Abstract
Background
Severe middle cerebral artery stroke (MCA) is associated with a high rate of morbidity and mortality. We assessed the hypothesis that patient-specific variables may be associated with outcomes. We also sought to describe under-recognized patient-centered outcomes.
Methods
A consecutive, multi-institution, retrospective cohort of adult patients (≤70 years) was established from 2009 to 2011. We included patients with NIHSS score ≥15 and infarct volume ≥60 mL measured within 48 h of symptom onset. Malignant edema was defined as the development of midline brain shift of ≥5 mm in the first 5 days. Exclusion criterion was enrollment in any experimental trial. A univariate and multivariate logistic regression analysis was performed to model and predict the factors related to outcomes.
Results
46 patients (29 female, 17 male; mean age 57.3 ± 1.5 years) met study criteria. The mortality rate was 28 % (n = 13). In a multivariate analysis, only concurrent anterior cerebral artery (ACA) involvement was associated with mortality (OR 9.78, 95 % CI 1.15, 82.8, p = 0.04). In the malignant edema subgroup (n = 23, 58 %), 4 died (17 %), 7 underwent decompressive craniectomy (30 %), 7 underwent tracheostomy (30 %), and 15 underwent gastrostomy (65 %).
Conclusions
Adverse outcomes after severe stroke are common. Concurrent ACA involvement predicts mortality in severe MCA stroke. It is useful to understand the incidence of life-sustaining procedures, such as tracheostomy and gastrostomy, as well as factors that contribute to their necessity.
Similar content being viewed by others
Avoid common mistakes on your manuscript.
Introduction
Large territory middle cerebral artery strokes are devastating events that result in high rates of disability and death. In fact, nearly half of all stroke survivors never regain functional independence [1]. Additionally, stroke also carries an enormous cost. For example, during the acute hospitalization period there are many potential aspects of care that contribute to resource utilization, including the need for intensive care unit monitoring, mechanical ventilation, endovascular therapy, and even decompressive craniectomy [2, 3]. With this burden of disease in mind, it is necessary to define and predict poor outcomes in order to focus efforts on this “severe” stroke population. A better understanding of stroke severity may also allow for a more accurate determination of the effect from standard and experimental clinical interventions.
The severity of an ischemic infarct is classically defined by various criteria that relate to either factors that predict adverse outcomes [4–6] or the need for intensive therapy and surgical procedures [7–9]. It is possible that severe stroke may be independently defined by measures other than the two most common predictors of malignant edema formation and mortality (NIHSS score [10, 11] or infarct volume [7, 8]), such as the need for life-sustaining procedures. Currently, the rate of these procedures is unknown in the stroke population. We hypothesized that patient-specific variables may be associated with outcomes in severe anterior circulation ischemic stroke. We also sought to describe under-recognized outcomes as indicators of severe stroke in this population.
Methods
Study Population
We performed a consecutive retrospective cohort analysis of patients experiencing a severe anterior circulation ischemic stroke at the Massachusetts General Hospital and the University of Maryland Medical Center from January 2009–December 2011. This study was approved by respective institutional review boards.
Inclusion Criteria
Only adult patients (≤70 years and >18 years) with both left and right hemisphere ischemic stroke and admission NIHSS ≥15 were considered for inclusion. The NIHSS score cutoff was selected based on previous reports describing this population as “high-risk” for the development of malignant cerebral edema [10]. Patients were excluded beyond 70 years of age because of different management strategies for stroke in the elderly, particularly with respect to the use of decompressive craniectomy.
Exclusion Criteria
Patients were excluded if their initial infarct volume was ≤60 mL. We selected this value not as predictor value of malignant edema, but to identify patients in which malignant edema formation was possible. Patients were excluded if they were enrolled in any therapeutic experimental trial or if they presented with posterior circulation stroke.
Data Acquisition
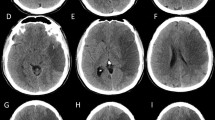
Patient characteristics were recorded including age, gender, nadir, and peak serum sodium within the first 5 days of admission, and in-hospital mortality. Other characteristics recorded included a determination of Glasgow Coma Scale (GCS) score decline by two or more points within the first 5 days of admission. Details of the stroke laterality, admission GCS score, anterior cerebral artery (ACA) involvement (vessel occlusion), and cardiac ejection fraction were recorded. The administration of hyperosmolar therapy was recorded as either continuous hyperosmolar therapy (3 % hypertonic saline infusion) and/or bolus hyperosmolar treatment (23.3 % hypertonic saline or mannitol). Details of any surgical procedure performed were noted, including decompressive craniectomy, tracheostomy, or gastrostomy. Infarct volume was estimated using the ellipsoid method of ABC/2 for the diffusion-weighted imaging bright area on initial MRI [12]. Malignant edema was defined as the development of midline brain shift (displacement of the septum pellucidum) of ≥5 mm in the first 5 days following admission [13].
Statistical Methods
Statistical analysis was performed using the R programming environment (Vienna, Austria). Univariate and multivariate logistic regression analysis was performed to model and predict the factors related to outcomes. Significance was predefined at p ≤ 0.05 (two-tailed).
Primary Analysis
Univariate and multivariate logistic regression analyses were used to analyze predictors of mortality in patients with severe anterior circulation stroke. The multivariate model was constructed using the least squares approach. Models were created including various predictors allowing for determination of individual regression coefficients and R-squared values. An analysis of variance was used to compare different models. Visual regression diagnostics were performed by plotting residual versus fitted values, standardized residuals versus theoretical quantiles, square root of standardized residuals versus fitted values, and standardized residuals versus leverage.
Secondary Analysis
Logistic regression analyses were then used to analyze predictors of secondary outcomes (including gastrostomy, tracheostomy, and malignant edema formation) in a similar fashion. Patients were censored from secondary analysis if therapeutic care was withdrawn within the first 48 h of admission.
Results
Primary Analysis
127 patients were first identified with NIHSS score ≥15. 81 patients were excluded due to either stroke size (n = 79) or participation in an experimental trial (n = 2). The final study population consisted of 46 patients (29 female, 17 male; mean age 57.3 ± 1.5 years). The mean time from symptom onset to decompressive craniectomy was 40.6 ± 6.8 h. Even though hyperosmolar therapy was administered in many patients, the correlation between serum sodium value and osmolality was good, with Pearson’s correlation coefficients of 0.85 and 0.77 for nadir and peak values, respectively. In patients receiving any form of hyperosmolar therapy, peak osmolality averaged 319.5 ± 4.3 mOsm/kg water. In comparison, patients receiving only mannitol averaged 326.6 ± 6.4 mOsm/kg water. If both mannitol and hypertonic saline were used, the mean peak osmolality was 331.0 ± 6.0 mOsm/kg water. The overall mortality rate was 28 % (n = 13). Univariate predictors of mortality were identified as infarct volume, administration of bolus ICP treatment, and anterior cerebral artery involvement (Table 1). In a multivariate model, only ACA involvement was predictive of mortality (OR 9.78, 95 % CI 1.15, 82.8, p = 0.04) (Table 2).
Secondary Analysis
Seven patients were excluded from secondary analysis because of early withdrawal of care. Univariate predictors of secondary outcomes were explored. Decompressive craniectomy and admission GCS score were associated with tracheostomy but not for gastrostomy. Univariate predictors of malignant edema included acute infarct volume, peak sodium, hyperosmolar therapy, and bolus ICP treatment (Table 3).
While no significant predictors of gastrostomy were identified in univariate analysis, significant independent predictors of tracheostomy and clinically predicted variables (age, infarct volume, ACA involvement, hyperosmolar therapy, bolus ICP treatment, midline shift) were introduced into a multivariate logistic regression analysis model, where only admission GCS was found to be predictive of tracheostomy (OR 0.59, 95 % CI 0.37, 0.94, p = 0.03) (Table 4).
Significant independent predictors of malignant edema formation and clinically predicted variables (age, NIHSS score, GCS score decline) were introduced into a multivariate logistic regression analysis model, where infarct volume was predictive of malignant edema formation (OR 1.02, 95 % CI 1.00, 1.04, p = 0.04) (Table 5). In the malignant edema subgroup (n = 23, 58 %) 4 died (17 %), 7 underwent DC (30 %), 7 underwent tracheostomy (30 %), and 15 underwent gastrostomy (65 %).
Additional rates of tracheostomy were 5/8 (63 %) in patients undergoing DC, 3/31 (9 %) in treated patients not undergoing DC, 0/13 (0 %) in patients suffering in-hospital mortality, and 8/33 (24 %) in all survivors.
Discussion
Severe middle cerebral artery (MCA) stroke can be generally defined based on the initial degree of neurological deficit, size of the stroke, or the propensity to require further interventions. With an emphasis on the latter, we utilized a large cohort of stringently selected patients to assess the hypothesis that patient-specific variables may be associated with outcomes. We also sought to describe under-recognized outcomes. The major finding of the analysis was that concurrent ACA involvement was associated with increased rates of mortality. Additionally, in certain subgroups, such as those undergoing decompressive craniectomy, a high percentage of patients underwent life-sustaining procedures such as tracheostomy (63 %). As the armamentarium in stroke care is growing with the expansion of image-guided decision making [14–16], novel pharmacologic therapies [17, 18], endovascular therapy [19–24], neurosurgery [25–28], and telemedicine [29, 30], it is important to establish benchmarks to evaluate outcomes related to these changes.
In our cohort, only ACA involvement was predictive of mortality. The ACA is well known to provide important collateral blood flow to the conventionally defined MCA territory [31], and therefore ACA ischemia is likely to be detrimental to the perfusion of various MCA territories as well. This is consistent with the finding that poor collateral circulation correlates with worse outcome [32–34]. The underlying mechanism, although not well defined, could be related to the development of cerebral edema. It has been shown that impaired collateral circulation is associated with this phenomenon [35, 36], one of the key determinants of outcome in severe stroke [9, 10, 37]. Therefore, it is possible that ACA involvement contributes to mortality as a mediator of collateral circulation and cerebral edema formation. It is also possible that ACA involvement co-varied with stroke volume, explaining why infarct volume was not a significant predictor in the multivariate analysis of mortality.
Our study is relevant in the context of an overall trend in severe stroke care towards being more interventional than observational. The increasing rate of endovascular treatment is likely to be magnified with the recent results of several stentreiver trials [19, 20]. Furthermore, surgical procedures that were once controversial, such as decompressive craniectomy, are becoming standard practice following recent randomized controlled trials demonstrating efficacy in selected populations [25–28]. With any of these treatment interventions, it is important to both define and predict outcomes. Severe strokes are more likely to require intensive care, have longer length of stays, require more neuroimaging, have a need for ventilator support, and suffer complications related to their hospitalization [38–42]. Importantly, our study quantifies that they may also require both life-saving and life-sustaining procedures, such as decompressive craniectomy, tracheostomy, and gastrostomy. This data may be useful for patient counseling, particularly when prognosticating an individual patient’s hospital course and the need for further intervention.
The vast majority of strokes can be described as “non-severe” [43, 44], therefore our study is strengthened by the utilization of two high-volume centers to maximize enrollment with this relatively small subset of patients. Our stringent selection criteria of both initial neurological deficit and stroke size allowed for a more homogenous selection of an inherently heterogeneous population. The use of any one single variable to screen for patients with “severe” stroke has the potential to miscategorize patients. For example, it is possible to have patients with NIHSS ≥15 without significant propensity for cerebral edema or neurological deterioration because of small volume, punctate lesions in eloquent cortex. Furthermore, we were also able to obtain detailed information from the medical record, such as neurological decline and neuroimaging volumetrics, variables that are not necessarily available in larger databases [45].
Limitations of the study are mainly attributable to its retrospective nature [46]. We attempted to overcome selection bias by utilizing a consecutive cohort from a comprehensive registry. There also exists practice variability between institutions and even between individual patients that is difficult to account for [47–49]. Additionally, while several factors were identified as significant, no single factor can predict outcome or neurological deterioration in severe stroke. One of the key applicable pieces of data useful for everyday practice is the quantitative assessment of life-sustaining procedures. These are outcome measures that can be used as benchmarks for future study and to guide prognostication for individual patients.
Conclusions
Adverse outcomes after severe stroke are common. Concurrent ACA involvement predicts mortality in severe MCA stroke. Knowledge of the incidence of life-sustaining procedures, such as tracheostomy and gastrostomy, is meaningful in clinical practice and should continue to be assessed in future study.
References
Roger VL, Go AS, Lloyd-Jones DM, Adams RJ, Berry JD, Brown TM, Carnethon MR, Dai S, de Simone G, Ford ES. Executive summary: heart disease and stroke statistics—2011 update a report from the American Heart Association. Circulation. 2011;123(4):459–63.
Qureshi AI, Suri MFK, Nasar A, Kirmani JF, Ezzeddine MA, Divani AA, Giles WH. Changes in cost and outcome among US patients with stroke hospitalized in 1990 to 1991 and those hospitalized in 2000 to 2001. Stroke. 2007;38(7):2180–4.
Mayer SA, Copeland D, Bernardini GL, Boden-Albala B, Lennihan L, Kossoff S, Sacco RL. Cost and outcome of mechanical ventilation for life-threatening stroke. Stroke. 2000;31(10):2346–53.
Warach S, Dashe JF, Edelman RR. Clinical outcome in ischemic stroke predicted by early diffusion-weighted and perfusion magnetic resonance imaging: a preliminary analysis. J Cereb Blood Flow Metab. 1996;16(1):53–9.
Sacco RL. Risk factors and outcomes for ischemic stroke. Neurology. 1995;45(2 Suppl 1):S10.
Castillo J, Leira R, García MM, Serena J, Blanco M, Dávalos A. Blood pressure decrease during the acute phase of ischemic stroke is associated with brain injury and poor stroke outcome. Stroke. 2004;35(2):520–6.
Oppenheim C, Samson Y, Manai R, Lalam T, Vandamme X, Crozier S, Srour A, Cornu P, Dormont D, Rancurel G. Prediction of malignant middle cerebral artery infarction by diffusion-weighted imaging. Stroke. 2000;31(9):2175–81.
Thomalla GJ, Kucinski T, Schoder V, Fiehler J, Knab R, Zeumer H, Weiller C, Röther J. Prediction of malignant middle cerebral artery infarction by early perfusion-and diffusion-weighted magnetic resonance imaging. Stroke. 2003;34(8):1892–9.
Hacke W, Schwab S, Horn M, Spranger M, De Georgia M, von Kummer R. ‘Malignant’middle cerebral artery territory infarction: clinical course and prognostic signs. Arch Neurol. 1996;53(4):309.
Krieger DW, Demchuk AM, Kasner SE, Jauss M, Hantson L. Early clinical and radiological predictors of fatal brain swelling in ischemic stroke. Stroke. 1999;30(2):287–92.
Smith EE, Shobha N, Dai D, Olson DM, Reeves MJ, Saver JL, Hernandez AF, Peterson ED, Fonarow GC, Schwamm LH. Risk score for in-hospital ischemic stroke mortality derived and validated within the get with the Guidelines-Stroke Program. Circulation. 2010;122(15):1496–504.
Sims J, Gharai LR, Schaefer P, Vangel M, Rosenthal E, Lev M, Schwamm L. ABC/2 for rapid clinical estimate of infarct, perfusion, and mismatch volumes. Neurology. 2009;72(24):2104–10.
Pullicino P, Alexandrov A, Shelton J, Alexandrova N, Smurawska L, Norris J. Mass effect and death from severe acute stroke. Neurology. 1997;49(4):1090–5.
Ribo M, Molina CA, Rovira A, Quintana M, Delgado P, Montaner J, Grivé E, Arenillas JF, Álvarez-Sabín J. Safety and efficacy of intravenous tissue plasminogen activator stroke treatment in the 3-to 6-hour window using multimodal transcranial Doppler/MRI selection protocol. Stroke. 2005;36(3):602–6.
Abou-Chebl A. Endovascular treatment of acute ischemic stroke may be safely performed with no time window limit in appropriately selected patients. Stroke. 2010;41(9):1996–2000.
Lees KR, Bluhmki E, Von Kummer R, Brott TG, Toni D, Grotta JC, Albers GW, Kaste M, Marler JR, Hamilton SA. Time to treatment with intravenous alteplase and outcome in stroke: an updated pooled analysis of ECASS, ATLANTIS, NINDS, and EPITHET trials. Lancet. 2010;375(9727):1695.
Walcott BP, Kahle KT, Simard JM. Novel treatment targets for cerebral edema. Neurotherapeutics. 2012;9(1):65–72.
Sheth KN, Kimberly WT, Elm J, Yarbrough K, O’Connor S, Hammer M, Kane A, Busl K, Cole T, Yoo AJ et al. GAMES (Glyburide Advantage in Malignant Edema and Stroke) Pilot Study In: International Stroke Conference. Hawaii; 2013.
Nogueira RG, Lutsep HL, Gupta R, Jovin TG, Albers GW, Walker GA, Liebeskind DS, Smith WS. Trevo versus Merci retrievers for thrombectomy revascularisation of large vessel occlusions in acute ischemic stroke (TREVO 2): a randomised trial. Lancet. 2012;380(9849):1231–40.
Saver JL, Jahan R, Levy EI, Jovin TG, Baxter B, Nogueira RG, Clark W, Budzik R, Zaidat OO. Solitaire flow restoration device versus the Merci Retriever in patients with acute ischemic stroke (SWIFT): a randomised, parallel-group, non-inferiority trial. Lancet. 2012;380(9849):1241–9.
Meyers PM, Schumacher HC, Connolly ES Jr, Heyer EJ, Gray WA, Higashida RT. Current status of endovascular stroke treatment. Circulation. 2011;123(22):2591–601.
Nogueira R, Schwamm L, Hirsch J. Endovascular approaches to acute stroke, part 1: drugs, devices, and data. AJNR Am J Neuroradiol. 2009;30(4):649–61.
Nogueira R, Yoo A, Buonanno F, Hirsch J. Endovascular approaches to acute stroke, part 2: a comprehensive review of studies and trials. AJNR Am J Neuroradiol. 2009;30(5):859–75.
Brinjikji W, Rabinstein AA, Kallmes DF, Cloft HJ. Patient outcomes with endovascular embolectomy therapy for acute ischemic stroke a study of the national inpatient sample: 2006 to 2008. Stroke. 2011;42(6):1648–52.
Jüttler E, Schwab S, Schmiedek P, Unterberg A, Hennerici M, Woitzik J, Witte S, Jenetzky E, Hacke W. Decompressive surgery for the treatment of malignant infarction of the middle cerebral artery (DESTINY) a randomized, controlled trial. Stroke. 2007;38(9):2518–25.
Vahedi K, Vicaut E, Mateo J, Kurtz A, Orabi M, Guichard JP, Boutron C, Couvreur G, Rouanet F, Touzé E. Sequential-design, multicenter, randomized, controlled trial of early decompressive craniectomy in malignant middle cerebral artery infarction (DECIMAL Trial). Stroke. 2007;38(9):2506–17.
Hofmeijer J, Kappelle LJ, Algra A, Amelink GJ, van Gijn J, van der Worp HB. Surgical decompression for space-occupying cerebral infarction (the hemicraniectomy after middle cerebral artery infarction with life-threatening edema trial [HAMLET]): a multicentre, open, randomised trial. Lancet Neurol. 2009;8(4):326–33.
Walcott BP, Kuklina EV, Nahed BV, George MG, Kahle KT, Simard JM, Asaad WF, Coumans JVCE. Craniectomy for malignant cerebral infarction: prevalence and outcomes in US Hospitals. PLoS ONE. 2011;6(12):e29193.
Pervez MA, Silva G, Masrur S, Betensky RA, Furie KL, Hidalgo R, Lima F, Rosenthal ES, Rost N, Viswanathan A. Remote supervision of IV-tPA for acute ischemic stroke by telemedicine or telephone before transfer to a regional stroke center is feasible and safe. Stroke. 2010;41(1):e18–24.
Schwamm LH, Holloway RG, Amarenco P, Audebert HJ, Bakas T, Chumbler NR, Handschu R, Jauch EC, Knight WA, Levine SR. A review of the evidence for the use of telemedicine within stroke systems of care a scientific statement from the American Heart Association/American Stroke Association. Stroke. 2009;40(7):2616–34.
Coyle P, Heistad DD. Blood flow through cerebral collateral vessels one month after middle cerebral artery occlusion. Stroke. 1987;18(2):407–11.
Souza L, Yoo A, Chaudhry Z, Payabvash S, Kemmling A, Schaefer P, Hirsch J, Furie K, González R, Nogueira R. Malignant CTA collateral profile is highly specific for large admission DWI infarct core and poor outcome in acute stroke. AJNR Am J Neuroradiol. 2012;33(7):1331–6.
Tan I, Demchuk A, Hopyan J, Zhang L, Gladstone D, Wong K, Martin M, Symons S, Fox A, Aviv R. CT angiography clot burden score and collateral score: correlation with clinical and radiologic outcomes in acute middle cerebral artery infarct. AJNR Am J Neuroradiol. 2009;30(3):525–31.
Maas MB, Lev MH, Ay H, Singhal AB, Greer DM, Smith WS, Harris GJ, Halpern E, Kemmling A, Koroshetz WJ. Collateral vessels on CT angiography predict outcome in acute ischemic stroke. Stroke. 2009;40(9):3001–5.
Kasner SE, Demchuk AM, Berrouschot J, Schmutzhard E, Harms L, Verro P, Chalela JA, Abbur R, McGrade H, Christou I. Predictors of fatal brain edema in massive hemispheric ischemic stroke. Stroke. 2001;32(9):2117–23.
Jaramillo A, Gongora-Rivera F, Labreuche J, Hauw JJ, Amarenco P. Predictors for malignant middle cerebral artery infarctions a postmortem analysis. Neurology. 2006;66(6):815–20.
Simard JM, Chen M, Tarasov KV, Bhatta S, Ivanova S, Melnitchenko L, Tsymbalyuk N, West GA, Gerzanich V. Newly expressed SUR1-regulated NCCa-ATP channel mediates cerebral edema after ischemic stroke. Nat Med. 2006;12(4):433–40.
Rordorf G, Koroshetz W, Efird JT, Cramer SC. Predictors of mortality in stroke patients admitted to an intensive care unit. Crit Care Med. 2000;28(5):1301.
Burtin P, Bollaert P, Feldmann L, Nace L, Lelarge P, Bauer P, Larcan A. Prognosis of stroke patients undergoing mechanical ventilation. Intensive Care Med. 1994;20(1):32–6.
Gujjar A, Deibert E, Manno E, Duff S, Diringer M. Mechanical ventilation for ischemic stroke and intracerebral hemorrhage Indications, timing, and outcome. Neurology. 1998;51(2):447–51.
Steiner T, Mendoza G, De Georgia M, Schellinger P, Holle R, Hacke W. Prognosis of stroke patients requiring mechanical ventilation in a neurological critical care unit. Stroke. 1997;28(4):711–5.
Menon SC, Pandey DK, Morgenstern LB. Critical factors determining access to acute stroke care. Neurology. 1998;51(2):427–32.
Feigin VL, Lawes CMM, Bennett DA, Barker-Collo SL, Parag V. Worldwide stroke incidence and early case fatality reported in 56 population-based studies: a systematic review. Lancet Neurol. 2009;8(4):355–69.
Petty GW, Brown RD Jr, Whisnant JP, Sicks JRD, O’Fallon WM, Wiebers DO. Ischemic stroke subtypes: a population-based study of incidence and risk factors. Stroke. 1999;30(12):2513–6.
Kleindorfer D, Lindsell CJ, Brass L, Koroshetz W, Broderick JP. National US estimates of recombinant tissue plasminogen activator Use ICD-9 codes substantially underestimate. Stroke. 2008;39(3):924–8.
Mantel N, Haenszel W. Statistical aspects of the analysis of data from retrospective studies of disease. J Natl Cancer Inst. 1959;22(4):719–48.
Mehta B, Leslie-Mazwi T, Chandra R, Chaudhry Z, Rabinov J, Hirsch J, Schwamm L, Rost N, Yoo A. Assessing variability in neurointerventional practice patterns for acute ischemic stroke. J Neurointerv Surg. 2013;5:i52–7.
Reeves MJ, Gargano J, Maier KS, Broderick JP, Frankel M, LaBresh KA, Moomaw CJ, Schwamm L. Patient-level and hospital-level determinants of the quality of acute stroke care a multilevel modeling approach. Stroke. 2010;41(12):2924–31.
Desai A, Bekelis K, Zhao W, Ball PA, Erkmen K. Association of a higher density of specialist neuroscience providers with fewer deaths from stroke in the United States population. J Neurosurg. 2013;118(2):431–6.
Disclosure
None.
Author information
Authors and Affiliations
Corresponding author
Rights and permissions
About this article
Cite this article
Walcott, B.P., Miller, J.C., Kwon, CS. et al. Outcomes in Severe Middle Cerebral Artery Ischemic Stroke. Neurocrit Care 21, 20–26 (2014). https://doi.org/10.1007/s12028-013-9838-x
Published:
Issue Date:
DOI: https://doi.org/10.1007/s12028-013-9838-x