Abstract
Background
The association between low-density lipoprotein cholesterol (LDL-C)/high-density lipoprotein cholesterol (HDL-C) ratio and the clinical outcomes of acute intracranial hemorrhage (ICH) remains unclear. In this study, we attempt to investigate whether low LDL-C/HDL-C ratio is associated with poor clinical outcomes in patients with ICH.
Methods
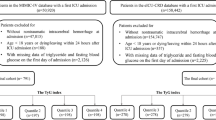
The database was collected from a multicenter, prospective, observational cohort study, conducted in 13 hospitals in Beijing from January 2014 to September 2016. A total of 1,964 patients with ICH were initially screened in our database. Next, we selected patients with admission serum lipid information for retrospective analysis. Patients were categorized into four groups based on LDL-C/HDL-C ratio quartiles. The main outcomes were 30-day and 90-day poor functional outcome, which is defined as modified Rankin Scale score of 3 to 6, and 90-day all-cause death. Logistic regression was used to assess the association between LDL-C/HDL-C ratio and 30-day or 90-day poor functional outcome. Kaplan–Meier survival analysis and Cox regression were used to assess the association between LDL-C/HDL-C ratio and 90-day all-cause death. Restricted cubic splines were used to explore the nonlinear association between LDL-C/HDL-C ratio and the outcome of patients with ICH.
Results
A total of 491 patients with spontaneous ICH were finally enrolled in our study. The mean age was 57.6 years old, and 72.1% (357/491) were men. After adjustment for confounders, patients in the lowest LDL-C/HDL-C quartile (< 1.74) had a significantly higher risk of 30-day and 90-day poor functional outcome compared with those in the highest quartile (> 3.16; 30-day: adjusted odds ratio 3.61, 95% confidence interval 1.68–7.72; 90-day: adjusted odds ratio 2.82, 95% confidence interval 1.33–5.95). Restricted cubic splines depicted a nonlinear association between LDL-C/HDL-C ratio and 90-day poor functional outcomes, indicating LDL-C/HDL-C ratio of 3.1–3.5 was correlated with better 90-day functional outcome. However, no significant correlation was found between low LDL-C/HDL-C ratio and 90-day all-cause death.
Conclusions
Lower LDL-C/HDL-C ratio (< 1.74) is independently associated with an increased risk of poor functional outcome in patients with ICH. In the population of patients whom we studied, there is a nonlinear association between LDL-C/HDL-C ratio and 90-day poor functional outcome, and patients with an LDL-C/HDL-C ratio of 3.1 to 3.5 tend to have the lowest risk of 90-day poor functional outcome.

Similar content being viewed by others
References
Wang W, Jiang B, Sun H, Ru X, Sun D, Wang L, et al. Prevalence, incidence, and mortality of stroke in China: results from a nationwide population-based survey of 480 687 adults. Circulation. 2017;135:759–71.
Feigin VL, Stark BA, Johnson CO, Roth GA, Bisignano C, Abady GG, et al. Global, regional, and national burden of stroke and its risk factors, 1990–2019: a systematic analysis for the Global Burden of Disease Study 2019. Lancet Neurol. 2021;20:795–820.
Cannon CP. Low-density lipoprotein cholesterol: lower is totally better. J Am Coll Cardiol. 2020;75:2119–21.
Mach F, Baigent C, Catapano AL, Koskinas KC, Casula M, Badimon L, et al. 2019 ESC/EAS Guidelines for the management of dyslipidaemias: Lipid modification to reduce cardiovascular risk. Eur Heart J. 2020;41:111–88.
Katakami N, Kaneto H, Osonoi T, Saitou M, Takahara M, Sakamoto F, et al. Usefulness of lipoprotein ratios in assessing carotid atherosclerosis in Japanese type 2 diabetic patients. Atherosclerosis. 2011;214:442–7.
Zhong Z, Hou J, Zhang Q, Zhong W, Li B, Li C, et al. Assessment of the LDL-C/HDL-C ratio as a predictor of one year clinical outcomes in patients with acute coronary syndromes after percutaneous coronary intervention and drug-eluting stent implantation. Lipids Health Dis. 2019;18:40.
Gao P, Wen X, Ou Q, Zhang J. Which one of LDL-C /HDL-C ratio and non-HDL-C can better predict the severity of coronary artery disease in STEMI patients. BMC Cardiovasc Disord. 2022;22:318.
Kunutsor SK, Zaccardi F, Karppi J, Kurl S, Laukkanen JA. Is high serum LDL/HDL cholesterol ratio an emerging risk factor for sudden cardiac death? Findings from the KIHD study. J Atheroscler Thromb. 2017;24:600–8.
Rodriguez-Luna D, Rubiera M, Ribo M, Coscojuela P, Pagola J, Piñeiro S, et al. Serum low-density lipoprotein cholesterol level predicts hematoma growth and clinical outcome after acute intracerebral hemorrhage. Stroke. 2011;42:2447–52.
Ramírez-Moreno JM, Casado-Naranjo I, Portilla JC, Calle ML, Tena D, Falcón A, et al. Serum cholesterol LDL and 90-day mortality in patients with intracerebral hemorrhage. Stroke. 2009;40:1917–20.
Elkhatib THM, Shehta N, Bessar AA. Hematoma expansion predictors: laboratory and radiological risk factors in patients with acute intracerebral hemorrhage: a prospective observational study. J Stroke Cerebrovasc Dis. 2019;28:2177–86.
Wang Y, Wu J, Gu H, Yang K, Jiang R, Li Z, et al. Lower low-density lipoprotein cholesterol levels are associated with an increased risk of hematoma expansion and ensuing mortality in acute ICH patients. Neurol Sci. 2022;43:3121–9.
Yuan S, Huang X, Ma W, Yang R, Xu F, Han D, et al. Associations of HDL-C/LDL-C with myocardial infarction, all-cause mortality, haemorrhagic stroke and ischaemic stroke: A longitudinal study based on 384 093 participants from the UK Biobank. Stroke Vasc Neurol. 2022;svn-2022–001668.
You S, Zhong C, Xu J, Han Q, Zhang X, Liu H, et al. LDL-C/HDL-C ratio and risk of all-cause mortality in patients with intracerebral hemorrhage. Neurol Res. 2016;38:903–8.
Kothari RU, Brott T, Broderick JP, Barsan WG, Sauerbeck LR, Zuccarello M, et al. The ABCs of measuring intracerebral hemorrhage volumes. Stroke. 1996;27.
Spence JD. Statins do not cause intracerebral hemorrhage. Neurology. 2012;79:1076–7.
Sanz-Cuesta BE, Saver JL. Lipid-lowering therapy and hemorrhagic stroke risk: comparative meta-analysis of statins and PCSK9 inhibitors. Stroke. 2021;52:3142–50.
Amarenco P, Kim JS, Labreuche J, Charles H, Giroud M, Lavallée PC, et al. Intracranial hemorrhage in the TST trial. Stroke. 2022;53:457–62.
Gu X, Li Y, Chen S, Yang X, Liu F, Li Y, et al. Association of lipids with ischemic and hemorrhagic stroke: a prospective cohort study among 267 500 Chinese. Stroke. 2019;50:3376–84.
Amarenco P, Goldstein LB, Szarek M, Sillesen H, Rudolph AE, Callahan A, et al. Effects of intense low-density lipoprotein cholesterol reduction in patients with stroke or transient ischemic attack: the stroke prevention by aggressive reduction in cholesterol levels (SPARCL) trial. Stroke. 2007;38:3198–204.
Wang X, Li S, Bai Y, Fan X, Sun K, Wang J, et al. Inverse association of plasma level of high-density lipoprotein cholesterol with intracerebral hemorrhage. J Lipid Res. 2011;52:1747–54.
O’Donnell MJ, McQueen M, Sniderman A, Pare G, Wang X, Hankey GJ, et al. Association of lipids, lipoproteins, and apolipoproteins with stroke subtypes in an international case control study (INTERSTROKE). J Stroke. 2022;24:224–35.
Sturgeon JD, Folsom AR, Longstreth WT, Shahar E, Rosamond WD, Cushman M. Risk factors for intracerebral hemorrhage in a pooled prospective study. Stroke. 2007;38:2718–25.
Wang X, Dong Y, Qi X, Huang C, Hou L. Cholesterol levels and risk of hemorrhagic stroke: a systematic review and meta-analysis. Stroke. 2013;44:1833–9.
Ooneda G, Yoshida Y, Suzuki K, Shinkai H, Hori S, Kobori K, et al. Smooth muscle cells in the development of plasmatic arterionecrosis, arteriosclerosis, and arterial contraction. J Vasc Res. 1978;15:148–56.
Konishi M, Iso H, Komachi Y, Iida M, Shimamoto T, Jacobs DR, et al. Associations of serum total cholesterol, different types of stroke, and stenosis distribution of cerebral arteries. Akita Pathol Study Stroke. 1993;24:954–64.
Chui D, Marotta F, Rao M, Liu D, Zhang S, Ideo C. Cholesterol-rich LDL perfused at physiological LDL-cholesterol concentration induces platelet aggregation and PAF-acetylhydrolase activation. Biomed Pharmacother. 1991;45:37–42.
Davis SM, Broderick J, Hennerici M, Brun NC, Diringer MN, Mayer SA, et al. Hematoma growth is a determinant of mortality and poor outcome after intracerebral hemorrhage. Neurology. 2006;66:1175–81.
Hankey GJ. Nutrition and the risk of stroke. Lancet Neurol. 2012;11:66–81.
Jayanama K, Theou O, Blodgett JM, Cahill L, Rockwood K. Frailty, nutrition-related parameters, and mortality across the adult age spectrum. BMC Med. 2018;16:188.
Funding
The study was supported by National Natural Science Foundation of China (Grant No. 82371302), Chinese Academy of Medical Sciences Innovation Fund for Medical Sciences (2019-I2M-5–029), National Key Research and Development Program of China (2018YFC1312200/ 2018YFC131224), Beijing Municipal Committee of Science and Technology (Z201100005620010), Beijing Natural Science Foundation (Z200016), Beijing key clinical specialty and Ministry of Science and Technology of the People’s Republic of China (National Key R&D Program of China, 2018YFC1705003). We thank all patients who participated in our study.
Author information
Authors and Affiliations
Contributions
LW analyzed, interpreted the data, and drafted the original manuscript. KK analyzed and interpreted the data. AW and XZ conducted the statistical analyses. WW designed the research. XZ designed the research, and handled the funding and supervision. The final manuscript was approved by all authors.
Corresponding author
Ethics declarations
Conflict of Interest
The authors report no conflict of interest in this work.
Ethical approval/informed consent
This study protocol was reviewed and approved by the Institutional Review Board of Beijing Tiantan Hospital, Capital Medical University, approval number KY2014-023–02. Written informed consents were obtained from all participants or their legal relatives for the publication of any potentially identifiable data or images included in this article.
Additional information
Publisher's Note
Springer Nature remains neutral with regard to jurisdictional claims in published maps and institutional affiliations.
Supplementary Information
Below is the link to the electronic supplementary material.
Rights and permissions
Springer Nature or its licensor (e.g. a society or other partner) holds exclusive rights to this article under a publishing agreement with the author(s) or other rightsholder(s); author self-archiving of the accepted manuscript version of this article is solely governed by the terms of such publishing agreement and applicable law.
About this article
Cite this article
Wu, L., Wang, A., Kang, K. et al. Low LDL-C/HDL-C Ratio is Associated with Poor Clinical Outcome After Intracerebral Hemorrhage: A Retrospective Analysis of Multicenter, Prospective Cohort Data in China. Neurocrit Care (2023). https://doi.org/10.1007/s12028-023-01905-z
Received:
Accepted:
Published:
DOI: https://doi.org/10.1007/s12028-023-01905-z