Abstract
The present study demonstrates capacity of α-MSH to augment recovery from ischemia/reperfusion (I/R)-induced retinal damage in vivo and correlation of its protective effects with expression of heme oxygenase-1 (HO-1). Used techniques include ocular ischemia and reperfusion, electroretinography, histology, electron microscopy, and molecular-biological techniques. The results demonstrate the α-MSH-mediated inhibition of I/R-induced functional deterioration of the retina. Outcomes suggest that the protective effects of α-MSH occur mainly through HO-1-dependent pathways but HO-1-independent mechanisms may also contribute to protection. The observation that post-ischemic treatment with α-MSH exhibits therapeutic efficacy in the same range as pre-ischemic treatment, is a novel result. This outcome suggests a highly conserved protective role for α-MSH as a major stress response mechanism—and offers the possibility for development of novel therapeutic strategies utilizing this hormone, in particular in treatment of conditions resulting from I/R injury, such as deterioration of retinal microcirculation. The merit of the study lies in the fact that I/R injury contribute significantly to the severity of retinopathies. However, currently there are no evidence-based treatments for retinal I/R injury available for clinical use. Our finding suggests that α-MSH may have a very wide range of uses in the prevention of I/R-mediated pathologies.
Similar content being viewed by others
Avoid common mistakes on your manuscript.
Introduction
Ischemia/reperfusion (I/R) injury and the resulting deterioration of tissue microcirculatory capacity are major contributing factors in many diseases, including retinal vascular occlusion (Jonas et al. 2010), glaucoma (Agarwal et al. 2009), and diabetic retinopathy (Curtis et al. 2009). Despite an evolving understanding of I/R-associated disease pathogenesis, no evidence-based strategies for the prevention and therapy of I/R-related ocular diseases are available at the time of this writing. The results of previous work by the authors of this report suggest that alpha-melanocyte-stimulating hormone (α-MSH) may have potential for the prevention and treatment of I/R-associated pathologies, including ocular disease (Vecsernyes et al. 2003).
This tridecapeptid homone is derived from posttranslational processing of a precursor protein called proopiomelanocortin. Physiological functions of melanocyte-stimulating hormones include: stimulation of melanogenesis (Tsatmali et al. 2002), regulation of appetite and energy balance (Morton et al. 2006), sexual arousal, and erectile function (Shadiack et al. 2007), along with a wide range of anti-inflammatory and protective effects, most notably protection from I/R injury (Lipton et al. 1994). α-MSH is known to protect against ischemic damage of the brain (Forslin Aronsson et al. 2006), kidney (Chiao et al. 1997), and gastrointestinal tract (Zou et al. 2003). Additionally, authors have demonstrated α-MSH-mediated preservation of ischemic-reperfused myocardium (Bazzani et al. 2001; Vecsernyes et al. 2003). Ocular I/R pathologies typically cause significantly adverse effects on retinal tissue as well. However, at the time of this writing, the ability of α-MSH to protect the retina has not been comprehensively investigated.
Heme oxygenase 1 (HO-1), also known as heat shock protein 32, has been shown to mitigate the effects of many human diseases by contributing to the regulation of inflammatory processes and restoration of normal immune homeostatic conditions (Csonka et al. 1999; Juhasz et al. 2011; Haines et al. 2012). The enzyme has also been reported to play a critical role in α-MSH protection against I/R injury in skin (Kokot et al. 2009), gut (Zou et al. 2003), and peritoneal macrophages (Lam et al. 2005). The present investigation evaluates a correlation between HO-1 expression and α-MSH amelioration of I/R injury to the retina. The outcomes reported here are the first demonstrations of α-MSH-mediated recovery from I/R-induced retinal damage.
Study Goals
The present study demonstrates the protective effects of α-MSH on the recovery of I/R-induced retinal damage in a rat model. A major goal of this research was to identify an effective α-MSH dose range to achieve significant preventive and therapeutic effects in the test animals. These evaluations were conducted using electroretinography (ERG), as described below. Following the identification of an optimal dose range for the outcomes measured, assessments of related physiological parameters were investigated, including α-MSH effects on the degree of I/R-induced retinal edema, structural degenerative changes on the retina, and HO-1 protein expression. Results shown here demonstrate a correlation between α-MSH, therapeutic outcomes, and HO-1 expression. A corollary objective of the present study was to suggest whether non-HO-1-dependent mechanisms downstream of α-MSH might also contribute to protective effects of the hormone. Finally, a hypothesis that α-MSH is an evolutionarily conserved stress response hormone was evaluated by studying the effect of post-ischemic treatment with α-MSH.
Materials and Methods
Animals
The experiments described in the present report were conducted using male Sprague Dawley rats (Crl/SD). Animals weighing 300–350 g were purchased from Charles River Laboratories International, Inc. (Wilmington, Massachusetts). All animals received humane care in compliance with the ARVO Statement for the Use of Animals in Ophtalmic and Vision Research and the NIH guidelines. All of the protocols used in the present study were approved by the Institutional Animal Care Committee of University of Debrecen in Debrecen, Hungary. The rats were fed regular rodent chow ad libitum with free access to water until the initiation of experimental procedures.
Ocular I/R
The animals were anaesthetized with intramuscular injections of ketamin/xylazine (50/5 mg/kg) at the outset of each experimental procedure. Subsequently, the retinal artery supplying blood to left eye of each animal was surgically occluded using a protocol previously applied by the authors of related studies (Szabo et al. 2004). Briefly, eyelids were retracted using sutures, followed by the use of a traction-type occluder (a silk suture thread through a polyethylene guide cannula) for retinal artery blockage. The suture was placed behind the eyeball, loosely around the optic nerve, central retinal artery, ciliary arteries, and the retrobulbar connective tissue. By pulling the suture and pressing the tube against the surface of the optic nerve, ischemia was induced and maintained for the required length of time. Ischemia was verified macroscopically with a 120-D lens. Reperfusion of retinal tissue was accomplished by post-ischemic release of the occluder, allowing resumption of blood flow through the retinal artery.
Electroretinography
The animals were prepared for electroretinographic measurements by anesthesia with 50/5 mg/kg of ketamin/xylazine, administered as intramuscular injections. Both pupils of each animal were dilated with 0.5 % cyclopentolate hydrochloride (Humapent, Teva, Hungary) and 10 % phenylephrine hydrochloride (Neosynephrin-HCL, Ursapharm, Saarbruecken, Germany).
Detailed description of the system used by our workgroup for recording electroretinograms is as follows. Five silver needle electrodes were used for each measurement. In clinical practice ERG is praised for being a noninvasive technique, however, in our case, where eyes of the animals are used as experimental samples for different molecular biological assessments, this was not a requirement. And we found that in contrast to regular contact lens type electrodes, electrical contact, and signal throughput of needle electrodes carefully and superficially inserted into corneal surface, is much better. Retinal signals were analyzed using two measuring electrodes (one on each eye), inserted into corneal surfaces so as to avoid scleral damage or corneal perforation. Two reference electrodes were positioned on the earlobes of each animal (one on each earlobe) and the main ground electrode at the glabella. Effective electrical contacts and protection of eyes from dehydration was provided by a solution of methylcellulose (0.5 %). After a short dark adaptation period (20 min), the eyes were illuminated with a self-built stroboscope (20 cd/m2, 0.5 Hz). Electrical signals corresponding to retinal changes passed through an ERG-recording system (ADInstruments, Australia) composed of an amplifier and an analog–digital converter (Bridge Amp and PowerLab, ADInstruments, Australia), displayed on a PC monitor, and analyzed using a software, PowerLab Chart (Version 5.2.2., ADInstruments, Australia). Obtained electroretinograms contain well identifiable, definite spikes composed of a negative peak followed by a highly positive peak which then fade out through another negative peak, and a steady, moderate extraneous signal (background noise). Although the appearance is not the same as with other “standard” ERG-systems, the highly positive peak is definitely the maximum of b wave, preceded by a negative peak (the negative maximum of a wave). This conclusion can be drawn from the fact that these electrical activities (spikes) occur consistently after light stimulus with the same rhythm, same frequency the stroboscope has (0.5 Hz), and that the most intense electrical activity on a common, “standard” ERG recording to cause such highly positive peak is the b wave alone. However, a waves or other minor components of the ERG cannot be clearly identified: e.g., amplitude of the probable a waves was in the same range as extraneous signal (background noise) present in each of the recordings, which hinders clear interpretation of a wave ERG data. Nevertheless, it should also be mentioned that in this study there was no need to be able to measure such subtleties as c waves or oscillatory potencials, only changes in electrical activity of retina, which is related to retina function. Actual amplitudes of b waves were measured between the (preceding) negative and the highly positive peaks of a spike. The outcome of ERG experiments formerly conducted by the authors with the same recording system demonstrated that the aforementioned experimental strategy provides reproducible, cost-effective data on retinal function, closely correlated to the survival of retinal cells (Varga et al. 2011).
Processing for Examination by Light and Electron Microscopy
Samples designated for examination by light or fluorescent microscopy were produced according to the following general protocol: the fixation of retinal tissue was accomplished via trans-aortic cardiac cannulization, accompanied by a surgical incision in the right ventricle to allow a free outflow of blood. The vasculature of each animal was flushed (perfused) with physiological saline (0.9 % NaCl) to clear their system of blood. In each case, perfusion time was limited to 20-s interval to minimize nervous tissue edema. Physiological saline rinses were conducted concurrently with the fixation of retinas with 100 ml Bouin solution, followed by an extraction of bulbi and coronalis sectioning, bisecting each eyeball along the ora serrata. The vitreum of each eye was removed, and the bulbs were fixed, alcohol dehydrated, and paraffinized.
Some paraffinized bulbi were processed into 7-μm sagittal sections, which were then dyed with hematoxylin–eosin (HE) and examined by light microscopy. According to previous reports, I/R-induced edema formation is well recognized and documented in the inner plexiform layer of the retina (Shakib and Ashton 1966; Juarez et al. 1986). The average thickness for each eye was measured in the inner plexiform layer in sagittal sections at near the optic disc and expressed in micrometers using a manual scale on each glass slide.
Paraffinized bulbi from a second group of eyes were sectioned into 60-μm sagittal slices and prepared for electron microscopic (EM) examination by fixation of tissue lipids with osmium tetroxide (OsO4). (Fixation of tissue proteins was done earlier by the formaldehyde constituent of the Bouin solution.) Samples fixed with OsO4 were alcohol dehydrated and embedded into Araldite epoxy, and then heat treated at 56 °C for 2 days to induce polymerization (hardening). The samples were subsequently processed by ultramicrotome into (ultrathin) sections adequate for EM-based analysis.
Western Blot Analysis for HO-1 Protein Expression
Enucleated bulbi were suspended in a homogenisation buffer composed of Tris, 25 mM; NaCl, 25 mM; Na-orthovanadate, 1 mM; NaF, 10 mM; Na-pyrophosphate, 10 mM; Okadaic acid, 10 nM; EDTA, 0.5 mM; PMSF, 1 mM; protease inhibitor cocktail; and distilled water (Sigma-Aldrich, St. Louis, Missouri). Samples of homogenized bulbi (50 μg protein per sample) and protein standards were electrophoretically fractionated using SDS-polyacrylamide gels with 12 % acrylamide-to-bis ratios. Protein standards included PageRuler Prestained Protein Ladder (Fermentas GmBH, Germany). Fractionized proteins were subsequently transferred onto Protran Nitrocellulose Membranes (Whatman International Ltd., UK) in a protocol using Mini Trans-Blot Electrophoretic Transfer Cell (Bio-Rad Laboratories Ltd.). Blocking of each blot was accomplished using Tris-buffered saline with Tween 20 for 1.5 h with 5 % (w/v) nonfat dry milk. Subsequently each blot was incubated overnight at 4 °C with primary anti-HO-1 antibodies (Sigma-Aldrich), diluted 1:1,000 in TBS-T. Subsequently, each blot was incubated for 1 h with horseradish peroxidase-conjugated secondary antibody, diluted 1:2,000 in TBS-T, and 5 % (w/v) nonfat dry milk. After incubation and a short wash period, blots were treated with enhanced chemiluminescence reagents (Millipore, Billerica, MA). Detection was carried out via autoradiography for varying lengths of time with Medical X-Ray Film (Agfa-Gevaert N.V., Belgium). Films were scanned and evaluated with Scion Image software (Scion Corporation, Torrance, CA). GAPDH was used as loading control (Sigma-Aldrich).
Measurement of Heme Oxygenase Activity
Activity of heme oxygenase (HO) in bulbal tissue was measured according to the following general protocol: enucleated bulbi were homogenized in a solution containing HEPES, 10 mM; sucrose, 32 mM; DTT, 1 mM; EDTA, 0.1 mM; soybean trypsin inhibitor, 10 μg/ml; Leupeptin, 10 μg/ml; Aprotinin, 2 μg/ml; pH 7.4 (homogentisate buffer). All reagents were purchased from Sigma-Aldrich. The supernatant was collected by centrifugation of the homogenate for 30 min at 20,000×g at 4 °C. Assessment of HO activity was performed on each sample of supernatant, according to procedures used by Tenhunen et al. (1968). Briefly, HO activity was estimated based on a spectrophotometric measurement of bilirubin formation in a reaction mixture containing: an aliquot of the supernatant, plus glucose-6-phosphate, 2 mM; glucose-6-phosphate dehydrogenase, 0.14 U/ml; heme, 15 μM; NADPH, 150 μM, rat liver cytosol as a source of biliverdin reductase, 120 μg/ml; MgCl2, 2 mM, and KH2PO4, 100 mM. After incubation in darkness for 60 min, the reaction was stopped by putting the samples on ice. Bilirubin formation was calculated on the basis of difference between optical densities obtained at 460 and 530 nm. The amount of bilirubin (in nanomoles) produced per hour per milligram protein was defined as one unit of HO activity.
Differences seen between results of two activity measurements from two different samples but from the same tissue type may be attributed to HO-1 activity since other isoforms of the enzyme are of the noninducible, constitutive form.
Major Investigative Strategies
Experimental Design Strategy I (Part 1 Experiments)
The first major strategy used in the present study was conducted to find the best dosage and to evaluate the capacity of α-MSH to mitigate I/R-induced ocular pathologies. This strategy (Table 1) included the following major features: the animals were divided randomly into two major treatment groups, groups I-a and I-b (n = 30 in each group). Group I-a served as a dose–response study group and included five subgroups: a control group and four treatment groups (n = 6 in each subgroup). Twelve hours before induction of ischemia, vehicle-treated controls were given subcutaneous (s.c.) physiological saline, while the other four groups were administered s.c. 50, 250, 500, and 1,000 μg/kg α-MSH (Sigma-Aldrich), respectively. α-MSH used for experiments described here was prepared as a solution of the hormone in physiological saline.
Group I-b, which was considered to estimate the effects of α-MSH, included two subgroups (n = 15 in each subgroup). Twelve hours before induction of ischemia vehicle-treated controls were given physiological saline (s.c.), while the other subgroup was administered 500 μg/kg α-MSH (s.c.), an effective dose previously identified in group I-a by electroretinographic measurements.
Animals in group I-a were subjected to 30 min of ischemia in one eye as described above, followed by a 24-h period of reperfusion and ERG measurements as described above. Group I-b animals received 90 min of ischemia in one eye, followed by the same 24-h reperfusion treatment that group I-a animals were administered. The basis for selection of the two aforementioned ischemic time intervals is based on a previous observation by the authors of the present study that retinal edema, a focus of study in this research, fails to develop following only 30 min of ischemia but develops definitively in rat eyes treated for 90 min (Szabo et al. 1991). However, a 90-min ischemic period induces near blindness, making ERG measurements impractical. Hence, the design strategy for part 1 of the present study incorporated two major groups of animals segregated according to the length of the ischemic period prior to reperfusion.
Bulbi collected from group I-b were divided into three groups (n = 5 in each group), and segregated according to processing for evaluation of α-MSH influence on I/R-related pathologies. The first group of samples was subjected to histological examination using HE-stained sections and light microscopy; the second group was osmium-fixed and analyzed by electron microscopy; and a third group of bulbar samples was used as source material for a Western blot assay as described above.
Experimental Design Strategy II (Part 2 Experiments)
Part II experiments were conducted to evaluate the efficacy of post-ischemic α-MSH-treatment against I/R injury and also to assess the significance of HO-1 in the effect of α-MSH. This experimental design strategy (Table 2.) included the following major features: Animals (group II; n = 20) were divided randomly into four major treatment cohorts (n = 5 in each group), designated as shown below with drugs administered according to the indicated timeline.
Control animals were treated intraperitoneally (i.p.) with vehicle of SnPP (described below) 5, 3, and 1 day before induction of ischemia, and then with physiological saline (vehicle of α-MSH) subcutaneously at the outset of post-ischemic reperfusion.
A second group of animals were treated with vehicle of SnPP (i.p.) 5, 3, and 1 day before induction of ischemia and then with 500 μg/kg α-MSH (s.c.) at the outset of postischemic reperfusion. α-MSH used for experiments described here was prepared as a solution of the hormone in physiological saline.
A third group of animals were treated with 50 μmol/kg SnPP (i.p.) 5, 3, and 1 day before the induction of ischemia, and then with 500 μg/kg α-MSH (s.c.) at the outset of post-ischemic reperfusion. SnPP (Frontier Scientific Inc., Logan, Utah) is a potent inhibitor of HO-1 (Drummond and Kappas 1981). SnPP was dissolved in 0.1 N sodium hydroxide, adjusted with HCl to pH 7.4 and diluted with physiological saline. Each batch of SnPP was prepared within 1 h of use and protected from light.
A fourth group of animals were treated with 50 μmol/kg SnPP (i.p.) 5, 3, and 1 day before induction of ischemia, and then with physiological saline (s.c.) at the outset of post-ischemic reperfusion.
Retinal ischemia was applied in each group for 30 min followed by 24 h of reperfusion. Then ERG and retinal tissue HO activity measurement were performed to evaluate the effect of the abovementioned treatment combinations on I/R injury.
Statistical Analysis
A one-way analysis of variance with a Tukey posttest was used for Gaussian data results from the D’Agostino and Pearson omnibus normality test. Data with nonparametric distribution was analyzed using the Kruskal–Wallis test along with the Dunn’s posttest.
In Figs. 2, 6b, and 7, results are represented as percentages with SEM. SEM is also calculated in percentage using the following formula: (SEM/R)*(R%), where R is the average of individual result values (not percentage). SEM is standard error of the mean calculated from the individual result values, and R% is the R expressed in percentage.
Results
Outcomes of Experimental Design Strategy I (Part I Experiments)
Electroretinographic Selection of Optimal α-MSH Dosage
The initial objective of work performed in part I of the present study was to identify an effective dose range of α-MSH using ERG. Figure 1 shows actual voltage levels and the time course of ERG spikes observed in part I studies, while percentages of mean values of all ischemic b waves relative to control baseline are shown in Fig. 2. Significant differences between non-I/R values were not observed (data not shown).
Effects of α-MSH doses on ERG b waves (group I-a). Shown here are percentages of mean values of b waves measured in electroretinogramms of baseline and ischemic/reperfused eyes of vehicle-treated (control) animals and ischemic/reperfused eyes of rats treated with 50, 250, 500, and 1,000 μg/kg α-MSH with standard error of the mean (SEM). Percentages were calculated relative to control baseline values. Horizontal lines indicate comparisons. The significance of comparisons is indicated as follows: ns not significant; *p < 0.05; **p < 0.01; ***p < 0.001
I/R injury as measured by ERG b-wave measurements degraded retinal function to 31.64 % of that exhibited by nonischemic (baseline) eyes of control animals (Fig. 2). Administration of α-MSH dose responsively improved retinal function in I/R-injured eyes of animals to a value of 66.18 % of control baseline—a significant outcome achieved in I/R-injured eyes of animals treated with a 1,000 μg/kg α-MSH (p < 0.001 vs. control I/R). I/R-mediated retinal damage was severe to such an extent that α-MSH treatment could not fully restore function of the tissue to normal levels. Moreover, dose-responsive improvement in tissue functional parameters leveled off at a dosage of 1,000 μg/kg, beyond which it is anticipated that negligibly more favorable changes would be observed.
The optimal effective dose range identified in the present experimental setting was observed to be 250–500 μg/kg of α-MSH. Measureable effects of α-MSH-treatment on the b waves of ERG were also observed at a dosage as low as 50 μg/kg (35.64 % of control baseline); however, the magnitude of improvements was not statistically significant at this dosage, only at higher doses, such as 250 (48.00 %, p < 0.001 vs. control I/R) and 500 μg/kg (64.36 %, p < 0.001 vs. control I/R). Treatment with 1,000 μg/kg mediated a significant protective effect on retinal function, but since no statistically significant improvement in outcome was observed between 500 and 1,000 μg/kg (64.36 vs. 66.18 %), it has been concluded that a 500-μg/kg dosage is sufficient and probably optimal for inhibition of I/R-mediated retinal damage.
Evaluation of the Capacity of α-MSH to Mitigate I/R-Induced Ocular Pathologies
Histology
As shown in Fig. 3, retinal layers become thickened as a result of I/R-induced interstitial edema formation, an effect seen by comparison of Fig. 3a, the nonischemic control retinal sections (control non-I/R) in which no evidence of tissue damage may be seen, with Fig. 3b, the I/R-injured retinal tissue from rats not treated with α-MSH (control I/R). The effect of 500 μg/kg α-MSH is shown in Fig. 3c, which demonstrates the ability of the hormone to inhibit the development of I/R-induced damage, principally retinal edema and resultant thickening. The relative effects on retinal thickness of I/R injury and α-MSH treatment are shown in Fig. 3d. Significant differences between control and treated non-I/R values were not observed (data not shown).
Effect of α-MSH on I/R-induced retinal edema (group I-b). Sagittal sections of the rat retina showing the structure of layers in nonischemic retinal tissue of vehicle-treated (control) animals (a), I/R-injured retinal tissue from vehicle-treated (control) rats (b), and I/R-injured retinal tissue from animals treated with 500 μg/kg α-MSH (c). d The effect of α-MSH on the extent of retinal edema following I/R injury, in the inner plexiform layer. Thickness was measured using a manual scale on each glass slides. Mean ± SEM; *p < 0.05 vs. control I/R
Electron microscopy
EM ultrastructure of retinal pigment cells and photoreceptors revealed no apparent morphological changes in cells in the outer retinal layers following I/R injury (data not shown). However, I/R-mediated damage to mitochondria of inner retinal cells was clearly observed. Figure 4a through c shows damaged mitochondria in inner retinal cells of I/R-injured retinal tissue from control animals. These images demonstrate disintegration of the mitochondria due to formation of interior vacuoles. By contrast, inner retinal cell mitochondria from I/R-injured retinas taken from animals treated with 500 μg/kg α-MSH appeared intact with no vacuolization (Fig. 4d through g). Significant differences between control and treated non-I/R ultrastructure were not observed (data not shown).
EM studies (group I-b). a–c Mitochondria in I/R-injured inner retinal cells from rats not treated with α-MSH. These images demonstrate disintegration of the mitochondria due to formation of interior vacuoles (arrows). Mitochondria in I/R-injured inner retinal cells from animals treated with 500 μg/kg α-MSH are shown in (d–g). No vacuolization is seen here
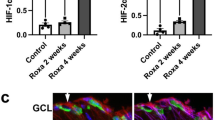
Western Blot Analysis
Western blot analysis of HO-1 expression in ocular tissue revealed significantly greater amounts of HO-1 protein in I/R-injured bulbi taken from animals receiving 500 μg/kg α-MSH treatment than from vehicle-treated rats (p < 0.05). The results of these experiments are shown in Fig. 5. Significant differences between control and treated non-I/R values were not observed (data not shown).
Outcomes of Experimental Design Strategy II (Part II Experiments)
Experiments conducted under part II of the present study evaluated the efficacy of post-ischemic treatment with α-MSH in ameliorating I/R injury. Part II experiments also assessed the significance of HO-1 in outcomes mediated by α-MSH. Major strategies for making the aforementioned determinations included post-ischemic administration of α-MSH at the onset of reperfusion and treatment of selected groups of animals with SnPP a potent inhibitor of HO-1 (Drummond and Kappas 1981).
Electroretinography
The outcome of part II ERG studies is shown in Fig. 6. Figure 6a demonstrates one representative ischemic ERG spike of each of the four treatment groups with showing actual voltage levels and time-course of ERG spikes observed in part II studies. ERG outcomes suggest three major trends with respect to effect of each treatment on retinal integrity: the data in Fig. 6 show that relative to waveforms recorded for nonischemic retinas (Control Baseline), I/R injury, and SnPP-mediated HO-1 inhibition decreased the amplitude and altered the waveform characteristics in ways indicative of degraded retinal tissue function. By contrast α-MSH treatment shifted retinal responses toward improved retinal function. Interestingly, administration of SnPP together with α-MSH did decrease but did not thoroughly abolish this protective effect of α-MSH.
Effects of SnPP and post-ischemic α-MSH treatment on ERG voltage profiles (a) and ERG b-waves (b) obtained in part II experiments (group II). Results are shown for five groups including: nonischemic retinas from vehicle-treated rats (Control Baseline) and I/R-injured retinas from vehicle- (Control Ischemia), α-MSH- (MSH Ischemia), SnPP + α-MSH- (SnPP + MSH Ischemia), and SnPP-treated rats (SnPP Ischemia). Shown on (a) are representative ERG spikes; shown on (b) are mean percentage values (relative to control baseline) for b waves measured in electroretinograms of the aforementioned groups. Horizontal lines indicate comparisons. The significance of comparisons is indicated as follows: ns not significant; *p < 0.05; **p < 0.01; ***p < 0.001
The effects of retinal I/R injury and post-ischemic treatments may be clearly visualized by ERG histogram data shown in Fig. 6b. Here, it can be seen that mean percentage of b waves relative to control baseline (i.e., effect of post-ischemic treatment) was 67.69 % of control baseline values in animals treated with 500 μg/kg α-MSH (p < 0.001 vs. control I/R). This value is even a little bit higher than what could be observed in outcomes of the part I experiments (i.e. effect of pre-ischemic treatment), which was 64.36 % of control baseline values in animals treated with 500 μg/kg α-MSH (p < 0.001 vs. control I/R; see Fig. 2). Mean percentage of b waves relative to control baseline measured in I/R-injured retinas from vehicle-treated rats (Control Ischemia) of second experimental studies were 33.44 %. Figures 2 and 6b allow clear comparison of b wave ratios in I/R-injured retinas from vehicle-treated vs. α-MSH-treated rats in parts I vs. II ERG experiments. Percentage of SnPP-treated I/R retinas were observed to be 19.76 % (p < 0.001 vs. control I/R). Dual-treatment (SnPP + MSH) significantly lowered the b wave percentages vs. MSH-only treatment (55.77 vs. 67.69 %; p < 0.01). However, percentage of SnPP + MSH-treated I/R retinas proved to be significantly higher than that of SnPP-only treatment (55.77 vs. 19.76 %; p < 0.001). Significant differences between control and treated non-I/R values were not observed (data not shown).
Measurement of Heme Oxygenase Activity
The outcome of HO activity measurement in ocular tissue of rats used for part II experiments is provided in Fig. 7. Tissue activity of the enzyme was amplified by I/R (119.58 % of control baseline), and even more by treatment of animals with 500 μg/kg α-MSH (159.42 %). Latter effect was diminished by combined administration of α-MSH with the HO-1 inhibitor SnPP (108.77 %). However, there was a slight difference between SnPP + MSH- and SnPP-only-treated groups (108.77 and 96.60 %, respectively). Nevertheless, the results of HO-activity measurements exhibit a variability of such magnitude as to diminish the statistical validity of the data. Significant differences between control and treated non-I/R values were also not observed (data not shown).
Relative HO activities in ocular tissue from eyes harvested in part II experiments (group II). Results are shown for five groups including: nonischemic retinas from vehicle-treated rats (Control Baseline) and I/R-injured retinas from vehicle- (Control Ischemia), α-MSH- (MSH Ischemia), SnPP + α-MSH- (SnPP + MSH Ischemia), and SnPP-treated rats (SnPP Ischemia). Activity of the enzyme in ocular tissue of an aforementioned group is shown as percentage of bilirubin production by a particular group relative to control baseline eye values with SEM
Discussion
The experiments conducted in part I of the present investigation examined the capacity of α-MSH to protect against I/R-induced retinal injury. In these studies, α-MSH was observed to significantly preserve functions of the eyes subjected to I/R injury. Evidence for this protective effect is provided by ERG experiments that demonstrated an α-MSH dose-dependent increase in I/R-damaged retinal b wave magnitude (Figs. 1 and 2). These results represent the first demonstration of α-MSH-mediated protection against I/R injury to the retina. The aforementioned outcomes are significant in the context of a February 2013 report describing the capacity of resveratrol, a plant polyphenol, to therapeutically increase b wave amplitude and ameliorate the effects of retinal ischemia induced by high intraocular pressure through a mechanism that prominently includes upregulation of HO-1 (Liu et al. 2013). Present study demonstrate that HO-1 activity, although it is not an exclusive component of α-MSH-mediated protection of retinal tissue, increases correlating with α-MSH administration as shown in Fig. 7.
HO-1 expression in injured tissue is a highly conserved adaptive response that is observed in many tissues in a very diverse range of organisms (Haines et al. 2012). Previous work by the authors to develop therapeutic potential of this enzyme show that upregulation of HO-1 with an inducer mediates powerful therapeutic effects in vivo (Bak et al. 2006; Bak et al. 2011), further supporting the potential clinical application of agents that upregulate HO-1.
The activity of HO-1 is increased in response to a wide variety of stressors, including oxidative and inflammatory insults (Haines et al. 2012), as well as metabolic and hemodynamic factors such as high glucose (Mahmoud et al. 2013). Nevertheless, in most cases, the pathophysiological activation of HO-1 results only in a transient or marginal increase of HO-1 activity that falls below the threshold necessary to activate downstream signaling components of the HO system at levels capable of achieving significant remission of serious inflammatory pathologies (Mahmoud et al. 2013). Thus, strategies for use of HO-1 as definitive prophylaxis or treatment for retinopathies and other diseases are expected to increasingly make use of pharmacological agents capable of increasing expression and activity of the enzyme. Previously, the authors have demonstrated that sour cherry kernel extract is capable of protecting rat retinas against I/R injury in vivo through activation of HO-1 (Szabo et al. 2004). The results of Western blot analysis of the present study revealed significantly increased expression of HO-1 in retinal tissue of I/R-injured eyes from 500 μg/kg α-MSH treated rats in comparison to expression of the enzyme in I/R-injured eyes from vehicle-treated animals (Fig. 5). This outcome suggests that HO-1 may be upregulated by α-MSH in ways that might be significantly augmented by its concurrent pharmacological induction as a therapeutic strategy. α-MSH-mediated increase of expression of HO-1 in retinal tissue, is not an unexpected observation. Moreover, results shown in Fig. 7 of the present study demonstrate that HO-1 activity correlates with the therapeutic effect of α-MSH, suggesting that inducers of HO-1 may exhibit additive and perhaps synergistic therapeutic effects when administered concurrently with α-MSH.
Histological examination of tissue in the present study revealed that α-MSH-treated animals exhibited significantly reduced retinal edema following I/R injury (Fig. 3). This finding is also potentially significant in the context of the role of HO-1 in protection against retinal edema. Related studies demonstrate that resveratrol-induced HO-1 upregulation is observed to protect against retinal damage (Liu et al. 2013). These results may contribute to development of novel strategies for alleviation of retinal edema in ocular disorders.
This study also provides EM demonstrations of suppression of I/R-induced damage to mitochondria of inner retinal cells by α-MSH at subcellular level (Fig. 4), which is also a novel result.
The experiments conducted in part II of the present investigation examined the capacity of post-ischemic administration of α-MSH to protect against I/R-induced retinal injury. A corollary objective was to suggest whether non-HO-1-dependent pathways might also contribute to protective effects of α-MSH.
The results of the part II ERG studies reveal that the amplitude of waveforms, which is a function of healthy retinal function, was decreased by I/R injury but, most strikingly, increased by post-ischemic α-MSH treatment (Fig. 6). At the same time, eyes from rats treated with the HO-1 inhibitor SnPP and α-MSH together exhibited reduced ERG waveform amplitude. Also, tissue HO-1 activity correlated with waveform amplitudes (Fig. 7). Taken together, clear correlation between α-MSH, mitigation of I/R injury to retinas, and HO-1 involvement suggest that α-MSH may mediate protection from I/R injury substantially via an HO-1-dependent pathway. Results presented here cannot rule out partial involvement of some other, as-yet unidentified non-HO-1-dependent mechanisms as well. Exploration of this possibility is the focus of future research by the authors. Avenues of investigation are suggested by the work by other investigators, showing that α-MSH has anti-cytokine activity, inhibits proinflammatory protein expression, decreases fever, and modulates neuroimmune activity (Macaluso et al. 1994; Delgado et al. 1998).
The present study provides the first demonstration of the efficacy of α-MSH in protecting against I/R-induced retinal damage when administered either before or after an ischemic event. Moreover, the ability of this hormone to protect the retina following a period of ischemia lends strength to the hypothesis that α-MSH expression is a major physiological countermeasure to a wide range of stressors, developed early in vertebrate evolution and conserved as an important survival trait. The observation that post-ischemic administration of α-MSH mediates protective effects in the same range as pre-ischemic treatment is encouraging from the perspective of its potential therapeutic use as well.
Results of the present study validate the hypothesis that α-MSH mitigates the severity of I/R-induced retinal injury and reinforce evidence for possible involvement of HO-1. Of particular interest is the capacity of α-MSH to reconstitute the function of retinal tissue when administered following a period of ischemia. This finding suggests that α-MSH may have a very wide range of uses in the prevention of I/R-mediated pathologies.
Abbreviations
- α-MSH:
-
Alpha-melanocyte-stimulating hormone
- ERG:
-
Electroretinography
- HO-1:
-
Heme oxygenase-1
- I/R:
-
Ischemia/reperfusion; control baseline = nonischemic vehicle-treated control
- SnPP:
-
Sn-protoporphyrin IX
References
Agarwal R, Gupta SK, Agarwal P, Saxena R, Agrawal SS (2009) Current concepts in the pathophysiology of glaucoma. Indian J Ophthalmol 57:257–266
Bak I, Lekli I, Juhasz B et al (2006) Cardioprotective mechanisms of Prunus cerasus (sour cherry) seed extract against ischemia–reperfusion-induced damage in isolated rat hearts. Am J Physiol Heart Circ Physiol 291:H1329–1336
Bak I, Czompa A, Csepanyi E et al (2011) Evaluation of systemic and dermal toxicity and dermal photoprotection by sour cherry kernels. Phytother Res 25:1714–1720
Bazzani C, Guarini S, Botticelli AR et al (2001) Protective effect of melanocortin peptides in rat myocardial ischemia. J Pharmacol Exp Ther 297:1082–1087
Chiao H, Kohda Y, McLeroy P, Craig L, Housini I, Star RA (1997) Alpha-melanocyte-stimulating hormone protects against renal injury after ischemia in mice and rats. J Clin Invest 99:1165–1172
Csonka C, Varga E, Kovacs P et al (1999) Heme oxygenase and cardiac function in ischemic/reperfused rat hearts. Free Radic Biol Med 27:119–126
Curtis TM, Gardiner TA, Stitt AW (2009) Microvascular lesions of diabetic retinopathy: clues towards understanding pathogenesis? Eye (Lond) 23:1496–1508
Delgado R, Carlin A, Airaghi L et al (1998) Melanocortin peptides inhibit production of proinflammatory cytokines and nitric oxide by activated microglia. J Leukoc Biol 63:740–745
Drummond GS, Kappas A (1981) Prevention of neonatal hyperbilirubinemia by tin protoporphyrin IX, a potent competitive inhibitor of heme oxidation. Proc Natl Acad Sci U S A 78:6466–6470
Forslin AS, Spulber S, Popescu LM et al (2006) Alpha-melanocyte-stimulating hormone is neuroprotective in rat global cerebral ischemia. Neuropeptides 40:65–75
Haines DD, Lekli I, Teissier P, Bak I, Tosaki A (2012) Role of haeme oxygenase-1 in resolution of oxidative stress-related pathologies: focus on cardiovascular, lung, neurological and kidney disorders. Acta Physiol (Oxf) 204:487–501
Jonas J, Paques M, Mones J, Glacet-Bernard A (2010) Retinal vein occlusions. Dev Ophthalmol 47:111–135
Juarez CP, Tso MO, van Heuven WA, Hayreh MS, Hayreh SS (1986) Experimental retinal vascular occlusion. III. An ultrastructural study of simultaneous occlusion of central retinal vein and artery. Int Ophthalmol 9:89–101
Juhasz B, Varga B, Czompa A et al (2011) Postischemic cardiac recovery in heme oxygenase-1 transgenic ischemic/reperfused mouse myocardium. J Cell Mol Med 15:1973–1982
Kokot A, Sindrilaru A, Schiller M et al (2009) alpha-melanocyte-stimulating hormone suppresses bleomycin-induced collagen synthesis and reduces tissue fibrosis in a mouse model of scleroderma: melanocortin peptides as a novel treatment strategy for scleroderma? Arthritis Rheum 60:592–603
Lam CW, Getting SJ, Perretti M (2005) In vitro and in vivo induction of heme oxygenase 1 in mouse macrophages following melanocortin receptor activation. J Immunol 174:2297–2304
Lipton JM, Ceriani G, Macaluso A et al (1994) Antiinflammatory effects of the neuropeptide alpha-MSH in acute, chronic, and systemic inflammation. Ann N Y Acad Sci 741:137–148
Liu XQ, Wu BJ, Pan WH et al (2013) Resveratrol mitigates rat retinal ischemic injury: the roles of matrix metalloproteinase-9, inducible nitric oxide, and heme oxygenase-1. J Ocul Pharmacol Ther 29:33–40
Macaluso A, McCoy D, Ceriani G et al (1994) Antiinflammatory influences of alpha-MSH molecules: central neurogenic and peripheral actions. J Neurosci 14:2377–2382
Mahmoud F. F., Al-Awadhi R., Haines D. D., et al. (2013) Sour cherry seed kernel extract increases heme oxygenase-1 expression and decreases representation of CD3+ TNF-alpha+ and CD3+ IL-8+ subpopulations in peripheral blood leukocyte cultures from type 2 diabetes patients. Phytother Res (in press)
Morton GJ, Cummings DE, Baskin DG, Barsh GS, Schwartz MW (2006) Central nervous system control of food intake and body weight. Nature 443:289–295
Shadiack AM, Sharma SD, Earle DC, Spana C, Hallam TJ (2007) Melanocortins in the treatment of male and female sexual dysfunction. Curr Top Med Chem 7:1137–1144
Shakib M, Ashton N (1966) II. Ultrastructural changes in focal retinal ischaemia. Br J Ophthalmol 50:325–384
Szabo ME, Droy-Lefaix MT, Doly M, Carre C, Braquet P (1991) Ischemia and reperfusion-induced histologic changes in the rat retina. Demonstration of a free radical-mediated mechanism. Invest Ophthalmol Vis Sci 32:1471–1478
Szabo ME, Gallyas E, Bak I et al (2004) Heme oxygenase-1-related carbon monoxide and flavonoids in ischemic/reperfused rat retina. Invest Ophthalmol Vis Sci 45:3727–3732
Tenhunen R, Marver HS, Schmid R (1968) The enzymatic conversion of heme to bilirubin by microsomal heme oxygenase. Proc Natl Acad Sci U S A 61:748–755
Tsatmali M, Ancans J, Thody AJ (2002) Melanocyte function and its control by melanocortin peptides. J Histochem Cytochem 50:125–133
Varga B, Szabadfi K, Kiss P et al (2011) PACAP improves functional outcome in excitotoxic retinal lesion: An electroretinographic study. J Mol Neurosci 43:44–50
Vecsernyes M, Juhasz B, Der P et al (2003) The administration of alpha-melanocyte-stimulating hormone protects the ischemic/reperfused myocardium. Eur J Pharmacol 470:177–183
Zou L, Sato N, Attuwaybi BO, Kone BC (2003) Delayed administration of alpha-melanocyte-stimulating hormone or combined therapy with BAY 11-7085 protects against gut ischemia–reperfusion injury. Shock 20:469–475
Acknowledgments
This study was supported by grants from OTKA (78223 and 104017), Richter Gedeon Foundation, and in part by the project of New Hungary Development Plan, co-financed by the European Union and the European Social Fund of TAMOP-4.2.1/B-09/1/KONV-2010-0007, TAMOP-4.2.2./B-10/1-2010-0024, and TAMOP-4.2.2.A-11/1/KONV-2012-0045. The research took place under the project with identification number of TÁMOP 4.2.4.A/2-11-1-2012-0001 entitled “National Excellence Program—Convergence program for elaboration and operation of support-system sponsoring Hungarian students and researchers,” funded by the European Union, co-financed by the European Social Fund.
Author information
Authors and Affiliations
Corresponding author
Rights and permissions
Open Access This article is distributed under the terms of the Creative Commons Attribution License which permits any use, distribution, and reproduction in any medium, provided the original author(s) and the source are credited.
About this article
Cite this article
Varga, B., Gesztelyi, R., Bombicz, M. et al. Protective Effect of Alpha-Melanocyte-Stimulating Hormone (α-MSH) on the Recovery of Ischemia/Reperfusion (I/R)-Induced Retinal Damage in A Rat Model. J Mol Neurosci 50, 558–570 (2013). https://doi.org/10.1007/s12031-013-9998-3
Received:
Accepted:
Published:
Issue Date:
DOI: https://doi.org/10.1007/s12031-013-9998-3