Abstract
Background
With a growing number of patients on new oral anticoagulants, interest in reversal agents is rising. Andexanet alfa is used for reversal of factor Xa inhibitors in intracranial hemorrhage.
Methods
We provide a brief review on andexanet-alfa-associated heparin resistance and discuss potentially critical situations from different clinical perspectives.
Results
Case reports point out that andexanet alfa can cause unresponsiveness to heparin, leading to catastrophic events. As a result, regulatory bodies have issued warning notices to avoid heparinization parallel to the use of andexanet alfa.
Conclusions
Although well known to hematologists, the phenomenon is underrecognized among stroke clinicians. However, patients with intracranial hemorrhage frequently undergo endovascular or surgical interventions that require periprocedural administration of heparin.
Similar content being viewed by others
Avoid common mistakes on your manuscript.
Background
With a growing number of patients treated with direct oral anticoagulants, general interest in reversal agents in patients with hemorrhagic stroke is rising. Andexanet alfa (AA) is the only reversal agent approved by the European Medicines Agency (EMA) and US Food and Drug Administration for oral direct factor Xa (FXa) inhibitors rivaroxaban and apixaban in situations when reversal of anticoagulation is needed because of life-threatening or uncontrolled bleeding. Safety and efficacy were evaluated in two prospective randomized placebo-controlled studies. Both studies analyzed anti-FXa activity in healthy volunteers receiving either apixaban (ANNEXA-A) or rivaroxaban (ANNEXA-R) [1]. This was followed by the ANNEXA-4 study published in 2019 on 352 patients who had acute major bleeding within 18 h after administration of an FXa inhibitor [2]. Just recently, the post hoc ANNEXA-4 substudy on hemostatic efficacy and anti-FXa reversal in intracranial hemorrhage (ICH) was published [3]. The authors conclude that AA reduced anti-FXa activity in FXa-inhibitor-treated patients with traumatic as well as spontaneous ICH with high rates of hemostatic efficacy. Results of the ongoing ANNEXA-I trial (NCT03661528), a randomized controlled trial evaluating the efficacy and safety of AA versus usual care in patients with ICH on FXa inhibitors, are excitedly awaited. In the absence of such a randomized controlled trial, safety and efficacy are being questioned by different groups of health care professionals, especially when considering the high cost of therapy with AA [4, 5].
AA-Associated Heparin Resistance
AA is a recombinant modified FXa decoy protein that has been shown to reverse the effects of direct FXa inhibitors apixaban and rivaroxaban by binding with higher affinity to these molecules compared with endogenous FXa. Although it was developed as an antagonist for direct FXa inhibitors, AA has also been shown to bind to antithrombin-dependent FXa inhibitors, such as unfractionated heparin (UFH), via binding to heparin-activated antithrombin [6, 7] (Fig. 1). These findings even led to the conclusion that AA may be suitable as an alternative to protamine in reversal of UFH [8].
Simplified schematic outline of andexanet-alfa-associated heparin resistance. Rivaroxaban and apixaban inhibit factor Xa (FXa), which normally catalyzes the formation of thrombin (dotted line). Andexanet alfa reverses the effects of apixaban and rivaroxaban by binding with higher affinity to these molecules compared with endogenous FXa (dotted line). Unfractionated heparin (UFH) potentiates the antithrombin (AT)-mediated inhibition of FXa. Andexanet alfa also binds to heparin-activated AT and thereby neutralizes the effect of heparin (intersected line)
UFH is administered during open vascular and endovascular procedures to reduce the risk of thromboembolic events. The use of AA prior to interventions with intended heparin anticoagulation has been reported to cause unresponsiveness to heparin. Few case reports from the field of cardiovascular surgery were published pointing out this problem [9,10,11]. All publications report clinical cases of patients who underwent reversal of direct FXa inhibitors with AA for life-threatening hemorrhage caused by either aortic aneurysm rupture or pericardial tamponade and subsequently developed critical intraoperative thromboembolism in the setting of periprocedural heparin administration (Table 1). Despite the supratherapeutic dose of UFH, point-of-care testing using activated clotting time failed to demonstrate a therapeutic heparinization that was necessary for cardiopulmonary bypass circulation [9,10,11]. Intraoperative UFH resistance is a well-known phenomenon in the field and is often attributed to antithrombin deficiency, increased UFH clearance, elevation in UFH binding protein, or high levels of factor VIII or fibrinogen [12, 13]. Administration of AA prior to heparinization was identified as another potential cause of heparin resistance. As a result, AA is now critically discussed in the cardiothoracic surgery community [14,15,16]. The above-mentioned case reports, together with further suspected adverse events reported to the EMA, have led to publication of a direct health care professional communication that was disseminated in November 2020. Although extent and duration of the interaction have not been evaluated, the EMA recommends avoiding the use of AA before heparinization [17].
Once identified as such, standardized protocols to address AA-associated heparin resistance are lacking. One single case of successful antithrombin substitution can be appreciated [9]. Another group reports on administration of fresh frozen plasma [11]. Both strategies were adopted from management of heparin resistance in coronary bypass surgery, in which antithrombin deficiency was found to be a major risk factor [18]. Because AA has been shown to bind to heparin-activated antithrombin, raising the overall concentration of AA is a potential salvage strategy [18]. For fresh frozen plasma, the effect on heparin resistance is highly speculative [19]. If the application of AA was followed by heparinization, we recommend to immediately stopping the AA infusion protocol. Because data supporting indications of clinical benefit with antithrombin supplementation outside of cardiac surgery are lacking, we propose treatment with direct thrombin inhibitors argatroban or bivalirudin [20]. These agents are favorable because of their therapeutic effect downstream of AA in the coagulation cascade [11]. Importantly, all these substances have not been studied in detail for treatment of AA-associated heparin resistance.
Special Considerations in the Management of Complex Hemorrhagic Stroke
Despite doubts about the evidence for use of AA among patients with hemorrhagic stroke, the substance is currently being used in clinical practice [5]. In the management of secondary-cause ICH (e.g., aneurysmal subarachnoid hemorrhage, ruptured arteriovenous fistulas, or arteriovenous malformation), microsurgical open vascular or endovascular procedures may be necessary to timely address the source of bleeding. Importantly, such procedures may well require temporary heparinization. Because the cardiothoracic community has already embraced the notion that AA should not be used for patients requiring heparinization, this issue has not yet been discussed within the neurovascular community [16]. With no data on AA-associated heparin resistance in patients with stroke available, the potential hazard of this association mandates translation of findings from cardiovascular medicine into stroke care. The distinct vascular physiology of cerebral circulation makes thromboembolism even more likely to cause harm here than in the extremity vasculature, which occurred in two cardiovascular case reports. Within the following paragraphs we sought to emphasize potential caveats of AA-associated heparin resistance and the need for vigilant management among all different angles of care to help prevent dramatic and potentially life-threatening situations.
Acute Stroke Care Perspective
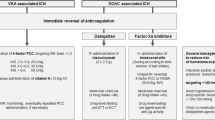
For primary care facilities, AA administration can be a valuable part of the initial resuscitative bundle prior to transfer of a patient to a stroke referral center. AA would normalize coagulation parameters during the highest risk period of interfacility transport, and its short half-life would allow it to clear by the time the patient arrives at the referral center [11]. Importantly, AA reverses FXa inhibitor levels for only 3 h, and then levels return to baseline, as compared with treatment with placebo. The pharmacokinetic half-life, however, is 5–7 h. As a result, heparin resistance may last for several hours after infusion [1, 2]. Conversely, a safe starting time for heparin has not been established. Starting AA before transport to a referral center can therefore be associated with potential morbidity for the patient. Ideally, the decision to administer AA should be made collaboratively between different specialties involved in hemorrhagic stroke care. To ease this decision-making process, we have established a simple administration algorithm at our institution (Fig. 2). On the basis of available computed tomography or magnetic resonance vascular imaging, each case is reviewed by an interdisciplinary team consisting of an attending neurologist, a neurointerventionalist, and a neurosurgeon. If a secondary vascular cause, such as a ruptured aneurysm or other vascular malformation (with potential need for heparinization during further treatment), is identified, a decision will be taken to administer a prothrombin complex concentrate at a dose of 50 IU/kg body weight instead of AA to address coagulopathy associated with direct oral anticoagulants. This is a situation in which AA should certainly not be administered. Importantly, considering limited evidence on safety and efficacy, a clear recommendation to administer AA over prothrombin complex concentrate in all other situations cannot me made. Including a pharmacist in the interdisciplinary team evaluating the optimal anticoagulation reversal strategy based on patient characteristics may help with decision-making. If AA was started without interdisciplinary review, the neuroendovascular and surgical teams will be notified, and decision-making processes can be adapted accordingly.
Surgical Perspective
The AA approval study does not provide any safety or efficacy data that can be extrapolated to the setting of a surgical procedure because the study excluded surgical patients. Still, optimal and timely hemostasis is highly desirable prior to any open intracranial neurosurgery. Several groups have already reported on the successful use of AA prior to hematoma evacuation [21,22,23]. However, AA-associated heparin resistance can be a problem when complex open neurovascular procedures, such as bypass surgery for trapping of a complex ruptured aneurysm, require heparinization to avoid formation of thromboembolism at the suture sites [24].
Neurointerventional Perspective
Patients with intracerebral hemorrhage frequently undergo acute endovascular interventions for treatments of aneurysms, arteriovenous malformations, or fistulas. Importantly, thromboembolic events represent the most frequent procedure-related complication [25]. Underlying causes include prothrombotic effects of endothelial injury, thrombus formation on the catheter hardware, and reduced flow in access route vessels and their vascular territories [25, 26]. Although practices of coagulation management vary, it is widely accepted that heparinization should be used to prevent thromboembolic complications during and after the procedure [27,28,29,30]. Notably, heparin resistance during neurovascular interventions may not be encountered as frequently as in many vascular surgery settings, where cardiopulmonary bypass and higher doses of UFH are often necessary. Here, heparin resistance can occur in up to 22% [18]. Although during endovascular procedures, repetitive angiography allows for early recognition of thromboembolic events, and thrombectomy via the same route can be executed immediately, repetitive vascular manipulation in the setting of AA-associated heparin resistance may be ineffective and can lead to a higher degree of local thrombosis and thromboembolism.
Conclusions
Stroke clinicians need to understand that AA can lead to heparin resistance with serious thromboembolic complications. It is crucial to early identify patients potentially undergoing procedures that necessitate periinterventional heparinization. To our knowledge, this is the first appreciation of AA-associated heparin resistance in acute neurological care literature, and we invite colleagues to discuss and apply our institutional decision support algorithm. More evidence is needed to appropriately judge the clinical significance of AA-associated heparin resistance in acute neurovascular diseases.
References
Siegal DM, Curnutte JT, Connolly SJ, et al. Andexanet alfa for the reversal of factor Xa inhibitor activity. N Engl J Med. 2015;373:2413–24.
Connolly SJ, Crowther M, Eikelboom JW, et al. Full study report of andexanet alfa for bleeding associated with factor Xa inhibitors. N Engl J Med. 2019;380:1326–35.
Demchuk AM, Yue P, Zotova E, et al. Hemostatic efficacy and anti-FXa (Factor Xa) reversal with andexanet alfa in intracranial hemorrhage: ANNEXA-4 substudy. Stroke. 2021;52:2096–105.
Yin E, McConnell KJ. Request for an andexxa value analysis. Ann Pharmacother. 2020;54:715–7.
Armahizer MJ, Badjatia N. Evidence for andexanet alpha in reversing intracerebral hemorrhage due to factor Xa inhibitors? Stroke. 2021;52:2106–8.
Kalathottukaren MT, Creagh AL, Abbina S, et al. Comparison of reversal activity and mechanism of action of UHRA, andexanet, and PER977 on heparin and oral FXa inhibitors. Blood Adv. 2018;2:2104–14.
Siddiqui F, Tafur A, Bontekoe E, et al. Assay-based differentiation in the neutralization profile of unfractionated heparin, enoxaparin, and fondaparinux by andexanet alfa. Clin Appl Thromb Hemost. 2020;26:1076029619895120.
Maneno JN, Ness GL. Andexanet alfa, the possible alternative to protamine for reversal of unfractionated heparin. Ann Pharmacother. 2021;55:261–4.
Apostel H, Winckers K, Bidar E, Schreiber JU. Successful antithrombin administration in andexanet alfa-associated heparin resistance. J Cardiothorac Vasc Anesth. 2021;35:904–7.
Eche IM, Elsamadisi P, Wex N, et al. Intraoperative unfractionated heparin unresponsiveness during endovascular repair of a ruptured abdominal aortic aneurysm following administration of andexanet alfa for the reversal of rivaroxaban. Pharmacotherapy. 2019;39:861–5.
Watson CJ, Zettervall SL, Hall MM, Ganetsky M. Difficult intraoperative heparinization following andexanet alfa administration. Clin Pract Cases Emerg Med. 2019;3:390–4.
Fredenburgh JC, Anderson JA, Weitz JI. Antithrombin-independent anticoagulation by hypersulfated low-molecular-weight heparin. Trends Cardiovasc Med. 2002;12:281–7.
Anderson JA, Saenko EL. Heparin resistance. Br J Anaesth. 2002;88:467–9.
Levy JH, Welsby I. Andexanet alfa use in patients requiring cardiopulmonary bypass: quo vadis? A A Pract. 2019;13:477.
Erdoes G, Birschmann I, Nagler M, Koster A. Andexanet alfa-induced heparin resistance: when anticoagulation really remains reversed. J Cardiothorac Vasc Anesth. 2021;35:908–9.
Levy JH, Connors JM. Andexanet alfa use in cardiac surgical patients: a Xa inhibitor and heparin reversal agent. J Cardiothorac Vasc Anesth. 2021;35:265–6.
European Medicines Agency. Direct healthcare professional communication: Ondexxya (andexanet alfa): avoid use of andexanet prior to heparinization. 2020.
Spiess BD. Treating heparin resistance with antithrombin or fresh frozen plasma. Ann Thorac Surg. 2008;85:2153–60.
Sabbagh AH, Chung GK, Shuttleworth P, Applegate BJ, Gabrhel W. Fresh frozen plasma: a solution to heparin resistance during cardiopulmonary bypass. Ann Thorac Surg. 1984;37:466–8.
Levy JH, Connors JM. Heparin resistance-clinical perspectives and management strategies. N Engl J Med. 2021;385:826–32.
Barra ME, Das AS, Hayes BD, et al. Evaluation of andexanet alfa and four-factor prothrombin complex concentrate (4F-PCC) for reversal of rivaroxaban- and apixaban-associated intracranial hemorrhages. J Thromb Haemost. 2020;18:1637–47.
Ammar AA, Ammar MA, Owusu KA, et al. Andexanet alfa versus 4-factor prothrombin complex concentrate for reversal of factor Xa inhibitors in intracranial hemorrhage. Neurocrit Care. 2021;35:255–61.
Vestal ML, Hodulik K, Mando-Vandrick J, et al. Andexanet alfa and four-factor prothrombin complex concentrate for reversal of apixaban and rivaroxaban in patients diagnosed with intracranial hemorrhage. J Thromb Thrombolysis. 2022;53:167–75.
Zhang J, Feng Y, Zhao W, Liu K, Chen J. Safety and effectiveness of high flow extracranial to intracranial saphenous vein bypass grafting in the treatment of complex intracranial aneurysms: a single-centre long-term retrospective study. BMC Neurol. 2021;21:307.
Naggara ON, Lecler A, Oppenheim C, Meder JF, Raymond J. Endovascular treatment of intracranial unruptured aneurysms: a systematic review of the literature on safety with emphasis on subgroup analyses. Radiology. 2012;263:828–35.
Michelson AD, Frelinger AL 3rd. Thrombus formation. In: Wakhloo AK, Gounis MJ, Lieber BB, Mericle RA, Linfante I, editors. Thrombus and stroke. Boca Raton (FL): CRC Press; 2008. p. 3–14.
Lim Fat MJ, Al-Hazzaa M, Bussiere M, dos Santos MP, Lesiuk H, Lum C. Heparin dosing is associated with diffusion weighted imaging lesion load following aneurysm coiling. J Neurointerv Surg. 2013;5:366–70.
Benali F, van der Leij C, Staals J, van Zwam WH. Use of heparinized saline flush during endovascular thrombectomy for acute ischemic stroke; a survey of clinical practice in the Netherlands. CVIR Endovasc. 2021;4:76.
Ogilvy CS, Stieg PE, Awad I, et al. AHA scientific statement: recommendations for the management of intracranial arteriovenous malformations: a statement for healthcare professionals from a special writing group of the Stroke Council. Am Stroke Assoc Stroke. 2001;32:1458–71.
Vance AZ, Jayaraman MV, Dubel GJ, Doberstein CE, Haas RA. Safety of intravenous heparin administration after endovascular treatment for ruptured intracranial aneurysms. J Neurointerv Surg. 2009;1:136–41.
Funding
Open Access funding enabled and organized by Projekt DEAL. No funding was received for this work.
Author information
Authors and Affiliations
Contributions
All authors fulfill the criteria for authorship set by the International Committee of Medical Journal Editors. Individual authors put special emphasis on conception and design (MM, WS, HW, JM), acquisition of data (MM, WS), analysis and interpretation of data (RMM, MM, WS), and drafting and revising (MM, WS, RMM, MH).
Corresponding author
Ethics declarations
Conflicts of interest
None of the authors report a conflict of interest.
Ethical Approval/Informed Consent
For this commentary no primary patient data are included and no institutional review board approval was obtained.
Additional information
Publisher's Note
Springer Nature remains neutral with regard to jurisdictional claims in published maps and institutional affiliations.
Rights and permissions
Open Access This article is licensed under a Creative Commons Attribution 4.0 International License, which permits use, sharing, adaptation, distribution and reproduction in any medium or format, as long as you give appropriate credit to the original author(s) and the source, provide a link to the Creative Commons licence, and indicate if changes were made. The images or other third party material in this article are included in the article's Creative Commons licence, unless indicated otherwise in a credit line to the material. If material is not included in the article's Creative Commons licence and your intended use is not permitted by statutory regulation or exceeds the permitted use, you will need to obtain permission directly from the copyright holder. To view a copy of this licence, visit http://creativecommons.org/licenses/by/4.0/.
About this article
Cite this article
Müther, M., Schwindt, W., Mesters, R.M. et al. Andexanet-Alfa-Associated Heparin Resistance in the Context of Hemorrhagic Stroke. Neurocrit Care 37, 372–376 (2022). https://doi.org/10.1007/s12028-022-01573-5
Received:
Accepted:
Published:
Issue Date:
DOI: https://doi.org/10.1007/s12028-022-01573-5