Abstract
Background
We present an exploratory analysis of the occurrence of early corticothalamic connectivity disruption after aneurysmal subarachnoid hemorrhage (SAH) and its correlation with clinical outcomes.
Methods
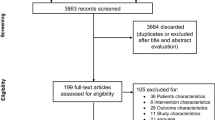
We conducted a retrospective study of patients with acute SAH who underwent continuous electroencephalography (EEG) for impairment of consciousness. Only patients undergoing endovascular aneurysm treatment were included. Continuous EEG tracings were reviewed to obtain artifact-free segments. Power spectral analyses were performed, and segments were classified as A (only delta power), B (predominant delta and theta), C (predominant theta and beta), or D (predominant alpha and beta). Each incremental category from A to D implies greater preservation of corticothalamic connectivity. We dichotomized categories as AB for poor connectivity and CD for good connectivity. The modified Rankin Scale score at follow-up and in-hospital mortality were used as outcome measures.
Results
Sixty-nine patients were included, of whom 58 had good quality EEG segments for classification: 28 were AB and 30 were CD. Hunt and Hess and World Federation of Neurological Surgeons grades were higher and the initial Glasgow Coma Scale score was lower in the AB group compared with the CD group. AB classification was associated with an adjusted odds ratio of 5.71 (95% confidence interval 1.61–20.30; p < 0.01) for poor outcome (modified Rankin Scale score 4–6) at a median follow-up of 4 months (interquartile range 2–6) and an odds ratio of 5.6 (95% confidence interval 0.98–31.95; p = 0.03) for in-hospital mortality, compared with CD.
Conclusions
EEG spectral-power-based classification demonstrates early corticothalamic connectivity disruption following aneurysmal SAH and may be a mechanism involved in early brain injury. Furthermore, the extent of this disruption appears to be associated with functional outcome and in-hospital mortality in patients with aneurysmal SAH and appears to be a potentially useful predictive tool that must be validated prospectively.




Similar content being viewed by others
References
Pobereskin LH. Incidence and outcome of subarachnoid haemorrhage: a retrospective population based study. J Neurol Neurosurg Psychiatry. 2001;70(3):340–3.
Cesarini KG, Hårdemark HG, Persson L. Improved survival after aneurysmal subarachnoid hemorrhage: review of case management during a 12-year period. J Neurosurg. 1999;90(4):664–72.
Luo YC, Shen CS, Mao JL, Liang CY, Zhang Q, He ZJ. Ultra-early versus delayed coil treatment for ruptured poor-grade aneurysm. Neuroradiology. 2015;57(2):205–10.
Dhandapani S, Singh A, Singla N, et al. Has outcome of subarachnoid hemorrhage changed with improvements in neurosurgical services? Stroke. 2018;49(12):2890–5.
Naval NS, Chang T, Caserta F, Kowalski RG, Carhuapoma JR, Tamargo RJ. Improved aneurysmal subarachnoid hemorrhage outcomes: a comparison of 2 decades at an academic center. J Crit Care. 2013;28(2):182–8.
La Pira B, Singh TD, Rabinstein AA, Lanzino G. Time trends in outcomes after aneurysmal subarachnoid hemorrhage over the past 30 years. Mayo Clin Proc. 2018;93(12):1786–93.
Carpenter KL, Czosnyka M, Jalloh I, et al. Systemic, local, and imaging biomarkers of brain injury: more needed, and better use of those already established? Front Neurol. 2015;18(6):26.
Hunt WE, Hess RM. Surgical risk as related to time of intervention in the repair of intracranial aneurysms. J Neurosurg. 1968;28(1):14–20.
Dengler NF, Diesing D, Sarrafzadeh A, Wolf S, Vajkoczy P. The barrow neurological institute scale revisited: predictive capabilities for cerebral infarction and clinical outcome in patients with aneurysmal subarachnoid hemorrhage. Neurosurgery. 2017;81(2):341–9.
Rosenthal ES, Biswal S, Zafar SF, et al. Continuous electroencephalography predicts delayed cerebral ischemia after subarachnoid hemorrhage: a prospective study of diagnostic accuracy. Ann Neurol. 2018;83(5):958–69.
Maciel CB, Gilmore EJ. Seizures and Epileptiform patterns in SAH and their relation to outcomes. J Clin Neurophysiol. 2016;33(3):183–95.
Allen BB, Forgacs PB, Fakhar MA, et al. Association of seizure occurrence with aneurysm treatment modality in aneurysmal subarachnoid hemorrhage patients. Neurocrit Care. 2018;29(1):62–8.
Sitt JD, King JR, El Karoui I, et al. Large scale screening of neural signatures of consciousness in patients in a vegetative or minimally conscious state. Brain. 2014;137(Pt 8):2258–70.
Schiff ND. Recovery of consciousness after brain injury: a mesocircuit hypothesis. Trends Neurosci. 2010;33(1):1–9.
Forgacs PB, Frey HP, Velazquez A, et al. Dynamic regimes of neocortical activity linked to corticothalamic integrity correlate with outcomes in acute anoxic brain injury after cardiac arrest. Ann Clin Transl Neurol. 2017;4(2):119–29.
Scannell JW, Burns GA, Hilgetag CC, O’Neil MA, Young MP. The connectional organization of the cortico-thalamic system of the cat. Cereb Cortex. 1999;9(3):277–99.
MacNeil MA, Lomber SG, Payne BR. Thalamic and cortical projections to middle suprasylvian cortex of cats: constancy and variation. Exp Brain Res. 1997;114(1):24–32.
Adams JH, Graham DI, Jennett B. The neuropathology of the vegetative state after an acute brain insult. Brain. 2000;123(Pt 7):1327–38.
Maxwell WL, MacKinnon MA, Smith DH, McIntosh TK, Graham DI. Thalamic nuclei after human blunt head injury. J Neuropathol Exp Neurol. 2006;65(5):478–88.
Van der Werf YD, Witter MP, Groenewegen HJ. The intralaminar and midline nuclei of the thalamus. Anatomical and functional evidence for participation in processes of arousal and awareness. Brain Res Brain Res Rev. 2002;39(2–3):107–40.
Schiff ND. Central thalamic contributions to arousal regulation and neurological disorders of consciousness. Ann N Y Acad Sci. 2008;1129(1):105–18.
Fridman EA, Beattie BJ, Broft A, Laureys S, Schiff ND. Regional cerebral metabolic patterns demonstrate the role of anterior forebrain mesocircuit dysfunction in the severely injured brain. Proc Natl Acad Sci USA. 2014;111(17):6473–8.
Chen P, Xie Q, Wu X, et al. Abnormal effective connectivity of the anterior forebrain regions in disorders of consciousness. Neurosci Bull. 2018;34(4):647–58.
Mikell CB, Banks GP, Frey HP, et al. Frontal networks associated with command following after hemorrhagic stroke. Stroke. 2015;46(1):49–57.
Owen AM, Coleman MR, Boly M, Davis MH, Laureys S, Pickard JD. Detecting awareness in the vegetative state. Science. 2006;313(5792):1402.
Schiff ND. Cognitive motor dissociation following severe brain injuries. JAMA Neurol. 2015;72(12):1413–5.
Edlow BL, Chatelle C, Spencer CA, et al. Early detection of consciousness in patients with acute severe traumatic brain injury. Brain. 2017;140(9):2399–414.
Claassen J, Velazquez A, Meyers E, et al. Bedside quantitative electroencephalography improves assessment of consciousness in comatose subarachnoid hemorrhage patients. Ann Neurol. 2016;80(4):541–53.
Claassen J, Doyle K, Matory A, et al. Detection of brain activation in unresponsive patients with acute brain injury. N Engl J Med. 2019;380:2497–505.
Forgacs PB, Conte MM, Fridman EA, et al. Preservation of electroencephalographic organization in patients with impaired consciousness and imaging-based evidence of command-following. Ann Neurol. 2014;76(6):869–79.
Mani R, Arif H, Hirsch LJ, Gerard EE, LaRoche SM. Interrater reliability of ICU EEG research terminology. J Clin Neurophys. 2012;29(3):203–12.
Teasdale G, Jennett B. Assessment of coma and impaired consciousness. A practical scale. Lancet. 1974;304(7872):81–4.
Andersen CR, Fitzgerald E, Delaney A, Finfer S. A systematic review of outcome measures employed in aneurysmal subarachnoid hemorrhage (aSAH) clinical research. Neurocrit Care. 2019;30(3):534–41.
Connolly ES Jr, Rabinstein AA, Carhuapoma JR, et al. Guidelines for the management of aneurysmal subarachnoid hemorrhage: a guideline for healthcare professionals from the American Heart Association/american Stroke Association. Stroke. 2012;43(6):1711–37.
Thomson DJ. Spectrum estimation and harmonic analysis. Proc IEEE. 1982;70(9):1055–96.
Schiff ND, Nauvel T, Victor JD. Large-scale brain dynamics in disorders of consciousness. Curr Opin Neurobiol. 2014;25:7–14.
Petzold A, Keir G, Kay A, Kerr M, Thompson EJ. Axonal damage and outcome in subarachnoid haemorrhage. J Neurol Neurosurg Psychiatry. 2006;77(6):753–9.
Nelson S, Edlow BL, Wu O, Rosenthal ES, Westover MB, Rordorf G. Default mode network perfusion in aneurysmal subarachnoid hemorrhage. Neurocrit Care. 2016;25(2):237–42.
Mangat H, Ivanidze J, Mao X, et al. Selective frontal lobe metabolic dysfunction after subarachnoid hemorrhage—evidence for flow-metabolism uncoupling? Neurology 2017; 88(suppl 16):P5.067.
Zanier ER, Refai D, Zipfel GJ, et al. Neurofilament light chain levels in ventricular cerebrospinal fluid after acute aneurysmal subarachnoid haemorrhage. J Neurol Neurosurg Psychiatry. 2011;82(2):157–9.
Hviid CVB, Lauridsen SV, Gyldenholm T, Sunde N, Parkner T, Hvas AM. Plasma neurofilament light chain is associated with poor functional outcome and mortality rate after spontaneous subarachnoid hemorrhage. Transl Stroke Res. 2020;11(4):671–7.
Fridman EA, Schiff ND. Neuromodulation of the conscious state following severe brain injuries. Curr Opin Neurobiol. 2014;29:172–7.
Wang M, Rajan SS, Jacob AP, et al. Retrospective collection of 90-day modified Rankin Scale is accurate. Clin Trials. 2020;17(6):637–43.
Funding
Dr. Forgacs reports grants from the National Institute of Neurological Disorders and Stroke (Grant No. K23-NS096222), grants from the Leon Levy Neuroscience Fellowship Award, grants from the National Center for Advancing Translational Sciences (Grant No. UL1-TR000043), grants from the Rockefeller Clinical and Translational Science Award Program, and grants from the Stavros Niarchos Foundation during the conduct of the study. Dr. Allen has nothing to disclose. Ms. Wu reports grants from the National Center for Advancing Translational Sciences. Dr. Gerber reports grants from the National Center for Advancing Translational Sciences. Dr. Boddu has nothing to disclose. Dr. Fakhar has nothing to disclose. Dr. Stieg has nothing to disclose. Dr. Schiff reports grants from the National Institute of Neurological Disorders and Stroke (Grant No. RO1-HD051912), grants from the James S. McDonnell Foundation, and grants from the Jerold B. Katz Foundation. Dr. Mangat has nothing to disclose.
Author information
Authors and Affiliations
Contributions
Peter B. Forgacs, MD, designed and conceptualized the study, analyzed and interpreted the data, and drafted the manuscript for intellectual content. Baxter B. Allen, MD, designed and conceptualized the study, analyzed and interpreted the data, and drafted and revised the manuscript for intellectual content. Xian Wu, MPH, analyzed the data and drafted the manuscript for intellectual content. Linda M. Gerber, PhD, analyzed the data and drafted the manuscript for intellectual content. Srikanth Boddu, MD, contributed a major role in the acquisition of data and revised the manuscript for intellectual content. Malik Fakhar, MD, contributed a major role in the acquisition of data. Phillip E. Stieg, PhD, MD, designed and conceptualized the study. Nicholas D. Schiff, MD, designed and conceptualized the study and revised the manuscript for intellectual content. Halinder S. Mangat, MD, designed and conceptualized the study, interpreted the data, and drafted and revised the manuscript for intellectual content.
Corresponding author
Ethics declarations
Conflicts of interest
The authors declare no conflict of interest.
Ethical approval/informed consent
The institutional review board for research integrity at Weill Cornell Medicine approved the study, and all ethical guidelines were adhered to.
Additional information
Publisher's Note
Springer Nature remains neutral with regard to jurisdictional claims in published maps and institutional affiliations.
Supplementary Information
Below is the link to the electronic supplementary material.
Rights and permissions
About this article
Cite this article
Forgacs, P.B., Allen, B.B., Wu, X. et al. Corticothalamic Connectivity in Aneurysmal Subarachnoid Hemorrhage: Relationship with Disordered Consciousness and Clinical Outcomes. Neurocrit Care 36, 760–771 (2022). https://doi.org/10.1007/s12028-021-01354-6
Received:
Accepted:
Published:
Issue Date:
DOI: https://doi.org/10.1007/s12028-021-01354-6