Abstract
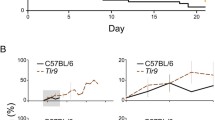
Knockdown studies have shown lymphotoxin-α (Lt-α) as a critical molecule for Experimental cerebral malaria (ECM) pathogenesis. We investigated the role of lymphotoxin-α in regulating active caspase-3 and calpain1. T cell infiltration into the brains, and subsequent neuronal cell death are the essential features of Plasmodium berghei ANKA(PbA)-induced ECM. Our results showed increased Lt-α levels during ECM. Treatment of naïve mice with serum from ECM mice and exogenous Lt-α was lethal. We inhibited Lt-α in vivo during PbA infection by injecting the mice with anti-Lt-α antibody. Inhibition of Lt-α mitigated neuronal cell death and increased mice’s survival until 30-day post-infection (p.i.) compared to only 15 days survival of PbA control mice.






Similar content being viewed by others
References
Anand SS, Maruthi M, Babu PP (2013) The specific, reversible JNK inhibitor SP600125 improves survivability and attenuates neuronal cell death in experimental cerebral malaria (ECM). Parasitol Res 112:1959–1966
Belnoue E, Kayibanda M, Vigario AM, Deschemin JC, van Rooijen N, Viguier M, Snounou G, Renia L (2002a) On the pathogenic role of brain-sequestered alpha beta CD8(+) T cells in experimental cerebral malarial. J Immunol 169:6369–6375
Belnoue E, Kayibanda M, Vigario AM, Deschemin JC, van Rooijen N, Viguier M, Snounou G, Renia L (2002b) On the pathogenic role of brain-sequestered alphabeta CD8+ T cells in experimental cerebral malaria. J Immunol 169:6369–6375
Belnoue E, Potter SM, Rosa DS, Mauduit M, Gruner AC, Kayibanda M, Mitchell AJ, Hunt NH, Renia L (2008) Control of pathogenic CD8+ T cell migration to the brain by IFN-gamma during experimental cerebral malaria. Parasite Immunol 30:544–553
Brown H, Turner G, Rogerson S, Tembo M, Mwenechanya J, Molyneux M, Taylor T (1999) Cytokine expression in the brain in human cerebral malaria. J Infect Dis 180:1742–1746
Calmon-Hamaty F, Combe B, Hahne M, Morel J (2011) Lymphotoxin alpha revisited: general features and implications in rheumatoid arthritis. Arthritis Res Ther 13:232
Carlson J (1993) Erythrocyte rosetting in Plasmodium falciparum malaria–with special reference to the pathogenesis of cerebral malaria. Scand J Infect Dis Suppl 86:1–79
Carlson J, Helmby H, Hill AV, Brewster D, Greenwood BM, Wahlgren M (1990) Human cerebral malaria: association with erythrocyte rosetting and lack of anti-rosetting antibodies. Lancet 336:1457–1460
Combes V, Rosenkranz AR, Redard M, Pizzolato G, Lepidi H, Vestweber D, Mayadas TN, Grau GE (2004) Pathogenic role of P-selectin in experimental cerebral malaria: importance of the endothelial compartment. Am J Pathol 164:781–786
Combes V, Coltel N, Faille D, Wassmer SC, Grau GE (2006) Cerebral malaria: role of microparticles and platelets in alterations of the blood-brain barrier. Int J Parasitol 36:541–546
Craig AG, Grau GE, Janse C, Kazura JW, Milner D, Barnwell JW, Turner G, Langhorne J (2012) participants of the Hinxton Retreat meeting on Animal Models for Research on Severe M: The role of animal models for research on severe malaria. PLoS Pathog 8:e1002401
Dende C, Meena J, Nagarajan P, Panda AK, Rangarajan PN, Padmanaban G (2015) Simultaneously targeting inflammatory response and parasite sequestration in brain to treat Experimental Cerebral Malaria. Sci Rep 5:12671
Dorovini-Zis K, Schmidt K, Huynh H, Fu W, Whitten RO, Milner D, Kamiza S, Molyneux M, Taylor TE (2011) The neuropathology of fatal cerebral malaria in malawian children. Am J Pathol 178:2146–2158
Eeka P, Phanithi PB (2018) Cytotoxic T Lymphocyte Granzyme-b mediates neuronal cell death during Plasmodium berghei ANKA induced experimental cerebral malaria. Neurosci Lett 664:58–65
Engwerda CR, Mynott TL, Sawhney S, De Souza JB, Bickle QD, Kaye PM (2002) Locally up-regulated lymphotoxin alpha, not systemic tumor necrosis factor alpha, is the principle mediator of murine cerebral malaria. J Exp Med 195:1371–1377
Engwerda CR, Ato M, Stager S, Alexander CE, Stanley AC, Kaye PM (2004) Distinct roles for lymphotoxin-alpha and tumor necrosis factor in the control of leishmania donovani infection. Am J Pathol 165:2123–2133
Favre N, Da Laperousaz C, Ryffel B, Weiss NA, Imhof BA, Rudin W, Lucas R, Piguet PF (1999) Role of ICAM-1 (CD54) in the development of murine cerebral malaria. Microbes Infect 1:961–968
Franke-Fayard B, Janse CJ, Cunha-Rodrigues M, Ramesar J, Buscher P, Que I, Lowik C, Voshol PJ, den Boer MA, van Duinen SG et al (2005) Murine malaria parasite sequestration: CD36 is the major receptor, but cerebral pathology is unlinked to sequestration. Proc Natl Acad Sci U S A 102:11468–11473
Grau GE, Piguet PF, Vassalli P, Lambert PH (1989) Tumor-necrosis factor and other cytokines in cerebral malaria: experimental and clinical data. Immunol Rev 112:49–70
Haque A, Best SE, Amante FH, Mustafah S, Desbarrieres L, de Labastida F, Sparwasser T, Hill GR, Engwerda CR (2010) CD4+ natural regulatory T cells prevent experimental cerebral malaria via CTLA-4 when expanded in vivo. PLoS Pathog 6:e1001221
Haque A, Best SE, Unosson K, Amante FH, de Labastida F, Anstey NM, Karupiah G, Smyth MJ, Heath WR, Engwerda CR (2011) Granzyme B expression by CD8+ T cells is required for the development of experimental cerebral malaria. J Immunol 186:6148–6156
Helmers AJ, Lovegrove FE, Harlan JM, Kain KC, Liles WC (2008) Failure of two distinct anti-apoptotic approaches to reduce mortality in experimental cerebral malaria. Am J Trop Med Hyg 79:823–825
Hempel C, Combes V, Hunt NH, Kurtzhals JAL, Grau GER (2011) CNS hypoxia is more pronounced in murine cerebral than noncerebral malaria and is reversed by erythropoietin. Am J Pathol 179:1939–1950
Howland SW, Claser C, Poh CM, Gun SY, Renia L (2015) Pathogenic CD8+ T cells in experimental cerebral malaria. Semin Immunopathol 37:221–231
Huang Y, Yu X, Wang L, Zhou S, Sun J, Feng N, Nie S, Wu J, Gao F, Fei B et al (2013) Four genetic polymorphisms of lymphotoxin-alpha gene and cancer risk: a systematic review and meta-analysis. PloS One 8:e82519
Hunt NH, Grau GE (2003) Cytokines: accelerators and brakes in the pathogenesis of cerebral malaria. Trends Immunol 24:491–499
Langhorne J, Buffet P, Galinski M, Good M, Harty J, Leroy D, Mota MM, Pasini E, Renia L, Riley E et al (2011) The relevance of non-human primate and rodent malaria models for humans. Malar J 10:23
Lochhead J, Movaffaghy A, Falsini B, Harding S, Riva C, Molyneux M (2010) The effects of hypoxia on the ERG in paediatric cerebral malaria. Eye (lond) 24:259–264
Lovegrove FE, Tangpukdee N, Opoka RO, Lafferty EI, Rajwans N, Hawkes M, Krudsood S, Looareesuwan S, John CC, Liles WC, Kain KC (2009) Serum angiopoietin-1 and -2 levels discriminate cerebral malaria from uncomplicated malaria and predict clinical outcome in African children. PloS One 4:e4912
Lundie RJ, de Koning-Ward TF, Davey GM, Nie CQ, Hansen DS, Lau LS, Mintern JD, Belz GT, Schofield L, Carbone FR et al (2008) Blood-stage Plasmodium infection induces CD8+ T lymphocytes to parasite-expressed antigens, largely regulated by CD8alpha+ dendritic cells. Proc Natl Acad Sci U S A 105:14509–14514
Maneerat Y, Viriyavejakul P, Punpoowong B, Jones M, Wilairatana P, Pongponratn E, Turner GDH, Udomsangpetch R (2000) Inducible nitric oxide synthase expression is increased in the brain in fatal cerebral malaria. Histopathology 37:269–277
Medana IM, Day NP, Sachanonta N, Mai NT, Dondorp AM, Pongponratn E, Hien TT, White NJ, Turner GD (2011) Coma in fatal adult human malaria is not caused by cerebral oedema. Malar J 10:267
Miu J, Mitchell AJ, Muller M, Carter SL, Manders PM, McQuillan JA, Saunders BM, Ball HJ, Lu B, Campbell IL, Hunt NH (2008) Chemokine gene expression during fatal murine cerebral malaria and protection due to CXCR3 deficiency. J Immunol 180:1217–1230
Nacer A, Movila A, Baer K, Mikolajczak SA, Kappe SH, Frevert U (2012) Neuroimmunological blood brain barrier opening in experimental cerebral malaria. PLoS Pathog 8:e1002982
Nitcheu J, Bonduelle O, Combadiere C, Tefit M, Seilhean D, Mazier D, Combadiere B (2003) Perforin-dependent brain-infiltrating cytotoxic CD8+ T lymphocytes mediate experimental cerebral malaria pathogenesis. J Immunol 170:2221–2228
Ockenhouse CF, Tegoshi T, Maeno Y, Benjamin C, Ho M, Kan KE, Thway Y, Win K, Aikawa M, Lobb RR (1992) Human vascular endothelial cell adhesion receptors for Plasmodium falciparum-infected erythrocytes: roles for endothelial leukocyte adhesion molecule 1 and vascular cell adhesion molecule 1. J Exp Med 176:1183–1189
Penet MF, Viola A, Confort-Gouny S, Le Fur Y, Duhamel G, Kober F, Ibarrola D, Izquierdo M, Coltel N, Gharib B et al (2005) Imaging experimental cerebral malaria in vivo: significant role of ischemic brain edema. J Neurosci 25:7352–7358
Persaud-Sawin DA, Lightcap A, Jean G (2009) HarryIsolation of rafts from mouse brain tissue by a detergent-free method. J Lipid Res 50(4):759–767. https://doi.org/10.1194/jlr.D800037-JLR200
Pino P, Taoufiq Z, Nitcheu J, Vouldoukis I, Mazier D (2005) Blood-brain barrier breakdown during cerebral malaria: suicide or murder? Thromb Haemost 94:336–340
Ponsford MJ, Medana IM, Prapansilp P, Hien TT, Lee SJ, Dondorp AM, Esiri MM, Day NP, White NJ, Turner GD (2012) Sequestration and microvascular congestion are associated with coma in human cerebral malaria. J Infect Dis 205:663–671
Postma NS, Mommers EC, Eling WM, Zuidema J (1996) Oxidative stress in malaria; implications for prevention and therapy. Pharm World Sci 18:121–129
Potter S, Chan-Ling T, Ball HJ, Mansour H, Mitchell A, Maluish L, Hunt NH (2006) Perforin mediated apoptosis of cerebral microvascular endothelial cells during experimental cerebral malaria. Int J Parasitol 36:485–496
Renia L, Potter SM, Mauduit M, Rosa DS, Kayibanda M, Deschemin JC, Snounou G, Gruner AC (2006) Pathogenic T cells in cerebral malaria. Int J Parasitol 36:547–554
Roach DR, Briscoe H, Saunders B, France MP, Riminton S, Britton WJ (2001) Secreted lymphotoxin-alpha is essential for the control of an intracellular bacterial infection. J Exp Med 193:239–246
Sanni LA (2001) The role of cerebral oedema in the pathogenesis of cerebral malaria. Redox Rep 6:137–142
Shukla M, Rajgopal Y, Babu PP (2006) Activation of calpains, calpastatin and spectrin cleavage in the brain during the pathology of fatal murine cerebral malaria. Neurochem Int 48:108–113
Taylor TE, Fu WJ, Carr RA, Whitten RO, Mueller JS, Fosiko NG, Lewallen S, Liomba NG, Molyneux ME (2004) Differentiating the pathologies of cerebral malaria by postmortem parasite counts. Nat Med 10:143–145
Van den Steen PE, Deroost K, Van Aelst I, Geurts N, Martens E, Struyf S, Nie CQ, Hansen DS, Matthys P, Van Damme J, Opdenakker G (2008) CXCR3 determines strain susceptibility to murine cerebral malaria by mediating T lymphocyte migration toward IFN-gamma-induced chemokines. Eur J Immunol 38:1082–1095
White NJ, Turner GD, Medana IM, Dondorp AM, Day NP (2010) The murine cerebral malaria phenomenon. Trends Parasitol 26:11–15
Wiese L, Kurtzhals JA, Penkowa M (2006) Neuronal apoptosis, metallothionein expression and proinflammatory responses during cerebral malaria in mice. Exp Neurol 200:216–226
Acknowledgements
Funding sources: DST- SERB Core grant, File Nos. CRG/2020/005021, CRG/2019/002570, and financial support to the University of Hyderabad-IoE by the Ministry of Education, Government of India (F11/9/2019-U3 (A). DST-FIST and UGC-SAP to the Department of Biotechnology and Bioinformatics, BUILDER-DBT-BT/INF/22/SP41176/2020 to the School of Life Sciences are gratefully acknowledged.
Funding
This study is funded by DBT (DBT: BT/PR18168/MED/29/1064/2016; DBT: BT/PR13111/MED/29/149/2009, dt. 24 June 2010; DBT-JRF/06–07/184), UPE (UH/UPE-2/28/2015 Dated. 01.12.2015; UH/UGC/UPE-2/Interface studies/Research Projects/B1.4, 24.04.2014), and DST (DST: D.O. No. SR/CSRI/196/2016; DST: SB/EMEQ-257/2013, dt. 12.07.2013).
Author information
Authors and Affiliations
Corresponding author
Ethics declarations
Competing Interests
The authors declare no competing interests.
Additional information
Publisher's Note
Springer Nature remains neutral with regard to jurisdictional claims in published maps and institutional affiliations.
Rights and permissions
Springer Nature or its licensor (e.g. a society or other partner) holds exclusive rights to this article under a publishing agreement with the author(s) or other rightsholder(s); author self-archiving of the accepted manuscript version of this article is solely governed by the terms of such publishing agreement and applicable law.
About this article
Cite this article
Eeka, P., Phanithi, P.B. Lymphotoxin-α Orchestrate Hypoxia and Immune factors to Induce Experimental Cerebral Malaria: Inhibition Mitigates Pathogenesis, Neurodegeneration, and Increase Survival. J Mol Neurosci 72, 2425–2439 (2022). https://doi.org/10.1007/s12031-022-02076-w
Received:
Accepted:
Published:
Issue Date:
DOI: https://doi.org/10.1007/s12031-022-02076-w