Abstract
Background
There are a range of opinions on the benefits and thresholds for the transfusion of red blood cells in critically ill patients with traumatic brain injury (TBI) and an urgent need to understand the neurophysiologic effects. The aim of this study was to examine the influence of red blood cell transfusions on cerebral tissue oxygenation (SctO2) in critically ill TBI patients.
Methods
This prospective observational study enrolled consecutive TBI patients with anemia requiring transfusion. Cerebral tissue oxygen saturation (SctO2) was measured noninvasively with bilateral frontal scalp probes using near-infrared spectroscopy (NIRS) technology. Data were collected at baseline and for 24 h after transfusion. The primary outcome was the applicability of a four-wavelength near-infrared spectrometer to monitor SctO2 changes during a transfusion. Secondary outcomes included the correlation of SctO2 with other relevant physiological variables, the dependence of SctO2 on baseline hemoglobin and transfusion, and the effect of red blood cell transfusion on fractional tissue oxygen extraction.
Results
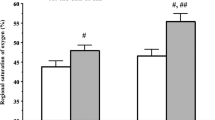
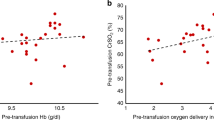
We enrolled 24 patients with severe TBI, of which five patients (21 %) were excluded due to poor SctO2 signal quality from large subdural hematomas and bifrontal decompressive craniectomies. Twenty transfusions were monitored in 19 patients. The mean pre- and post-transfusion hemoglobin concentrations were significantly different [74 g/L (SD 8 g/L) and 84 g/L (SD 9 g/L), respectively; p value <0.0001]. Post-transfusion SctO2 was not significantly greater than pre-transfusion SctO2 [left-side pre-transfusion 69 % (SD 7) vs. post-transfusion 70 % (SD 10); p = 0.68, and right-side pre-transfusion 69 % (SD 5) vs. post-transfusion 71 % (SD 7); p = 0.11]. In a multivariable mixed linear analysis, mean arterial pressure was the only variable significantly associated with a change in SctO2.
Conclusions
The bifrontal method of recording changes in NIRS signal was not able to detect a measurable impact on SctO2 in this sample of patients receiving red blood cell transfusion therapy in a narrow but conventionally relevant, range of anemia.


Similar content being viewed by others
References
Zauner A, Daugherty WP, Bullock MR, Warner DS. Brain oxygenation and energy metabolism: part I-biological function and pathophysiology. Neurosurgery. 2002;51:289–301 (discussion 2).
Chesnut RM, Marshall LF, Klauber MR, et al. The role of secondary brain injury in determining outcome from severe head injury. J Trauma. 1993;34:216–22.
McHugh GS, Engel DC, Butcher I, et al. Prognostic value of secondary insults in traumatic brain injury: results from the IMPACT study. J Neurotrauma. 2007;24:287–93.
Bratton SL, Chestnut RM, Ghajar J, et al. Guidelines for the management of severe traumatic brain injury. X. Brain oxygen monitoring and thresholds. J Neurotrauma. 2007;24(Suppl 1):S65–70.
Bratton SL, Chestnut RM, Ghajar J, et al. Guidelines for the management of severe traumatic brain injury. I. Blood pressure and oxygenation. J Neurotrauma. 2007;24(Suppl 1):S7–13.
Kiraly LN, Underwood S, Differding JA, Schreiber MA. Transfusion of aged packed red blood cells results in decreased tissue oxygenation in critically injured trauma patients. J Trauma. 2009;67:29–32.
Salim A, Hadjizacharia P, DuBose J, et al. Role of anemia in traumatic brain injury. J Am Coll Surg. 2008;207:398–406.
Warner MA, O’Keeffe T, Bhavsar P, et al. Transfusions and long-term functional outcomes in traumatic brain injury. J Neurosurg. 2010;113:539–46.
McIntyre LA, Fergusson DA, Hutchison JS, et al. Effect of a liberal versus restrictive transfusion strategy on mortality in patients with moderate to severe head injury. Neurocrit Care. 2006;5:4–9.
Boutin A, Chasse M, Shemilt M, et al. Red blood cell transfusion in patients with traumatic brain injury: a systematic review and meta-analysis. Transfus Med Rev. 2016;30:15–24.
Zygun DA, Nortje J, Hutchinson PJ, Timofeev I, Menon DK, Gupta AK. The effect of red blood cell transfusion on cerebral oxygenation and metabolism after severe traumatic brain injury. Crit Care Med. 2009;37:1074–8.
Smith MJ, Stiefel MF, Magge S, et al. Packed red blood cell transfusion increases local cerebral oxygenation. Crit Care Med. 2005;33:1104–8.
Topolovec-Vranic J, Santos M, Baker AJ, Smith OM, Burns KE. Deferred consent in a minimal-risk study involving critically ill subarachnoid hemorrhage patients. Can Respir J J Can Thorac Soc. 2014;21:293–6.
von Elm E, Altman DG, Egger M, Pocock SJ, Gotzsche PC, Vandenbroucke JP. Strengthening the reporting of observational studies in epidemiology (STROBE) statement: guidelines for reporting observational studies. BMJ (Clinical research ed). 2007;335:806–8.
Brain Trauma F, American Association of Neurological S, Congress of Neurological S. Guidelines for the management of severe traumatic brain injury. J Neurotrauma 2007;24(suppl 1):S1–106.
Wardle SP, Yoxall CW, Weindling AM. Determinants of cerebral fractional oxygen extraction using near infrared spectroscopy in preterm neonates. J Cereb Blood Flow Metab. 2000;20:272–9.
Watzman HM, Kurth CD, Montenegro LM, Rome J, Steven JM, Nicolson SC. Arterial and venous contributions to near-infrared cerebral oximetry. Anesthesiology. 2000;93:947–53.
Colquhoun DA, Tucker-Schwartz JM, Durieux ME, Thiele RH. Non-invasive estimation of jugular venous oxygen saturation: a comparison between near infrared spectroscopy and transcutaneous venous oximetry. J Clin Monit Comput. 2012;26:91–8.
Bland JM, Altman DG. Statistical methods for assessing agreement between two methods of clinical measurement. Lancet. 1986;1:307–10.
Kenward MG, Roger JH. Small sample inference for fixed effects from restricted maximum likelihood. Biometrics. 1997;53:983–97.
Leal-Noval SR, Rincon-Ferrari MD, Marin-Niebla A, et al. Transfusion of erythrocyte concentrates produces a variable increment on cerebral oxygenation in patients with severe traumatic brain injury: a preliminary study. Intensive Care Med. 2006;32:1733–40.
Nortje J, Gupta AK. The role of tissue oxygen monitoring in patients with acute brain injury. Br J Anaesth. 2006;97:95–106.
Rosenthal G, Hemphill JC 3rd, Manley G. Brain tissue oxygen tension is more indicative of oxygen diffusion than oxygen delivery and metabolism in patients with traumatic brain injury. Crit Care Med. 2009;37:379–80.
Kurtz P, Helbok R, Claassen J, et al. The effect of packed red blood cell transfusion on cerebral oxygenation and metabolism after subarachnoid hemorrhage. Neurocrit Care. 2016;24:118–21.
Sekhon MS, Griesdale DE, Czosnyka M, et al. The effect of red blood cell transfusion on cerebral autoregulation in patients with severe traumatic brain injury. Neurocrit Care. 2015;23:210–6.
Davies DJ, Su Z, Clancy MT, et al. Near-infrared spectroscopy in the monitoring of adult traumatic brain injury: a review. J Neurotrauma. 2015;32:933–41.
Acknowledgments
This work is supported by grants from Physicians’ Services Incorporated Foundation and St. Michael’s Trauma-Neuro Research Group.
Author Contribution
V.A.M. contributed to the literature search, study design, data analysis, data interpretation, writing, critical revision, and final approval. S.P. contributed to the literature search, study design, data interpretation, critical revision, and final approval. M.S. contributed to the data collection, critical revision, and final approval. W.X. contributed to the data analysis, data interpretation, critical revision, and final approval. A.L.D.O.M. contributed to data collection, critical revision, and final approval. A.R. contributed to the study design, data interpretation, critical revision, and final approval. G.M.H. contributed to the study design, data interpretation, critical revision, and final approval. M.G.C. contributed to the data interpretation, critical revision, and final approval. A.J.B. contributed to the study design, data analysis, data interpretation, writing, critical revision, and final approval.
Funding/Support
This work was supported by grants from the Physicians’ Services Incorporated Foundation and St. Michael’s Trauma-Neuro Research Group. Caster Medical Systems supplied the foresight cerebral tissue oximetry monitors during the study period. We separately purchased all the probes for study use. Rainbow® pulse co-oximetry monitors were provided by Masimo Canada, and probes were purchased for each study patient. All funding and support sources were not involved in the collection, analysis, and interpretation of data.
Author information
Authors and Affiliations
Corresponding author
Ethics declarations
Conflicts of interest
The authors have no conflicts of interest to declare.
Electronic supplementary material
Below is the link to the electronic supplementary material.
Rights and permissions
About this article
Cite this article
McCredie, V.A., Piva, S., Santos, M. et al. The Impact of Red Blood Cell Transfusion on Cerebral Tissue Oxygen Saturation in Severe Traumatic Brain Injury. Neurocrit Care 26, 247–255 (2017). https://doi.org/10.1007/s12028-016-0310-6
Published:
Issue Date:
DOI: https://doi.org/10.1007/s12028-016-0310-6