Abstract
Background and Aims
The relationship between serum lipid level and clinical outcome after spontaneous intracerebral hemorrhage (ICH) remains controversial. We sought to evaluate the association of serum lipid levels with clinical outcomes in patients with ICH.
Methods
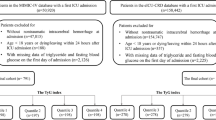
Data on consecutive patients hospitalized with spontaneous ICH were prospectively collected from May 2005 to May 2018 and retrospectively analyzed. Following clinical and demographic data, age and gender, risk factors, serum lipid levels [total cholesterol, triglycerides (TG), low-density lipoprotein (LDL), and high-density lipoprotein (HDL) cholesterol] and the outcomes were analyzed.
Results
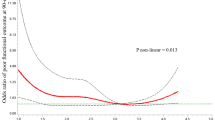
A total of 1451 patients with ICH (mean age, 60.41 ± 12.3 years; 32.6% women) was evaluated. Although admission TG levels were associated with the outcomes at hospital discharge and 3 months in initial univariate analyses, the former association did not retain its statistical significance in multivariate logistic regression analyses adjusting for potential confounders. However, lower admission TG levels were independently associated (p = 0.045) with a higher likelihood of 12-month unfavorable outcomes (odds ratio 0.91, 95% confidence interval 0.83–0.99) in multivariate logistic regression models.
Conclusions
Low TG levels at hospital admission were an independent predictor for unfavorable long-term outcomes in patients with spontaneous ICH. The exact mechanisms of the association need further investigations.

Similar content being viewed by others
References
Krishnamurthi RV, Feigin VL, Forouzanfar MH, et al. Global and regional burden of first-ever ischaemic and haemorrhagic stroke during 1990–2010: findings from the Global Burden of Disease Study 2010. Lancet Glob Health. 2013;1:e259–81.
Jolink WM, Klijn CJ, Brouwers PJ, Kappelle LJ, Vaartjes I. Time trends in incidence, case fatality, and mortality of intracerebral hemorrhage. Neurology. 2015;85:1318–24.
Mozaffarian D, Benjamin EJ, Writing Group M, et al. Heart disease and stroke statistics-2016 update: a report from the American Heart Association. Circulation. 2016;133:e38–360.
Freiberg JJ, Tybjaerg-Hansen A, Jensen JS, Nordestgaard BG. Nonfasting triglycerides and risk of ischemic stroke in the general population. JAMA. 2008;300:2142–52.
Shahar E, Chambless LE, Rosamond WD, et al. Plasma lipid profile and incident ischemic stroke: the Atherosclerosis Risk in Communities (ARIC) study. Stroke. 2003;34:623–31.
Navar AM. The evolving story of triglycerides and coronary heart disease risk. JAMA. 2019;321:347–9.
Wieberdink RG, Poels MM, Vernooij MW, et al. Serum lipid levels and the risk of intracerebral hemorrhage: the Rotterdam Study. Arterioscler Thromb Vasc Biol. 2011;31:2982–9.
Lei C, Lin S, Wu B, Li H, Liu M, You C. Lipid levels are regionally associated with cerebral microbleeds in patients with intracerebral hemorrhage. J Stroke Cerebrovasc Dis. 2014;23:1195–8.
Roquer J, Rodriguez Campello A, Gomis M, Ois A, Munteis E, Bohm P. Serum lipid levels and in-hospital mortality in patients with intracerebral hemorrhage. Neurology. 2005;65:1198–202.
Zhou JF, Wang JY, Luo YE, Chen HH. Influence of hypertension, lipometabolism disorders, obesity and other lifestyles on spontaneous intracerebral hemorrhage. Biomed Environ Sci. 2003;16:295–303.
Zia E, Pessah-Rasmussen H, Khan FA, et al. Risk factors for primary intracerebral hemorrhage: a population-based nested case-control study. Cerebrovasc Dis. 2006;21:18–25.
Akoudad S, Ikram MA, Portegies ML, et al. Genetic loci for serum lipid fractions and intracerebral hemorrhage. Atherosclerosis. 2016;246:287–92.
Chang JJ, Katsanos AH, Khorchid Y, et al. Higher low-density lipoprotein cholesterol levels are associated with decreased mortality in patients with intracerebral hemorrhage. Atherosclerosis. 2018;269:14–20.
Messe SR, Pervez MA, Smith EE, et al. Lipid profile, lipid-lowering medications, and intracerebral hemorrhage after tPA in get with the guidelines-stroke. Stroke. 2013;44:1354–9.
Hatano S. Experience from a multicentre stroke register: a preliminary report. Bull World Health Organ. 1976;54:541–53.
Banks JL, Marotta CA. Outcomes validity and reliability of the modified Rankin scale: implications for stroke clinical trials: a literature review and synthesis. Stroke. 2007;38:1091–6.
Wang X, Dong Y, Qi X, Huang C, Hou L. Cholesterol levels and risk of hemorrhagic stroke: a systematic review and meta-analysis. Stroke. 2013;44:1833–9.
Xie L, Wu W, Chen J, et al. Cholesterol levels and hemorrhagic stroke risk in East Asian versus non-East Asian populations: a systematic review and meta-analysis. Neurologist. 2017;22:107–15.
Sturgeon JD, Folsom AR, Longstreth WT Jr, Shahar E, Rosamond WD, Cushman M. Risk factors for intracerebral hemorrhage in a pooled prospective study. Stroke. 2007;38:2718–25.
Bonaventure A, Kurth T, Pico F, et al. Triglycerides and risk of hemorrhagic stroke vs. ischemic vascular events: the Three-City Study. Atherosclerosis. 2010;210:243–8.
Romero JR, Preis SR, Beiser A, et al. Risk factors, stroke prevention treatments, and prevalence of cerebral microbleeds in the Framingham Heart Study. Stroke. 2014;45:1492–4.
Noda H, Iso H, Irie F, et al. Low-density lipoprotein cholesterol concentrations and death due to intraparenchymal hemorrhage: the Ibaraki Prefectural Health Study. Circulation. 2009;119:2136–45.
Wang DN, Hou XW, Yang BW, Lin Y, Shi JP, Wang N. Quantity of cerebral microbleeds, antiplatelet therapy, and intracerebral hemorrhage outcomes: a systematic review and meta-analysis. J Stroke Cerebrovasc Dis. 2015;24:2728–37.
Lin WM, Yang TY, Weng HH, et al. Brain microbleeds: distribution and influence on hematoma and perihematomal edema in patients with primary intracerebral hemorrhage. Neuroradiol J. 2013;26:184–90.
Konishi M, Iso H, Komachi Y, et al. Associations of serum total cholesterol, different types of stroke, and stenosis distribution of cerebral arteries. The Akita Pathology Study. Stroke. 1993;24:954–64.
Silveira A, Karpe F, Johnsson H, Bauer KA, Hamsten A. In vivo demonstration in humans that large postprandial triglyceride-rich lipoproteins activate coagulation factor VII through the intrinsic coagulation pathway. Arterioscler Thromb Vasc Biol. 1996;16:1333–9.
Moor E, Silveira A, van’t Hooft F, et al. Coagulation factor VII mass and activity in young men with myocardial infarction at a young age. Role of plasma lipoproteins and factor VII genotype. Arterioscler Thromb Vasc Biol. 1995;15:655–64.
Ghaddar HM, Folsom AR, Aleksic N, et al. Correlation of factor VIIa values with factor VII gene polymorphism, fasting and postprandial triglyceride levels, and subclinical carotid atherosclerosis. Circulation. 1998;98:2815–21.
Priglinger M, Arima H, Anderson C, Krause M, Investigators I. No relationship of lipid-lowering agents to hematoma growth: pooled analysis of the intensive blood pressure reduction in acute cerebral hemorrhage trials studies. Stroke. 2015;46:857–9.
Mustanoja S, Strbian D, Putaala J, et al. Association of prestroke statin use and lipid levels with outcome of intracerebral hemorrhage. Stroke. 2013;44:2330–2.
Funding
No funding supports our research.
Author information
Authors and Affiliations
Contributions
QL: study concept and design, acquisition of data, analysis and interpretation, writing of the manuscript, critical revision of the manuscript for important intellectual content; WJZ, YH, YHX: analysis and interpretation, critical revision of the manuscript for important intellectual content; GEZ: study concept and design, analysis and interpretation, critical revision of the manuscript for important intellectual content.
Corresponding author
Ethics declarations
Conflict of interest
The authors declare that the research was conducted in the absence of any commercial or financial relationships that could be construed as a potential conflict of interest.
Ethical Approval/Informed Consent
The study protocol was approved by the Ethics Committee for Medical Research at Tianjin Huanhu Hospital, and each participant recruited to the study provided informed consent.
Additional information
Publisher's Note
Springer Nature remains neutral with regard to jurisdictional claims in published maps and institutional affiliations.
Rights and permissions
About this article
Cite this article
Liu, Q., Zhao, W., Xing, Y. et al. Low Triglyceride Levels are Associated with Unfavorable Outcomes in Patients with Spontaneous Intracerebral Hemorrhage. Neurocrit Care 34, 218–226 (2021). https://doi.org/10.1007/s12028-020-01023-0
Published:
Issue Date:
DOI: https://doi.org/10.1007/s12028-020-01023-0