Abstract
Background
Delirium screening instruments (DSIs) should be used to detect delirium, but they only show moderate sensitivity in patients with neurocritical illness. We explored whether, for these patients, DSI validity is impacted by patient-specific covariates.
Methods
Data were prospectively collected in a single-center quality improvement project. Patients were screened for delirium once daily using the Intensive Care Delirium Screening Checklist (ICDSC) and the Confusion Assessment Method for the Intensive Care Unit (CAM-ICU). Reference was the daily assessment using criteria from the Diagnostic and Statistical Manual, 4th Edition, Text Revision (DSM-IV-TR). In a two-step receiver operating characteristics regression analysis adjusting for repeated measurements, the impact of acute diagnosis of stroke or transient ischemic attack (TIA), neurosurgical intervention, Richmond Agitation Sedation Scale, and ventilation status on test validity was determined.
Results
Of 181 patients screened, 101 went into final analysis. Delirium incidence according to DSM-IV-TR was 29.7%. For the first complete assessment series (CAM-ICU, ICDSC, and DSM-IV-TR), sensitivity for the CAM-ICU and the ICDSC was 73.3% and 66.7%, and specificity was 91.8% and 94.1%, respectively. Consideration of daily repeated measurements increased sensitivity for the CAM-ICU and ICDSC to 75.7% and 73.4%, and specificity to 97.3% and 98.9%, respectively. Receiver operating characteristics regression revealed that lower Richmond Agitation Sedation Scale levels significantly impaired validity of the ICDSC (p = 0.029) and the CAM-ICU in its severity scale version (p = 0.004). Neither acute diagnosis of stroke or TIA nor neurosurgical intervention or mechanical ventilation significantly influenced DSI validity.
Conclusions
The CAM-ICU and ICDSC perform well in patients requiring neurocritical care, regardless of the presence of acute stroke, TIA, or neurosurgical interventions. Yet, even very light or moderate sedation can significantly impair DSI performance.
Similar content being viewed by others
Avoid common mistakes on your manuscript.
Introduction
Delirium is the most typical manifestation of a per-definition secondary encephalopathy in the critical care context [1]. Studies revealed that up to 82% of mechanically ventilated patients suffer from delirium [1]. Because delirium impairs outcomes [1,2,3], regular screening with a validated delirium screening instrument (DSI) is recommended in national and international guidelines, with a high level of evidence [4, 5]. DSIs such as the Confusion Assessment Method for the Intensive Care Unit (CAM-ICU) [6] and the Intensive Care Delirium Screening Checklist (ICDSC) [7] have shown a sufficient diagnostic validity and reliability in medical and surgical intensive care and are considered to be the standard for the diagnosis of delirium [8].
There are only a few studies pertaining to delirium in patients with neurocritical illness. These patients show a pooled delirium prevalence rate of 11.8% to 45.9% in prospective cohort studies [9]. Just like in other patient populations, delirium in this cohort is associated with increased intensive care unit (ICU) and hospital length of stay, cost of care, and occurrence of postintensive care syndrome, particularly long-term cognitive impairments [9].
Neurological and neurosurgical patients typically show symptoms that, by their nature, are related to the patient’s primary pathology (e.g., edema, seizures, or ischemia). These symptoms could potentially alter and overlap with symptoms that are assessed during a delirium screening and therefore lead to a false positive DSI result and delayed diagnosis of the underlying problem. At worst, exacerbation of the underlying disease could be misinterpreted as delirium. In a meta-analysis, Patel et al. [9] rightfully caution their readership that information from a delirium screening should only be considered complementary to the neurological examination, which is paramount to diagnose complex complications. Therefore, validation of the DSIs in the context of neurocritical care is of utmost importance. Previously, the diagnostic validity of the CAM-ICU and the ICDSC in patients with neurological and neurosurgical critical illness was assessed in five studies that revealed a moderate sensitivity and a good to excellent specificity [10,11,12,13,14]. Yet, no study to date has investigated whether the Richmond Agitation Sedation Scale (RASS), mechanical ventilation, presence of an acute stroke or a transient ischemic attack (TIA), and neurosurgical interventions directly impact the diagnostic validity of the CAM-ICU and the ICDSC in patients with neurocritical illness.
Methods
Project Setting and Design
We report on a quality improvement (QI) project conducted at Charité – Universitätsmedizin Berlin. Data were prospectively collected as part of internal QI procedures, as part of delirium assessment according to the hospital’s standard operating procedure (SOP), and according to a national guideline. Approval of data protection was obtained before data collection. Scientific publication of results was approved by the Ethics Committee at Charité – Universitätsmedizin Berlin (EA1/228/15) post-hoc and written informed consent was waived. The research has been carried out in accordance with the Declaration of Helsinki from 1964 and its amendments.
Patients
We consecutively enrolled patients with critical illness admitted to one neurological/neurosurgical ICU at Charité – Universitätsmedizin Berlin between 15 September 2011 and 14 October 2011 (first assessment period) and between 1 February and 14 April 2012 (second assessment period). Exclusion criteria of the QI project were as follows: Age below 18 years, lack of German proficiency, clinically manifest dementia or other psychiatric disorder, lack of willingness to participate in assessments, and patient likely to pass away in the subsequent 24 h.
Delirium Assessments
Patients were assessed for delirium once daily using the ICDSC and the CAM-ICU from the day of ICU admission until discharge or end of assessment period (Fig. 1). As a reference standard, Diagnostic and Statistical Manual, 4th Edition, Text Revision (DSM-IV-TR) assessment was conducted once daily. Independent from routine care, ICDSC and CAM-ICU were assessed by specially trained QI project staff (DU, among others) under the supervision of experienced intensivists (AL, among others). DSM-IV-TR was assessed by specially trained QI project staff under supervision of an intensivist who was backed up by a board-certified psychiatrist. Assessors received training as previously described [15]. Briefly, training comprised oral presentations, printed information material, hands-on application, and reference testing of five consecutive patients who had previously been tested by two experienced intensivists. Differences between assessors and experienced intensivists were discussed to reach consensus [15]. DSIs and DSM-IV-TR were always applied at the same time of the day and in the same order (Fig. 1). To avoid bias due to between-observer variation, each assessment tool was consistently applied by one assessor. To ensure that each assessor was blinded to the results of the other assessors, there were gaps of 20 min between delirium assessments. All assessments were conducted within 90 min to avoid fluctuations of symptoms. Daily and in synchrony with delirium assessments, vigilance [Glasgow Coma Scale (GCS)] and level of sedation (RASS) were documented. The RASS was used for intubated and nonintubated patients. If a patient was comatose or deeply sedated (RASS < − 3 or GCS < 9), no delirium assessment was conducted on that particular occasion. Immediately after assessments, results were electronically documented with a patient-specific pseudonym using LimeSurvey (LimeSurvey GmbH, Hamburg, Germany). Patients were excluded from analysis if, due to deep sedation or coma, no complete assessment series (ICDSC, CAM-ICU, and DSM-IV-TR) could be conducted until discharge or end of assessment period. Results of the CAM-ICU were transformed from a binary to an ordinal scale as previously described for the transformation of the pediatric CAM-ICU [16]. Accordingly, the ordinal CAM-ICU was named severity scale for the CAM-ICU (ssCAM-ICU).
Delirium assessment and data collection schedule. APACHE II Acute Physiology and Chronic Health Disease Classification System II, CAM-ICU Confusion Assessment Method for the Intensive Care Unit, DSM-IV-TR Diagnostic and Statistical Manual, 4th Edition, Text Revision, GCS Glasgow Coma Scale, ICDSC Intensive Care Delirium Screening Checklist, ICU, intensive care unit, Inv. mech. ventilation Invasive mechanical ventilation, RASS Richmond Agitation Sedation Scale, SAPS II, Simplified Acute Physiology Score II
Assessment of Patient Characteristics
On project enrollment, patients’ age, sex, weight, reason of admission (including neurosurgical intervention), main International Classification of Diseases, 10th revision (ICD-10), diagnosis (including acute diagnosis of stroke/TIA), history of clinically manifest dementia, diagnosis of alcohol use disorder, and history of stroke or TIA were documented. Six months after the assessment period, the following data were extracted from the patients’ electronic medical record: ICU length of stay, presence and duration of invasive mechanical ventilation, Acute Physiology and Chronic Health Disease Classification System II (APACHE II) and Simplified Acute Physiology Score II (SAPS II) scores upon admission, in-hospital mortality, and place of discharge.
Statistical Analysis
Descriptive analysis of the QI project population with corresponding distributions is presented as either median with limits of the interquartile range (25th to 75th percentile) or as absolute (n) or relative (%) frequencies. Differences in characteristics between the group of patients who were delirium-positive according to DSM-IV-TR in at least one assessment and the group of patients who were delirium-negative were compared using the Mann–Whitney U-test for continuous variables, Fisher’s exact test for frequencies with two categories, and χ2 test for frequencies with three or more categories. Using each patient’s first complete assessment series, sensitivity, specificity, positive predictive value (PPV), and negative predictive value (NPV) were calculated and compared using McNemar test. The first complete assessment series was defined as the first time all assessment tools (ICDSC, CAM-ICU, and DSM-IV-TR) were applied. Empirical receiver operating characteristics (ROC) curves of the ICDSC and ssCAM-ICU were plotted for the first complete assessment series using the DSM-IV-TR as the binary classifier for delirium, area under the curve (AUC) determined and compared according to DeLong et al. [17]. Including all assessments of the ICDSC and the CAM-ICU, we fitted a logistic regression model with random effects to determine sensitivity, specificity, PPV and NPV, adjusting for repeated measurements per patient (binary clustered data) [18,19,20]. All assessments were defined as any assessment pair of DSM-IV-TR and ICDSC or CAM-ICU, respectively. Empirical ROC curves were plotted for all assessments of the ICDSC and ssCAM-ICU using the DSM-IV-TR as the binary classifier for delirium, AUCs determined and compared using Somer’s D and Harrell’s c, adjusting for repeated assessments [21, 22]. Pietra indexes were calculated for the ROC curves. The Pietra index describes a test’s ability to distinguish between patients who were delirium-positive and delirium-negative and has a range of 0 (no distinction between patients who were delirium-positive and delirium-negative) and 1 (perfect distinction between patients who were delirium-positive and delirium-negative) [23]. We assessed the influence of the following covariates on DSI validity: RASS score, mechanical ventilation (yes/no), sex (male/female), neurosurgical intervention (yes/no), and acute diagnosis of stroke/TIA (yes/no). Acute diagnosis of stroke/TIA and neurosurgical intervention (which included surgical procedures only) were selected because they resemble common and distinct patient cohorts in neurocritical care. Patients who underwent neurosurgical interventions are commonly treated in non-neurological ICUs, whereas patients with acute stroke/TIA are commonly treated in specialized stroke units or neurological ICUs. To assess the effect of the covariates on DSI validity, we performed a two-step ROC regression analysis [24], defining covariates for the control population (DSM-IV-TR negative) and case population (DSM-IV-TR positive), including all assessments and adjusting for repeated assessments. To confirm ROC regression results, empirical, covariate-adjusted ROC curves were plotted and AUCs determined. Analysis was performed with STATA 13.1 (StataCorp LP, College Station, TX).
Results
Characteristics of the Project Cohort
Out of n = 181 patients screened to participate in the QI project, n = 80 (44.2%) were excluded, leaving n = 101 (55.8%) patients for analysis (Fig. 2). Baseline characteristics are described in Table 1. Thirty (29.7%) patients were tested positive for delirium according to DSM-IV-TR on at least one occasion. Patients in the delirium group showed a higher severity of illness [APACHE II on admission 20 (16–26) vs. 13 (7–19), p < 0.001; SAPS II on admission 39.5 (31–49) vs. 25.5 (15–38), p < 0.001]. Significantly more patients in the delirium group were mechanically ventilated [n = 22 (73.3%) vs. n = 22 (31.0%), p < 0.001] with longer duration [105.5 (0–185) vs. 0 (0–11) hours, p < 0.001]. Patients in the delirium group had a longer ICU length of stay [15.5 (9–22) vs. 3 (1–6) days, p < 0.001], higher in-hospital mortality [n = 5 (16.7%) vs. n = 0 (0%), p = 0.002] and spent more days with sedation [1.5 (0–5) vs. 0 (0–0), p < 0.001]. Sedation was defined as at least light sedation (RASS − 2 or lower) during the assessment.
Validity of the ICDSC, CAM-ICU, and ssCAM-ICU for the First Complete Assessment Series
In the first complete assessment series, n = 15 (15%) patients were diagnosed positive for delirium according to DSM-IV-TR. The CAM-ICU showed a sensitivity of 73.3%, a specificity of 91.8%, a PPV of 61.1%, and a NPV of 95.1%. The ICDSC had a sensitivity of 66.7%, a specificity of 94.1%, a PPV of 66.7%, and a NPV of 94.1% (Table 2). Test validities of the CAM-ICU and the ICDSC were not significantly different (p = 0.317). As shown in Fig. 3a, b, ROC analysis revealed an AUC of 0.913 for the ICDSC and 0.912 for the ssCAM-ICU, with no significant difference (p = 0.993). The Pietra index was 0.50 for the ICDSC and 0.39 for the ssCAM-ICU. The difference in Pietra indexes indicates that the ICDSC has a better ability to distinguish between patients who were delirium-positive and delirium-negative.
ROC curves of the ICDSC and ssCAM-ICU for the first complete assessment series (a, b) and for all assessments (c, d). The first complete assessment series was defined as first time all assessment tools (ICDSC, CAM-ICU, and DSM-IV-TR) were applied. All assessments were defined as any assessment pair of DSM-IV-TR and ICDSC or CAM-ICU, respectively. The DSM-IV-TR was used as reference for delirium assessments. CAM-ICU Confusion Assessment Method for the Intensive Care Unit, DSM-IV-TR Diagnostic and Statistical Manual, 4th Edition, Text Revision, ICDSC Intensive Care Delirium Screening Checklist, ROC Receiver operating characteristic, ssCAM-ICU Severity scale Confusion Assessment Method for the Intensive Care Unit
Validity of the ICDSC, CAM-ICU, and ssCAM-ICU for all Assessments
For the CAM-ICU, n = 324 corresponding DSM-IV-TR and CAM-ICU assessments were conducted, and for the ICDSC, n = 346 corresponding DSM-IV-TR and ICDSC assessments were conducted. For the CAM-ICU, the logistic regression model with random effects revealed a sensitivity of 75.7%, a specificity of 97.3%, a PPV of 52.8%, and a NPV of 98.9% (Table 3). For the ICDSC, the model revealed a sensitivity of 73.4%, a specificity of 98.9%, a PPV of 61.2%, and a NPV of 94.6%. Comparison of test validities showed no significant differences. ROC analysis yielded an AUC of 0.893 for the ICDSC and 0.907 for the ssCAM-ICU (Fig. 3c, d) with no significant differences (p = 0.465). The ability of the DSIs to distinguish between patients who were delirium-positive and delirium-negative as measured with the Pietra index was 0.62 for the ICDSC and 0.46 for the ssCAM-ICU. Just like for the first complete assessment series, the difference in Pietra indexes indicates that the ICDSC has a better ability to distinguish between patients who were delirium-positive and delirium-negative.
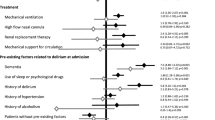
Impact of Patient-Specific Covariates on the Validity of ICDSC and ssCAM-ICU
As shown in Tables 4 and 5, the parametric ROC regression model revealed that only the RASS score had a significantly positive effect on the ROC curve of the ICDSC (coefficient 0.634, p = 0.029), and the ssCAM-ICU (coefficient 0.920, p = 0.004). Thus, higher RASS scores were associated with better test validities of the ICDSC and the ssCAM-ICU. Figure 4 illustrates ROC curves for different RASS scores and shows that for both DSIs, AUCs of ROC curves for sedated patients (RASS − 2) are smaller than for nonsedated patients (RASS − 1 or 0). Neither a neurosurgical intervention nor an acute diagnosis of stroke/TIA had a significant impact on the ROC curves of the ssCAM-ICU or the ICDSC. Results were confirmed by plotting empirical ROC curves for covariates, as depicted in Supplement 2. AUCs of the empirical ROC curves for patients with a RASS score of 0 or − 1 were greater than AUCs of the empirical ROC curves for patients with a RASS score outside this range, whereas AUCs of empirical ROC curves of other covariates, including neurosurgical intervention and acute diagnosis of stroke/TIA, did not show great differences.
ROC regression analysis for the ICDSC (a) and ssCAM-ICU (b) for different RASS scores, including all assessments. All assessments were defined as any assessment pair of DSM-IV-TR and ICDSC or CAM-ICU, respectively. DSM-IV-TR Diagnostic and Statistical Manual, 4th Edition, Text Revision, ICDSC Intensive Care Delirium Screening Checklist, RASS Richmond Agitation Sedation Scale, ROC Receiver operating characteristic, ssCAM-ICU Severity scale Confusion Assessment Method for the Intensive Care Unit
Discussion
In this single-center QI project, we prospectively assessed the diagnostic validity of the most common DSIs CAM-ICU and ICDCS in a neurocritical care population. Taking into account single and multiple testing on one patient, we revealed a moderate to good sensitivity and an excellent specificity in this patient cohort. In a second step, we examined the influence of neurocritical care-specific and general covariates on the diagnostic validities of the CAM-ICU and ICDSC, which revealed a significant influence of the RASS score on the diagnostic performance of the DSIs. Neither acute diagnosis of stroke/TIA or neurosurgical intervention, nor the general covariates sex, age, or mechanical ventilation had a significant impact on DSI validities.
The delirium rate of 29.7% found in this QI project lies within the expected range in patients with neurocritical illness. Previous trials reported a delirium prevalence ranging from 11.8 to 45.9% [10,11,12, 25,26,27]. Variations are most likely because of different compositions of the study populations. For example, Patel et al. [9] found in a systematic review that the incidence of mechanical ventilation varied from less than 10% to more than 60% between studies, and the relationship between ventilator status, severity of illness and prevalence of delirium has previously been described [1].
Regarding the diagnostic validity of the DSIs, our findings are in line with a recently published observational study of 123 neurocritical care patients [14], which revealed a sensitivity and specificity of 66.9% and 93.3% for the CAM-ICU, as well as 69.9% and 93.9% for the ICDCS. In that study, the ICD-10 was used as a reference standard, which is known to be less sensitive in diagnosing delirium than the DSM-IV-TR that was used in our QI project [28]. In addition, the authors report a significant association between a positive DSI and the presence of neurological symptoms, which implies that a positive delirium screening should lead to further neurological diagnostics to delineate if the patient has delirium or another neurological condition. Contrary to their results, our data suggest that the presence of acute stroke or TIA does not diminish diagnostic validity of the DSIs. In fact, the specificity of both DSIs remains excellent.
Patel et al. [9] identified four additional studies that assessed the validity of different DSIs versus a reference standard in patients with neurocritical illness [10,11,12,13]. The CAM-ICU and the ICDSC were most commonly used as DSIs. Two studies using the CAM-ICU against the reference standard DSM-IV and DSM-IV-TR, respectively, revealed a sensitivity of 76.0% and 62%, and a specificity of 98.1% and 74%, respectively [10, 12]. One study that used the ICDSC against the DSM-IV-TR as a reference standard revealed a sensitivity of 64% and a specificity of 79% [10]. Compared with these studies, our data suggest a comparable or slightly better diagnostic validity. The most recently published data in a medical/surgical critical care population exhibit comparable diagnostic validities for the ICDSC and the CAM-ICU [29]. Our observation that diagnostic validity slightly increases if one accounts for multiple testing is also a consistent finding among studies with medical/surgical patients with critical illness [15, 29].
This work adds to current literature that DSI validity is influenced by the same covariates in neurocritical care patients as in medical/surgical critical care patients [15, 29], namely the RASS score. We do not see an effect of neurocritical care-specific covariates, which allows for the conclusion that scores remain valid despite neurological diagnoses or neurosurgical procedures, which contrasts previous findings [14]. However, the number of potential differential diagnoses for a positive DSI in neurocritical care patients exceeds the number of differential diagnoses in medical/surgical ICU patients. This means that diagnoses such as nonconvulsive seizures and intracerebral pathologies are generally observed more frequently compared with the medical/surgical ICU context. This underscores that clinicians should refrain from using DSIs without a full neurological examination to determine whether a patient suffers from delirium or a primary encephalopathy, leading to a false positive DSI result.
This QI project has several limitations. Our patient cohort consisted of a heterogeneous group of patients with neurocritical illness. On the one hand, this can be considered a strength as it does not limit the results to one specific neurocritical care patient subgroup, on the other hand, our study might underestimate the impact of covariates in individual subgroups. Because the project results were in line with previous works, this limitation might be mitigated. In addition, a larger sample size would have increased the precision of our estimates and the statistical power to detect a significant influence of covariates on DSI validity. However, our sample size was comparable to other DSI validation studies [14,15,16, 29]. Furthermore, no detailed neurological examination was performed, which could have identified neurological symptoms or syndromes that show a similar appearance to delirium and therefore cause false positive DSI results. Future studies should therefore take a standardized neurological status to delineate delirium and primary encephalopathies. Ultimately, this is a single-center QI project, which limits its generalizability because center-related effects, such as context-specific SOPs, might influence our results.
Conclusions
In summary, delirium screening in patients with neurocritical illness performs with an adequate diagnostic validity, irrespective of the presence of acute stroke, TIA, or neurosurgical interventions. However, even a very light sedation level significantly impairs DSI performance. Notably, a false positive DSI in neurocritical care patients might be due to different differential diagnoses than that in the medical or surgical critical care population.
Data Availability
Data will be made available from the corresponding author upon a reasonable request.
Abbreviations
- APACHE II:
-
Acute Physiology and Chronic Health Disease Classification System II
- AUC:
-
Area under the curve
- CI:
-
Confidence interval
- CAM-ICU:
-
Confusion Assessment Method for the Intensive Care Unit
- CPR:
-
Cardiopulmonary resuscitation
- DSI:
-
Delirium screening instrument
- DSM-IV-TR:
-
Diagnostic and Statistical Manual, 4th Edition, Text Revision
- GCS:
-
Glasgow Coma Scale
- ICDSC:
-
Intensive Care Delirium Screening Checklist
- ICU:
-
Intensive care unit
- NPV:
-
Negative predictive value
- PPV:
-
Positive predictive value
- RASS:
-
Richmond Agitation Sedation Scale
- ROC curve:
-
Receiver operating characteristics curve
- SAPS II:
-
Simplified Acute Physiology Score II
- SOP:
-
Standard operating procedure
- ssCAM-ICU:
-
Severity Scale Confusion Assessment Method for the Intensive Care Unit
- TIA:
-
Transient ischemic attack
References
Ely EW, Shintani A, Truman B, et al. Delirium as a predictor of mortality in mechanically ventilated patients in the intensive care unit. JAMA. 2004;291(14):1753–62.
Pandharipande PP, Girard TD, Jackson JC, et al. Long-term cognitive impairment after critical illness. N Engl J Med. 2013;369(14):1306–16.
Ely E, Gautam S, Margolin R, et al. The impact of delirium in the intensive care unit on hospital length of stay. Intensive Care Med. 2001;27(12):1892–900.
Devlin JW, Skrobik Y, Gélinas C, et al. Clinical practice guidelines for the prevention and management of pain, agitation/sedation, delirium, immobility, and sleep disruption in adult patients in the ICU. Crit Care Med. 2018;46(9):e825–73.
Baron R, Binder A, Biniek R, et al. Evidence and consensus based guideline for the management of delirium, analgesia, and sedation in intensive care medicine. Revision 2015 (DAS-Guideline 2015)—short version. GMS Ger Med Sci. 2015;13:Doc19.
Ely EW, Margolin R, Francis J, et al. Evaluation of delirium in critically ill patients: validation of the confusion assessment method for the intensive care unit (CAM-ICU). Crit Care Med. 2001;29(7):1370–9.
Devlin JW, Fong JJ, Schumaker G, et al. Use of a validated delirium assessment tool improves the ability of physicians to identify delirium in medical intensive care unit patients. Crit Care Med. 2007;35(12):2721–4.
Gusmao-Flores D, Salluh JIF, Chalhub, R.Á.Quarantini, L.C. . The confusion assessment method for the intensive care unit (CAM-ICU) and intensive care delirium screening checklist (ICDSC) for the diagnosis of delirium: a systematic review and meta-analysis of clinical studies. Crit Care. 2012;16(4):R115.
Patel MB, Bednarik J, Lee P, et al. Delirium monitoring in neurocritically ill patients: a systematic review. Crit Care Med. 2018;46(11):1832–41.
Frenette AJ, Bebawi ER, Deslauriers LC, et al. Validation and comparison of CAM-ICU and ICDSC in mild and moderate traumatic brain injury patients. Intensive Care Med. 2016;42(1):122–3.
Kostalova M, Bednarik J, Mitasova A, et al. Towards a predictive model for post-stroke delirium. Brain Inj. 2012;26(7–8):962–71.
Mitasova A, Kostalova M, Bednarik J, et al. Poststroke delirium incidence and outcomes: validation of the confusion assessment method for the intensive care unit (CAM-ICU). Crit Care Med. 2012;40(2):484–90.
Lees R, Corbet S, Johnston C, et al. Test accuracy of short screening tests for diagnosis of delirium or cognitive impairment in an acute stroke unit setting. Stroke. 2013;44(11):3078–83.
von Hofen-Hohloch J, Awissus C, Fischer MM, et al. Delirium screening in neurocritical care and stroke unit patients: a pilot study on the influence of neurological deficits on CAM-ICU and ICDSC outcome. Neurocrit Care. 2020;33(3):708–17.
Luetz A, Heymann A, Radtke FM, et al. Different assessment tools for intensive care unit delirium: which score to use? Crit Care Med. 2010;38(2):409–18.
Luetz A, Gensel D, Müller J, et al. Validity of different delirium assessment tools for critically ill children: covariates matter*. Crit Care Med. 2016;44(11):2060–9.
DeLong ER, DeLong DM, Clarke-Pearson DL. Comparing the areas under two or more correlated receiver operating characteristic curves: a nonparametric approach. Biometrics. 1988;44(3):837–45.
Verbeke G, Molenberghs G. Linear mixed models for longitudinal data. 2nd ed. New York: Springer; 2000.
Gatsonis CA. Random-effects models for diagnostic accuracy data. Acad Radiol. 1995;2(Suppl 1):S14-21.
Genders TS, Spronk S, Stijnen T, et al. Methods for calculating sensitivity and specificity of clustered data: a tutorial. Radiology. 2012;265(3):910–6.
Newson R. Parameters behind “nonparametric” statistics: Kendall’s tau, Somers’ D and median differences. Stata J. 2002;2(1):45–64.
Harrell FE Jr, Califf RM, Pryor DB, Lee KL, Rosati RA. Evaluating the yield of medical tests. JAMA. 1982;247(18):2543–6.
Lee W-C. Probabilistic analysis of global performances of diagnostic tests: interpreting the Lorenz curve-based summary measures. Stat Med. 1999;18(4):455–71.
Janes H, Pepe MS. Adjusting for covariate effects on classification accuracy using the covariate-adjusted receiver operating characteristic curve. Biometrika. 2009;96(2):371–82.
Rosenthal LJ, Francis BA, Beaumont JL, et al. Agitation, delirium, and cognitive outcomes in intracerebral hemorrhage. Psychosomatics. 2017;58(1):19–27.
Oldenbeuving AW, de Kort PL, Jansen BP, et al. Delirium in the acute phase after stroke: incidence, risk factors, and outcome. Neurology. 2011;76(11):993–9.
Naidech AM, Beaumont JL, Rosenberg NF, et al. Intracerebral hemorrhage and delirium symptoms. Length of stay, function, and quality of life in a 114-patient cohort. Am J Respir Crit Care Med. 2013;188(11):1331–7.
Sepulveda E, Franco JG, Trzepacz PT, et al. Delirium diagnosis defined by cluster analysis of symptoms versus diagnosis by DSM and ICD criteria: diagnostic accuracy study. BMC Psychiatry. 2016;16(1):167.
Nacul FE, Paul N, Spies CD, et al. Influence of sedation level and ventilation status on the diagnostic validity of delirium screening tools in the ICU—an international, prospective, bi-center observational study (IDeAS). Medicina (Kaunas). 2020;56(8):411.
Acknowledgments
We would like to thank the staff of the neuro-ICU for their support of this QI project. Further, we thank Peter Braun und Weronika Lisiuk for their help during data collection. The manuscript complies with the instructions to authors. All authors meet requirements for authorship and approved the final manuscript. The manuscript has not been published else-where and is not under consideration for publication by another journal.
Funding
Open Access funding enabled and organized by Projekt DEAL. This work did not receive any grant from funding agencies in the public, commercial, or not-for-profit sector.
Author information
Authors and Affiliations
Contributions
BW: writing (original draft preparation, review and editing). NP: writing (original draft preparation, reviewing and editing), formal analysis, visualization, and methodology. CDS: conceptualization, methodology, writing (reviewing and editing), supervision, and project administration. DU: writing (original draft preparation, reviewing and editing), data curation, and investigation. IA: writing (reviewing and editing) and investigation. FS: writing (reviewing and editing) and investigation. SW: writing (reviewing and editing) and investigation. AL: conceptualization, methodology, project administration, and writing (reviewing and editing).
Corresponding author
Ethics declarations
Conflicts of Interest
BW reports personal fees from Orion Pharma outside the submitted work. NP, DU, IA, FS and SW declare that they have no conflicts of interest. CDS reports Grants from Drägerwerk AG & Co. KGaA, Grants from Deutsche Forschungsgemeinschaft/German Research Society, Grants from Deutsches Zentrum für Luft- und Raumfahrt e. V. (DLR)/German Aerospace Center, Grants from Einstein Stiftung Berlin/Einstein Foundation Berlin, Grants from Gemeinsamer Bundesausschuss/Federal Joint Committee (G-BA), Grants from Inneruniversitäre Forschungsförderung/Inner University Grants, Grants from Projektträger im DLR/Project Management Agency, Grants from Stifterverband/Nonprofit Society Promoting Science and Education, Grants from WHOCC, Grants from Baxter Deutschland GmbH, Grants from Cytosorbents Europe GmbH, Grants from Edwards Lifesciences Germany GmbH, Grants from Fresenius Medical Care, Grants from Grünenthal GmbH, Grants from Masimo Europe Ltd., Grants from Pfizer Pharma PFE GmbH, personal fees from Georg Thieme Verlag, Grants from Dr. F. Köhler Chemie GmbH, Grants from Sintetica GmbH, Grants from Stifterverband für die deutsche Wissenschaft e.V. Philips Grants from Stiftung Charité, Grants from AGUETTANT Deutschland GmbH, Grants from AbbVie Deutschland GmbH & Co. KG, Grants from Amomed Pharma GmbH, Grants from InTouch Health, Grants from Copra System GmbH, Grants from Correvio GmbH, Grants from Max-Planck-Gesellschaft zur Förderung der Wissenschaften e.V., Grants from Deutsche Gesellschaft für Anästhesiologie & Intensivmedizin (DGAI), Grants from Stifterverband für die deutsche Wissenschaft e.V./Metronic, Grants from Philips Electronics Nederland BV, Grants from BMG, Grants from BMBF, Grants from Deutsche Forschungsgemeinschaft/ German Research Society, outside the submitted work. In addition, CDS has a patent 10 2014 215 211.9 licensed, a patent 10 2018 114 364.8 licensed, a patent 10 2018 110 275.5 licensed, a patent 50 2015 010 534.8 licensed, a patent 50 2015 010 347.7 licensed, and a patent 10 2014 215 212.7 licensed. AL reports personal fees from Hill-Rom, personal fees from Köhler Chemie, personal fees from Philips Healthcare, outside the submitted work. In addition, AL has a patent 10 2014 215 211.9 pending, and a patent 10 2014 215 212.7 pending.
Ethical Approval/Informed Consent
This quality improvement project was performed in adherence to the ethical standards described in the Declaration of Helsinki from 1964 and its later amendments. Scientific publication of the data were approved by the Ethics Committee at Charité – Universitätsmedizin Berlin (EA1/228/15), and informed consent was waived.
Additional information
Publisher's Note
Springer Nature remains neutral with regard to jurisdictional claims in published maps and institutional affiliations.
Supplementary Information
Below is the link to the electronic supplementary material.
Rights and permissions
Open Access This article is licensed under a Creative Commons Attribution 4.0 International License, which permits use, sharing, adaptation, distribution and reproduction in any medium or format, as long as you give appropriate credit to the original author(s) and the source, provide a link to the Creative Commons licence, and indicate if changes were made. The images or other third party material in this article are included in the article's Creative Commons licence, unless indicated otherwise in a credit line to the material. If material is not included in the article's Creative Commons licence and your intended use is not permitted by statutory regulation or exceeds the permitted use, you will need to obtain permission directly from the copyright holder. To view a copy of this licence, visit http://creativecommons.org/licenses/by/4.0/.
About this article
Cite this article
Weiss, B., Paul, N., Spies, C.D. et al. Influence of Patient-Specific Covariates on Test Validity of Two Delirium Screening Instruments in Neurocritical Care Patients (DEMON-ICU). Neurocrit Care 36, 452–462 (2022). https://doi.org/10.1007/s12028-021-01319-9
Received:
Accepted:
Published:
Issue Date:
DOI: https://doi.org/10.1007/s12028-021-01319-9