Abstract
Lung cancer is the prime cause of cancer-related deaths globally, with a contribution of 85% from non-small cell lung cancer. Before a few decades back, conventional chemotherapy was the most chosen treatment option for NSCLC but with side effects. Now, the treatment approaches have shifted to a new trend, targeted therapy, and a better treatment strategy with minimal side effects compared to chemotherapy. Advances in technologies and understanding the pathways lead to the discovery of new targets and through which it is possible to improve treatment outcomes and patient compliance. Unlike chemotherapy, targeted therapy focuses on the tumor cells and does not produce toxicity to healthy cells. The last two decades were very crucial in the development of many small molecules with the capability to target-specific proteins or genes in the disease progression pathway. Although the targeted therapy approach was a gemstone with many successful drugs for the treatment of NSCLC, various resistance mechanisms and activation of bypass signaling pathways put many of these drugs in the trash. In this review, we will discuss the major targeted proteins involved in NSCLC as well as the inhibitor drugs developed to target them for now and along with the future directions.
Graphical abstract




Similar content being viewed by others
Abbreviations
- ALK:
-
Anaplastic lymphoma kinase
- ATP:
-
Adenosine triphosphate
- C:
-
Cysteine
- EGF:
-
Epidermal growth factor
- EGFR:
-
Epidermal growth factor receptor
- FGF:
-
Fibroblast growth factor
- FGFR:
-
Fibroblast growth factor receptors
- HER:
-
Human epidermal growth factor receptor
- KRAS:
-
Kirsten rat sarcoma 2 viral oncogene
- L:
-
Leucine
- M:
-
Methionine
- MET:
-
Mesenchymal epithelial transition
- MPLC:
-
Multiple primary lung cancer
- NSCLC:
-
Non-small cell lung cancer
- NTRK:
-
Neurotrophic tyrosine receptor kinase
- ORR:
-
Overall response rate
- OS:
-
Overall survival
- PFS:
-
Progression-free survival
- R:
-
Arginine
- RET:
-
Rearranged during transfection
- RTK:
-
Receptor tyrosine kinase
- S:
-
Serine
- SCLC:
-
Small cell lung cancer
- SOS:
-
Son of sevenless
- T:
-
Threonine
- TKI:
-
Tyrosine kinase inhibitor
- VEGF:
-
Vascular endothelial growth factor
- VEGFR:
-
Vascular endothelial growth factor receptor
References
Cancer n.d. https://www.who.int/news-room/fact-sheets/detail/cancer. Accessed 2 Oct 2021.
Malik PS, Raina V. Lung cancer: prevalent trends & emerging concepts. Indian J Med Res Suppl. 2015;141:5–7. https://doi.org/10.4103/0971-5916.154479.
Types of Lung Cancer: Common, Rare and More Varieties | CTCA n.d. https://www.cancercenter.com/cancer-types/lung-cancer/types. Accessed 7 Nov 2021
Raut NV, Srivastava S, Gangwani GD, Ali HS. A case report of primary resistance to EGFR TKI in lung adenocarcinoma due to coexisting MET Exon 14 skipping mutation with excellent response to combination of Gefitinib and Capmatinib. Indian J Med Paediatr Oncol. 2021;42:204–7. https://doi.org/10.1055/s-0041-1731851.
Treating Non-Small Cell Lung Cancer n.d.:1–46. https://www.cancer.org/cancer/lung-cancer/treating-non-small-cell.html
Yuan M, Huang LL, Chen JH, Wu J, Xu Q. The emerging treatment landscape of targeted therapy in non-small-cell lung cancer. Signal Transduct Target Ther. 2019. https://doi.org/10.1038/s41392-019-0099-9.
Parambi DGT, Noorulla KM, Uddin MS, Mathew B. Epidermal growth factor receptor: promising targets for non-small-cell lung cancer. Oxid Stress Lung Dis. 2020;2:465–71. https://doi.org/10.1007/978-981-32-9366-3_21.
Aita M, Fasola G, Defferrari C, Brianti A, Bello MGD, Follador A, et al. Targeting the VEGF pathway: antiangiogenic strategies in the treatment of non-small cell lung cancer. Crit Rev Oncol Hematol. 2008;68:183–96. https://doi.org/10.1016/j.critrevonc.2008.05.002.
Yarden Y, Sliwkowski MX. Untangling the ErbB signalling network. Nat Rev Mol Cell Biol. 2001;2:127–37. https://doi.org/10.1038/35052073.
Antonicelli A, Cafarotti S, Indini A, Galli A, Russo A, Cesario A, et al. EGFR-targeted therapy for non-small cell lung cancer: focus on EGFR oncogenic mutation. Int J Med Sci. 2013. https://doi.org/10.7150/ijms.4609.
Chan BA, Hughes BGM. Targeted therapy for non-small cell lung cancer: current standards and the promise of the future. Transl Lung Cancer Res. 2015;4:36–54. https://doi.org/10.3978/j.issn.2218-6751.2014.05.01.
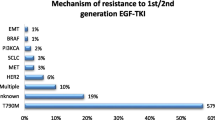
Stewart EL, Tan SZ, Liu G, Tsao MS. Known and putative mechanisms of resistance to EGFR targeted therapies in NSCLC patients with EGFR mutations—a review. Transl Lung Cancer Res. 2015;4:67. https://doi.org/10.3978/J.ISSN.2218-6751.2014.11.06.
Chang YS, Choi CM, Lee JC. Mechanisms of epidermal growth factor receptor tyrosine kinase inhibitor resistance and strategies to overcome resistance in lung adenocarcinoma. Tuberc Respir Dis. 2016;79:248. https://doi.org/10.4046/TRD.2016.79.4.248.
Shepherd FA, Rodrigues Pereira J, Ciuleanu T, Tan EH, Hirsh V, Thongprasert S, et al. Erlotinib in previously treated non-small-cell lung cancer. N Engl J Med. 2005. https://doi.org/10.1056/NEJMOA050753.
Thatcher N, Chang A, Parikh P, Pereira JR, Ciuleanu T, Von Pawel J, et al. Gefitinib plus best supportive care in previously treated patients with refractory advanced non-small-cell lung cancer: results from a randomised, placebo-controlled, multicentre study (Iressa Survival Evaluation in Lung Cancer). Lancet. 2005;366:1527–37. https://doi.org/10.1016/S0140-6736(05)67625-8.
Thomas P, Vincent B, George C, Joshua J, Pavithran K, Vijayan M. A comparative study on erlotinib & gefitinib therapy in non-small cell lung carcinoma patients. Indian J Med Res. 2019;150:67–72. https://doi.org/10.4103/IJMR.IJMR_1896_17.
Gelatti ACZ, Drilon A, Santini FC. Optimizing the sequencing of tyrosine kinase inhibitors (TKIs) in epidermal growth factor receptor (EGFR) mutation-positive non-small cell lung cancer (NSCLC). Lung Cancer. 2019;137:113–22. https://doi.org/10.1016/J.LUNGCAN.2019.09.017.
Park K, Kim JS, Kim JH, Kim YC, Kim HG, Cho EK, et al. An open-label expanded access program of afatinib in EGFR tyrosine kinase inhibitor-naïve patients with locally advanced or metastatic non-small cell lung. BMC Cancer. 2021. https://doi.org/10.1186/S12885-021-08445-9.
Reungwetwattana T, Rohatgi N, Mok TS, Prabhash K. Dacomitinib as first-line treatment for EGFR mutation-positive non-small cell lung cancer. Expert Rev Precis Med Drug Dev. 2021;6:161–71. https://doi.org/10.1080/23808993.2021.1909420/FORMAT/EPUB.
Arcila ME, Oxnard GR, Nafa K, Riely GJ, Solomon SB, Zakowski MF, et al. Rebiopsy of lung cancer patients with acquired resistance to EGFR inhibitors and enhanced detection of the T790M mutation using a locked nucleic acid-based assay. Clin Cancer Res. 2011;17:1169–80. https://doi.org/10.1158/1078-0432.CCR-10-2277.
Ramalingam SS, Yang JCH, Lee CK, Kurata T, Kim DW, John T, et al. Osimertinib as first-line treatment of EGFR mutation-positive advanced non-small-cell lung cancer. J Clin Oncol. 2018;36:841–9. https://doi.org/10.1200/JCO.2017.74.7576.
Ohe Y, Imamura F, Nogami N, Okamoto I, Kurata T, Kato T, et al. Osimertinib versus standard-of-care EGFR-TKI as first-line treatment for EGFRm advanced NSCLC: FLAURA Japanese subset. Jpn J Clin Oncol. 2019;49:29–36. https://doi.org/10.1093/jjco/hyy179.
Van Der Steen N, Caparello C, Rolfo C, Pauwels P, Peters GJ, Giovannetti E. New developments in the management of non-small-cell lung cancer, focus on rociletinib: what went wrong? Onco Targets Ther. 2016;9:6065–74. https://doi.org/10.2147/OTT.S97644.
Murtuza A, Bulbul A, Shen JP, Keshavarzian P, Woodward BD, Lopez-Diaz FJ, et al. Novel third-generation EGFR tyrosine kinase inhibitors and strategies to overcome therapeutic resistance in lung cancer. Cancer Res. 2019;79:689–98. https://doi.org/10.1158/0008-5472.CAN-18-1281.
Song HN, Jung KS, Yoo KH, Cho J, Lee JY, Lim SH, et al. Acquired C797S mutation upon treatment with a T790M-specific third-generation EGFR inhibitor (HM61713) in non-small cell lung cancer. J Thorac Oncol. 2016;11:e45–7. https://doi.org/10.1016/J.JTHO.2015.12.093.
Wang S, Tsui ST, Liu C, Song Y, Liu D. EGFR C797S mutation mediates resistance to third-generation inhibitors in T790M-positive non-small cell lung cancer. J Hematol Oncol. 2016. https://doi.org/10.1186/s13045-016-0290-1.
Yu HA, Tian SK, Drilon AE, Borsu L, Riely GJ, Arcila ME, et al. Acquired resistance of EGFR-mutant lung cancer to a T790M-specific EGFR inhibitor: emergence of a third mutation (C797S) in the EGFR tyrosine kinase domain. JAMA Oncol. 2015;1:982–4. https://doi.org/10.1001/JAMAONCOL.2015.1066.
Wang S, Song Y, Liu D. EAI045: the fourth-generation EGFR inhibitor overcoming T790M and C797S resistance. Cancer Lett. 2017;385:51–4. https://doi.org/10.1016/J.CANLET.2016.11.008.
Zhang M, Wang Y, Wang J, Liu Z, Shi J, Li M, et al. Design, synthesis and biological evaluation of the Quinazoline derivatives as L858R/T790M/C797S triple mutant epidermal growth factor receptor tyrosine kinase inhibitors. Chem Pharm Bull. 2020;68:971–80. https://doi.org/10.1248/CPB.C20-00411.
Juchum M, Günther M, Döring E, Sievers-Engler A, Lämmerhofer M, Laufer S. Trisubstituted imidazoles with a rigidized hinge binding motif act as single digit nM inhibitors of clinically relevant EGFR L858R/T790M and L858R/T790M/C797S mutants: an example of target hopping. J Med Chem. 2017;60:4636–56. https://doi.org/10.1021/acs.jmedchem.7b00178.
Engelman JA, Zejnullahu K, Mitsudomi T, Song Y, Hyland C, Joon OP, et al. MET amplification leads to gefitinib resistance in lung cancer by activating ERBB3 signaling. Science. 2007;316:1039–43. https://doi.org/10.1126/SCIENCE.1141478/SUPPL_FILE/ENGELMAN_SOM_REVISED.PDF.
Ji W, Choi CM, Rho JK, Jang SJ, Park YS, Chun SM, et al. Mechanisms of acquired resistance to EGFR-tyrosine kinase inhibitor in Korean patients with lung cancer. BMC Cancer. 2013;13:1–8. https://doi.org/10.1186/1471-2407-13-606/FIGURES/5.
Folkman J. Tumor angiogenesis: therapeutic implications. N Engl J Med. 1971. https://doi.org/10.1056/nejm197111182852108.
Krock BL, Skuli N, Simon MC. Hypoxia-induced angiogenesis: good and evil. Genes Cancer. 2011;2:1117. https://doi.org/10.1177/1947601911423654.
Maniscalco WM, D’Angio CT. Vascular endothelial growth factor. Encycl Respir Med Four-Volume Set. 2006. https://doi.org/10.1016/B0-12-370879-6/00434-8.
Johnson DH, Fehrenbacher L, Novotny WF, Herbst RS, Nemunaitis JJ, Jablons DM, et al. Randomized phase II trial comparing bevacizumab plus carboplatin and paclitaxel with carboplatin and paclitaxel alone in previously untreated locally advanced or metastatic non-small-cell lung cancer. J Clin Oncol. 2004;22:2184–91. https://doi.org/10.1200/JCO.2004.11.022.
Takeda K, Daga H. Ramucirumab for the treatment of advanced or metastatic non-small cell lung cancer. Expert Opin Biol Ther. 2016;16:1541–7. https://doi.org/10.1080/14712598.2016.1248397.
Garon EB, Ciuleanu TE, Arrieta O, Prabhash K, Syrigos KN, Goksel T, et al. Ramucirumab plus docetaxel versus placebo plus docetaxel for second-line treatment of stage IV non-small-cell lung cancer after disease progression on platinum-based therapy (REVEL): a multicentre, double-blind, randomised phase 3 trial. Lancet. 2014;384:665–73. https://doi.org/10.1016/S0140-6736(14)60845-X.
Boumber Y. Recent advances in targetable therapeutics in metastatic non-squamous nSCLC. Front Oncol. 2016;6:1–9. https://doi.org/10.3389/fonc.2016.00112.
Tanimura K, Yamada T, Omura A, Shiotsu S, Kataoka N, Takeda T, et al. The impact of VEGF inhibition on clinical outcomes in patients with advanced non-small cell lung cancer treated with immunotherapy: a retrospective cohort study. Front Oncol. 2021;11:1–8. https://doi.org/10.3389/fonc.2021.663612.
El yacoubi H, Sow ML, Kettani F, Gamra L, Mestari A, Jabri L, et al. Frequency of anaplastic lymphoma kinase rearrangements in Moroccan patients with non small cell lung cancer: a multi-institutional national retrospective study. BMC Cancer. 2020;20:1–5. https://doi.org/10.1186/S12885-020-06973-4.
Hallberg B, Palmer RH. The role of the ALK receptor in cancer biology. Ann Oncol. 2016;27:iii4–15. https://doi.org/10.1093/annonc/mdw301.
Carcereny E, Fernández-Nistal A, López A, Montoto C, Naves A, Segú-Vergés C, et al. Head to head evaluation of second generation ALK inhibitors brigatinib and alectinib as first-line treatment for ALK+ NSCLC using an in silico systems biology-based approach. Oncotarget. 2021;12:316–32. https://doi.org/10.18632/ONCOTARGET.27875.
Du X, Shao Y, Qin HF, Tai YH, Gao HJ. ALK-rearrangement in non-small-cell lung cancer (NSCLC). Thorac Cancer. 2018;9:423–30. https://doi.org/10.1111/1759-7714.12613.
Solomon BJ, Mok T, Kim D-W, Wu Y-L, Nakagawa K, Mekhail T, et al. First-line crizotinib versus chemotherapy in ALK-positive lung cancer. N Engl J Med. 2014;371:2167–77. https://doi.org/10.1056/nejmoa1408440.
Shaw AT, Kim TM, Crinò L, Gridelli C, Kiura K, Liu G, et al. Ceritinib versus chemotherapy in patients with ALK-rearranged non-small-cell lung cancer previously given chemotherapy and crizotinib (ASCEND-5): a randomised, controlled, open-label, phase 3 trial. Lancet Oncol. 2017;18:874–86. https://doi.org/10.1016/S1470-2045(17)30339-X.
Camidge DR, Kim HR, Ahn M-J, Yang JC-H, Han J-Y, Lee J-S, et al. Brigatinib versus crizotinib in ALK-positive non-small-cell lung cancer. N Engl J Med. 2018;379:2027–39. https://doi.org/10.1056/nejmoa1810171.
Sreelakshmi M, George JG, Mishra R, Aneesh TP. Targeting apoptosis by inhibiting cMET amplification due to EGFR resistance using benzofuran derivatives. Res J Chem Environ. 2019;23:11–8.
Zhang Y, Xia M, Jin K, Wang S, Wei H, Fan C, et al. Function of the c-Met receptor tyrosine kinase in carcinogenesis and associated therapeutic opportunities. Mol Cancer. 2018;17:1–14. https://doi.org/10.1186/S12943-018-0796-Y.
Wang Q, Yang S, Wang K, Sun SY. MET inhibitors for targeted therapy of EGFR TKI-resistant lung cancer. J Hematol Oncol. 2019;12:1–11. https://doi.org/10.1186/s13045-019-0759-9.
Heist RS, Shim HS, Gingipally S, Mino-Kenudson M, Le L, Gainor JF, et al. MET Exon 14 skipping in non-small cell lung cancer. Oncologist. 2016;21:481–6. https://doi.org/10.1634/THEONCOLOGIST.2015-0510.
Vansteenkiste JF, Van De Kerkhove C, Wauters E, Van Mol P. Capmatinib for the treatment of non-small cell lung cancer. Expert Rev Anticancer Therapy. 2019;19:659–71. https://doi.org/10.1080/14737140.2019.1643239.
Wolf J, Seto T, Han J-Y, Reguart N, Garon EB, Groen HJM, et al. Capmatinib in MET Exon 14-mutated or MET-amplified non–small-cell lung cancer. N Engl J Med. 2020;383:944–57. https://doi.org/10.1056/nejmoa2002787.
Paik PK, Felip E, Veillon R, Sakai H, Cortot AB, Garassino MC, et al. Tepotinib in non-small-cell lung cancer with MET Exon 14 skipping mutations. N Engl J Med. 2020;383:931–43. https://doi.org/10.1056/nejmoa2004407.
Zhang H, Bao Z, Liao H, Li W, Chen Z, Shen H, et al. The efficacy and safety of tivantinib in the treatment of solid tumors: a systematic review and meta-analysis. Oncotarget. 2017;8:113153–62.
Medlineplus. KRAS Gene. Definitions 2020:1–6. https://doi.org/10.32388/id1hoh.
Kessler D, Gerlach D, Kraut N, McConnell DB. Targeting son of sevenless 1: THE pacemaker of KRAS. Curr Opin Chem Biol. 2021;62:109–18. https://doi.org/10.1016/j.cbpa.2021.02.014.
Kempf E, Rousseau B, Besse B, Paz-Ares L. KRAS oncogene in lung cancer: focus on molecularly driven clinical trials. Eur Respir Rev. 2016;25:71–6. https://doi.org/10.1183/16000617.0071-2015.
Blair HA. Sotorasib: first approval. Drugs. 2021;81:1573–9. https://doi.org/10.1007/S40265-021-01574-2.
Erlanson DA, Webster KR. Targeting mutant KRAS. Curr Opin Chem Biol. 2021;62:101–8. https://doi.org/10.1016/j.cbpa.2021.02.010.
Yang A, Li M, Fang M. The research progress of direct KRAS G12C mutation inhibitors. Pathol Oncol Res. 2021;27:1–8. https://doi.org/10.3389/pore.2021.631095.
Han J, Liu Y, Yang S, Wu X, Li H, Wang Q. MEK inhibitors for the treatment of non-small cell lung cancer. J Hematol Oncol. 2021;14:1–12. https://doi.org/10.1186/s13045-020-01025-7.
Bustamante Alvarez JG, Otterson GA. Agents to treat BRAF-mutant lung cancer. Drugs Context. 2019;8:31–5. https://doi.org/10.7573/dic.212566.
Kawamura T, Murakami H. Dabrafenib in patients with BRAF-mutated non-small cell lung cancer. Transl Cancer Res. 2016. https://doi.org/10.21037/8755.
Mazieres J, Cropet C, Montané L, Barlesi F, Souquet PJ, Quantin X, et al. Vemurafenib in non-small-cell lung cancer patients with BRAF V600 and BRAF nonV600 mutations. Ann Oncol Off J Eur Soc Med Oncol. 2020;31:289–94. https://doi.org/10.1016/J.ANNONC.2019.10.022.
Subbiah V, Gervais R, Riely G, Hollebecque A, Blay JY, Felip E, et al. Efficacy of vemurafenib in patients with non-small-cell lung cancer with BRAF V600 mutation: an open-label, single-arm cohort of the histology-independent VE-BASKET study. JCO Precis Oncol. 2019;3:1–9. https://doi.org/10.1200/PO.18.00266.
Planchard D, Smit EF, Groen HJM, Mazieres J, Besse B, Helland Å, et al. Dabrafenib plus trametinib in patients with previously untreated BRAFV600E-mutant metastatic non-small-cell lung cancer: an open-label, phase 2 trial. Lancet Oncol. 2017;18:1307–16. https://doi.org/10.1016/S1470-2045(17)30679-4.
Drilon A, Jenkins C, Iyer S, Schoenfeld A, Keddy C, Davare MA. ROS1-dependent cancers—biology, diagnostics and therapeutics. Nat Rev Clin Oncol. 2021;18:35–55. https://doi.org/10.1038/s41571-020-0408-9.
Sehgal K, Patell R, Rangachari D, Costa DB. Targeting ROS1 rearrangements in non-small cell lung cancer with crizotinib and other kinase inhibitors. Transl Cancer Res. 2018;7:S779. https://doi.org/10.21037/TCR.2018.08.11.
Rossi G, Jocollé G, Conti A, Tiseo M, Marino FZ, Donati G, et al. Detection of ROS1 rearrangement in non-small cell lung cancer: current and future perspectives. Lung Cancer Targets Ther. 2017;8:45–55. https://doi.org/10.2147/LCTT.S120172.
Ng K, Main K, Forster M. Molecular targetable pathways and therapy—ROS1, vol. 2007. 2nd ed. Amsterdam: Elsevier Inc.; 2022.
Joshua JM, Salima KD, Pavithran K, Vijayan M. Crizotinib, an effective agent in ROS1-rearranged adenocarcinoma of lungs: a case report. Clin Med Insights Case Rep. 2018;11:1–3. https://doi.org/10.1177/1179547617749615.
Roys A, Chang X, Liu Y, Xu X, Wu Y, Zuo D. Resistance mechanisms and potent-targeted therapies of ROS1-positive lung cancer. Cancer Chemother Pharmacol. 2019;84:679–88. https://doi.org/10.1007/S00280-019-03902-6.
Wang Y, Chen Z, Han X, Li J, Guo H, Shi J. Acquired MET D1228N mutations mediate crizotinib resistance in lung adenocarcinoma with ROS1 fusion: a case report. Oncologist. 2021;26:178–81. https://doi.org/10.1002/onco.13545.
Patil T, Smith DE, Bunn PA, Aisner DL, Le AT, Hancock M, et al. The incidence of brain metastases in stage IV ROS1-rearranged non-small cell lung cancer and rate of central nervous system progression on crizotinib. J Thorac Oncol. 2018;13:1717–26. https://doi.org/10.1016/J.JTHO.2018.07.001.
Drilon A, Siena S, Dziadziuszko R, Barlesi F, Krebs MG, Shaw AT, et al. Entrectinib in ROSI fusion-positive non-small-cell lung cancer: integrated analysis of three phase 1–2 trials. Lancet Oncol. 2020;21:261–70. https://doi.org/10.1016/S1470-2045(19)30690-4.
Jiang T, Wang G, Liu Y, Feng L, Wang M, Liu J, et al. Development of small-molecule tropomyosin receptor kinase (TRK) inhibitors for NTRK fusion cancers. Acta Pharm Sin B. 2021;11:355–72. https://doi.org/10.1016/j.apsb.2020.05.004.
Drilon A. TRK inhibitors in TRK fusion-positive cancers. Ann Oncol. 2019;30:VIII23–30. https://doi.org/10.1093/annonc/mdz282.
Bebb DG, Banerji S, Blais N, Desmeules P, Gill S, Grin A, et al. Canadian consensus for biomarker testing and treatment of TRK fusion cancer in adults. Curr Oncol. 2021;28:523–48. https://doi.org/10.3390/CURRONCOL28010053.
Haratake N, Seto T. NTRK fusion-positive non-small-cell lung cancer: the diagnosis and targeted therapy. Clin Lung Cancer. 2021;22:1–5. https://doi.org/10.1016/J.CLLC.2020.10.013.
Lin JJ, Kummar S, Tan DS-W, Lassen UN, Leyvraz S, Liu Y, et al. Long-term efficacy and safety of larotrectinib in patients with TRK fusion-positive lung cancer. 2021;39:9109–09. https://doi.org/10.1200/JCO.2021.39.15_SUPPL.9109.
Liu Z, Yu P, Dong L, Wang W, Duan S, Wang B, et al. Discovery of the next-generation pan-TRK kinase inhibitors for the treatment of cancer. J Med Chem. 2021;64:10286–96. https://doi.org/10.1021/acs.jmedchem.1c00712.
RET Therapy for NSCLC, a New Generation of Inhibitors | IASLC n.d. https://www.iaslc.org/iaslc-news/ilcn/ret-therapy-nsclc-new-generation-inhibitors. Accessed 7 Oct 2021.
Jhiang SM. The RET proto-oncogene in human cancers. Oncogene. 2000;19:5590–7. https://doi.org/10.1038/sj.onc.1203857.
Tsuta K, Kohno T, Yoshida A, Shimada Y, Asamura H, Furuta K, et al. RET-rearranged non-small-cell lung carcinoma: a clinicopathological and molecular analysis. Br J Cancer. 2014;110:1571–8. https://doi.org/10.1038/bjc.2014.36.
Benayed R, Offin M, Mullaney K, Sukhadia P, Rios K, Desmeules P, et al. High yield of RNA sequencing for targetable kinase fusions in lung adenocarcinomas with no mitogenic driver alteration detected by DNA sequencing and low tumor mutation burden. Clin Cancer Res. 2019;25:4712–22. https://doi.org/10.1158/1078-0432.CCR-19-0225.
Jakob C, Stock G, Tay R, Dawod M, Gomes F, Califano R. Targeted therapy for RET-rearranged non-small cell lung cancer: clinical development and future directions. OncoTargets Therapy. 2019;12:7857–64.
Drilon A, Oxnard GR, Tan DSW, Loong HHF, Johnson M, Gainor J, et al. Efficacy of selpercatinib in RET fusion-positive non-small-cell lung cancer. New Engl J Med. 2020;383:813–24. https://doi.org/10.1056/NEJMOA2005653.
Gainor JF, Curigliano G, Kim DW, Lee DH, Besse B, Baik CS, et al. Pralsetinib for RET fusion-positive non-small-cell lung cancer (ARROW): a multi-cohort, open-label, phase 1/2 study. Lancet Oncol. 2021;22:959–69. https://doi.org/10.1016/S1470-2045(21)00247-3.
Dai S, Zhou Z, Chen Z, Xu G, Chen Y. Structures and small molecule inhibitors. Cell. 2019;2019:1–15.
Desai A, Adjei AA. FGFR signaling as a target for lung cancer therapy. J Thorac Oncol. 2016;11:9–20. https://doi.org/10.1016/j.jtho.2015.08.003.
Touat M, Ileana E, Postel-Vinay S, André F, Soria JC. Targeting FGFR signaling in cancer. Clin Cancer Res. 2015;21:2684–94. https://doi.org/10.1158/1078-0432.CCR-14-2329.
Hibi M, Kaneda H, Tanizaki J, Sakai K, Togashi Y, Terashima M, et al. FGFR gene alterations in lung squamous cell carcinoma are potential targets for the multikinase inhibitor nintedanib. Cancer Sci. 2016;107:1667–76. https://doi.org/10.1111/cas.13071.
Rijavec E, Genova C, Barletta G, Biello F, Rossi G, Tagliamento M, et al. Investigational drugs targeting fibroblast growth factor receptor in the treatment of non-small cell lung cancer. Expert Opin Investig Drugs. 2017;26:551–61. https://doi.org/10.1080/13543784.2017.1316714.
Bronte G, Passiglia F, Galvano A, Barraco N, Listì A, Castiglia M, et al. Nintedanib in NSCLC: evidence to date and place in therapy. Ther Adv Med Oncol. 2016;8:188–97. https://doi.org/10.1177/1758834016630976.
Zeng J, Ma W, Young RB, Li T. Targeting HER2 genomic alterations in non-small cell lung cancer. J Natl Cancer Cent. 2021;1:58–73. https://doi.org/10.1016/j.jncc.2021.04.001.
Li BT, Ross DS, Aisner DL, Chaft JE, Hsu M, Kako SL, et al. HER2 amplification and her2 mutation are distinct molecular targets in lung cancers. J Thorac Oncol. 2016;11:414–9. https://doi.org/10.1016/j.jtho.2015.10.025.
Dziadziuszko R, Smit EF, Dafni U, Wolf J, Wasąg B, Biernat W, et al. Afatinib in NSCLC with HER2 mutations: results of the prospective, open-label phase II NICHE trial of European Thoracic Oncology Platform (ETOP). J Thorac Oncol. 2019;14:1086–94. https://doi.org/10.1016/j.jtho.2019.02.017.
Ross HJ, Blumenschein GR, Aisner J, Damjanov N, Dowlati A, Garst J, et al. Randomized phase II multicenter trial of two schedules of lapatinib as first- or second-line monotherapy in patients with advanced or metastatic non-small cell lung cancer. Clin Cancer Res. 2010;16:1938–49. https://doi.org/10.1158/1078-0432.CCR-08-3328.
Ni J, Zhang L. Progress in treatment of non-small cell lung cancer harboring her2 aberrations. Onco Targets Ther. 2021;14:4087–98. https://doi.org/10.2147/OTT.S312820.
Acknowledgements
We are thankful to Dr. Sabitha M, Principal, Amrita School of Pharmacy, Amrita Vishwa Vidyapeetham, AIMS Health Sciences Campus, Kochi-682041, Kerala, India, for assisting with this work. We also are grateful to Sarath S Kumar for creating the illustrations for this work.
Funding
The authors declare that no funds, grants, or other support were received during the preparation of this manuscript.
Author information
Authors and Affiliations
Contributions
All authors have equally contributed to and approved the final manuscript.
Corresponding authors
Ethics declarations
Conflicts of interest
Ajay P Jayan, Anandu K R, Krishnadas Madhu, and Saiprabha V N have no conflict of interest.
Research involving human and animal rights
This article does not contain any studies with human participants or animals performed by any of the authors.
Consent for publication
All authors gave final approval of the version to be published.
Additional information
Publisher's Note
Springer Nature remains neutral with regard to jurisdictional claims in published maps and institutional affiliations.
Rights and permissions
About this article
Cite this article
Jayan, A.P., Anandu, K.R., Madhu, K. et al. A pharmacological exploration of targeted drug therapy in non-small cell lung cancer. Med Oncol 39, 147 (2022). https://doi.org/10.1007/s12032-022-01744-6
Received:
Accepted:
Published:
DOI: https://doi.org/10.1007/s12032-022-01744-6