Abstract
Objective
Current evidence-based guidelines for the management of aneurysmal subarachnoid hemorrhage (aSAH) focus primarily on timing, modality and technique of aneurysm occlusion, and on prevention and treatment of delayed cerebral ischemia. Significant aspects of management in the intensive care unit (ICU) during the later course of aSAH such as ventilation and sedation (VST) remain unaddressed. aSAH patients present unique challenges not accounted for in general ICU recommendations and guidelines, which is why we attempted to further characterize ICU practices in aSAH patients in Germany.
Methods
We conducted a nationwide survey on ICU practices in aSAH in Germany. Secondarily, we assessed the existence of and compliance with current guidelines regarding ICU practices. The questionnaire was designed in interdisciplinary fashion and distributed online through the kwiksurvey® platform (Bristol, UK).
Results
A total of 50 responses were received, accounting for a response rate of 49%. Twenty-one were university hospitals (UH), 23 high-volume centers (HVC), 6 low-volume centers (LVC). Half of the participating centers do not take into consideration WFNS at presentation to indicate ventilation. While 42% of centers rely on the P/F ratio to indicate ventilation, 62% of them have a cutoff value of < 200, and 38% of < 100. While most UH and HVC used propofol for the first phase of sedation (95%), LVC employed benzodiazepines (100%). Sedation deepening was done with ketamine in UH (75%) and HVC (60%), whereas LVC used predominantly clonidine (100%).
Conclusions
Our study clearly demonstrates that attitudes and practices pertaining to ICU management in aSAH are enormously heterogeneous, reflecting the lack of good quality evidence and differing interpretations thereof.
Similar content being viewed by others
Avoid common mistakes on your manuscript.
Introduction
Although mortality rates from aneurysmal subarachnoid hemorrhage (aSAH) declined over the past decades, case fatality remains high [1]. Evidence-based guidelines for the management of aSAH [2,3,4,5] focus primarily on the timing, modality and technique of aneurysm occlusion, and the prevention and treatment of DCI, while many of the problems encountered in the intensive care unit (ICU) during the later course of aSAH are unaddressed. Core aspects of ICU therapy, such as sedation and analgesia, and indication and targets of mechanical ventilation, must be considered and adapted for aSAH patients, for they are only addressed in general ICU recommendations and guidelines [6]. Although general principles apply for most ICU patients, aSAH patients can present unique challenges [3] not accounted for in these general recommendations and guidelines.
An international survey showed great treatment heterogeneity among centers treating patients with aSAH, particularly between North America and Europe, and between high-volume and low-volume centers [7]. A Scandinavian survey on sedation principles and monitoring techniques in patients with severe traumatic brain injury (TBI) and aSAH in neurocritical centers also revealed marked differences among the institutions analyzed [8]. Germany is no exception to the latter: a survey about contemporary management of aSAH revealed variance among centers, but most aspects interrogated pertained to aneurysm occlusion and postinterventional therapy [9].
Given the heterogeneity in practice and the lack of specific guidelines, it is important to better characterize how physicians are approaching intensive care management of aSAH patients, especially when it comes to ventilation and sedation therapy (VST), since these aspects are underappreciated in the literature. The hypothesis of this study is that aSAH treatment strategies most likely vary enormously from center to center. The aim of this study is to characterize the differences in neurocritical care (NCC) strategies of aSAH in Germany. To do so, we conducted a nationwide survey, evaluating distinct key treatment concepts during the ICU stay. We focus on the results of VST and neuromonitoring.
Materials and Methods
Since our aim was to analyze the differences and variability regarding the very basic but scientifically underappreciated treatment aspects of NCC in aSAH undertaken in Germany, we attempted to incorporate questions on indication, execution and treatment goals of VST. Also, current national and international guidelines were reviewed to assess the presence of recommendations on VST in aSAH. Based on these guidelines, a 70-question online survey was designed (kwiksurveys®, Bristol, United Kingdom) to determine NCC practices in aSAH in Germany. The questions were designed in interdisciplinary fashion, aiming to assess six categories of NCC: general department information, ventilation management, sedation management, perceived adverse events (AE) due to VST, monitoring, and surgical interventions during aSAH course. After the primary version of the questionnaire was done, we handed it out to two non-participating intensivists as a test run. After this, the questionnaire was slightly modified and finalized. The full questionnaire can be found in supplemental electronic material, SEM).
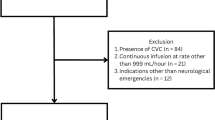
The survey was then distributed per e-mail to intensivists and neurosurgeons from 103 German hospitals. Institutions were primarily identified based on registration with the German Society of Neurological Surgery (“Deutsche Gesellschaft für Neurochirurgie”, DGNC). Private practices and outpatient clinics were excluded. Individuals from the selected institutions were contacted based on their DGNC directory listing, prior personal communication with the senior author, or referral as the primary neurointensivist by the initially approached colleague. The questionnaire was online from June 2, 2017, to January 2, 2018. Follow-up e-mails were sent to non-respondents after 8 weeks. Institutional review board (IRB) approval was obtained. Implied consent was obtained by participating in the survey.
Institutions were categorized in: (a) academic/university hospitals (UH); (b) non-academic high-volume centers (HVC), with ≥ 30 aSAH/year; and (c) non-academic low-volume centers (LVC), with < 30 aSAH/year. ICU run by neurologists and/or neurosurgeons were considered “pure neuro”, whereas ICU run by intensivists, neurosurgeons, and specialists from other non-neurological specialties were considered “interdisciplinary”.
Responses are reported as percentage values of agreement/non agreement and were analyzed for statistically significant differences by means of Pearson’s Chi Square test, assuming significance at a p value of less than .05 (p ≤ .05) using SPSS® Statistics software package (SPSS® v.25, IBM®, Armonk, New York, United States).
Results
Existing VST Guidelines for aSAH
Current ICU management in Germany is guided by the AWMF (Arbeitsgemeinschaft der Wissenschaftlichen Medizinischen Fachgesellschaften, Association of the Scientific Medical Societies in Germany) [6] guidelines, in which ventilation goals and sedation recommendations are summarized. In these guidelines, some special remarks are made pertaining to NCC patients. Additionally, the Brain Trauma Foundation has issued comprehensive guidelines for the management of TBI patients [10], including ventilation and sedation in patients with intracranial hypertension (IHTN). In Table 1, we have summarized the recommendations pertaining to VST, and whether they mention aSAH patients.
Survey
A total of 50 responses were received, accounting for a response rate of 49%. Due to the length and plurality of the survey, we will report on and discuss the most important findings. Because it was not mandatory to respond to all questions, some items have a lower response rate; this is stated whenever pertinent.
Generalizability and Representativeness
Twenty-one UH, 23 HVC and 6 LVC answered the questionnaire and thus constitute the sample. The answers of the participating centers represent 63% of the treatment volume of aSAH in Germany, based on an incidence of aSAH of 7.5/100.000/year and the aSAH caseload in the reporting institutions.
Hospital Characteristics
Most survey participants were HVC n = 23/50 (46%) followed by UH n = 21/50 (42%), and LVC n = 6/50 (12%). In terms of ICU structure, most centers were led in interdisciplinary fashion (mixed-ICU; n = 42/50 (84%), with pure neuro-ICUs n = 8/50 (16%) being mostly represented in UH n = 5/8 (62%), where they accounted for n = 5/21 (24%) of all ICUs. Because of the great heterogeneity of the group sizes between interdisciplinary ICUs and neuro-ICUs, we refrained from making any further statistical analyses between these two groups to avoid type II error.
Ventilation Management and Indications for Tracheostomy
Most centers do not have strictly defined cutoff values to indicate ventilation in aSAH, as illustrated in Fig. 1. Nearly half of the centers answered that the modified Fisher score is a potential reason to indicate mechanical ventilation. More than half of the centers n = 26/45 (58%) do not include the P/F ratio to objectify the level of pulmonary insufficiency. If the P/F ratio is used, more than one third of all centers tend to intubate relatively late (P/F ratio < 100 mmHg).
Indications for ventilation in the interrogated centers. All participating institutions were asked if WFNS grade, modified Fisher score, P/F ratio, cerebral vasospasm or cardiac involvement, as determined by PiCCO or echocardiography, were indications for ventilation. HVC high-volume centers, LVC low-volume centers, UH university hospitals
Normocapnia and normoxia are strived for by most reporting centers (n = 42/45 (93%); n = 22/46 (48%), respectively), but great variability was seen in their target paO2, as opposed to a fair consensus regarding target paCO2, as illustrated in Table 2.
No consensus was seen regarding tracheostomy: of n = 37/50 (74%) reporting centers, n = 17/37 (46%) perform late tracheostomies after 10 days, whereas n = 16/37 (43%) perform them between days 3–10, and n = 4/37 (11%) do so before day 3 (p = 0.064).
Monitoring
With regards to monitoring, most centers rely on the Richmond agitation and sedation scale (RASS) n = 30/42 (71%) and intracranial pressure (ICP) values n = 24/42 (57%) to assess sedation levels. Invasive ICP monitoring is performed by either an intraparenchymal ICP probe n = 35/44 (79%) and/or external ventricular drainage n = 39/44 (89%). Most centers also manage blood pressure in accordance to cerebral perfusion pressure (CPP) n = 37/41 (90%), but heterogeneity was observed in CPP target values both within and between the groups, as illustrated in Table 3. The use of advanced hemodynamic monitoring by means of pulse contour cardiac output (PiCCO) was mainly reported by UH n = 8/20 (40%) and HVC n = 8/20 (40%). Brain tissue oxygen (PtiO2) was reported exclusively in UH n = 10/20 (50%) and HVC n = 3/20 (15%).
Sedation Management
Most centers n = 46/50 (92%) reported on the amount of aSAH patients undergoing VST: in n = 21/46 (46%) of centers, > 50% of their aSAH patients undergo VST. Most institutions n = 44/50 (88%) reported on the drugs used for the first phase of sedation therapy. As illustrated in Fig. 2, heterogeneity was seen both within and between UH, HVC and LVC. While propofol appears to be used by the majority n = 41/44 (93%), it is variably combined with opiates, benzodiazepines and ketamine. First-line sedative for the maintenance of sedation was reported by n = 38/50 (74%) of the participating institutions; here, great variability was seen both within and between UH, HVC and LVC. Only one UH n = 1/38 (3%) reported on the use of volatile sedatives for the maintenance of sedation (Fig. 3). There appears to be no consensus with regards to the type of drug employed to deepen sedation level among the n = 43/50 (84%) reporting institutions (Fig. 4). UH and HVC reported the use of barbiturates more frequently than LVC to deepen sedation level (p = .297). Most institutions reporting on the maximum number of sedatives used n = 33/43 (77%) routinely employ three or more medications, with no statistically significant difference between UH, HVC and LVC (p = 0.851). The drug dosages used for sedation are also largely variable, as illustrated by two examples in Fig. 5.
Drugs used for the first phase of sedation in the interrogated centers, stratified by center type. While great variability was observed, most centers appear to use a combination of propofol and opiates to induce sedation in aSAH patients. HVC high-volume centers, LVC low-volume centers, UH university hospitals
Drugs used for the maintenance of sedation in the interrogated centers, stratified by center type. While great variability was observed, most centers appear to use a combination of propofol, midazolam and sufentanil to maintain sedation in aSAH patients. Only one UH employs inhalational anesthetics to maintain sedation in this patient population. HVC high-volume centers, LVC low-volume centers, UH university hospitals
Variability of the maximum dosages of midazolam and sufentanil. Maximum dosages of midazolam vary by a factor of 8.5 (smallest “maximum” dosage = 7 mg/h, largest “maximum” dosage = 60 mg/h), while maximum dosages of the opioid sufentanil vary by a factor of 62.5 (smallest “maximum” dosage = 40 µg/h, largest “maximum” dosage > 2500 µg/h
Discussion
While evidence-based guidelines for aneurysm occlusion and the detection and prevention of DCI in the setting of aSAH have been published [2, 4], NCC of this patient population is less well standardized. As summarized in Table 3, most guidelines fail to make specific recommendations regarding NCC management of aSAH patients. The Neurocritical Care Society attempted to overcome this gap by issuing a multidisciplinary consensus conference (NCCSMCC) in 2011 [3]. Here, management of DCI and systemic complications were addressed, but an essential part of NCC, VST, was completely left unmentioned. Almost half of aSAH patients undergo VST, as evinced in our survey, making this a formidable gap in patient care. In this study, we found great heterogeneity in all aspects analyzed, possibly reflecting this lack of guidelines and/or published expert consensus.
Ventilation and Indications for Tracheostomy
Evidence regarding ventilation therapy in aSAH patients is practically non-existant; there are German national guidelines for invasive ventilation [6], but they do not consider the particular challenges of ventilation in the aSAH population. The guidelines of the Brain Trauma Foundation also comment on ventilation therapy, but for patients with severe TBI [10]. Both guidelines might be partially adoptable for indicating, adjusting and steering ventilation in aSAH patients, but they were not issued taking into consideration the specific needs of this population.
In TBI, prior guidelines recommended hyperventilation as a temporizing measure for the reduction of elevated ICP. However, the most recent guidelines for TBI issued by The Brain Trauma Foundation have revised this notion and currently advocate for normoventilation. Some survey respondents reported target hyperventilation. This practice is particularly concerning given that hyperventilation has been shown to exacerbate DCI in cases of aSAH due to additional vasoconstriction [11, 12], thus rendering the extrapolation of now outdated TBI guidelines for aSAH potentially dangerous. Additionally, most centers reported a narrow corridor for their target paCO2 between 35 and 45 mmHg. However, recent evidence has exhibited potential benefits of controlled hypercapnia in patients with aSAH, for paCO2 > 60 mmHg has been shown to increase cerebral blood flow (CBF) and thus possibly prevent DCI [13]. Therefore, consideration of patient-tailored paCO2/CBF is important.
Regarding tracheostomy, no consensus in its indication was observed among the reporting centers. A recent meta-analysis [14] on early versus late tracheostomy in patients with early brain injury (EBI) suggested reductions in mortality and ICU length of stay favoring early tracheostomy. On the other hand, the SETPOINT trial [15], conducted on 60 patients with different forms of severe stroke, showed reduced use of sedatives and ICU mortality favoring early tracheostomy. However, this study was not powered to assess these secondary endpoints, and its successor SETPOINT2 [16] is still underway. A subgroup analysis of aSAH patients enrolled in SETPOINT2 might yield higher quality evidence pertaining to the optimal timepoint for tracheostomy in aSAH. However, no controlled trials have assessed the optimal timing of tracheotomy in aSAH patients, and guidelines fail to address this point as well, thus providing an explanation for the heterogeneity in the answers received in our survey.
Monitoring
In accordance with the International Multidisciplinary Consensus Conference on Multimodality Monitoring (IMCCMM) [13], most centers perform ICP monitoring, either by an intraparenchymal probe and/or EVD. Additionally, most surveyed centers employ RASS to monitor sedation level in their aSAH patients. RASS is the only diagnostic tool to evaluate both sedation level and agitation/delirium that has been validated for NCC patients and that has been shown to provide reliable information when assessing aSAH patients [17].
Multimodality monitoring was almost exclusively used by UH and HVC. On the one hand, both the American Heart Association (AHA) guidelines for the management of aSAH [2] and the Neurocritical Care Society consensus [3] recommend advanced hemodynamic monitoring using thermodilution methods in unstable aSAH patients. On the other hand, monitoring cerebral oxygenation in high-grade aSAH patients can provide valuable information and warn of impending DCI and/or infarction [18]. Additionally, IMCCMM [13] recommends the use of multimodality monitoring in poor-grade aSAH. Failure to adhere to these recommendations and to employ these adjuncts in LVC might have a detrimental effect on patient outcome and should be critically evaluated on a national level to ensure patient safety.
Another striking finding in our survey was the great heterogeneity in CPP targets reported by centers. While CPP-oriented therapy has proven to be efficient in TBI, with guidelines recommending CPP maintenance between 60 and 70 mmHg [10], recent studies have emphasized the importance of targeting the optimal CPP (CPPopt) for each patient based on their unique autoregulation, as estimated by the pressure reactivity index (PRx) [19]. In the setting of poor-grade aSAH, CPP values below 70 mmHg have been associated with poor functional recovery and brain tissue hypoxia [20], but CPPopt is also emerging as a potentially useful tool in the diagnosis and treatment of DCI [21]. Evidently, further studies are needed to guide CPP management in aSAH, and further recommendations in this regard should be incorporated into national and international guidelines.
Sedation
Our survey revealed great heterogeneity in the choice of medications used for sedation irrespective of center caseload, but we were able to identify some commonalities. Firstly, propofol was the most commonly used drug for the first phase of sedation therapy and maintenance in surveyed centers. This drug has become an extremely popular sedative in NCC, as it has a rapid onset and a short duration of action, thus allowing for “daily sedation interruption” (DSI) and regular neurological examinations.
Similarly, midazolam was one of the most commonly used drugs to maintain sedation. This GABAergic drug has an established role in the management of IHTN in TBI [10], which could possibly explain its use in the aSAH patient population as an extrapolation of the TBI experience. The use of both these drugs has been commented on in the most current guidelines for TBI [10], but the evidence behind them does not suffice for the investigators to make a recommendation on them. In our national guidelines for VST [6], both drugs are regarded with equipoise, but the administration of propofol is recommended over midazolam in case of desired prompt neurological evaluation.
Another drug commonly used for sedation maintenance in our survey was sufentanil. One could hypothesize that both propofol and sufentanil are popular due to their short duration of action and the ability to perform DSI, which is also mentioned as one of their advantages in our national guidelines [6]. However, in a meta-analysis evaluating sedation protocols versus DSI, no statistically significant differences were observed regarding patient outcome [22].
Sedation Deepening
When interrogated on sedation deepening, most UH und HVC reported the use of ketamine. German national guidelines [6] comment amply about the use of ketamine in patients with TBI and IHTN; most of their recommendations are classified as “could do”, and do not have a binding character. Nonetheless, there is emerging data in the literature advocating for the use of ketamine in aSAH [23, 24], as it has been associated with a lower incidence of DCI-related infarctions and lower ICP in aSAH patients. Interestingly, LVC resort to clonidine for the deepening of sedation. This drug fails to find mention in national guidelines and the evidence supporting its use in the ICU is very scarce [25].
Another interesting finding of our survey regarding sedation deepening was the establishment of barbiturate coma in UH and HVC, but not in LVC. TBI guidelines recommend sedation deepening with these drugs for refractory IHTN [10]. In aSAH, barbiturates have been shown to reduce refractory symptomatic vasospasm [26], underscoring their potential role in the management of aSAH beyond ICP control.
Similarly, only one UH reported the use of inhalational anesthetics as first-line therapy to maintain sedation, and the use of volatile sedation was more common in UH than in HVC/LVC. Guidelines fail to mention the use of inhalational anesthetics in aSAH or NCC, and this form of anesthesia can be considered experimental in this setting, as there are only smaller studies evaluating it in aSAH to date [27, 28].
In sum, our survey revealed that most UH and HVC manage sedation in similar fashion, incorporating more recent evidence pertaining to the specific pharmacological effects of different drugs in aSAH. On the contrary, LVC adhere to general guidelines and extrapolate TBI ones in their drug selection.
Future Directions
Based on the results obtained, we have identified several questions that, in our opinion, merit the development of randomized-controlled trials and/or expert consensus guidelines to both homogenize and improve patient treatment in this devastating condition:
-
Optimal sedatives in the setting of aSAH, pertaining not only to ICP and cerebral metabolism control, but also to the reduction of DCI and poor patient outcome.
-
Ventilator settings and goals of ventilation therapy in aSAH.
-
Timing of tracheostomy in aSAH patients.
Limitations
Results obtained from a voluntary survey should be interpreted with caution. One of the main drawbacks of a survey is its susceptibility to both selection and recall biases, as it relies on self-report and cannot be controlled for its accuracy. In our study in particular, survey answers might have been skewed one way or another depending on the subspecialty of the reporting colleague (intensivist vs neurosurgeon vs neurologist), thus reflecting their personal preferences with regards to drug selection for sedation and preferred ventilator parameters, and not their institutional average at large. Furthermore, colleagues might have interpreted questions differently and understood “sedation induction”/“first phase of sedation” and “sedation deepening” in differing ways, for instance.
The overall response rate to our survey was high, at nearly 50%. Based on their reported treatment volume and the incidence of aSAH in Germany, we calculated the representativeness of our results to be at 63% of the treatment volume of aSAH in Germany. While these figures appear high, a subset of questions was answered only by some of the participating centers, thus lowering the overall generalizability of our results. The length of our survey, with 70 questions, might have been a deterring factor influencing survey completion.
Another aspect that might limit generalizability of our results is differing treatment protocols and available medications in other countries: different benzodiazepines and opioids might be used in other parts of the world with greater predilection than in Germany.
Conclusions
Our study demonstrates that attitudes and practices pertaining to NCC in aSAH are heterogeneous, possibly reflecting the lack of good quality evidence and differing interpretations thereof. We observed some extrapolation of TBI guidelines for the management of aSAH, such as thresholds for ventilation and target CPP in some centers, but the pathophysiology of both entities is completely different. Failing that, expert consensus statements would greatly contribute to guiding NCC of aSAH.
References
Cross DT, Tirschwell DL, Clark MA, et al. Mortality rates after subarachnoid hemorrhage: variations according to hospital case volume in 18 states. J Neurosurg. 2003;99:810.
Connolly ES, Rabinstein AA, Carhuapoma JR, et al. Guidelines for the management of aneurysmal subarachnoid hemorrhage. Stroke. 2012;43:1711–37.
Diringer MN, Bleck TP, Claude Hemphill J, et al. Critical care management of patients following aneurysmal subarachnoid hemorrhage: recommendations from the neurocritical care society’s multidisciplinary consensus conference. Neurocrit Care. 2011;15:211.
Steiner T, Juvela S, Unterberg A, Jung C, Forsting M, Rinkel G. European stroke organization guidelines for the management of intracranial aneurysms and subarachnoid haemorrhage. Cerebrovasc Dis. 2013;35:93–112.
Meurer WJ, Walsh B, Vilke GM, Coyne CJ. Clinical guidelines for the emergency department evaluation of subarachnoid hemorrhage. J Emerg Med. 2016;50:696–701.
Martin J, Heymann A, Bäsell K, et al. Evidence and consensus-based German guidelines for the management of analgesia, sedation and delirium in intensive care-short version. Ger Med Sci. 2010. https://doi.org/10.3205/000091.
Stevens RD, Naval NS, Mirski MA, Citerio G, Andrews PJ. Intensive care of aneurysmal subarachnoid hemorrhage: an international survey. Intensive Care Med. 2009;35:1556–66.
Skoglund K, Enblad P, Marklund N. Monitoring and sedation differences in the management of severe head injury and subarachnoid hemorrhage among neurocritical care centers. J Neurosci Nurs. 2013;45:360–8.
Sakowitz OW, Raabe A, Vucak D, Kiening KL, Unterberg AW. Contemporary management of aneurysmal subarachnoid hemorrhage in Germany: results of a survey among 100 neurosurgical departments. Neurosurgery. 2006;58:137–45.
Carney N, Totten AM, O’Reilly C, et al. Guidelines for the management of severe traumatic brain injury, Fourth Edition. Neurosurgery. 2016;80:6–15.
Curley G, Kavanagh BP, Laffey JG. Hypocapnia and the injured brain: more harm than benefit. Crit Care Med. 2010;38:1348–59.
Westermaier T, Stetter C, Kunze E, et al. Controlled hypercapnia enhances cerebral blood flow and brain tissue oxygenation after aneurysmal subarachnoid hemorrhage: results of a phase 1 study. Neurocrit Care. 2016;25:205–14.
Helbok R, Olson DM, Le Roux PD, Vespa P. Monitoring TPitIMCCoM. intracranial pressure and cerebral perfusion pressure monitoring in non-TBI patients: special considerations. Neurocritical Care. 2014;21:85–94.
McCredie VA, Alali AS, Scales DC, et al. Effect of early versus late tracheostomy or prolonged intubation in critically ill patients with acute brain injury: a systematic review and meta-analysis. Neurocrit Care. 2017;26:14–25.
Bosel J, Schiller P, Hook Y, et al. Stroke-related early tracheostomy versus prolonged orotracheal intubation in neurocritical care trial (SETPOINT): a randomized pilot trial. Stroke. 2013;44:21–8.
Schonenberger S, Niesen WD, Fuhrer H, et al. Early tracheostomy in ventilated stroke patients: study protocol of the international multicentre randomized trial SETPOINT2 (stroke-related early tracheostomy vs. prolonged orotracheal intubation in neurocritical care trial 2). Int J Stroke Off J Int Stroke Soc. 2016;11:368–79.
Riker RR, Fugate JE. Monitoring AtPitIM-dCCoM. Clinical monitoring scales in acute brain injury: assessment of coma, pain, agitation, and delirium. Neurocritical Care. 2014;21:27–37.
Sarrafzadeh AS, Vajkoczy P, Bijlenga P, Schaller K. Monitoring in neurointensive care—the challenge to detect delayed cerebral ischemia in high-grade aneurysmal ASAH. Front Neurol. 2014;5:134.
Kramer AH, Couillard PL, Zygun DA, Aries MJ, Gallagher CN. Continuous assessment of “optimal” cerebral perfusion pressure in traumatic brain injury: a cohort study of feasibility, reliability, and relation to outcome. Neurocrit Care. 2019;30:51–61.
Schmidt JM, Ko SB, Helbok R, et al. Cerebral perfusion pressure thresholds for brain tissue hypoxia and metabolic crisis after poor-grade subarachnoid hemorrhage. Stroke. 2011;42:1351–6.
Bijlenga P, Czosnyka M, Budohoski KP, et al. “Optimal cerebral perfusion pressure” in poor grade patients after subarachnoid hemorrhage. Neurocrit Care. 2010;13:17–23.
Nassar Junior AP, Park M. Protocolos de sedação versus interrupção diária de sedação: uma revisão sistemática e metanálise. Revis Bras de Ter Intensiva. 2016;28:444–51.
Carlson AP, Abbas M, Alunday RL, Qeadan F, Shuttleworth CW. Spreading depolarization in acute brain injury inhibited by ketamine: a prospective, randomized, multiple crossover trial. J Neurosurg. 2018;130:1513.
Von der Brelie C, Seifert M, Rot S, et al. Sedation of patients with acute aneurysmal subarachnoid hemorrhage with ketamine is safe and might influence the occurrence of cerebral infarctions associated with delayed cerebral ischemia. World Neurosurg. 2017;97:374–82.
Jamadarkhana S, Gopal S. Clonidine in adults as a sedative agent in the intensive care unit. J Anaesthesiol Clin Pharmacol. 2010;26(4):439–45.
Heo DH, Hu C, Cho SM, Whang K, Pyen JS, Kim HJ. Barbiturate coma therapy in severe and refractory vasospasm following subarachnoid hemorrhage. J Korean Neurosurg Soc. 2003;33:142–8.
Purrucker JC, Renzland J, Uhlmann L, et al. Volatile sedation with sevoflurane in intensive care patients with acute stroke or subarachnoid haemorrhage using AnaConDa: an observational study. Br J Anaesth. 2015;114:934–43.
Villa F, Iacca C, Molinari AF, et al. Inhalation versus endovenous sedation in subarachnoid hemorrhage patients: effects on regional cerebral blood flow*. Crit Care Med. 2012;40:2797–804.
Author information
Authors and Affiliations
Contributions
SH-D: Data analysis, manuscript conception and writing; CS: Data collection and figure creation; JS: Study design; OM: Data analysis, manuscript redaction; VR: Study design, manuscript redaction; DM: Manuscript redaction; CB: Study conception, data anaylsis, study design, manuscript conception and writing.
Corresponding author
Ethics declarations
Conflict of interest
The authors declare that they have no conflicts of interest.
Additional information
Publisher's Note
Springer Nature remains neutral with regard to jurisdictional claims in published maps and institutional affiliations.
Electronic supplementary material
Below is the link to the electronic supplementary material.
Rights and permissions
About this article
Cite this article
Hernández-Durán, S., Salfelder, C., Schaeper, J. et al. Mechanical Ventilation, Sedation and Neuromonitoring of Patients with Aneurysmal Subarachnoid Hemorrhage in Germany: Results of a Nationwide Survey. Neurocrit Care 34, 236–247 (2021). https://doi.org/10.1007/s12028-020-01029-8
Published:
Issue Date:
DOI: https://doi.org/10.1007/s12028-020-01029-8