Abstract
A significant number of patients with intermediate- or high-risk bladder cancer treated with intravesical Bacillus Calmette–Guérin (BCG) immunotherapy are non-responders to this treatment. Since we cannot predict in which patients BCG therapy will fail, markers for responders are needed. UroVysion® is a multitarget fluorescence in situ hybridization (FISH) test for bladder cancer detection. The aim of this study was to evaluate whether FISH can be used to early identify recurrence during treatment with BCG. In a multicenter, prospective study, three bladder washouts at different time points during treatment (t 0 = week 0, pre-BCG, t 1 = 6 weeks following TURB, t 2 = 3 months following TURB) were collected for FISH from patients with bladder cancer treated with BCG between 2008 and 2013. Data on bladder cancer recurrence and duration of BCG maintenance therapy were recorded. Thirty-six (31.6%) out of 114 patients developed a recurrence after a median of 6 months (range 2–32). No significant association was found between a positive FISH test at t 0 or t 1 and risk of recurrence (p = 0.79 and p = 0.29). A positive t 2 FISH test was associated with a higher risk of recurrence (p = 0.001). Patients with a positive FISH test 3 months following TURB had a 4.0–4.6 times greater risk of developing a recurrence compared to patients with a negative FISH. Patients with a positive FISH test 3 months following TURB and induction BCG therapy have a higher risk of developing tumor recurrence. FISH can therefore be a useful additional tool for physicians when determining a treatment strategy.
Similar content being viewed by others
Avoid common mistakes on your manuscript.
Introduction
Non-muscle-invasive bladder cancer (NMIBC) is a heterogeneous histopathological condition with different prognoses. Based on risk factors, patients are classified into risk groups with low, intermediate and high risk of recurrence and progression [1]. For intermediate- or high-risk NMIBC, adjuvant intravesical therapy with Bacillus Calmette–Guérin (BCG) is recommended in the guidelines of the European Association of Urology and the American Urological Association [1, 2].
In spite of its effectiveness, intravesical BCG therapy is not devoid of limitations [3]. BCG treatment may induce local side effects in 62.8% and systemic side effects in 30.6% of patients with possible fatal outcome [4]. This may lead to interruption or discontinuation of BCG treatment in up to 20% of patients [5]. Besides, in up to 40% of patients BCG treatment fails [6,7,8]. BCG failure can be divided into different types: BCG intolerant, refractory and relapsing. BCG intolerant patients have to stop due to side effects, whereas BCG refractory patients do not respond to BCG induction therapy and have persistent disease, while BCG relapsing patients initially do respond to BCG treatment, but after a disease-free period develops a recurrence [9, 10]. Since BCG is mainly given to treat patients with a high risk of progression to muscle-invasive disease, it is important to identify non-responding patients early. However, currently no diagnostic tool is available to discriminate between BCG responders and BCG non-responders. A predictive test is desirable and might be helpful in treatment decision.
UroVysion® (Abbott Molecular, Illinois, USA) FISH is able to detect genetic alterations most commonly associated with bladder cancer. The assay detects aneuploidy of chromosomes 3, 7 and 17 and a deletion of locus 9p21 [11]. Since FISH is based on detection of genetic alterations, results or interpretation of the test will not be influenced by the inflammatory response of the bladder to BCG, as opposed to cystoscopy and urine cytology [12].
If we can predict which patients are at risk of developing a recurrence during BCG treatment, it is possible to prevent under-treatment by timely changing from BCG therapy to other intravesical therapy or to radical therapy, i.e., radical cystectomy. Furthermore, early identification of BCG non-responders will limit the associated risks of BCG therapy. The aim of this study is to determine the usefulness of FISH as predictor of tumor recurrence in patients with NMIBC treated with BCG instillations.
Materials and methods
Patient inclusion
From 2008 to 2013, five centers included patients with NMIBC treated with BCG instillations in a prospective study evaluating the accuracy of FISH in bladder washout. Informed consent was verbally obtained of all participants prior to inclusion. Patients had histologically confirmed primary or recurrent intermediate- or high-risk NMIBC (CIS, Ta, T1, all grades) and were scheduled for BCG induction therapy after complete transurethral resection of the bladder tumor(s) (TURB). Administration of a single immediate postoperative chemotherapy instillation or re-resection was left to the discretion of the treating urologist. Exclusion criteria included presence of muscle-invasive disease, no histologic confirmation of bladder tumor and synchronous upper urinary tract urothelial carcinoma.
BCG instillation protocol
All patients were scheduled to receive at least induction BCG therapy of six weekly instillations following TURB. Maintenance therapy was administered depending on hospitals’ protocols. In general, maintenance therapy consisted of three weekly instillations during 1 to 3 years (at 3, 6, 12, 18, 24, 30, 36 months). Patients were followed by cystoscopy every 3 months during the first two years after inclusion or until a recurrence was diagnosed. Data on bladder cancer recurrence and duration of BCG maintenance therapy were recorded. A recurrence was defined as histopathologically proven NMIBC or muscle-invasive disease (T ≥ 2). Tumor grade was assessed based on the 1973 WHO classification. Progression was defined as the histologic confirmation of muscle-invasive disease (T ≥ 2).
Bladder washout protocol
Bladder washouts (BWOs) for FISH evaluation were collected at three time points: before the first BCG instillation (t 0), before the last induction BCG instillation at 6 weeks (t 1) and at 3 months during first cystoscopy follow-up (t 2). BWOs at t 0 and t 1 were done via a catheter, and 50 cc 0.9% saline was used to flush the bladder. At t 2, the BWO was done at the end of the cystoscopy via the working channel of the cystoscope. Each BWO was preserved in carbowax (polyethylene glycol). Cytospins were made within 72 h and stored in a −20 °C freezer until FISH test was performed.
FISH protocol
All BWOs were analyzed using the multitarget UroVysion® bladder cancer kit. The FISH kit is composed of a mixture of four-target multicolor probes, three chromosome enumeration probes (CEP 3, CEP 7 and CEP 17) and one single locus-specific indicator probe (LSI 9p21). Cytospins were made of collected BWOs and fixed using Carnoy’s solution (3:1 methanol/glacial acetic acid). Slides were pre-treated using the Vysis pre-treatment kit (Abbott Molecular, Illinois, USA), and FISH was performed according to the manufacturer’s instructions provided with the assay. In short, slides were denatured in 2 × SSC at 73 ± 1 °C for 2 min and incubated in pepsin buffer at 37 °C for 10 min. After 5-min washing at room temperature with phosphate-buffered saline (PBS), the slides were fixed in 1% formaldehyde during 5 min. The slides were washed again in PBS at room temperature for 5 min and dehydrated in consecutively 70, 85 and 100% ethanol, for 1 min each. For hybridization the multitarget UroVysion® probe mixture was added and incubated overnight at 73 °C (denaturation 2 min) and 37 °C (hybridization 8–16 h) using the ThermoBrite System. Post-hybridization the slides were washed in 0.4 SSC at room temperature for 5 min, 0.4 SSC at 73 °C for maximum 2 min and 2 × SSC at room temperature for 1 min. Nuclei were counterstained with DAPI (4′,6-diamidino-2-phenylindole). FISH assays were examined using a fluorescence microscope (Leica DM 5000B and Leica DM 5500) with the following filters: A4 (DAPI), TX2 (CEP 3, red), L5 (CEP 7, green), SAQ (CEP 17, aqua) and SGO (LSI 9p21, gold).
Data analysis
Slides were screened for 25 morphologically abnormal cells (large nuclear size, irregular nuclear shape, patchy DAPI staining or cell clusters) and considered positive if one of the following criteria were met: ≥4 cells have a gain of 2 or more chromosomes (3, 7 or 17), or ≥12 cells have a loss of both copies of LSI 9p21 [13]. During the course of the trial, three designated researchers evaluated all slides. The researchers were instructed and trained by one of the manufacturer’s cytogenetic consultants.
Statistics
Data were analyzed using SPSS Statistics version 23. Descriptive statistics were used for patient characteristics. Patient and tumor characteristics of patients with a FISH result available at t 1 and t 2 were compared with the whole cohort with a FISH result available at t 0, to evaluate whether missing cases at t 1 and t 2 influenced the results. P values were calculated by using one-sample test proportion. Kaplan–Meier method was used to estimate recurrence-free survival and progression-free survival based on positive or negative FISH test at the three time points (t 0, t 1 and t 2). The log-rank test was used for statistical significance. Hazard ratios were calculated using Cox proportional regression analysis. Sensitivity, specificity, positive predictive value (PPV), negative predictive value (NPV) and accuracy of the test at each time point during evaluation were calculated using 2 × 2 tables.
Results
Patient characteristics and outcomes
In total 147 patients were enrolled during the study period with 114 patients finally being eligible for data evaluation. Patient and tumor characteristics are summarized in Tables 1 and 2. Sixty-six patients received BCG maintenance (4–25 months). Median follow-up for the whole cohort was 23 months (range 2–32). During follow-up 36 patients (31.6%) developed a recurrence (Table 3) at a median time of 6 months (range 3–28). Disease progression to muscle-invasive bladder cancer occurred in 4 of the 36 patients after a median time of 13 months (range 7–23). High-grade tumor recurrence occurred in 25 patients (Table 3). During follow-up, one patient developed a ureter tumor and 15 patients died: 3 patients as a result of metastatic bladder cancer, 6 patients due to non-urologic reasons and 6 patients with an unknown cause. Six patients were lost to follow-up, with no available data.
FISH results
Patients were considered suitable for analysis if at least two evaluable BWOs were available for FISH, with one sample being collected at t 0 and a second sample at either t 1 or t 2 (Fig. 1). Of 58 patients (50.9%) FISH results at all 3 time points were available, and of 56 patients (49.1%) 2 FISH samples were available (n = 48 for t 0 and t 1, n = 8 for t 0 and t 2). FISH test was available at t 0 in 114 patients and was positive in 48 patients (42.1%). At t 1 FISH test was available in 106 patients. Thirty-six patients converted from pre-BCG-positive FISH to post-BCG-negative FISH at t 1. In total 16 patients (15.1%) had a positive FISH result at t 1. At first cystoscopic surveillance or t 2, 66 FISH results were available, of which 18 were positive (27.3%). Of these patients, 10 patients (15.2%) initially had a negative pre-BCG FISH result that converted to a positive FISH result at t 2.
Survival analysis
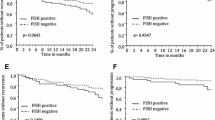
Kaplan–Meier curves for recurrence of the whole cohort and for the three time points in which FISH was performed are shown in Fig. 2. No association between a positive FISH result and tumor recurrence was found at t 0 (p = 0.79), and a nonsignificant correlation was observed at t 1 (p = 0.29). At t 2 a positive FISH test was significantly associated with a higher risk of recurrence (p = 0.001). Cox regression showed that patients with a positive FISH test at t 2 had a 4.6 times greater risk of tumor recurrence compared to patients with a negative FISH test at 3 months following TURB (95% CI: 1.71–11.84). When corrected for an immediate postoperative chemotherapy instillation, repeat TURB and number of maintenance BCG instillations, a positive FISH test at t 2 had a 4.0 greater risk (95% CI: 1.45–11.10) of tumor recurrence compared to patients with a negative FISH test.
Recurrence-free survival curves of t 0, t 1 and t 2 and hazard curve of t 2, corrected for possible confounding. a Kaplan–Meier curve of patients with a positive FISH test versus negative FISH test pre-BCG (t 0). b Kaplan–Meier curve of patients with a positive FISH test versus a negative FISH test post-BCG induction at 6 weeks (t 1). c Kaplan–Meier curve of patients with a positive FISH test versus negative FISH test post-BCG at 3 months (t 2). d Hazard curve of t 2, corrected for immediate postoperative instillation, repeat TURB and number of BCG maintenance instillations
Due to the small number of progression events during the study period, a separate Kaplan–Meier analysis for this outcome was not possible.
Diagnostic test evaluation
Sensitivity of FISH at t 0, t 1 and t 2 was 44, 21 and 59%, and specificity was 59, 88 and 84%, respectively. For the three different points in time, PPV was 33, 44 and 56% and NPV was 70, 71 and 85%, respectively. Accuracy of the FISH test at t 0, t 1 and t 2 was 54, 67 and 77%, respectively (Table 4).
Discussion
The results from this study confirm earlier data from smaller or single-center studies, establishing the potential of FISH as a part of a predictive diagnostic workup. This study demonstrates that the UroVysion® FISH test 3 months following TURB and BCG induction can be of value when considering disease management for patients with intermediate- or high-risk NMIBC. Patients with a positive FISH test at t2 had a 4.0–4.6 times greater risk to develop a recurrence than patients with a negative FISH test. At t 2, sensitivity, specificity and accuracy of FISH were 59, 84 and 77%, respectively. On the contrary, despite a trend at t 1, the results of the FISH test at t 0 and t 1 were not significantly associated with the risk of tumor recurrence. Risk assessment for tumor progression using FISH could not be determined due to the small number of progression events.
The literature regarding the efficacy of UroVysion® for predicting recurrence risk following adjuvant instillations is scarce. Kipp et al. and Whitson et al. published results of patients who received bladder instillations using intravesical therapy including BCG, MMC and Thiotepa [14, 15]. Both groups reported that a positive FISH test following intravesical therapy was associated with a higher risk of recurrence. Additionally, a positive FISH test prior to intravesical treatment was associated with a higher risk of recurrence, and a positive FISH test following intravesical treatment was associated with a higher risk of progression to muscle-invasive disease [14]. Three other studies focused on risk assessment for tumor recurrence using FISH in patients treated with BCG instillations only [16,17,18]. These groups also reported that a positive FISH test following BCG therapy was associated with a higher risk of recurrence. Our results at t0 and t1 are in line with results reported by Mengual et al. and Savic et al. [16, 17]. However, Kamat et al. found a positive association for t 0. This discordance could be explained by the difference in patient cohorts. In the cohort evaluated by Kamat et al., 89% of the patients had a previously treated bladder tumor and 48% had CIS as secondary finding, whereas in our cohort this was 30 and 18%, respectively [18].
Although not significant, the association between a positive FISH test at t1 and the risk of recurrence indicates a positive trend. We hypothesize that patients with a false positive FISH at t1 did not fully benefit from the BCG induction therapy yet, since BCG-induced delayed immune reaction may differ in each patient [19, 20].
At first cystoscopic surveillance following TURB, 18 patients had a positive FISH test. However, some had a false positive FISH test. A follow-up of 2 years might be too short to detect progression and leads to underestimation of recurrent and progressive disease. Conversely, a negative FISH test 3 months following initial TURB does not exclude patients to develop a recurrence. In our study 7 patients had a false negative FISH test at t 2 (15% of all patients with a negative FISH result at t 2) and did develop a recurrence bladder tumor during follow-up at a median of 7 months (range 2–24). Of these, 2 patients progressed to muscle-invasive disease (supplemental table S1). Although UroVysion® is designed to detect genetic changes associated with most bladder cancers, some bladder tumors have different genetic changes that will not be detected using this test [21,22,23,24,25].
A limitation of this study is the number of BWO samples not available or suitable for analysis. This reduces the power of the study. Secondly, the number of patients with an available FISH result at t 2 is limited. When comparing patients with available FISH results at t 2 and at t 0, patient and tumor characteristics were similar, except for tumor focality. This could imply that tumors of patients that had a FISH result available at t 2 were slightly more aggressive (supplemental tables S2 and S3). Furthermore, in this study BWOs were used for logistic reasons. Though UroVysion® is intended to be performed in voided urine samples, it has been demonstrated that the test is valid when performed in BWO samples [13]. Also, BWOs were processed over the course of 7 years. It cannot be ruled out that during this period some samples were improperly handled or stored. However, six and a half years after collecting the urine samples still good fluorescent signals were obtained. Lastly, the duration of BCG maintenance therapy is still a subject of debate. Patients received a 6-week induction course of BCG, and in the majority of cases this was followed by BCG maintenance therapy depending on hospital protocol. This may have influenced the chance of developing a recurrence [26]. We could not assess the effect of the different maintenance protocols.
Based on our results, a positive UroVysion® FISH result alone is not sufficient to decide to switch from BCG to radical cystectomy at an early stage (3 months following TURB). There is a substantial risk of overtreatment if all patients with a positive FISH test at t 2 would undergo more aggressive treatment. A positive FISH test following BCG treatment (t 2) is, however, associated with a higher risk of developing a recurrence. A recent update of the guideline of the American Urological Association recommends the use of UroVysion® to assess response to intravesical BCG therapy (level of recommendation: expert opinion) [2]. We recommend for future clinical trials to incorporate FISH at later time points after induction therapy (≥3 months following initial TURB).
Conclusion
This study demonstrates that a positive UroVysion® test at 3 months following TURB and induction BCG therapy for intermediate- and high-risk urothelial carcinoma of the bladder is associated with a statistical significant higher risk of recurrence. Therefore, it can be a useful tool for urologists to assess which patients have a higher risk of developing a recurrence.
References
Babjuk M, Böhle A, Burger M, Capoun O, Cohen D, Compérat EM, et al. EAU guidelines on non-muscle-invasive urothelial carcinoma of the bladder: update 2016. Eur Urol. 2017;71(3):447–461. doi:10.1016/j.eururo.2016.05.041.
Chang SS, Boorjian SA, Chou R, Clark PE, Daneshmand S, Konety BR, et al. Diagnosis and treatment of non-muscle invasive bladder cancer: AUA/SUO guideline. J Urol (Elsevier Ltd). 2016;196:1021–9.
Morales A, Eidinger D, Bruce A. Intracavitary Bacillus Calmette–Guerin in the treatment of superficial bladder tumors. J Urol. 1976;116:180–3.
Brausi M, Oddens J, Sylvester R, Bono A, Van De Beek C, Van Andel G, et al. Side effects of Bacillus Calmette–Guérin (BCG) in the treatment of intermediate- and high-risk Ta, T1 papillary carcinoma of the bladder: results of the EORTC genito-urinary cancers group randomised phase 3 study comparing one-third dose with full dose and 1 year with 3 years of maintenance BCG. Eur Urol. 2014;65:69–76.
Van der Meijden APM, Sylvester RJ, Oosterlinck W, Hoeltl W, Bono AV. Maintenance Bacillus Calmette–Guerin for Ta T1 bladder tumors is not associated with increased toxicity: results from a European organisation for research and treatment of cancer genito-urinary group phase III trial. Eur Urol. 2003;44:429–34.
Pansadoro V, Emiliozzi P, de Paula F, Scarpone P, Pansadoro A, Sternberg CN. Long-term follow-up of G3T1 transitional cell carcinoma of the bladder treated with intravesical bacille Calmette–Guérin: 18-year experience. Urology. 2002;59:227–31.
Böhle A, Jocham D, Bock PR. Intravesical Bacillus Calmette–Guerin versus mitomycin C for superficial bladder cancer: a formal meta-analysis of comparative studies on recurrence and toxicity. J Urol. 2003;169:90–5.
Nepple KG, Lightfoot AJ, Rosevear HM, O’Donnell MA, Lamm DL. Bacillus Calmette–Guérin with or without interferon a-2b and megadose versus recommended daily allowance vitamins during induction and maintenance intravesical treatment of nonmuscle invasive bladder cancer. J Urol. 2010;184:1915–9.
Herr HW, Milan TN, Dalbagni G. BCG-refractory versus BCG-relapsing non-muscle-invasive bladder cancer: a prospective cohort outcomes study. Urol Oncol (Elsevier). 2015;33:108.e1–4.
Kamat AM, Sylvester RJ, Bohle A, Palou J, Lamm DL, Brausi M, et al. Definitions, end points, and clinical trial designs for non-muscle-invasive bladder cancer: recommendations from the international bladder cancer group. J Clin Oncol. 2016;34:1935–44.
Halling KC, King W, Sokolova IA, Meyer RG, Burkhardt HM, Halling AC, et al. A comparison of cytology and fluorescence in situ hybridization for the detection of urothelial carcinoma. J Urol. 2000;164:1768–75.
Pycha A, Mian C, Hofbauer J, Haitel A, Wiener H, Marberger M. Does topical instillation therapy influence chromosomal aberrations in superficial bladder cancer? J Urol. 1998;159:265–9.
Bubendorf L, Grilli B, Sauter G, Mihatsch MJ, Gasser TC, Dalquen P. Multiprobe FISH for enhanced detection of bladder cancer in voided urine specimens and bladder washings. Am J Clin Pathol. 2001;116:79–86.
Kipp BR, Karnes RJ, Brankley SM, Harwood AR, Pankratz VS, Sebo TJ, et al. Monitoring intravesical therapy for superficial bladder cancer using fluorescence in situ hybridization. J Urol. 2005;173:401–4.
Whitson J, Berry A, Carroll P, Konety B. A multicolour fluorescence in situ hybridization test predicts recurrence in patients with high-risk superficial bladder tumours undergoing intravesical therapy. BJU Int. 2009;104:336–9.
Mengual L, Marin-Aguilera M, Ribal MJ, Burset B, Villavicencio H, Oliver A, et al. Clinical utility of fluorescent in situ hybridization for the surveillance of bladder cancer patients treated with Bacillus Calmette–Guerin therapy. Eur Urol. 2007;52:752–9.
Savic S, Zlobec I, Thalmann GN, Engeler D, Schmauss M, Lehmann K, et al. The prognostic value of cytology and fluorescence in situ hybridization in the follow-up of nonmuscle-invasive bladder cancer after intravesical Bacillus Calmette–Guérin therapy. Int J Cancer. 2009;124:2899–904.
Kamat AM, Dickstein RJ, Messetti F, Anderson R, Pretzsch SM, Gonzalez GN, et al. Use of fluorescence in situ hybridization to predict response to Bacillus Calmette–Guerin therapy for bladder cancer: results of a prospective trial. J Urol. 2012;187:862–7.
Gandhi NM, Morales A, Lamm DL. Bacillus Calmette–Guérin immunotherapy for genitourinary cancer. BJU Int. 2013;112:288–97.
de Reijke TM, Boer ECDE, Kurth KH, Schamhart DHJ. Urinary interleukin-2 monitoring during prolonged Bacillus Calmette–Guerin treatment: Can it predict the optimal number of instillations? J Urol. 1999;161:67–71.
Voorter C, Joos S, Bringuier PP, Vallinga M, Poddighe P, Schalken J, et al. Detection of chromosomal imbalances in transitional cell carcinoma of the bladder by comparative genomic hybridization. Am J Pathol. 1995;146:1341–54.
Simon R, Bürger H, Brinkschmidt C, Böcker W, Hertle L, Terpe HJ. Chromosomal aberrations associated with invasion in papillary superficial bladder cancer. J. Pathol. 1998;185:345–51.
Stoehr R, Wissmann C, Suzuki H, Knuechel R, Krieg RC, Klopocki E, et al. Deletions of chromosome 8p and loss of sFRP1 expression are progression markers of papillary bladder cancer. Lab. Investig. 2004;84:465–78.
Goebell PJ, Knowles MA. Bladder cancer or bladder cancers? Genetically distinct malignant conditions of the urothelium. Urol Oncol Semin Orig Investig (Elsevier Inc). 2010;28:409–28.
Cancer T, Atlas G, Weinstein JN, Akbani R, Broom BM, Wang W, et al. Comprehensive molecular characterization of urothelial bladder carcinoma. Nature (Nature Publishing Group). 2014;507:315–22.
Oddens J, Brausi M, Sylvester R, Bono A, Van De Beek C, Van Andel G, et al. Final results of an EORTC-GU cancers group randomized study of maintenance Bacillus calmette-guérin in intermediate- and high-risk Ta, T1 papillary carcinoma of the urinary bladder: one-third dose versus full dose and 1 year versus 3 years of maintenance. Eur Urol. 2013;63:462–72.
Acknowledgements
This study was supported by Abbott and the Cure for Cancer foundation (http://www.cureforcancer.nl). We thank the participating urologists: RJA van Moorselaar (VU Medical Center, Amsterdam), MC Hovius (Onze Lieve Vrouwe Gasthuis Oost, Amsterdam), EA Heldeweg (Onze Lieve Vrouwe Gasthuis West, Amsterdam), J van der Wijk (Refaja ziekenhuis, Stadskanaal) and the department of pathology of the AMC for their support.
Author information
Authors and Affiliations
Corresponding author
Ethics declarations
Conflict of interest
The authors declare no conflicts of interest.
Human and animal rights
The medical ethical committee of the Academic Medical Center reviewed the study protocol and concluded that the study did not imply that participants of the study were subjected to procedures or were required to follow rules of behavior according the ‘Wet Medisch-wetenschappelijk onderzoek met mensen’ (WMO). The WMO is the Medical Research involving Human Beings Act. When the research does not fall under the scope of the WMO, then the protocol does not have to be reviewed by an accredited medical research ethical committee. Therefore, approval of the medical ethical committee was not required. A copy of this decision is available.
Informed consent
Informed consent was verbally obtained from all participants prior to inclusion.
Electronic supplementary material
Below is the link to the electronic supplementary material.
Rights and permissions
Open Access This article is distributed under the terms of the Creative Commons Attribution 4.0 International License (http://creativecommons.org/licenses/by/4.0/), which permits unrestricted use, distribution, and reproduction in any medium, provided you give appropriate credit to the original author(s) and the source, provide a link to the Creative Commons license, and indicate if changes were made.
About this article
Cite this article
Liem, E.I.M.L., Baard, J., Cauberg, E.C.C. et al. Fluorescence in situ hybridization as prognostic predictor of tumor recurrence during treatment with Bacillus Calmette–Guérin therapy for intermediate- and high-risk non-muscle-invasive bladder cancer. Med Oncol 34, 172 (2017). https://doi.org/10.1007/s12032-017-1033-z
Received:
Accepted:
Published:
DOI: https://doi.org/10.1007/s12032-017-1033-z