Abstract
Background
The oxygen reactivity index (ORx) has been introduced to assess the status of cerebral autoregulation after traumatic brain injury (TBI) or subarachnoid hemorrhage (SAH). Currently, there is some controversy about whether the ORx depends on the type of PbrO2-sensor technology used for its calculation. To examine if the probe technology does matter, we compared the ORx and the resulting optimal cerebral perfusion pressures (CPPopt) of simultaneously implanted Licox (CC1.SB, Integra Neuroscience, France) and Neurovent-PTO (Raumedic, Germany) probes in patients after aneurysmal SAH or severe TBI.
Methods
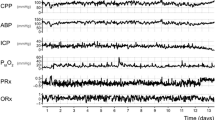
Licox and Raumedic probes were implanted side by side in 11 patients after TBI or SAH. ORx and CPPopt were recorded continuously. The equivalence of both probes was examined using Bland–Altman analyses.
Results
The mean difference in ORx was 0.1, with Licox producing higher values. The limits of agreement regarding ORx ranged from −0.6 to +0.7. When both probes’ ORx values were compared in each patient, no specific pattern in their relationship was seen. The mean difference in CPPopt was 0 mmHg with limits of agreement between −16.5 and +16.4 mmHg.
Conclusions
Owing to the rather limited number of patients, we view the results of this study as preliminary. The main result is that Licox and Raumedic showed consistent differences in ORx and CPPopt. Therefore, ORx values of both probes cannot be interchanged and should not be viewed as equivalent. This should be taken into consideration when discussing ORx data generated by different PbrO2 probe types.



Similar content being viewed by others
References
Sorrentino E, Diedler J, Kasprowicz M, et al. Critical thresholds for cerebrovascular reactivity after traumatic brain injury. Neurocrit Care. 2011. doi:10.1007/s12028-011-9630-8.
Czosnyka M, Balestieri M, Steiner L, et al. Age, intracranial pressure, autoregulation, and outcome after brain injury. J Neurosurg. 2005;102:450–1.
Jaeger M, Schuhmann MU, Soehle M, Meixensberger J. Continuous assessment of cerebrovascular autoregulation after traumatic brain injury using brain tissue oxygen pressure reactivity. Crit Care Med. 2006;34(6):1783–8.
Jaeger M, Schuhmann MU, Soehle M, Nagel C, Meixensberger J. Continuous monitoring of cerebrovascular autoregulation after subarachnoid hemorrhage by brain tissue oxygen pressure reactivity and its relation to delayed cerebral infarction. Stroke. 2007;38(3):981–6.
Radolovich DK, Czosnyka M, Timofeev I, et al. Reactivity of brain tissue oxygen to change in cerebral perfusion pressure in head injured patients. Neurocrit Care. 2009;10(3):274–9.
Jaeger M. Different indices to assess cerebrovascular autoregulation have different dynamic properties. Neurocrit Care. 2010;13(1):163–5.
Dengler J, Frenzel C, Vajkoczy P, Wolf S, Horn P. Cerebral tissue oxygenation measured by two different probes: challenges and interpretation. Intensive Care Med. 2011;37(11):1809–15.
The R project for statistical computing R 2.13.1. 2011. http://www.r-project.org. Accessed 20 September 2011.
Steiner LA, Czosnyka M, Piechnik SK, et al. Continuous monitoring of cerebrovascular pressure reactivity allows determination of optimal cerebral perfusion pressure in patients with traumatic brain injury. Crit Care Med. 2002;30(4):733–8.
Bland JM, Altman DG. Statistical methods for assessing agreement between two methods of clinical measurement. Lancet. 1986;1(8476):307–10.
Myles PS, Cui J. Using the Bland–Altman method to measure agreement with repeated measures. Br J Anaesth. 2007;99(3):309–11.
Bland JM, Altman DG. Agreement between methods of measurement with multiple observations per individual. J Biopharm Stat. 2007;17(4):571–82.
Critchley LA, Critchley JA. A meta-analysis of studies using bias and precision statistics to compare cardiac output measurement techniques. J Clin Monit Comput. 1999;15(2):85–91.
Haitsma I, Rosenthal G, Morabito D, Rollins M, Maas AI, Manley GT. In vitro comparison of two generations of Licox and Neurotrend catheters. Acta Neurochir Suppl (Wien). 2008;102:197–202.
Hoelper BM, Alessandri B, Heimann A, Behr R, Kempski O. Brain oxygen monitoring: in vitro accuracy, long-term drift and response-time of Licox- and Neurotrend sensors. Acta Neurochir (Wien). 2005;47:767–74.
Purins K, Enblad P, Sandhagen B, Lewen A. Brain tissue oxygen monitoring: a study of in vitro accuracy and stability of Neurovent-PTO and Licox sensors. Acta Neurochir (Wien). 2005;152(4):681–8.
Orakciouglu B, Sakowitz OW, Neumann JO, Kentar MM, Unterberg A, Kiening KL. Evaluation of a novel brain tissue oxygenation probe in an experimental swine model. Neurosurgery. 2010;67(6):1716–22.
Huschak G, Hoell T, Hohaus C, Kern C, Minkus Y, Meisel HJ. Clinical evaluation of a new multiparameter neuromonitoring device: measurement of brain tissue oxygen, brain temperature, and intracranial pressure. J Neurosurg Anesthesiol. 2009;21(2):155–60.
Barth M, Woitzik J, Weiss C, et al. Correlation of clinical outcome with pressure-, oxygen-, and flow-related indices of cerebrovascular reactivity in patients following aneurysmal SAH. Neurocrit Care. 2009;12(2):234–43.
Disclosure
The authors are not subject to any conflict of interest. The study was exclusively funded by the Department of Neurosurgery of the Charité, Berlin.
Author information
Authors and Affiliations
Corresponding author
Rights and permissions
About this article
Cite this article
Dengler, J., Frenzel, C., Vajkoczy, P. et al. The Oxygen Reactivity Index and Its Relation to Sensor Technology in Patients with Severe Brain Lesions. Neurocrit Care 19, 74–78 (2013). https://doi.org/10.1007/s12028-012-9686-0
Published:
Issue Date:
DOI: https://doi.org/10.1007/s12028-012-9686-0