373–388.
Habibi, P., Soccol, C. R., O’Keefe, B. R., Krumpe, L. R. H., Wilson, J., et al. (2018). Gene-silencing suppressors for high-level production of the HIV-1 entry inhibitor griffithsin in Nicotiana benthamiana. Process Biochemistry, 70, 45–54.
Arlen, P. A., Falconer, R., Cherukumilli, S., Cole, A., Cole, A. M., Oishi, K. K., & Daniel, l H. (2007). Field production and functional evaluation of chloroplast-derived interferon-alpha2b. Plant Biotechnol Journal, 5, 511–525.
Buyel, J., Twyman, R., & Fischer, R. (2017). Very-large-scale production of antibodies in plants: The biologization of manufacturing. Biotechnology Advances, 35, 458–465.
Holtz, B. R., Berquist, B. R., Bennett, L. D., Kommineni, V. J., Munigunti, R. K., White, E. L., et al. (2015). Commercial-scale biotherapeutics manufacturing facility for plant-made pharmaceuticals. Plant Biotechnology Journal, 13, 1180–1190.
Riley, E. M., & Stewart, V. A. (2013). Immune mechanisms in malaria: New insights in vaccine development. Nature Medicine, 19, 168.
Laurens, M. B. (2018). The promise of a malaria vaccine—Are we closer? Annual Review of Microbiology, 72, 273–292.
Clemente, M., & Corigliano, M. G. (2012). Overview of plant-made vaccine antigens against malaria. Journal of Biomedicine and Biotechnology, 2012, 8.
Farrance, C. E., Chichester, J. A., Musiychuk, K., Shamloul, M., Rhee, A., Manceva, S. D., et al. (2011). Antibodies to plant-produced Plasmodium falciparum sexual stage protein Pfs25 exhibit transmission blocking activity. Human Vaccines, 7, 191–198.
Sriraman, R., Bardor, M., Sack, M., Vaquero, C., Faye, L., Fischer, R., Finnern, R., & Lerouge, P. (2004). Recombinant anti-hCG antibodies retained in the endoplasmic reticulum of transformed plants lack core-xylose and core-α (1, 3)-fucose residues. Plant Biotechnology Journal, 2, 279–287.
Bardor, M., Faveeuw, C., Fitchette, A.-C., Gilbert, D., Galas, L., Trottein, F., Faye, L., & Lerouge, P. (2003). Immunoreactivity in mammals of two typical plant glyco-epitopes, core α (1, 3)-fucose and core xylose. Glycobiology, 13, 427–434.
Boes, A., Spiegel, H., Edgue, G., Kapelski, S., Scheuermayer, M., Fendel, R., Remarque, E., Altmann, F., Maresch, D., & Reimann, A. (2015). Detailed functional characterization of glycosylated and nonglycosylated variants of malaria vaccine candidate Pf AMA 1 produced in Nicotiana benthamiana and analysis of growth inhibitory responses in rabbits. Plant Biotechnology Journal, 13, 222–234.
Glick, B. R., Patten, J. P. J., & Li, C. (2010). Molecular biotechnology: Principles and applications of recombinant DNA (4th ed.). John Wiley & Sons.
Gleba, Y. Y., Tusé, D., & Giritch, A. (2013). Plant viral vectors for delivery by Agrobacterium. In K. Palmer & Y. Gleba (Eds.), Plant viral vectors (pp. 155–192). Berlin Heidelberg: Springer.
Peyret, H., & Lomonossoff, G. P. (2015). When plant virology met Agrobacterium: The rise of the deconstructed clones. Plant Biotechnology Journal, 13, 1121–1135.
Giritch, A., Marillonnet, S., Engler, C., van Eldik, G., Botterman, J., Klimyuk, V., & Gleba, Y. (2006). Rapid high-yield expression of full-size IgG antibodies in plants coinfected with noncompeting viral vectors. Proceedings of the National Academy of Sciences of the United States of America., 103, 14701–14706.
He, X., Haselhorst, T., von Itzstein, M., Kolarich, D., Packer, N. H., & Kermode, A. R. (2012). Influence of an ER-retention signal on the N-glycosylation of recombinant human alpha-L-iduronidase generated in seeds of Arabidopsis. Plant Molecular Biology, 79, 157–169.
Lai, H., & Chen, Q. (2012). Bioprocessing of plant-derived virus-like particles of Norwalk virus capsid protein under current good manufacture practice regulations. Plant Cell Reports, 31, 573–584.
Phoolcharoen, W., Bhoo, S. H., Lai, H., Ma, J., Arntzen, C. J., Chen, Q., & Mason, H. S. (2011). Expression of an immunogenic Ebola immune complex in Nicotiana benthamiana. Plant Biotechnology Journal, 9, 807–816.
Webster, D. E., Wang, L., Mulcair, M., Ma, C., Santi, L., Mason, H. S., Wesselingh, S. L., & Coppel, R. L. (2009). Production and characterization of an orally immunogenic Plasmodium antigen in plants using a virus-based expression system. Plant Biotechnol Journal, 7, 846–855.
O’Neill, K. M., Larsen, J. S., & Curtis, W. R. (2008). Scale-up of Agrobacterium-mediated transient protein expression in bioreactor-grown Nicotiana glutinosa plant cell suspension culture. Biotechnology Progress, 2, 372–376.
Fischer, R., Schillberg, S., Hellwig, S., Twyman, R. M., & Drossard, J. (2012). GMP issues for recombinant plant-derived pharmaceutical proteins. Biotechnol Advances, 30, 434–439.
Buyela, J. F. (2018). Plants as sources of natural and recombinant anti-cancer agents. Biotechnology advances, 36, 506–520.
Stoger, E., Fischer, R., Moloney, M., & Ma, J. K. C. (2014). Plant molecular pharming for the treatment of chronic and infectious diseases. Annual Reviews Plant Biology, 65, 743–768.
Spiegel, H., Boes, A., Voepel, N., Beiss, V., Edgue, G., Rademacher, T., Sack, M., Schillberg, S., Reimann, A., & Fischer, R. (2015). Application of a scalable plant transient gene expression platform for malaria vaccine development. Frontiers in Plant Science, 6, 1169.
Khan, I., & Daniell, H. (2021). Oral delivery of therapeutic proteins bioencapsulated in plant cells: Preclinical and clinical advances. Current Opinion in Colloid Interface Sciences, 54, 101452.
Davoodi-Semiromi, A., Schreiber, M., Nalapalli, S., Verma, D., Singh, N. D., Banks, R. K., et al. (2010). Chloroplast-derived vaccine antigens confer dual immunity against cholera and malaria by oral or injectable delivery. Plant Biotechnology Journal, 8, 223–242.
Gregory, J. A., Topol, A. B., Doerner, D. Z., Mayfield, S. (2013). Algae-produced cholera toxin-Pfs25 fusion proteins as oral vaccines. Applied and Environmental Microbiology, 00714–00713.
Srinivasan, A., Herzog, R. W., Khan, I., Sherman, A., Bertolini, T., Wynn, T., et al. (2021). Preclinical development of plant-based oral immune-modulatory therapy for haemophilia B. Plant Biotechnology Journal, 10, 1952–1966.
Druilhe, P., Brandicourt, O., Chongsuphajaisiddhi, T., & Berthe, J.(1988). Activity of a combination of three cinchona bark alkaloids against Plasmodium falciparum in vitro. Antimicrobial agents and Chemotherapy, 32(2), 250–254. https://doi.org/10.1128/AAC.32.2.250
Elford, B. C., Roberts, M. F., Phillipson, J. D., & Wilson R. J. (1987). Potentiation of the antimalarial activity of qinghaosu by methoxylated flavones. Transactions of the Royal Society of Tropical Medicine and Hygiene 81(3), 434–436.
Dwivedi, V., Khan, A., Vasco, A., Fatima, N., Soni, V. K., Dangi, A., Misra-Bhattacharya, S., & Owais, M. (2008). Immunomodulator effect of picroliv and its potential in treatment against resistant Plasmodium yoelii (MDR) infection in mice. Pharmaceutical Research, 25(10), 2312–2319.
Mishra, K., Dash, A. P., Swain, B. K., & Dey, N. (2009). Anti-malarial activities of Andrographis paniculata and Hedyotis corymbosa extracts and their combination with curcumin. Malaria Journal, 8(1), 1–9. https://doi.org/10.1186/1475-2875-8-26
Iwalokun, B. (2008). Enhanced antimalarial effects of chloroquine by aqueous Vernonia amygdalina leaf extract in mice infected with chloroquine resistant and sensitive Plasmodium berghei strains. African Health Sciences, 8(1), 25–35.
Mbacham, W. F., Njuabe, M. T., Evehe, M. S., Moyou, R., & Ekobo, A. (2005) Antimalarial drug studies in cameroon reveal deteriorating fansidar and amodiaquine cure rates. Journal of the Cameroon Academy of Sciences, 5, 58–63.
Delhaes, L., Abessolo, H., Biot, C., Berry, L., Delcourt, P., Maciejewski, L., Brocard, J., Camus, D., & Dive, D. (2001). In vitro and in vivo antimalarial activity of ferrochloroquine, a ferrocenyl analogue of chloroquine against chloroquine-resistant malaria parasites. Parasitology Research, 87(3), 239–244. https://doi.org/10.1007/s004360000317
Frederich, M., Hayette, M. P., Tits, M., De Mol, P., & Angenot, L. (2001). Reversal of chloroquine and mefloquine resistance in Plasmodium falciparum by the two monoindole alkaloids, icajine and isoretuline. Planta medica, 67(06), 523–527. https://doi.org/10.1055/s-2001-16476
Sannella, A. R., Messori, L., Casini, A., Vincieri, F. F., Bilia, A. R., Majori, G. & Severini, C. (2007). Antimalarial properties of green tea. Biochemical and Biophysical Research Communications, 353(1), 177–181. https://doi.org/10.1016/j.bbrc.2006.12.005
Nandakumar, D. N., Nagaraj, V. A., Vathsala, P. G., Rangarajan, P. & Padmanaban, G. (2006). Curcumin-artemisinin combination therapy for malaria. Antimicrobial Agents and Chemotherapy, 50(5), 1859–1860. https://doi.org/10.1128/AAC.50.5.1859-1860.2006
Adegbolagun, O. M., Emikpe, B. O., Woranola, I. O. & Ogunremi, Y. (2013). Synergistic effect of aqueous extract of Telfaria occidentalis on the biological activities of artesunate in Plasmodium berghei infected mice. African Health Sciences, 13(4), 970–976. https://doi.org/10.4314/ahs.v13i4.16
Shoba, G., Joy, D., Joseph, T., Majeed, M., Rajendran, R. & Srinivas, P. (1998). Influence of piperine on the pharmacokinetics of curcumin in animals and human volunteers. Planta Medica, 64(04), 353–356. https://doi.org/10.1055/s-2006-957450
Lambert, J. D., Hong, J., Kim, D. H., Mishin, V. M., & Yang, C. S. (2004). Piperine enhances the bioavailability of the tea polyphenol (−)-epigallocatechin-3-gallate in mice. The Journal of nutrition, 134(8), 1948–1952. https://doi.org/10.1093/jn/134.8.1948
Vathsala, P. G., Dende, C., Nagaraj, V. A., Bhattacharya, D., Das, G., Rangarajan, P. N., & Padmanaban, G. (2012). Curcumin-arteether combination therapy of Plasmodium berghei-infected mice prevents recrudescence through immunomodulation. PloS One, 7(1), e29442. https://doi.org/10.1371/journal.pone.0029442
Rasoanaivo, P., Wright, C. W., Willcox, M. L. & Gilbert, B. (2011). Whole plant extracts versus single compounds Whole plant extracts versus single compounds for the treatment of malaria: synergy and positive interactions. Malaria Journal, 10(1), 1–12. https://doi.org/10.1186/1475-2875-10-S1-S4
Wang, L., Webster, D. E., Campbell, A. E., Dry, I. B., Wesselingh, S. L. & Coppel, R. L. (2008). Immunogenicity of Plasmodium yoelii merozoite surface protein 4/5 produced in transgenic plants. International Journal for Parasitology, 38(1), 103–110. https://doi.org/10.1016/j.ijpara.2007.06.005
Webster, D. E., Wang, L., Mulcair, M., Ma, C., Santi, L., Mason, H. S., Wesselingh, S. L. & Coppel, R. L. (2009). Production and characterization of an orally immunogenic Plasmodium antigen in plants using a virus-based expression system. Plant Biotechnology Journal, 7(9), 846–855. https://doi.org/10.1111/j.1467-7652.2009.00447.x
Ma, C., Wang, L., Webster, D. E., Campbell, A. E., & Coppel, R. L. (2012). Production, characterisation and immunogenicity of a plant-made Plasmodium antigen—the 19 kDa C-terminal fragment of Plasmodium yoelii merozoite surface protein 1. Applied Microbiology and Biotechnology, 94(1), 151–161. https://doi.org/10.1007/s00253-011-3772-7
Lau, O. S., Ng, D. W.-K., Chan, W. W. L., Chang, S. P. & Sun, S. S. (2010). Production of the 42-kDa fragment of Plasmodium falciparum merozoite surface protein 1, a leading malaria vaccine antigen, in Arabidopsis thaliana seeds. Plant Biotechnology Journal, 8(9), 994–1004. https://doi.org/10.1111/j.1467-7652.2010.00526.x
Davoodi-Semiromi, A., Schreiber, M., Nalapalli, S., Verma, D., Singh, N. D., Banks, R. K., Chakrabarti, D., & Daniell, H. (2010). Chloroplast-derived vaccine antigens confer dual immunity against cholera and malaria by oral or injectable delivery. Plant Biotechnology Journal, 8(2), 223–242.
Lee, C., Kim, H. H., Mi Choi, K., Won Chung, K., Choi, Y. K., Jang, M. J., Kim, T. S., Chung, N. J., Rhie, H. G., Lee, H. S., & Sohn, Y. (2011). Murine immune responses to a Plasmodium vivax-derived chimeric recombinant protein expressed in Brassica napus. Malaria Journal, 10(1), 1–10. https://doi.org/10.1186/1475-2875-10-106
Farrance, C. E., Rhee, A., Jones, R. M., Musiychuk, K., Shamloul, M., Sharma, S., Mett, V., Chichester, J. A., Streatfield, S. J., Roeffen, W., & van de Vegte-Bolmer, M. (2011). A plant-produced Pfs230 vaccine candidate blocks transmission of Plasmodium falciparum. Clinical and Vaccine Immunology, 18(8), 1351–1357. https://doi.org/10.1128/CVI.05105-11
Jones, R. M., Chichester, J. A., Manceva, S., Gibbs, S. K., Musiychuk, K., Shamloul, M., Norikane, J., Streatfield, S. J., van de Vegte-Bolmer, M., Roeffen, W.. & Sauerwein, R. W. (2015). A novel plant-produced Pfs25 fusion subunit vaccine induces long-lasting transmission blocking antibody responses. Human Vaccines & Immunotherapeutics, 11(1), 124–132. https://doi.org/10.4161/hv.34366
Gregory, J. A., Li, F., Tomosada, L. M., Cox, C. J., Topol, A. B., Vinetz, J. M., & Mayfield, S. (2012). Algae-produced Pfs25 elicits antibodies that inhibit malaria transmission. PloS One, 7(5), e37179. https://doi.org/10.1371/journal.pone.0037179
Beiss, V., Spiegel, H., Boes, A., Kapelski, S., Scheuermayer, M., Edgue, G., Sack, M., Fendel, R., Reimann, A., Schillberg, S., & Pradel, G. (2015). Heat-precipitation allows the efficient purification of a functional plant-derived malaria transmission-blocking vaccine candidate fusion protein. Biotechnology and Bioengineering, 112(7), 1297–1305. https://doi.org/10.1002/bit.25548
Beiss, V., Spiegel, H., Boes, A., Scheuermayer, M., Reimann, A., Schillberg, S., & Fischer, R. (2015). Plant expression and characterization of the transmission-blocking vaccine candidate Pf GAP50. BMC Biotechnology, 15(1), 1–10. https://doi.org/10.1186/s12896-015-0225-x
Voepel, N., Boes, A., Edgue, G., Beiss, V., Kapelski, S., Reimann, A., Schillberg, S., Pradel, G., Fendel, R., Scheuermayer, M., & Spiegel, H. (2014). Malaria vaccine candidate antigen targeting the pre-erythrocytic stage of Plasmodium falciparum produced at high level in plants. Biotechnology Journal, 9(11), 1435–1445. https://doi.org/10.1002/biot.201400350
Boes, A., Spiegel, H., Voepel, N., Edgue, G., Beiss, V., Kapelski, S., Fendel, R., Scheuermayer, M., Pradel, G., Bolscher, J. M., & Behet, M. C. (2015). Analysis of a multi-component multi-stage malaria vaccine candidate—tackling the cocktail challenge. PloS One, 10(7), e0131456. https://doi.org/10.1371/journal.pone.0131456
Jones, R. M., Chichester, J. A., Mett, V., Jaje, J., Tottey, S., Manceva, S., Casta, L. J., Gibbs, S. K., Musiychuk, K., Shamloul, M., & Norikane, J. (2013). A plant-produced Pfs25 VLP malaria vaccine candidate induces persistent transmission blocking antibodies against Plasmodium falciparum in immunized mice. PloS One, 8(11), e79538. https://doi.org/10.1371/journal.pone.0079538
Gregory, J. A., Topol, A. B., Doerner, D. Z., & Mayfield, S. (2013). Alga-produced cholera toxin-Pfs25 fusion proteins as oral vaccines. Applied and Environmental Microbiology, 79(13), 3917–3925. https://doi.org/10.1128/AEM.00714-13
Funding
Not applicable.
Author information
Authors and Affiliations
Corresponding author
Ethics declarations
Conflicts of Interest
No conflict of interest.
Ethical Approval
Not applicable.
Consent to Participate
Not applicable.
Consent for Publication
Not applicable.
Additional information
Publisher's Note
Springer Nature remains neutral with regard to jurisdictional claims in published maps and institutional affiliations.
Rights and permissions
About this article
Cite this article
Habibi, P., Shi, Y., Fatima Grossi-de-Sa, M. et al. Plants as Sources of Natural and Recombinant Antimalaria Agents. Mol Biotechnol 64, 1177–1197 (2022). https://doi.org/10.1007/s12033-022-00499-9
Received:
Accepted:
Published:
Issue Date:
DOI: https://doi.org/10.1007/s12033-022-00499-9