Abstract
The associations of OPRM1 gene variants with opioid dependence have been demonstrated. This study investigated the association of rs495491, rs1799971 (A118G), rs589046, and rs10457090 variants of OPRM1 gene with opium dependence and their haplotypes among addicted individuals undergoing methadone treatment. Moreover, we investigated whether any of these variants were associated with libido dysfunction or insomnia among addicted people. A total of 404 individuals were genotyped by amplification refractory mutation system (ARMS) PCR. In silico studies were designed through homology modeling of A118G structures (N40 and D40) and docked with 41 FDA-approved drugs of OPRM1 protein by SWISS-MODEL, COACH, MolProbity, ProSA, Errat, Glide XP, and Autodock 4. Results revealed that rs495491, A118G, rs589046, and rs10457090 were significantly associated with opium dependence under recessive (P = 6.66E-10), dominant (P = 0.017), co-dominant (P = 0.001), and recessive (P = 9.28E-6) models of inheritance, respectively. Further analyses indicated three significant haplotypes including A-A-A-C (P-permutation < 1E-9), G-G-A-C (P-permutation = 0.04), and G-A-G-C (P-permutation = 8.69E-4). Genotype-phenotype associations of OPRM1 variants with insomnia and libido dysfunction showed no significant association. Docking showed the higher binding affinity of N40 rather than D40 model; however, methadone and morphine were bonded with D40 structure more powerful. Consequently, rs495491, A118G, rs589046, and rs10457090 were associated with opioid dependence among Iranians; also, A118G might be the most remarkable marker of OPRM1 owing to its vital structural roles.



Similar content being viewed by others
References
Ahmed M, Ul Haq I, Faisal M, Waseem D, Taqi MM (2018) Implication of OPRM1 A118G polymorphism in opioids addicts in Pakistan: in vitro and in silico analysis. J Mol Neurosci 65(4):472–479
Albonaim A, Fazel H, Sharafshah A, Omarmeli V, Rezaei S, Ajamian F, Fazel H, Sharafshah A, Omarmeli V, Rezaei S, Ajamian F, Keshavarz P (2017) Association of OPRK1 gene polymorphisms with opioid dependence in addicted men undergoing methadone treatment in an Iranian population. J Addict Dis 36(4):227–235
Amato L, Davoli M, Ferri MM, Ali R (2003) Methadone at tapered doses for the management of opioid withdrawal. Cochrane Database Syst Rev (2):CD003409. https://doi.org/10.1002/14651858.CD003409
Athanasos P, Smith CS, White JM, Somogyi AA, Bochner F, Ling WJP (2006) Methadone maintenance patients are cross-tolerant to the antinociceptive effects of very high plasma morphine concentrations. Pain 120(3):267–275
Bart G, Kreek MJ, Ott J, LaForge KS, Proudnikov D, Pollak L, Heilig MJN (2005) Increased attributable risk related to a functional μ-opioid receptor gene polymorphism in association with alcohol dependence in central Sweden. Neuropsychopharmacology 30(2):417
Bond C, LaForge KS, Tian M, Melia D, Zhang S, Borg L et al (1998) Single-nucleotide polymorphism in the human mu opioid receptor gene alters β-endorphin binding and activity: possible implications for opiate addiction. Proc Natl Acad Sci USA 95(16):9608–9613
Bunten H, Liang W, Pounder D, Seneviratne C, Osselton DJCP, Therapeutics (2010) OPRM1 and CYP2B6 gene variants as risk factors in methadone-related deaths. Clin Pharmacol Ther 88(3):383–389
Bunten H, Liang WJ, Pounder D, Seneviratne C, Osselton MD (2011) CYP2B6 and OPRM1 gene variations predict methadone-related deaths. Addict Biol 16(1):142–144
Chen VB, Arendall WB, Headd JJ, Keedy DA, Immormino RM, Kapral GJ et al (2010) MolProbity: all-atom structure validation for macromolecular crystallography. Acta Crystallographica Section D: Biological Crystallography 66(1):12–21
Clarke T-K, Crist RC, Kampman KM, Dackis CA, Pettinati HM, O’Brien CP et al (2013) Low frequency genetic variants in the μ-opioid receptor (OPRM1) affect risk for addiction to heroin and cocaine. Neuroscience letters 542:71–75
Colovos C, Yeates TO (1993) Verification of protein structures: patterns of nonbonded atomic interactions. Protein science 2(9):1511–1519
Corley RP, Zeiger JS, Crowley T, Ehringer MA, Hewitt JK, Hopfer CJ et al (2008) Association of candidate genes with antisocial drug dependence in adolescents. Drug Alcohol Depend 96(1-2):90–98
Deb I, Chakraborty J, Gangopadhyay PK, Choudhury SR, Das S (2010) Single-nucleotide polymorphism (A118G) in exon 1 of OPRM1 gene causes alteration in downstream signaling by mu-opioid receptor and may contribute to the genetic risk for addiction. J Neurochem 112(2):486–496
Dole VP, Nyswander MJJ (1965) A medical treatment for diacetylmorphine (heroin) addiction: a clinical trial with methadone hydrochloride. JAMA 193(8):646–650
Donny EC, Brasser SM, Bigelow GE, Stitzer ML, Walsh SLJA (2005) Methadone doses of 100 mg or greater are more effective than lower doses at suppressing heroin self-administration in opioid-dependent volunteers. Addiction 100(10):1496–1509
Drakenberg K, Nikoshkov A, Horváth MC, Fagergren P, Gharibyan A, Saarelainen K et al (2006) μ Opioid receptor A118G polymorphism in association with striatal opioid neuropeptide gene expression in heroin abusers. Proceedings of the National Academy of Sciences 103(20):7883–7888
Eap CB, Buclin T, Baumann PJC (2002) Interindividual variability of the clinical pharmacokinetics of methadone. Clin Pharmacokinet 41(14):1153–1193
Gowing L, Ali R, White J (2009) Opioid antagonists with minimal sedation for opioid withdrawal. Cochrane Database Syst Rev (4). https://doi.org/10.1002/14651858.CD002021
Guex N, Peitsch MC (1997) SWISS-MODEL and the Swiss-Pdb Viewer: an environment for comparative protein modeling. electrophoresis. Electrophoresis 18(15):2714–2723
Haerian BS, Haerian MSJP (2013) OPRM1 rs1799971 polymorphism and opioid dependence: evidence from a meta-analysis. Pharmacogenomics 14(7):813–824
Johnson AD, Zhang Y, Papp AC, Pinsonneault JK, Lim J-E, Saffen D et al (2008a) Polymorphisms affecting gene transcription and mRNA processing in pharmacogenetic candidate genes: detection through allelic expression imbalance in human target tissues. Pharmacogenet Genomics 18(9):781
Johnson SM, Kinney ME, Wiegel LM (2008b) Inhibitory and excitatory effects of μ-, δ-, and κ-opioid receptor activation on breathing in awake turtles Trachemys scripta. Am J Physiol Regul Integr Comp Physiol 295(5):R1599–R1612
Kelley LA, Mezulis S, Yates CM, Wass MN, Sternberg MJ (2015) The Phyre2 web portal for protein modeling, prediction and analysis. Nature protocols 10(6):845–858
Kreek MJJJ (1973) Medical safety and side effects of methadone in tolerant individuals. Jama 223(6):665–668
Kreek MJ, Levran O, Reed B, Schlussman SD, Zhou Y, Butelman ERJT (2012) Opiate addiction and cocaine addiction: underlying molecular neurobiology and genetics. J Clin Invest 122(10):3387–3393
Levran O, Londono D, O’hara K, Nielsen D, Peles E, Rotrosen J et al (2008) Genetic susceptibility to heroin addiction: a candidate gene association study. Genes, Brain and Behavior 7(7):720–729
Lu LJP p (2015) The impact of genetic variation on sensitivity to opioid analgesics in patients with postoperative pain: a systematic review and meta-analysis. Pain physician 18:131–152
Mattick RP, Breen C, Kimber J, Davoli MJCdosr (2009) Methadone maintenance therapy versus no opioid replacement therapy for opioid dependence. Cochrane Database Syst Rev (3):CD002209. https://doi.org/10.1002/14651858.CD002209
Max MB, Wu T, Atlas SJ, Edwards RR, Haythornthwaite JA, Bollettino AF, Hipp HS et al (2006) A clinical genetic method to identify mechanisms by which pain causes depression and anxiety. Molecular Pain 2(1):1744–8069
Miller S, Dykes D, Polesky H (1988) A simple salting out procedure for extracting DNA from human nucleated cells. Nucleic acids research 16(3):1215
Morris GM, Huey R, Lindstrom W, Sanner MF, Belew RK, Goodsell DS, Olson AJ (2009) AutoDock4 and AutoDockTools4: Automated docking with selective receptor flexibility. J Comput Chem 30(16):2785–2791
Nielsen D, Ji F, Yuferov V, Ho A, Chen A, Levran O et al (2008) Genotype patterns that contribute to increased risk for or protection from developing heroin addiction. Molecular psychiatry 13(4):417
Nikolov MA, Beltcheva O, Galabova A, Ljubenova A, Jankova E, Gergov G et al (2011) No evidence of association between 118A > G OPRM1 polymorphism and heroin dependence in a large Bulgarian case–control sample. Drug and alcohol dependence 117(1):62–65
Nishizawa D, Han W, Hasegawa J, Ishida T, Numata Y, Sato T et al (2006) Association of μ-opioid receptor gene polymorphism A118G with alcohol dependence in a Japanese population. Neuropsychobiology 53(3):137–141
Oertel BG, Kettner M, Scholich K, Renné C, Roskam B, Geisslinger G et al (2009) A common human μ-opioid receptor genetic variant diminishes the receptor signaling efficacy in brain regions processing the sensory information of pain. J Biol Chem 284(10):6530–6535
Olesen AE, Sato H, Nielsen LM, Staahl C, Droney J, Gretton S et al (2015) The genetic influences on oxycodone response characteristics in human experimental pain. Fundamental & Clinical Pharmacology 29(4):417–425
Pang GS, Wang J, Wang Z, Goh C, Lee CGJP (2009) The G allele of SNP E1/A118G at the μ-opioid receptor gene locus shows genomic evidence of recent positive selection. Pharmacogenomics 10(7):1101–1109
Rahimi Movaghar A, Mohammad K, Razzaghi EJHRJ (2002) Trend of drug abuse situation in Iran: a three-decade survey. Hakim Res J 5(3):171–181
Ray R, Jepson C, Patterson F, Strasser A, Rukstalis M, Perkins K et al (2006) Association of OPRM1 A118G variant with the relative reinforcing value of nicotine. Psychopharmacology 188(3):355–363
Savage SR, Kirsh KL, Passik SDJA s, practice, c (2008) Challenges in using opioids to treat pain in persons with substance use disorders. Addiction science & clinical practice 4(2):4
Serohijos AW, Yin S, Ding F, Gauthier J, Gibson DG, Maixner W et al (2011) Structural basis for μ-opioid receptor binding and activation. Structure 19(11):1683–1690
Sharafshah A, Fazel H, Albonaim A, Omarmeli V, Rezaei S, Mirzajani E et al (2017) Association of OPRD1 gene variants with opioid dependence in addicted male individuals undergoing methadone treatment in the North of Iran. J Psychoactive Drugs 49(3):242–251
Shi J, Hui L, Xu Y, Wang F, Huang W, Hu GJH m (2002) Sequence variations in the mu-opioid receptor gene (OPRM1) associated with human addiction to heroin. Human mutation 19(4):459–460
Shippenberg TS, Chefer VI, Thompson ACJB p (2009) Delta-opioid receptor antagonists prevent sensitization to the conditioned rewarding effects of morphine. Biological Psychiatry 65(2):169–174
Sippl MJ (1993) Recognition of errors in three-dimensional structures of proteins. Proteins: Structure, Function, and Bioinformatics 17(4):355–362
Wang S-C, Tsou H-H, Chen C-H, Chen Y-T, Ho K, Hsiao C-F et al (2012) Genetic polymorphisms in the opioid receptor mu1 gene are associated with changes in libido and insomnia in methadone maintenance patients. European Neuropsychopharmacology 22(10):695–703
Wiederstein M, Sippl MJ (2007) ProSA-web: interactive web service for the recognition of errors in three-dimensional structures of proteins. Nucleic acids research 35(suppl_2):W407–W410
Wolff K, Sanderson M, Hay A, Raistrick DJCC (1991) Methadone concentrations in plasma and their relationship to drug dosage. Clin Chem 37(2):205–209
Yang J, Roy A, Zhang Y (2012) BioLiP: a semi-manually curated database for biologically relevant ligand–protein interactions. Nucleic acids research 41(D1):D1096–D1103
Yang J, Roy A, Zhang Y (2013) Protein–ligand binding site recognition using complementary binding-specific substructure comparison and sequence profile alignment. Bioinformatics 29(20):2588–2595
Zhang Y, Wang D, Johnson AD, Papp AC, Sadée WJJoBC (2005) Allelic expression imbalance of human mu opioid receptor (OPRM1) caused by variant A118G. J Biol Chem 280(38):32618–32624
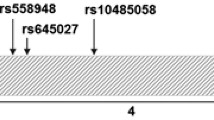
Zhang H, Luo X, Kranzler HR, Lappalainen J, Yang B-Z, Krupitsky E et al (2006) Association between two μ-opioid receptor gene (OPRM1) haplotype blocks and drug or alcohol dependence. Human Molecular Genetics 15(6):807–819
Zhang D, Shao C, Shao M, Yan P, Wang Y, Liu Y et al (2007) Effect of μ-opioid receptor gene polymorphisms on heroin-induced subjective responses in a. Chinese population. 61(11):1244–1251
Acknowledgments
The authors are grateful and have special thanks for the consultation and help of Dr. B. Soltani as the head of Cellular and Molecular Research Center (CMRC), and the other colleagues in CMRC, University of Medical Sciences, Guilan, Rasht.
Author information
Authors and Affiliations
Corresponding author
Ethics declarations
Conflict of Interest
The authors declare that they have no conflict of interest.
Additional information
Publisher’s Note
Springer Nature remains neutral with regard to jurisdictional claims in published maps and institutional affiliations.
Rights and permissions
About this article
Cite this article
Tolami, H.F., Sharafshah, A., Tolami, L.F. et al. Haplotype-Based Association and In Silico Studies of OPRM1 Gene Variants with Susceptibility to Opioid Dependence Among Addicted Iranians Undergoing Methadone Treatment. J Mol Neurosci 70, 504–513 (2020). https://doi.org/10.1007/s12031-019-01443-4
Received:
Accepted:
Published:
Issue Date:
DOI: https://doi.org/10.1007/s12031-019-01443-4