Abstract
Background
Endovascular therapy (EVT) for severe cerebral venous sinus thrombosis (CVST) is controversial in terms of indication and clinical benefit. The impact of delay of EVT on functional recovery is unclear. This study aimed to investigate the effect of early versus late initiation of EVT in severe CVST.
Methods
From prospective EVT and CVST registries, patients with CVST diagnosed between January 2010 and December 2022 were retrospectively identified for this multicenter collaboration. EVT was considered in severe CVST with features prone to a poor prognosis. We compared early (< 24 h) with late (> 24 h) initiation of EVT after the presentation in the emergency department and subsequent CVST diagnosis. Outcome parameters included functional independence (modified Rankin Scale [mRS] score 0–2) at 90 days, mRS score at discharge, in-hospital mortality, and mortality at 3 months.
Results
Of 363 patients with CVST, 45 (12.4%; 31 [early EVT] vs. 14 [late EVT]) were included in this study. We found a higher proportion of patients with functional independence at 3 months among early versus late EVT (66.7% vs. 27.3%; odds ratio [OR] 5.3; 95% confidence interval 1.02–25; p = 0.036). In multivariate logistic regression, late EVT was inversely correlated with functional independence (OR 0.17 [0.04–0.83]; p = 0.011). The mortality rate was 16.7% versus 36.4% (mRS 6 at 3 months, OR 0.34, 95% confidence interval 0.07–1.75; p = 0.217) at 90 days for early versus late EVT.
Conclusions
We observed a higher rate of functional independence in patients with early EVT. These preliminary findings must be confirmed in subsequent randomized controlled trials evaluating a “time-is-brain” paradigm for EVT in CVST.
Similar content being viewed by others
Avoid common mistakes on your manuscript.
Introduction
Cerebral venous sinus thrombosis (CVST) is a rare but potentially life-threatening condition associated with intracerebral hemorrhage (ICH), cerebral venous infarction, and brain edema [1,2,3] CVST accounts for approximately 0.5–1% of all strokes, with a global incidence of 1.32 per 100,000 person-years, and appears to be more common in children, young adults, and women [1, 3]. In recent years, increased incidence rates have been observed as both coronavirus disease-2019 adenoviral-based vaccinations and the coronavirus disease-2019 infection itself seem to facilitate the development of CVST [4, 5].
CVST prognosis is variable, with approximately 80% of patients regaining functional independence [1,2,3, 6, 7]. Yet, dependency rates are estimated to be around 15% of cases, with a case-specific mortality rate between 4 and 10% [1, 6, 7]. Treatment strategies include early anticoagulation with unfractionated or low-molecular-weight heparin even in cases of ICH [8, 9]. Despite a rapid treatment initiation, several patients undergo clinical deterioration during the course of the disease [10, 11]. Endovascular therapy (EVT) was suggested in to improve clinical outcomes in this specific patient population [12,13,14,15]. Results from the only published randomized controlled trial for EVT in CVST revealed that EVT provided no benefit over standard care [16]. However, because of sample size limitations, the authors could not exclude potentially relevant treatment effects either overall or in specific subgroups. In selected cases of severe CVST, EVT remained a therapeutic option as part of a rescue strategy [16,17,18].
Ischemic stroke studies demonstrated that the immediate implementation of recanalization therapies leads to superior patient outcomes and improved survival rates [19,20,21,22]. By contrast, the impact of time in patients diagnosed with acute CVST remains unclear. This retrospective observational study aimed to determine the impact of early versus late initiation of EVT in patients presenting with severe CVST. We hypothesized that early initiation of EVT (within 24 h of hospital admission and CVST diagnosis) will lead to reduced mortality and increased functional independence.
Methods
Study Design
This was a multicenter retrospective observational cohort study analyzing data from two comprehensive stroke centers (Neurocenter, Klinikum Stuttgart, Stuttgart, Germany, and Department of Neurology, Inselspital, Bern University Hospital and University of Bern, Bern, Switzerland). This study was approved by the local institutional review boards (Ethics Commission of the State Medical Association of Baden-Württemberg [F-2012-077]; Kantonale Ethikkommission Bern [231/14]). Additional approval and patient consent was required for inclusion in the EVT registry (Stuttgart). The study was conducted in accordance with the Declaration of Helsinki. The Strengthening the Reporting of Observational Studies in Epidemiology guidelines were used to ensure appropriate reporting of the findings from this retrospective observational study [23].
Study Population
Consecutive patients diagnosed with CVST of any etiology, evaluated by digital subtraction angiography (DSA), and that required EVT treatment between January 2010 and December 2022 were identified retrospectively from an ongoing prospective single-center EVT registry (Stuttgart) and the national stroke registry (Swiss Stroke Registry, Bern). The Swiss Stroke Registry is an obligatory registry prospectively including all patients with stroke (ischemic stroke, ICH, and CVST). Within established neurovascular networks, patients could be diagnosed and treated at the respective stroke center, or they might have been transferred from surrounding hospitals for EVT or neurointensive care [24]. There were no standard operating procedures declaring EVT mandatory in certain predefined situations. Treatment decisions were made on a case-by-case basis by an interdisciplinary team (neurology, interventional neuroradiology, and neurosurgery). In general, EVT was considered in patients who presented with a suspected poor prognosis (coma with a Glasgow Coma Scale [GCS] score < 9, ICH, involvement of deep cerebral veins, large thrombus load, and/or rapid clinical deterioration before EVT despite adequate anticoagulation therapy) as a rescue strategy. The presence of these clinical factors alone did not facilitate the decision to perform early or late EVT. This decision was made by the treatment team (emergency department, stroke unit, neurointensive care, interventional neuroradiology, and neurosurgery), required an interdisciplinary consultation and was based on course of the disease (i.e., slow or rapid deterioration), additional imaging findings (e.g., brain edema, venous infarction), and capacities. Various endovascular strategies (e.g., aspiration or stent retriever thrombectomy, stent placement, percutaneous transluminal angioplasty, rheolytic thrombectomy, or thrombus fragmentation) were used based on the decision of the interventional neuroradiologist. Stent placement was considered an option in cases of repeated and/or complete reocclusion. Strategies could be adapted and combined during the course of the procedure. All patients with confirmed CVST were initially treated with continuous unfractionated heparin (bolus; anti-Xa-activity controlled [therapeutic range: 0.3–0.7 IU/ml]) followed by either unfractionated or low-molecular weight heparin (after EVT). In cases of stent placement, an additional dual platelet aggregation inhibition was installed (aspirin at 100 mg per day plus clopidogrel at 75 mg per day or ticagrelor at 90 mg twice daily). If the patient underwent EVT within the first 24 h of diagnosis, we considered this approach as first-line rescue treatment, given the limited time interval between the initiation of medical therapy and the procedure.
Patients were eligible for further analysis if the following criteria were met: (1) the patient was hospitalized with acute symptoms that could be directly attributed to CVST; (2) CVST was revealed by acute cerebral imaging (magnetic resonance imaging or computed tomography with contrast for those with contraindications); (3) documentation of a modified Rankin Scale (mRS) score at discharge and/or during follow-up 3 months after the index event. Because CVST predominantly affects younger patient populations, we did not apply a lower age limit. Exclusion criteria included (1) performance of a DSA study that did not lead to a subsequent EVT (e.g., chronic CVST or cerebral sinus stenosis without thrombosis); (2) incidental detection of a chronic CVST by DSA (which was performed due to other conditions such as arteriovenous malformations); and (3) lack of informed consent.
To evaluate the impact of time (i.e., the time elapsed between emergency consultation/hospitalization and the initiation of treatment), patients were subdivided into two groups: (1) patients who underwent treatment within 24 h (early EVT) and (2) patients who underwent treatment more than 24 h after hospitalization and diagnosis of CVST (late EVT). Because there were no data on the impact of earlier versus later EVT treatment in this patient population, we decided to use the assumed time to treatment initiation in the only published randomized controlled trial on EVT in CVST (Thrombolysis or Anticoagulation for Cerebral Venous Thrombosis [TO-ACT]) as a cutoff [16]. Given an interquartile range (IQR) for the time from diagnosis to randomization between 0 and 1 days (patients had to be randomized within 24 h after CVST diagnosis), and a median time from randomization to EVT of 4.5 h (278 [IQR 105–724] minutes) plus an unknown time from emergency consultation until final diagnosis, the assumed time to treatment initiation would be approximately 24 h.
Outcome parameters included functional independence (mRS score 0–2) at 90 days, mortality (mRS 6) at 3 months, in-hospital mortality, and functional independence (mRS score 0–2) at discharge.
Data Collection
Baseline characteristics (age, sex, medical history, symptom onset, physical examination, and mRS score) were extracted from the respective registries (PB and VH; both masked for the time elapsed between emergency consultation and EVT) and—if required—retrospectively completed according to emergency department admission notes, referral papers, and/or discharge letters. For the scope of this article, we distinguished between coma (GCS < 9) and somnolence/stupor (GCS 9–14). Imaging data were stored and analyzed in our picture archiving and communications system. We used the reports of the original read in order to describe imaging findings, such as ICH or subarachnoid hemorrhage (SAH), venous congestion, venous infarction, or thrombus load, as well as the number and location of the involved sinus(es). These findings were acquired retrospectively and verified in an additional read prior to this analysis (VH). Partial recanalization after EVT was defined as recanalization of one or more affected sinuses (but not all; residual thrombus material). In both centers, outcome data were recorded prospectively during scheduled follow-up consultations. A trained and specialized study nurse (trained in neuroradiology and neurology) collected the 3-month follow-up data on functional outcomes (mRS) and mortality via telephone calls (Stuttgart). Follow-up visits were scheduled 3 months after the index event in the outpatient department (Bern).
Statistical Analysis
Numerical baseline characteristics were described using the median (± IQR) or mean (± standard deviation [SD]). Frequencies were used to present categorical parameters. Group comparisons of categorical parameters were performed using the Fisher exact t-test or the χ2 test. The Kruskal–Wallis test or the Mann–Whitney U-test were applied as appropriate to evaluate numerical (outcome) parameters. The comparison of outcome variables was reported using odds ratios (ORs) and 95% confidence intervals (CIs) with adjustment in case of significant differences in baseline characteristics. A p value of < 0.05 was considered statistically significant. Statistical analyses were performed using STATA/IC 13.1 for Windows (StataCorp, College Station, TX).
Multivariate logistic regression was performed in order to determine factors associated with good functional outcome. Because of sample size restrictions, we could only include a small number of covariables in the multivariate logistic regression. Besides time to EVT, we predefined coma and any hemorrhage (ICH and SAH) as the only covariables. Both were previously shown to be predictors of severity [25]. Because we expected a low absolute number of death cases, no multivariate analysis regarding mortality was conducted.
Results
Between January 2010 and December 2022, 363 patients were diagnosed with CVST. Of these, 66 patients underwent DSA (18.2%). Twenty-one patients did not meet the criteria for inclusion in this retrospective observational study: 19 patients did not undergo EVT or present with CVST as an incidental finding, and two patients did not provide informed consent (Fig. 1). We identified 45 patients (12.4%) eligible for further analysis; 31 patients in the early EVT group (underwent the procedure at < 24 h after hospitalization) and 14 patients in the late EVT group (underwent the procedure > 24 h after hospitalization) (Fig. 1). mRS scores at 90 days were available for 41 patients (30 in the early EVT group and 11 in the late EVT group).
Descriptive baseline patient characteristics, including information on CVST etiology, endovascular procedures and postprocedural medication, are shown in Table S1. There were no significant differences between the early EVT group and the late EVT group, including seizures and/or focal neurological deficits at the time of presentation (74.1% vs. 71.4%; p = 0.409), any impaired consciousness (somnolence/stupor or coma; 54.8% vs. 42.9%; p = 0.530), location and the number of affected sinuses (p = 0.166), deep vein involvement (25.8% vs. 7.1%; p = 0.236), or detection of ICH on initial imaging studies (51.7% vs. 71.4%; p = 0.329; see Table 1). The mean (SD) duration of the hospital stay was 12 (7) days for early EVT versus 16 (9) days for late EVT (p = 0.280; excluding in-hospital mortality).
The average time to treatment (emergency consultation/hospitalization to EVT; mean ± SD) was 24.9 ± 23.8 h. The average time elapsed between hospitalization and EVT was 9.8 ± 7.6 h for patients who underwent early and 58.1 ± 64.8 h for those who underwent late EVT (p < 0.001). Neurological deterioration (reduced level of consciousness, development of focal neurological deficits) was reported in 12.9% (n = 4) of those in the early treatment group and in 42.8% (n = 6) of those in the late treatment group (p = 0.149).
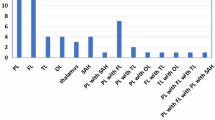
With respect to functional independence, 20/30 (66.7%) patients in the early versus 3/11 (27.3%) in the late group experienced a good functional outcome (mRS 0–2; OR 5.3; 95% CI, 1.02–25; p = 0.036; Table 2) at 90 days. There was no significant difference in functional independence (mRS 0–2) at discharge (15/31 [48.4%] vs. 4/14 [28.6%]; OR 2.3; 95% CI 0.6–9.1; p = 0.330). Our analysis revealed no significant changes in both 90-day mortality (5/30 [16.7%] in the early EVT group vs. 4/11 [36.4%] in the late EVT group; OR 0.35; 95% CI 0.07–1.75; p = 0.217) and in-hospital mortality (4/31 [12.9%] in early EVT vs. 4/14 [28.6%] in late EVT; OR 0.370; 95% CI 0.08–1.77; p = 0.370). The overall mortality rate in our cohort was 21.9% (n = 9). Outcome comparison between the two participating centers and time metrics are shown in the online supplement (supplemental material; Table S2).
In multivariate logistic regression, there was a negative association of late EVT (treatment after 24 h; OR 0.17 [0.04–0.83]; p = 0.011) and functional independence at three months (Table 3). The same was observed for any baseline hemorrhage (ICH and/or SAH; OR 0.14 [0.03–0.83]; p = 0.028) but not for coma at initial presentation (OR 0.30 [0.07–1.26]; p = 0.099). These results did not change when patients with traumatic CVST were removed from the analysis (treatment after 24 h: OR 0.16 [0.03–0.72], p = 0.017; baseline hemorrhage: OR 0.18 [0.04–0.90], p = 0.037; coma: OR 0.42 [0.07–1.36], p = 0.122).
In term of procedural complications, we observed one postinterventional subdural hematoma in the early EVT group. Follow-up DSA (n = 18) detected one dural arteriovenous fistula most likely to be attributable to the intervention (early EVT).
Discussion
The main finding of this retrospective multicenter cohort study indicates a significant increase in functional independence after early versus late EVT (66.7% vs. 27.3%) in patients with severe CVST prone to a poor prognosis. We observed a nonsignificant but potentially clinically relevant reduction in mortality (16.7% vs. 36.4%) for early EVT.
To the best of our knowledge, the question regarding a potential impact of time (meaning the time elapsed between emergency consultation/diagnosis of CVST and initiation of EVT) on functional outcomes after CVST is unanswered. Randomization in the TO-ACT trial had to occur within 24 h (from CVST diagnosis) plus an additional 278 min (median; IQR 105–724 min) from randomization to EVT [16]. There was no information on the time from emergency consultation until CVST diagnosis. Given the severity of symptoms in TO-ACT, it can be assumed that CVST was diagnosed early and within the first hours. Jedi et al. [26] reported the time from hospitalization to EVT (with a range between 0 and 7 days) in a single-center cohort without providing further analyses on a potential impact on functional outcomes. Patients included in our study were treated early (on average 24.9 h after emergency consultation). Nonetheless, there was a notable difference between the early EVT group (average interval of 9.8 h) and the late EVT group (average interval of 58.1 h).
We observed an increase in the frequency of good functional outcomes (66.7% vs. 27.3%; p = 0.036) for early EVT. This was regardless of the fraction of patients with features suggesting poor prognosis (e.g., impaired consciousness, 54.8% in the early EVT group vs. 42.9%; deep vein involvement, 25.8% vs. 7.1% in the late EVT group, or large thrombus load, 25.8% vs. 14.3% for late EVT). The effect of time remained significant in the multivariate logistic regression model.
Clinical deterioration prior to the intervention (e.g., a decrease in the level of consciousness, development of focal neurological symptoms) was reported more frequently in late (42.8%) as opposed to early EVT (12.9%). Although no correlation has been established in the literature, these results might be attributable to the effect of early recanalization (prior to any further brain damage). Early recanalization is assumed to be associated with less parenchymal injury and an immediate improvement of nonhemorrhagic brain damage [27]. Additional effects on long-term functional outcomes seem to be driven by an early recanalization (prior to the development of any secondary deterioration) [27, 28]. We observed a similar effect of early recanalization. Patients with late EVT did not improve over time (mRS 0–2 at discharge: 28.6%; mRS 0–2 at 3 months: 27.3%). In the early EVT group, patients did improve between discharge (48.4% with mRS 0–2) and follow-up after 3 months (66.7% with mRS 0–2).
At initial presentation, our patient population was severely affected. This may have prompted the decision to perform early EVT. A considerable number of patients presented with clinical or radiological risk factors that have been associated with a poor prognosis [10]. In addition, our patient cohort was slightly older with a higher percentage of male patients (both associated with poor functional outcomes) as compared with the literature [3, 10, 16]. This resulted in an overall mortality rate of 21.9%. Although in line with a recent case series, this is higher compared with meta-analysis data (including a higher percentage of less affected patients) [26, 29]. Although mortality rates in early EVT (16.7%) and TO-ACT (12%) were found to be comparable, increased mortality rates in our study seem to be attributable to the late EVT group (36.4%) [16].
Despite being one of the largest studies to evaluate EVT in CVST, sample size restrictions leading to a potential underestimation or misinterpretation of true treatment effects are the main limitation. Because of the retrospective study design, all associated biases apply. Based on the high percentage of patients with CVST who underwent EVT, we assume that most of the severely affected patients were provided with this treatment strategy. However, we have no outcome data on severely affected patients without EVT. Clinical deterioration prior to EVT was more frequent in the late EVT group. Although we believe that this was due to the course of the disease, together with other factors such as the presence of ICH or other medical reasons, it might have prompted the decision to perform EVT in this group. The difference in the time from emergency consultation until EVT (especially in late EVT) suggests variation between both centers (e.g., in terms of timing of the intervention). In addition, there was an imbalance in the number of patients included per center with the majority of patients (85%) being treated in one center (Stuttgart). Finally, there is a lack of information regarding the time of initial symptom onset (as a majority of patients presented with prior subacute headache lasting for several days). In most cases, the only reliable time point was the time of hospitalization. Because of the severity of symptoms, the time of the emergency department consultation most likely reflects either the onset of symptoms or an acute deterioration. Early EVT may not be early in the course of the disease, but it might be early after an acute deterioration immediately before or during hospitalization that is associated with clinical symptoms prone to a poor prognosis.
In conclusion, these preliminary results suggest a higher frequency of functional independence in early EVT as compared to late EVT in patients with severe CVST. In addition, early EVT may lead to a clinically relevant reduction in mortality. The recognition of a time-is-brain paradigm might be warranted when considering EVT for CVST in selected patients and needs to be a focus of future randomized controlled trials.
References
Ropper AH, Klein JP. Cerebral venous thrombosis. N Engl J Med. 2021;385(1):59–64.
Bousser M, Ferro JM. Cerebral venous thrombosis: an update. Lancet Neurol. 2007;6(2):162–70.
Coutinho JM, Zuurbier SM, Aramideh M, Stam J. The incidence of cerebral venous thrombosis: a cross-sectional study. Stroke. 2012;43:3375–7.
Al-Mufti F, Amuluru K, Sahni R, Bekelis K, Karimi R, Ogulnick J, et al. Cerebral venous thrombosis in COVID-19: a New York metropolitan cohort study. AJNR Am J Neuroradiol. 2021;42(7):1196–200.
Jaiswal V, Nepal G, Dijamco P, Ishak A, Dagar M, Sarfraz Z, et al. Cerebral venous sinus thrombosis following COVID-19 vaccination: a systematic review. J Prim Care Commun ity Health. 2022;13:21501319221074450.
Coutinho JM, Zuurbier SM, Stam J. Declining mortality in cerebral venous thrombosis: a systematic review. Stroke. 2014;45(5):1338–41.
Devianne J, Legris N, Crassard I, Bellesme C, Bejot Y, Guidoux C, et al. Epidemiology, clinical features, and outcome in a cohort of adolescents with cerebral venous thrombosis. Neurology. 2021;97(19):e1920–32.
Einhäupl KM, Villringer A, Meister W, Mehraein S, Garner C, Pellkofer M, et al. Heparin treatment in sinus venous thrombosis. Lancet. 1991;338(8767):597–600.
de Bruijn SFTM, Stam J. Randomized, placebo-controlled trial of anticoagulant treatment with low-molecular-weight heparin for cerebral sinus thrombosis. Stroke. 1999;30(3):484–8.
Ferro JM, Canhão P, Stam J, Bousser MG, Barinagarrementeria F, ISCVT Investigators. Prognosis of cerebral vein and dural sinus thrombosis results of the international study on cerebral vein and dural sinus thrombosis (ISCVT). Stroke. 2004;35(3):664–70.
Lee SK, Mokin M, Hetts SW, Fifi JT, Bousser MG, Fraser JF, Society of NeuroInterventional Surgery. Current endovascular strategies for cerebral venous thrombosis: Report of the SNIS Standards and Guidelines Committee. J Neurointerv Surg. 2018;10(8):803–10.
Andersen TH, Hansen K, Truelsen T, Cronqvist M, Stavngaard T, Cortsen ME, et al. Endovascular treatment for cerebral venous sinus thrombosis—a single center study. Br J Neurosurg. 2020;35(3):259–65.
Yang J, Wang H, Chen Y, Qiu M, Zhang B, Chen Z. Balloon-assisted thrombectomy and intrasinus urokinase thrombolysis for severe cerebral venous sinus thrombosis. Front Neurol. 2021;12:735540.
Stam J, Majoie CB, van Delden OM, van Lienden KP, Reekers JA. Endovascular thrombectomy and thrombolysis for severe cerebral sinus thrombosis: a prospective study. Stroke. 2008;39(5):1487–90.
Lu G, Shin JH, Song Y, Lee DH. Stenting of symptomatic lateral sinus thrombosis refractory to mechanical thrombectomy. Interv Neuroradiol. 2019;25(6):714–20.
Coutinho JM, Zuurbier SM, Bousser MG, Ji X, Canhão P, Roos YB, et al. Effect of endovascular treatment with medical management vs standard care on severe cerebral venous thrombosis: the TO-ACT randomized clinical trial. JAMA Neurol. 2020;77(8):966–73.
Saposnik G, Barinagarrementeria F, Brown RD Jr, Bushnell CD, Cucchiara B, Cushman M, et al. American Heart Association Stroke Council and the Council on Epidemiology and Prevention.: Diagnosis and management of cerebral venous thrombosis: a statement for healthcare professionals from the American Heart Association/American Stroke Association. Stroke. 2011;42(4):1158–92.
Bücke P, Hellstern V, Cimpoca A, Cohen JE, Horvath T, Ganslandt O, et al. Endovascular treatment of intracranial vein and venous sinus thrombosis—a systematic review. J Clin Med. 2022;11(14):4215.
Berkhemer OA, Fransen PS, Beumer D, van den Berg LA, Lingsma HF, Yoo AJ, et al. A randomized trial of intraarterial treatment for acute ischemic stroke. N Engl J Med. 2015;372(1):11–20.
Albers GW, Marks MP, Kemp S, Christensen S, Tsai JP, Ortega-Gutierrez S, et al. Thrombectomy for stroke at 6 to 16 hours with selection by perfusion imaging. N Engl J Med. 2018;378(8):708–18.
Bücke P, Pérez MA, Hellstern V, AlMatter M, Bäzner H, Henkes H. Endovascular thrombectomy in wake-up stroke and stroke with unknown symptom onset. AJNR Am J Neuroradiol. 2018;39(3):494–9.
Turc G, Bhogal P, Fischer U, Khatri P, Lobotesis K, et al. European Stroke Organisation (ESO)- European Society for Minimally Invasive Neurological Therapy (ESMINT) guidelines on mechanical thrombectomy in acute ischemic stroke. J Neurointerv Surg. 2019;11(6):535–8.
von Elm E, Altman DG, Egger M, Pocock SJ, Gøtzsche PC, Vandenbroucke JP. The Strengthening the Reporting of Observational Studies in Epidemiology (STROBE) statement: guidelines for reporting observational studies. J Clin Epidemiol. 2008;61(4):344–9.
Bücke P, Pérez MA, Schmid E, Nolte CH, Bäzner H, Henkes H. Endovascular thrombectomy in acute ischemic stroke: outcome in referred versus directly admitted patients. Clin Neuroradiol. 2018;28(2):235–44.
Lindgren E, Krzywicka K, de Winter MA, Sánchez Van Kammen M, Heldner MR, Hiltunen S, et al. A scoring tool to predict mortality and dependency after cerebral venous thrombosis. Eur J Neurol. 2023;30(8):2305–14.
Jedi F, Dethlefs G, Hauser TK, Hennersdorf F, Mengel A, Ernemann U, et al. Mechanical thrombectomy in cerebral venous sinus thrombosis: reports of a retrospective single-center study. J Clin Med. 2022;11(21):6381.
Aguiar de Sousa D, Lucas- Neto L, Arauz A, Sousa AL, Gabriel D, Correia M, et al. Early recanalization in patients with cerebral venous thrombosis treated with anticoagulation. Stroke. 2020;51(4):1174–81.
Rezoagli E, Martinelli I, Poli D, Scoditti U, Passamonti SM, Bucciarelli P, et al. The effect of recanalization on long-term neurological outcome after cerebral venous thrombosis. J Thromb Haemost. 2018;16(4):718–24.
Nepal G, Kharel S, Bhagat R, Coghlan MA, Yadav JK, Goeschl S, et al. Safety and efficacy of endovascular thrombectomy in patients with severe cerebral venous thrombosis: a meta-analysis. J Cent Nerv Syst Dis. 2022;14:11795735221131736.
Funding
Open access funding provided by University of Bern. There was no relevant funding obtained in order to conduct this study.
Author information
Authors and Affiliations
Contributions
PB and VH designed the study. HH, AC, EH, JK and VH collected the data. PB performed statistical analysis and wrote the manuscript. All authors significantly contributed to and critically reviewed the final version of the manuscript.
Corresponding author
Ethics declarations
Conflicts of interest
HH has a consultancy agreement with Phenox GmbH | Wallaby Medical and is co-founder and shareholder of CONTARA GmbH. MA reports speaker honoraria from Astra Zeneca, Bayer, Covidien, Medtronic, Sanofi and honoraria for scientific advisory boards from Amgen, Bayer, BMS, Daiichi Sankyo, Medtronic, and Pfizer, and research funding from the Swiss National Science Foundation, and the Swiss Heart Foundation. TRM reports grants from Bangerter-Rhyner Foundation during the conduct of the study. VH has a consultant and proctoring agreement with Phenox GmbH. All other authors report no disclosures relevant to the article.
Ethical Approval/Informed Consent
This study was approved by the local institutional review boards (Ethics Commission of the State Medical Association of Baden-Württemberg [F-2012-077]; Kantonale Ethikkommission Bern [231/14]). Additional approval and patient consent was required for inclusion in the EVT registry (Stuttgart).
Additional information
Publisher's Note
Springer Nature remains neutral with regard to jurisdictional claims in published maps and institutional affiliations.
This article is related to the original article available at https://link.springer.com/article/10.1007/s12028-024-02045-8.
Supplementary Information
Below is the link to the electronic supplementary material.
Rights and permissions
Open Access This article is licensed under a Creative Commons Attribution 4.0 International License, which permits use, sharing, adaptation, distribution and reproduction in any medium or format, as long as you give appropriate credit to the original author(s) and the source, provide a link to the Creative Commons licence, and indicate if changes were made. The images or other third party material in this article are included in the article's Creative Commons licence, unless indicated otherwise in a credit line to the material. If material is not included in the article's Creative Commons licence and your intended use is not permitted by statutory regulation or exceeds the permitted use, you will need to obtain permission directly from the copyright holder. To view a copy of this licence, visit http://creativecommons.org/licenses/by/4.0/.
About this article
Cite this article
Bücke, P., Henkes, H., Kaesmacher, J. et al. Early Versus Late Initiation of Endovascular Therapy in Patients with Severe Cerebral Venous Sinus Thrombosis. Neurocrit Care (2024). https://doi.org/10.1007/s12028-024-02046-7
Received:
Accepted:
Published:
DOI: https://doi.org/10.1007/s12028-024-02046-7